Abstract
Purpose
Although advocated for severe varus and valgus deformities, constrained implant designs are associated with a number of disadvantages in total knee arthroplasty (TKA). Combining a minimally invasive surgical approach with an interchangeable posterior stabilized (PS) implant design may allow adequate soft tissue balancing with a minimal amount of constraint and without residual instability.
Methods
Retrospectively 51 patients operated with the minimally invasive far medial subvastus approach for severe varus or valgus deformity, who underwent primary TKA with a fully interchangeable PS implant (Vanguard, Biomet Inc., Warsaw IN, USA) between 2009 and 2013 were examined. Soft tissue releases was performed using a piecrust needling technique. Preoperative alignment and surgical parameters were collected for all patients. All patients underwent preoperative and follow-up radiographic assessment and completed a battery of clinical assessments.
Results
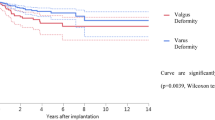
All procedures were performed successfully, with alignment improving from a preoperative mean (SD) varus deformity of 165° (3°) and a mean (SD) valgus deformity of 196° (4.5°) to an overall mean (SD) postoperative mechanical alignment of 179.5° (3.0°). Nine patients had postoperative varus, while three patients had a postoperative valgus deviation from neutral alignment >3°. The mean change in joint line position in extension was −0.0 ± 0.6 mm. Clinical scores at final follow-up were excellent for both groups.
Conclusions
Good TKA outcomes can be achieved in patients with substantial varus or valgus deformities using a combination of a minimally invasive far medial subvastus approach, interchangeable PS implants and soft tissue releases with a piecrust needling technique.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A stable and well-aligned joint is one of the primary goals of total knee arthroplasty (TKA) and is important for successful long-term clinical outcomes and patient satisfaction [25, 29], as well as implant survivorship [17, 49]. Central to this is the restoration of limb alignment by accurate implant positioning and soft tissue balancing [11, 33, 45, 46]. These challenges are magnified in TKA patients with severe deformity, particularly if the aim is to correct the deformity while balancing the soft tissues so as to use the least amount of constraint [37, 50]. The nature of preoperative deformity also differs from patient to patient [30], and varus and valgus knees present their own particular challenges. It has consequently been questioned whether it is even possible to predictably and successfully correct extreme deformity in a large number of cases [37].
Combining a primary posterior stabilized (PS) implant with minimally invasive surgery (MIS) offers several potential benefits, as MIS is associated with shorter hospitalization, reduced pain and more rapid return of function [10, 26, 39]. The surgical approach can have an important influence on soft tissue balancing. A medial collateral ligament (MCL)-sparing far medial subvastus approach in MIS TKA, was previously described with good surgical outcomes and no radiological malalignment [23, 52].
For the current study, primary TKA was performed in 51 patients with substantial preoperative deformities (at least >10° mechanical deformity), in which the far medial subvastus approach was combined with a PS implant and soft tissues releases performed with a piecrust needling technique [6, 7]. The hypothesis was that leaving the soft tissue sleeve intact would allow easier soft tissue balancing and that the use of the Vanguard (Biomet, Warsaw, US) implant, which allows full interchangeability of femoral and tibial sizes, would avoid the use of more constraint implants. Furthermore, the radiological and clinical outcome of these patients operated on with primary PS components was evaluated.
Materials and methods
Fifty-one patients (53 knees) with a fixed preoperative varus or valgus deformity, who had undergone primary TKA for primary osteoarthritis between 2009 and 2013 performed by a single surgeon (ET), were invited to participate in a retrospective study. All but seven patients (seven knee) consented to participate in the study, giving a population of 44 patients (46 knees). Seven patients were not included because one died, three lived in another country and three were not able to come back to the hospital for clinical and radiological examination. The living patients were all contacted by phone, as well as the family of the deceased patient. All were doing well and did not have symptoms of pain or instability and the deceased patient had not been revised before his death.
The mean (SD) age of the study population at the time of the surgery was 74 (9) years with 36 (70 %) women and 15 (30 %) men. Mean (SD) BMI was 31.5 (6) kg/m2. The mean (SD) follow-up time was 3 (2) years. Eight patients (16 %) developed arthritis post open meniscectomy. None of the patients had a history of previous fracture or osteotomy.
Hip–knee–ankle (HKA) angles were obtained from radiographic anteroposterior full-leg views of the lower extremity, with the patient standing in a weight-bearing position. Substantial deformity was defined as an angle of more than 10° of deviation on the neutral mechanical axis HKA measurement (<170° or >190° HKA angle) [35].
Surgical technique
All patients were operated by the same surgeon (ET), with staged bilateral knee replacement performed in two patients. A minimally invasive far medial subvastus approach [23, 52] was used in both varus and valgus deformities. A measured resection with a femur-first technique was taken. The level of resection was dependent on the deformity and the stability of the knee in extension. Massive valgus deformity associated with hyperextension/hyperlaxity usually requires a reduced depth of resection of the femur [14, 44], whereas varus with fixed flexion deformity often requires a deeper tibial resection depth to compensate for the eroded tibial bone and a more proximal femoral resection to obtain full extension. Another technique to accomodate for a deep posteromedial defect is to reduce the size of the tibial tray and lateralize the tibial component slightly, while resecting the overhung medial tibial bone (tibial reduction osteotomy) [13]. Deeper resection depth in the tibia during TKA leads to reduced surface area at the tibial plateau, in which case the implantation of a smaller tibia, is required due to the smaller surface of the underlying bone [9].
Alignment was confirmed with an extramedullary guide on the tibial side and an intramedullary guide on the femoral side. In patients with substantial varus deformity, the deep fibres of the MCL were released from the proximal tibia within the soft tissue sleeve. Soft tissue releases were performed using a needling technique [6], while the assistant applied valgus force to the leg. If necessary, the posterior oblique ligament, pes anserinus and/or the semimembranosus tendon were also released. In the knees with valgus deformity, release of the iliotibial band was performed via pie-crusting with a needle [6, 7, 44]. If required, additional release of the lateral collateral ligament, popliteus tendon and posterolateral capsule was carried out with great care, as there is a risk of posterolateral flexion gap instability, which necessitates the use of a constrained condylar prosthesis design [12, 27, 43, 56]. Ligament balancing was performed with the trial implants in place.
All patients received a cemented Vanguard PS knee (Biomet Inc., Warsaw IN, USA). No patients received a Condylar Constraint Knee or hinge design during the time period of the study. Postoperative rehabilitation consisted of immediate weight bearing and mobilization with the help of a physiotherapist. Full weight bearing was allowed as soon as the patient was able to perform a straight-leg raise.
Assessments
Clinical assessment was carried out using the Knee Society (KSS) clinical rating system [20], the patient-reported Knee Injury and Osteoarthritis Outcome Score (KOOS) [47] and the Forgotten Joint Score (FJS-12) [4, 53] at the final postoperative clinical evaluation. Residual pain, if present, was documented on a visual analogue scale (VAS). Each knee was also assessed for mobility and ligamentous stability.
Mean (SD) surgical time and type of approach was collected for each procedure, alongside the soft tissue releases performed and the need for femoral cut proximalization. Stability, as well as dynamic patellar tracking, was assessed during the procedure by the surgeon (ET). Postoperative morphine consumption, blood transfusion and length of stay were also collected.
At the final assessment, the tibial and femoral components were assessed radiographically using the Knee Society roentenographic evaluation system [15]. As well as implant position, each component was assessed for the presence of radiolucent lines. Preoperative and final radiographic assessment included weight-bearing full-leg alignment to measure the mechanical alignment of the lower limb (HKA angle) [35]. Outliers were defined as deviation of more than 3° from neutral alignment, as measured on a postoperative radiograph. Joint line restoration was measured in extension and in flexion [48]. In extension, the effect of the arthroplasty on patellar height, as measured using the modified Insall-Salvati ratio [18], was determined by comparing the preoperative and postoperative patella–patellar tendon ratio. This ratio was measured by determining the articular surface of the patella and the length of the patellar tendon to the insertion on the anterior surface of the proximal tibia.
Changes in preoperative and postoperative joint line position were documented. In flexion, the posterior condylar offset was evaluated on lateral radiographs by measuring the maximum thickness of the posterior condyle pre- and postoperatively, projected posteriorly to the tangent of the posterior cortex of the femoral shaft [5].
For the joint line and posterior condylar offset restoration, negative values indicated that the joint line position had been lowered, while positive values suggested that it had been raised.
Institutional Review Board approval was obtained by the Ethical Committee of the University Hospital Saint Luc, Brussels, Belgium.
Statistical analysis
Sample characteristics are presented as numbers, means, SDs and ranges. Categorical variables are presented as frequencies and percentages. The normal distribution of the data was assessed using the Kolmogorov–Smirnov test. The non-normally distributed data were analysed using the nonparametric statistical Mann–Whitney test for independent samples and Wilcoxon signed-rank test for dependent samples. Comparison of observed proportions was performed using chi-square and Fisher’s exact test. Logistic regression was used to assess the joint association of postoperative malalignment and the independent variables of interest: age; sex; and preoperative varus versus valgus angle. All analyses were performed using Stata 12.1 (StataCorp LP, College Station, TX, USA). A p value of <0.05 was considered significant.
Results
The mean (SD) preoperative varus deformity (N = 30) was 165° (3°) (range 169°–156°) and the mean (SD) preoperative valgus deformity (N = 16) was 196° (4.5°) (range 191°–213°) (p < 0.0001). Mean (SD) preoperative range of motion was an extension deficit of −3.5° (2°) and 115° (16°) of flexion. Postoperative clinical scores are presented in Table 1. Two patients had mild postoperative mediolateral instability (<5 mm), of which one had anteroposterior instability.
The mean (SD) surgical time was 97 (18) min without a difference for varus or valgus knees. Postoperative morphine was administered following 44 surgeries, at a mean (SD) dose of 48 (29) mg. The mean (SD) postoperative drop in haemoglobin (Hb) was 2 (0.5) g/dl. One patient (2 %) required postoperative blood transfusion. Another patient experienced patellofemoral pain and postoperative patellar clunk. No other major postoperative complications were recorded. Mean (SD) length of stay was 5.5 (1.5) days.
Radiolucent lines were absent in 40 patients. Four patients had radiolucent lines under the medial and lateral tibial baseplate, of those two patients had lines more medially and one patient had lines more laterally. These four patients had small tibias (Vanguard PS, size 63). Radiolucent lines were not observed around the femoral or patellar component. No aseptic loosening of components was seen.
By final follow-up, none of the patients required revision surgery and all implants were in situ. Mean (SD) overall postoperative mechanical alignment was 179.5° (3.0°) HKA angle. The mean (SD) postoperative alignment for the varus group (N = 30) was 178° (1°) with a range from 173° to 181°. The aim of the postoperative alignment was 178° from 2011 on, based on the under correction literature [8, 41, 54]. Nine (30 %) patients had a residual postoperative varus. The mean (SD) postoperative alignment for the valgus group (N = 16) was 180° (3°) with a range of 178°–187°. Three (19 %) patients had a postoperative valgus deviation from neutral alignment >3°. Mean (SD) coronal plane alignment of the femur was 85.5° (1°), while that for the tibia was 90° (1°). The mean (SD) change in joint line position in extension was −0.0 (0.5) mm. The mean (SD) change in posterior condylar offset was 2.1 (4.6) mm.
Logistic regression analysis revealed no significant associations between postoperative HKA angle deviation >3° and preoperative alignment, sex, age or the direction and magnitude of the preoperative deformity (Table 2).
Discussion
The most important finding of this study was that fixed deformities over 10° of mechanical malalignment can be treated with primary implants if: the approach does not destabilize the soft tissue sleeve; releases are titrated with a needling technique; and the primary implant allows for full interchangeability of femoral and tibial sizes.
The management of osteoarthritis in the presence of severe valgus and varus deformities is a surgical challenge that has been considered as one that calls for the use of higher constraint (CCK) or even hinged prostheses [34]. Concerns have been raised in the literature about constrained designs due to their disappointing results [30] and higher rate of complications [32, 38, 42]. Constrained implants are associated with increased polyethylene wear, higher modular and fixation interface stresses, reduced postoperative range of motion, increased operating time and prosthesis cost, and finally a high incidence of leg and thigh pain from canal invasion due to stem extension [2, 3, 19, 22, 24, 31, 36]. Constrained TKA is also associated with significantly more joint line elevation than unconstrained TKA in the valgus knee [40]. Varus–valgus constrained designs have been linked to removal of more femoral intercondylar bone to accommodate the femoral box [51] and an increased potential for aseptic loosening [16]. Despite recent work indicating that good outcomes can be obtained with constrained prostheses in primary cases [22], the recommendation that the minimum amount of constraint necessary to achieve stability should be used, still holds [31, 38, 51]. In this series of patients presenting with substantial deformities, the implantation of a primary standard PS knee design provided sufficient stability, and appropriately restored functional outcome. Intraoperative switch to a more constrained design was unnecessary, which is partly attributable to the knee design that was used allowing full interchangeability of sizes, such that the femoral component size can be selected independently of the tibial size. In cases where a deep tibial cut is necessary because of important wear, the use of a constrained knee design, in combination with block augmentation, can be avoided by a low resection of the tibia and covering the bone with a small tibial component. Interchangeability of component sizes obviates the need for femoral component downsizing to match the femur to a small tibia. Downsizing of the femoral component would lead to flexion instability, and the use of a thicker polyethylene insert to prevent this. As a result, the joint line is elevated [55]. In a recent study comparing joint line elevation in patients with valgus deformity, revision for global instability was required in 6 % of patients who received unconstrained TKA [41], where the mean joint elevation was 2.4 mm. Joint line elevation of +6 ± 2 mm, patella infera and impingement of the tibial post against the patellar component in deep flexion has been associated with constrained implants [40, 55]. In the current series, a mean (SD) change in joint line position in extension of −0.0 (0.5) mm was observed. This compares very favourably with results from previous investigations. One study of a posterior cruciate ligament–retaining, mobile-bearing TKA in 76 knees revealing a mean change in joint line position of +1.1 ± 4.6 mm [48], while a comparison of conventional and computer-assisted navigated (CAS) TKA in 493 primary TKAs suggested that conventional TKA was associated with an average joint line shift of 0.7 ± 4.4 and 0.6 ± 4.4 mm with CAS [21]. Furthermore, only two cases of postoperative instability were seen, suggesting that good ligament balancing was achieved.
Our findings show that the minimally invasive far medial subvastus approach, combined with an interchangeable PS implant, achieved excellent overall postoperative mechanical alignment, but a significant proportion of the cohort (27 %) showing deviation from neutral alignment >3°. The majority of patients did not have any radiolucent lines on postoperative follow-up without aseptic loosening, and average clinical outcome scores were highly suggesting the achievement of both good clinical outcomes and patient satisfaction. Furthermore, no patients required revision surgery. The observation of undercorrection in big deformities was made by other authors as well as the fact that undercorrected patients have better clinical outcome as observed for this study group [28, 30, 41, 54]. In the current study, it was observed that the mean Forgotten Joint Score (FJS-12) of these patients was higher (86.5) than the score for a normal control (82.5) in the index study on the FJS-12 from Behrend et al. [4]. This finding suggests that relative realignment for severe deformities results in a high degree of forgetting the joint because of the bad mechanical situation they were used to have previously.
During the literature review for this study, it was observed that the scientific semantics about lower limb alignment are very confusing and that this makes it difficult to compare results among papers as recently found by other authors [1]. Mechanical and anatomical alignment measurements are used across each other and sometimes alignment compared to the vertical axis is used with a wide range of normality depending of the author [37, 41, 45, 46]. In this paper, a new classification in different degrees of severity is proposed (Table 3) based on a literature review and the clinical experience of this study.
One of the primary limitations of our study is that it was a non-randomised, retrospective and of an observational nature study, which leaves it open to selection bias. Furthermore, relying on data from a single centre means that the findings may not be applicable to other institutions, where other surgical and rehabilitation protocols may be employed. The relatively small number of patients also means that drawing firm conclusions over improvements is difficult. The strength lies in the fact that a single surgeon using the same surgical approach and the same primary implant (Vanguard PS, Biomet, US) performed all the interventions.
Finally, after extensively reviewing the literature on mechanical alignment and lower limb deformities before TKA as well as our study group, a new classification for terminology of deformities is proposed in Table 3.
Conclusion
Highly favourable clinical, radiographic and alignment outcomes can be achieved with TKA in patients with severe varus or valgus deformities without recourse to constrained implant designs. The combination of a minimally invasive far medial subvastus approach, interchangeable PS implants and soft tissue release with a piecrust needling technique may imply that the benefits of more conventional implant designs can be made available to patients who would not hitherto be considered as potential candidates. Despite accurate component positioning, an important segment of patients retains their original alignment postoperatively on weight-bearing radiographs.
References
Abdel MP, Oussedik S, Parratte S, Lustig S (2014) Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J 96:857–862
Anderson JA, Baldini A, MacDonald JH, Pellicci PM, Sculco TP (2006) Primary constrained condylar knee arthroplasty without stem extensions for the valgus knee. Clin Orthop Relat Res 442:199–203
Barrack RL, Stanley T, Burt M, Hopkins S (2004) The effect of stem design on end-of-stem pain in revision total knee arthroplasty. J Arthroplasty 19(Suppl 2):119–124
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27:430–436
Bellemans J, Banks S, Victor J, Vandenneucker H, Moermans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84:50–53
Bellemans J (2011) Multiple needle puncturing: balancing the varus knee. Orthopedics 34(9):e510–e512
Bellemans J, Vandenneucker H, Van Lauwe J, Victor J (2010) A new surgical technique for medial collateral ligament balancing: multiple needle puncturing. J Arthroplasty 25(7):1151–1156
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Berend ME, Small SR, Ritter MA, Buckley CA (2010) The effects of bone resection depth and malalignment on strain in the proximal tibia after total knee arthroplasty. J Arthroplasty 25(2):314–318
Bonutti PM, Mont MA, McMahon M, Ragland PS, Kester M (2004) Minimally invasive total knee arthroplasty. J Bone Joint Surg Am 86-A(Suppl 2):26–32
Cameron HU, Hunter GA (1982) Failure in total knee arthroplasty: mechanisms, revisions, and results. Clin Orthop Relat Res 170:141–146
Carothers JT, Kim RH, Dennis DA (2008) Bent but not broken: managing severe deformity in total knee arthroplasty. Sem Arthr 19(1):103–108
Dixon M, Parsch D, Brown R, Scott R (2004) The correction of severe varus deformity in total knee arthroplasty by tibial component downsizing and resection of uncapped proximal medial bone. J Arthroplasty 19(1):19–22
Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS (2004) Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J Bone Joint Surg Am 86-A(12):2671–2676
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Forster MC (2003) Survival analysis of primary cemented total knee arthroplasty: which designs last? J Arthroplasty 18(3):265–270
Gioe TJ, Killeen KK, Grimm K, Mehle S, Scheltema K (2004) Why are total knee replacements revised?: analysis of early revision in a community knee implant registry. Clin Orthop Relat Res 428:100–106
Grelsamer RP, Meadows S (1992) The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res 282:170–176
Haas SB, Insall JN, Montgomery W 3rd, Windsor RE (1995) Revision total knee arthroplasty with use of modular components with stems inserted without cement. J Bone Joint Surg Am 77(11):1700–1707
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jawhar A, Shah V, Sohoni S, Scharf HP (2013) Joint line changes after primary total knee arthroplasty: navigated versus non-navigated. Knee Surg Sports Traumatol Arthrosc 21(10):2355–2362
King BR, Gladnick BP, Lee YY, Lyman S, Della Valle AG (2014) Range of motion and function are not affected by increased post constraint in patients undergoing posterior stabilized total knee arthroplasty. Knee 21(1):194–198
Koninckx A, Schwab PE, Deltour A, Thienpont E (2014) The minimally invasive far medial subvastus approach for total knee arthroplasty in valgus knees. Knee Surg Sports Traumatol Arthrosc 22:1765–1770
Krackow KA, Mihalko WM (1999) The effect of medial release on flexion and extension gaps in cadaveric knees: implications for soft-tissue balancing in total knee arthroplasty. Am J Knee Surg 12(4):222–228
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg [Am] 89A(4):780–785
Laskin RS, Beksac B, Phongjunakorn A, Pittors K, Davis J, Shim JC, Pavlov H, Petersen M (2004) Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res 428:74–81
Lombardi AV, Jr., Dodds KL, Berend KR, Mallory TH, Adams JB (2004) An algorithmic approach to total knee arthroplasty in the valgus knee. J Bone Joint Surg Am 86-A Suppl 2:62–71
Magnussen RA, Weppe F, Demey G, Servien E, Lustig S (2011) Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res 469:3443–3450
Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R (2011) The influence of preoperative deformity on intraoperative soft tissue balance in posterior-stabilized total knee arthroplasty. J Arthroplasty 26(8):1291–1298
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130:1487–1491
McAuley JP, Engh GA (2003) Constraint in total knee arthroplasty: when and what? J Arthroplasty 18(3 Suppl 1):51–54
McPherson EJ, Vince KG (1993) Breakage of a total condylar III knee prosthesis. A case report. J Arthroplasty 8(5):561–563
Mihalko WM, Miller C, Krackow KA (2000) Total knee arthroplasty ligament balancing and gap kinematics with posterior cruciate ligament retention and sacrifice. Am J Orthop (Belle Mead NJ) 29(8):610–616
Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA (2009) Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg 17(12):766–774
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69(5):745–749
Morgan H, Battista V, Leopold S (2005) Constraint in primary total knee arthroplasty. J Am Acad Orthop Surg 18(8):515–524
Mullaji AB, Padmanabhan V, Jindal G (2005) Total knee arthroplasty for profound varus deformity: technique and radiological results in 173 knees with varus of more than 20 degrees. J Arthroplasty 20(5):550–561
Naudie DD, Rorabeck CH (2004) Managing instability in total knee arthroplasty with constrained and linked implants. Instr Course Lect 53:207–215
Niki Y, Matsumoto H, Otani T, Enomoto H, Toyama Y, Suda Y (2010) Accuracy of implant positioning for minimally invasive total knee arthroplasty in patients with severe varus deformity. J Arthroplasty 25(3):381–386
Pang HN, Yeo SJ, Chong HC, Chin PL, Chia SL, Lo NN (2013) Joint line changes and outcomes in constrained versus unconstrained total knee arthroplasty for the type II valgus knee. Knee Surg Sports Traumatol Arthrosc 21(10):2363–2369
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF (2007) Rotating hinged total knee replacement: use with caution. J Bone Joint Surg Am 89(8):1735–1741
Rajgopal A, Dahiya V, Vasdev A, Kochhar H, Tyagi V (2011) Long-term results of total knee arthroplasty for valgus knees: soft-tissue release technique and implant selection. J Orthop Surg (Hong Kong) 19(1):60–63
Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S (2005) Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 87(Suppl 1):271–284
Ritter M, Davis K, Meding J, Pierson J, Berend M, Malinzak R (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg [Am] 93A(17):1588–1596
Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, Meding JB (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am 95(2):126–131
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Selvarajah E, Hooper G (2009) Restoration of the joint line in total knee arthroplasty. J Arthroplasty 24(7):1099–1102
Sharkey P, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today-has anything changed after 10 years? J Arthroplasty doi:10.1016/j.arth.2013.07.024
Siston RA, Goodman SB, Delp SL, Giori NJ (2007) Coronal plane stability before and after total knee arthroplasty. Clin Orthop Relat Res 463:43–49
Thienpont E (2012) Prosthesis selection: choosing the right type of constraint. In: Parvizi J (ed) Principles and techniques in revision total knee arthroplasty. American Academy of Orthopaedic Surgeons, Rosemount, pp 29–39
Thienpont E (2013) Faster quadriceps recovery with the far medial subvastus approach in minimally invasive total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21(10):2370–2374
Thienpont E, Opsomer G, Koninckx A, Houssiau F (2014) Joint awareness in different types of knee arthroplasty evaluated with the Forgotten Joint score. J Arthroplasty 29(1):48–51
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Verborgt O, Victor J (2004) Post impingement in posterior stabilised total knee arthroplasty. Acta Orthop Belg 70(1):46–50
Whiteside LA (1993) Correction of ligament and bone defects in total arthroplasty of the severely valgus knee. Clin Orthop Relat Res 288:234–245
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Muylder, J., Victor, J., Cornu, O. et al. Total knee arthroplasty in patients with substantial deformities using primary knee components. Knee Surg Sports Traumatol Arthrosc 23, 3653–3659 (2015). https://doi.org/10.1007/s00167-014-3269-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3269-x