Abstract
Purpose
A thorough understanding of the arthroscopic anatomy is important to recognise pathological conditions. Although some ankle ligaments have been described as intra-articular structures, no studies have assessed the full visibility of these structures. The purpose of this study was to assess arthroscopic visibility of medial and lateral ankle collateral ligaments.
Methods
Arthroscopy was performed in 20 fresh frozen ankles. The arthroscope was introduced through the anteromedial portal and the anterior compartment was explored in ankle dorsiflexion without distraction. Intra-articular structures were tagged using a suture-passer introduced percutaneously and they were listed in a table according to the surgeon’s identification. After the arthroscopic procedure, the ankles were dissected to identify the suture-tagged structures.
Results
According to the suture-tagged structures, 100% correlation was found between arthroscopy and dissection. In the anterior compartment, the superior fascicle of the anterior talofibular ligament, the distal fascicle of the anterior tibiofibular ligament and the anterior tibiotalar ligament on the medial side were observed. The deep fascicle of the posterior tibiofibular ligament and the intermalleolar ligament were tagged at the posterior compartment.
Conclusion
Ankle dorsiflexion and non-distraction arthroscopic technique allows full visualisation of the medial and lateral ankle collateral ligaments: the superior fascicle of the anterior talofibular ligament, the distal fascicle of the anterior tibiofibular ligament and the anterior tibiotalar ligament. When using distraction, posterior structures as the deep fascicle of the posterior tibiofibular ligament and the intermalleolar ligament can be observed with anterior arthroscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior ankle arthroscopy is a well-established technique, being used to treat numerous ankle pathologies [19]. A thorough understanding of the articular ankle anatomy or arthroscopic anatomy of the ankle is important to recognise pathological conditions and distinguish them from normal variants during any arthroscopic procedure.
Anterior arthroscopic anatomy of the ankle is of particular importance for the recently described arthroscopic techniques for lateral ankle instability [2, 4, 10, 12, 17, 18, 20, 21, 23].
Depending on their anatomical location relative to the capsule, ankle ligaments can be described as being intra-articular, partially intra-articular or extra-articular structures. The distal fascicle of the anterior tibiofibular ligament (ATiFL), and superior fascicle of the anterior talofibular ligament (ATFL) are intra-articular structures. The deep fascicle of the posterior tibiofibular ligament (PTiFL), intermalleolar ligament, deep layer of the deltoid ligament are partially intra-articular, whereas the ATFL’s inferior fascicle, calcaneofibular ligament, posterior talofibular ligament, superficial layer of the deltoid ligament, PTiFL’s superficial fascicle and the interosseous tibiofibular ligament are extra-articular [6, 22].
Intra-articular but extra-synovial structures can be visualized during arthroscopic procedures, while extra-articular structures can only be observed if the joint capsule is removed. However, studies assessing arthroscopic visibility of the lateral and medial ankle collateral ligaments have not been performed. A clear understanding of arthroscopic anatomy is important for diagnosis, arthroscopic exploration and treatment of ligamentous ankle injuries. In addition, clarification of the arthroscopically visualized structures and their correct terminology will assist in effective communication amongst clinicians.
We hypothesized that during anterior ankle arthroscopy with dorsiflexion and non-distraction technique the anterior part of both the lateral and medial ankle collateral ligaments (ATFL’s superior fascicle in the lateral aspect and anterior tibiotalar and tibionavicular ligaments in the medial aspect) can be visualized. In addition, when distraction is applied, the deep fascicle of PTiFL and intermalleolar ligament are visible at the posterior aspect of the ankle.
For this reason, this study was designed where ankle intra-articular ligamentous structures were corroborated via anatomic dissection.
Materials and methods
Twenty fresh frozen ankles (12 males and 8 females) amputated below the knee were used. IRB approval was obtained at our institution with IRB number 00003099.
The specimens were all of Caucasian origin with a median age of 64 years (mean 62, range 51–76). Specimens were excluded in the event of deformities, reduced ankle range of motion or scars indicating previous ankle surgery. Specimens were stabilised to the table using a holding device that grasped the proximal part of the tibia while allowing free ankle movement. The tibia was placed parallel to the floor.
A single surgeon, experienced in foot and ankle arthroscopy, performed all arthroscopic procedures. The procedure started with anterior compartment exploration in dorsiflexion without distraction. For the central (intra-articular or tibio-fibulo-talar) and the posterior compartments, distraction was required in all specimens.
A non-invasive distraction device attached to the surgeon’s waist was used to obtain ankle joint distraction when required.
The arthroscopic instruments include a 3.5 mm arthroscopic shaver and standard arthroscopic instruments. Two types of arthroscopes were used, a 4.0 mm 30° arthroscope for the anterior ankle compartment and a 2.7 mm 30° long arthroscope for the central and posterior compartments. No arthroscopic pump was used.
Two standard ankle arthroscopic portals, anteromedial and anterolateral, were created.
The anteromedial portal was created first. The portal was placed just medial to the tibialis anterior tendon. As the portal is created using a non-distraction technique, it should be at the ankle joint line or slightly proximal to it to avoid inadequate tilting of instruments when distraction is applied. This portal was regarded as the vision portal and arthroscopic exploration was carried out with the arthroscope introduced through it. A standardised arthroscopic exploration was performed in each compartment (anterior, central and posterior).
Once the anteromedial portal had been established, the anterolateral portal was created using a similar technique. This portal was regarded as the working portal for the introduction of instruments. The anterolateral portal was placed just lateral to the peroneus tertius tendon or to the extensor digitorum longus tendons.
A modified posterolateral portal [1] was created at the joint line, just posterior to the peroneal tendons, as an accessory portal to access the posterior compartment with instruments.
The anterior compartment was initially explored with the ankle in dorsiflexion using a 4 mm 30° arthroscope. Intra-articular soft tissue encountered in the anterior compartment was carefully debrided with a motorised shaver. The ankle joint capsule was not opened during soft-tissue debridement to avoid subcutaneous insufflation with fluid that could reduce intra-articular vision.
Ligaments were then identified and marked with a suture. The anterior ligamentous structures that were intended to be visualized laterally during arthroscopy were the ATFL’s superior fascicle and the ATiFL’s distal fascicle. On the medial side, it was the most anterior part of the deltoid ligament. Through direct arthroscopic vision, the ligaments were penetrated percutaneously with a suture-passer (Suture lasso, Arthrex, Naples, FL, USA) and a tag suture grabbed each ligament.
Distraction was then applied to the ankle joint. The arthroscope was then directed towards the posterior compartment. The posterior ligamentous structures intended to be visualized during posterior endoscopy were the intermalleolar ligament and the PTiFL’s deep fascicle (also known as the transverse ligament). Ligaments were also tagged using a percutaneously introduced suture-passer.
All the arthroscopic procedures were video recorded as part of the study and the tagged structures were listed in a table according to the surgeon’s identification.
After the arthroscopic procedure, the ankle was dissected to identify and visually corroborate the suture-tagged structures. All the specimens were dissected in a standardised manner by the same researcher, with extensive experience and specific training in anatomical plane-by-plane dissection. This dissection enabled the identification of the marked structures.
For anterior structures, a circular window was created, centred on the ankle joint. Tendons of the anterior compartment of the leg and the anterior joint capsule of the ankle were removed to visualise the ligamentous structures.
For the posterior structures, a window was created after removing the skin and local tendons, including the calcaneal or Achilles tendon, tibialis posterior, flexor digitorum longus and flexor hallucis longus tendons. Careful dissection of the posterior ankle joint capsule was then performed. It is important to note that the intermalleolar ligament is a thickening of the posterior ankle joint capsule and extreme caution is, therefore, required to avoid removing the ligament inadvertently. Once the tag sutures were visualized and the anatomic structures identified, the results were noted and photographs were taken.
The dissections were recorded digitally (Nikon D810, 105 mm Micro Nikon F 2.8 lens, raw format) to enable retrospective identification of structures.
Results
For both anterior and posterior ligamentous structures, full (100%) correlation was found between arthroscopy and dissection in all specimens.
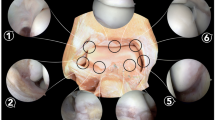
At the bottom of the lateral gutter, the ligamentous structure seen arthroscopically corresponds to the ATFL’s superior fascicle (Fig. 1). On the medial side, because of the disposition of the fibres of the deltoid ligament as superficial and deep layers, the dissected fibres correspond to the anterior fibres of the tibionavicular and anterior tibiotalar parts of the deltoid ligament. However, only the anterior fibres of the deep layer (anterior tibiotalar ligament) were observed arthroscopically (Fig. 2).
The PTiFL’s deep fascicle was tagged with a suture in the posterior ankle compartment, located at the most lateral aspect of the compartment, just posterior to the tibio-fibular joint line. The intermalleolar ligament was marked at its lateral part, just medial to the PTiFL’s deep fascicle. In this location, the ligament was observed during arthroscopic exploration in all specimens, while the medial part was covered by fatty tissue. A small area of joint capsule separates the PTiFL’s deep fascicle and the intermalleolar ligament. In all but one specimen, the flexor hallucis longus tendon was observed protruding through the posterior joint capsule.
Discussion
The most important finding in this study is that the anterior part of both the lateral and medial ankle collateral ligaments is observed through anterior ankle arthroscopy when using dorsiflexion and non-distraction technique. The intra-articular ligamentous structures seen arthroscopically correspond to the ATFL’s superior fascicle, the ATiFL’s distal fascicle and the anterior tibiotalar component of the deltoid ligament in the anterior compartment, plus the PTiFL’s deep fascicle and the intermalleolar ligament in the posterior compartment.
Anterior compartment ligaments are visible during ankle arthroscopy when applying dorsiflexion. Although some authors have described intra-articular portions of the ankle anatomy in a dorsiflexed position [18, 21], no detailed arthroscopic descriptions of the whole joint exist and no studies have correlated anatomic structures arthroscopically with anatomic dissection.
As observed in this study, the floor of the uninjured lateral gutter is formed by the ATFL’s superior fascicle that is relaxed with the ankle in dorsiflexion. It runs from the anterior aspect of the fibular malleolus to the lateral aspect of the talar neck, and it is seen as a hammock occupying the floor of the lateral gutter. The ATFL’s superior fascicle is an intra-articular ligament covered by a thin layer of synovial tissue [22]. However, when observed arthroscopically, only the medial border of the ligament is clearly defined while the lateral seems to be in continuity with the joint capsule. As a consequence, the ATFL’s superior fascicle has the false appearance of an extra-articular structure (Fig. 3).
Lateral view of a dissection of the ankle joint capsule. The capsule has been insufflated with air to clearly show its limits. 1, Anterior ankle joint capsule; 2, ATFL’s inferior fascicle; 3, dorsal talonavicular ligament; 4, dorsal calcaneocuboid ligament; 5, inferior peroneal retinaculum; 6, peroneus longus tendon; 7, peroneus brevis tendon. Nota bene: ATFL’s superior fascicle is not visible, as it is an intra-articular structure
The ATiFL’s distal fascicle, an intra-articular and constant ATiFL’s fascicle [6], covers the syndesmosis and the lateral shoulder of the talar dome. An important observation is the relationship between the ATiFL’s distal fascicle and the ATFL’s superior fascicle at their fibular origin. Although they are not anatomically connected, both origins are in continuity and this characteristic spot is arthroscopically visible during arthroscopy with the ankle in dorsiflexion. When an injury of the ATFL’s superior fascicle is present, a fibular bare or denuded area can be observed just distal to the fibular ATiFL insertion [11, 18], and a fibular gap between both ligaments can be observed.
In the posterior compartment, the PTiFL’s deep fascicle and the intermalleolar ligaments are visible through anterior portals and with the ankle joint in distraction. The superficial layer of the PTiFL, on the other hand, requires of hindfoot endoscopy for its visualisation. A number of ligamentous structures have been misidentified in the literature. The intermalleolar ligament has been erroneously identified as the PTiFL’s deep fascicle or the tibial slip, while the PTiFL’s deep fascicle has been called the postero-inferior tibiofibular ligament [7, 8, 15]. There is a need for clarification of the anatomic nomenclature that is used in the specialised literature. The correct name for the transverse ligament is “deep fascicle of the posterior tibiofibular ligament”, while the intermalleolar ligament is an intra-articular ligament reinforcing the posterior ankle capsule joint [5]. Controversy exists about the presence of the intermalleolar ligament which is encountered in the literature at varying rates, from 19 to 100% [3, 8, 13, 14, 16]. In the present study, this ligament was observed in all cases, and it is routinely identified by the authors in all arthroscopic procedures and anatomic dissections; thus, it has to be considered a constant posterior ankle ligament. The intermalleolar ligament has been reported as a potential cause of posterior impingement syndrome when it becomes trapped between the tibia and the talus in plantar flexion [9].
The limitations of this study include a small number of specimens and the elderly cohort of specimens. There is a higher risk of developing chronic ligamentous injuries with age, but any ligament tears identified during the study were excluded. All the ankles were first arthroscoped without applying distraction for the anterior compartment and thereafter under ankle distraction for the central and posterior compartments. Arthroscopic vision of the intra-articular ligaments in the anterior compartment can be limited or misrecognized when distraction is applied because of the effect of distraction itself.
The clinical relevance of the study is that the ATFL’s superior fascicle forms the floor of the lateral gutter and is seen as a hammock covered by synovial tissue. The most anterior part of the deep and superficial layers of the deltoid ligament is also recognised during ankle arthroscopy. The PTiFL’s deep fascicle and the intermalleolar ligament are recognized arthroscopically in the posterior compartment after ankle distraction is applied. As proved in this study, all these ligamentous structures can and should be recognised as part of the routine exploration during any ankle arthroscopic procedure. Surgeons specializing in ankle arthroscopy should be versed in the assessment of ligamentous injuries in the ankle and aim to ultimately treat these using entirely arthroscopic procedures.
Conclusions
Ligament structures observed arthroscopically have been corroborated in all dissected specimens. In the anterior compartment, only under ankle dorsiflexion and not under distraction, the ATFL’s superior fascicle can be observed on the floor of the lateral gutter, the ATiFL’s distal fascicle laterally, and the most anterior margin of the deltoid ligament in the medial gutter (anterior tibiotalar ligament). In the posterior compartment, and only under distraction, the PTiFL’s deep fascicle and the intermalleolar ligaments can be observed during arthroscopy.
References
Acevedo JI, Busch MT, Ganey TM, Hutton WC, Odgen JA (2000) Coaxial portals for posterior ankle arthroscopy: an anatomic study with clinical correlation on 29 patients. Arthroscopy 16:836–842
Acevedo JI, Mangone PG (2011) Arthroscopic lateral ankle ligament reconstruction. Tech Foot Ankle Surg 10:111–116
Bartonicek J (2003) Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat 25:379–386
Corte-Real NM, Moreira RM (2009) Arthroscopic repair of lateral ankle instability. Foot Ankle Int 30(3):213–217
Dalmau M, Vega J (2017) Letter regarding: cadaveric analysis of the distal tibiofibular syndesmosis. Foot Ankle Int 38(3):343–345
Dalmau M, Malagelada F, Kerkhoffs GMMJ, Karlsson J, Manzanares MC, Vega J (2018) The anterior tibiofibular ligament has a constant distal fascicle that contacts the anterolateral part of the talus. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5123-z
Ferkel RD (1966) Diagnostic arthroscopic anatomy. In: Whipple TL (ed) Arthroscopic surgery The foot and ankle. Lippincott-Raven, Philadelphia, pp 103–118
Golanó P, Mariani PP, Rodriguez-Niedenfuhr M, Mariani PF, Ruano-Gil D (2002) Arthroscopic anatomy of the posterior ankle ligaments. Arthroscopy 18:353–358
Golanó P, Vega J, de Leeuw PAJ, Malagelada F, Manzanares MC, Götzens V, van Dijk CN (2010) Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc 18(5):557–569
Guillo S, Archbold P, Perera A, Bauer T, Sonnery-Cottet B (2014) Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech 3(5):e593–e598
Kumai T, Takakura Y, Rufai A, Milz S, Benjamin M (2002) The functional anatomy of the human anterior talofibular ligament in relation to ankle sprains. J Anat 200(5):457–465
Matsui K, Takao M, Miyamoto W, Innami K, Matsushita T (2014) Arthroscopic Broström repair with Gould augmentation via an accessory anterolateral port for lateral instability of the ankle. Arch Orthop Trauma Surg 134:1461–1467
Milner CE, Soames RW (1998) Anatomy of the collateral ligaments of the human ankle joint. Foot Ankle Int 19:757–760
Oh CS, Won HS, Hur MS, Chung IH, Kim S, Suh JS, Sung KS (2006) Anatomic variations and MRI of the intermalleolar ligament. Am J Roentgenol 186(4):943–947
Patel D, Ghul JF (1988) Arthroscopic anatomy. In: Ghul JF (ed) Ankle arthroscopy. Slack, Thorofare, pp 13–24
Rosenberg ZS, Cheung YY, Beltran J, Sheskier S, Leong M, Jahss M (1995) Posterior intermalleolar ligament of the ankle: normal anatomy and MR imaging features. Am J Roentgenol 165(2):387–390
Takao M, Glazebrook M, Stone J, Guillo S (2015) Ankle Instability Group. Ankle arthroscopic reconstruction of lateral ligaments (ankle anti-ROLL). Arthrosc Tech 4(5):e595–e600
Vega J, Golanó P, Pellegrino A, Rabat E, Peña F (2013) All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot Ankle Int 34(12):1701–1709
Vega J, Dalmau M, Malagelada F, Fargues-Polo B, Peña F (2017) Ankle arthroscopy: an update. J Bone Joint Surg Am 99:1395–1407
Vega J, Allmendinger J, Malagelada F, Guelfi M, Dalmau M (2017) Combined arthroscopic all-inside repair of lateral and medial ankle ligaments is an effective treatment for rotational ankle instability. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4736-y
Vega J, Montesinos E, Malagelada F, Baduell A, Guelfi M, Dalmau-Pastor M (2018) Arthroscopic all-inside anterior talo-fibular ligament repair with suture augmentation gives excellent results in case of poor ligament tissue remnant quality. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5117-x
Vega J, Malagelada F, Manzanares MC, Dalmau M (2018) The lateral fibulotalocalcaneal ligament complex: an ankle stabilizing isometric structure. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5188-8
Vilá-Rico J, Cabestany-Castellà JM, Cabestany-Perich B, Núñez-Samper C, Ojeda-Thies C (2017) All-inside arthroscopic allograft reconstruction of the anterior talo-fibular ligament using an accessory transfibular portal. Foot Ankle Surg. https://doi.org/10.1016/j.fas.2017.12.008
Funding
No external funding was used for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
IRB approval was obtained at our institution with IRB number 00003099.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dalmau-Pastor, M., Malagelada, F., Kerkhoffs, G.M. et al. Redefining anterior ankle arthroscopic anatomy: medial and lateral ankle collateral ligaments are visible through dorsiflexion and non-distraction anterior ankle arthroscopy. Knee Surg Sports Traumatol Arthrosc 28, 18–23 (2020). https://doi.org/10.1007/s00167-019-05603-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05603-2