Abstract
Purpose
To evaluate the postoperative size of discoid lateral meniscus using magnetic resonance imaging (MRI) after partial meniscectomy relative to the size of medial meniscus midbody.
Methods
This study included 48 patients who underwent arthroscopic partial meniscectomy with or without repair for symptomatic complete discoid meniscus. The intraoperative size of midbody of medial meniscus was used as a reference for partial meniscectomy. MRIs were performed pre- and postoperatively. Quantitative evaluations of the height, width, extrusion of the meniscus, and relative percentage of extrusion in the coronal and sagittal planes were completed. Demographic data, preoperative shift, type of shift, and operative technique were analyzed while considering the remaining meniscus. Logistic regression analyses were used.
Results
The mean remaining discoid meniscal width in the coronal plane of MRI was not significantly different from the width of midbody of medial meniscus (9.1 ± 4.2 mm vs. 9.4 ± 1.4 mm, n.s.) Absolute meniscal extrusion and relative percentage of extrusion in the coronal plane and the ratio of t meniscus in sagittal plane of the final MRI were significantly increased as compared with the preoperative MRI. Preoperative shift was a risk factor for the reduction of remaining meniscal width (odds ratio 11.997, p = 0.016, 95% CI 1.586–90.737).
Conclusion
The size of midbody of medial meniscus could be a reference for partial meniscectomy in symptomatic complete discoid meniscus. Preoperative shift represents a risk factor for decreased remaining meniscal width. These findings could be helpful in ensuring appropriate surgical planning and explaining poor prognostic factors.
Level of evidence
Prospective cohort study, Level II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Discoid lateral meniscus (DLM) is the most common anatomical variation of the knee joint in pediatric patients. Discoid meniscus, when present, is almost always located on the lateral part of the knee, and medial discoid menisci are relatively rare [1, 2]. Anatomic variances, specifically abnormal shape, tissue thickness, abnormal collagen arrangement, loose attachment to the joint capsule, and poor vascularization [3,4,5], can be reasons for knee pain and functional limitations regardless of whether a meniscus tear is present [6].
Surgical treatment for a case of symptomatic discoid meniscus can be performed and includes partial meniscectomy, complete meniscectomy, meniscal repair, and regenerative techniques such as meniscal allograft transplantation [7,8,9]. Historically, total meniscectomy was preferred, because the collagen structure of the discoid meniscus varies from that of the normal meniscus [10,11,12,13]. For example, a total meniscectomy could be considered for an unstable discoid meniscus found without a meniscotibial ligament (Wrisberg variant) [5, 14]. However, total meniscectomy is not currently the first-line treatment option, because it leads to deteriorations of the lateral compartment, such as early degenerative arthritis [7, 15, 16]. Although partial meniscectomy of the central portion maintains meniscal function and preserves the peripheral meniscal remnant in discoid patients, a combination of meniscal repair options has shown better outcomes and resulted in less degenerative arthritis [17, 18]. Therefore, current treatment recommendations favor meniscal reshaping through partial meniscectomy with or without repair. Nonetheless, various guidelines for preserving the peripheral rim after reshaping in symptomatic DLM patients have been recommended in the literature (e.g., between 4–5 mm and 6–8 mm) [17, 19, 20]. Thus, there is no clear consensus as to how much peripheral rim of DLM should be preserved during surgery and what intraoperative anatomical references should be accepted to prevent a loss of function of the remaining DLM meniscus [7, 15, 17, 21,22,23]. The needs for intraoperative anatomical references certainly exist.
Meniscal extrusion is associated with cartilage degeneration and aggravated osteoarthritic changes after discoid meniscectomy as well as following meniscal transplantation or in the case of root and radial tears [24,25,26,27]. In particular, the morphology of collagen fibers in DLM is abnormal and there is a decreased amount of collagen fibers in comparison with in a normal meniscus [3, 28]. Recently, in a study by Yamasaki et al.,[23] it was found that the existence of less than 5 mm of remaining meniscal width and the occurrence of anterocentral meniscal shift could be risk factors for knee degeneration. Furthermore, they showed that the observation of anterocentral meniscal shift on preoperative magnetic resonance imaging (MRI) scan also could be a risk factor for less than 5 mm of remaining meniscal width.
Therefore, it is important to assess the factors that lead to meniscal extrusion and a smaller remaining meniscus after surgery for DLM. In addition, it is worthwhile to identify the ideal intraoperative references for meniscectomy to preserve the peripheral rim of DLM as much as possible. Thus, the purpose of this study was to evaluate the postoperative size of DLM using MRI after partial meniscectomy with or without repair and using the medial meniscus (MM) midbody as a size reference for surgery. In addition, we also attempted to identify factors associated with a smaller size in the remaining meniscus and with meniscal extrusion postoperatively. It has been hypothesized that the size of the MM midbody in a DLM knee would be a good intraoperative reference for partial meniscectomy [29,30,31,32]. It has also been suggested that the remaining meniscal size and position of DLM would be affected by predictive factors, including the presence of preoperative meniscal shift and the type of surgery.
Materials and methods
A prospective cohort study was performed involving a population who underwent arthroscopic surgery for a tear of the complete DLM between 2013 and 2016. The patient inclusion criteria were (1) symptomatic tear of complete-type DLM with arthroscopic surgery and (2) the completion of MRI evaluations in the preoperative and postoperative periods. The patient exclusion criteria were (1) a history of knee joint surgery or evidence of combined injury, such as ligament or osteochondral lesion; (2) incomplete discoid meniscus; (3) no definite unstable tear; and (4) subtotal or total meniscectomy patients.
All operations were performed by one experienced surgeon. Using the Watanabe classification, complete or incomplete DLM was determined from arthroscopic findings [33]. No cases of Wrisberg-type DLM were found. Partial meniscectomy was performed in 12 patients, while partial meniscectomy with repair was performed in 36 patients. Partial central meniscectomy was completed to remove the central portion of the thickened meniscus along with the torn, unstable portion, leaving behind a stable rim. The amount of partial meniscectomy was determined in reference to the intraoperative size of the MM midbody. The intraoperative size measurements were determined with a 5-mm probe or an arthroscopic ruler. After the central portion of the meniscus was removed, the remaining peripheral rim was carefully probed to ensure that there were no additional tears and that the rim was balanced and stable. When the peripheral rim tear of the DLM was reducible with a probe, suture repair was performed. All repairs were performed with absorbable sutures (No. 0 PDS; Ethicon, Somerville, NJ, USA), and different suture techniques were used depending on the properties of the tear site. However, when the loss of the posterolateral corner in the DLM was too large and not reducible with a probe, subtotal or total meniscectomy was considered instead.
MRI evaluation
All MRI examinations were performed on a 3.0-T scanner (Achieva; Phillips Medical Systems, Best, the Netherlands). Postoperative MRI scans were performed at a mean of 13.3 ± 2.4 months after surgery. During the scan, the knee was placed in a neutral position with an extremity coil. Coronal and sagittal images were acquired using turbo spin-echo (TSE) proton-density-weighted imaging (PDWI); sagittal TSE fat-saturated T2-weighted imaging (T2WI); axial, anterior cruciate ligament (ACL) oblique imaging; and posterior cruciate ligament (PCL) oblique fat-saturated TSE PDWI.
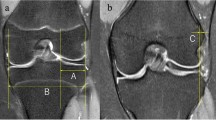
The width and height of the DLM and MM were measured in preoperative and postoperative MRI scans. Because maximum extrusion on the coronal plane usually occurs at the midbody, MM imaging in the coronal plane was used to evaluate the extrusion and size of the DLM and MM, respectively. The absolute extrusion length of DLM was defined as the distance between the outer margin of the tibial plateau and the meniscal outer margin [34]. A relative percentage of extrusion (RPE) was defined as the percentage of the width of an extruded meniscus compared to the entire meniscal width (Fig. 1a–c) [34,35,36].
Midbody image measurements in the coronal plane are shown. a Lateral meniscal midbody width and height are shown. b Measurement of absolute LM extrusion, which is defined as the distance between the outer margin of the tibial plateau and the meniscal outer margin, is shown. c Medial meniscal midbody width and height are shown
The mid positioned DLM image in the sagittal plane was used to measure the height of the DLM anterior and posterior horns and the width of the DLM. The DLM width was defined as follows: (a) the distance between the anterior margin of the tibial plateau and the meniscal anterior margin; (b) the distance between the meniscal anterior margin and the meniscal anterior–inner margin; (c) the distance between the meniscal anterior–inner margin and the meniscal posterior–inner margin; (d) the distance between the meniscal posterior–inner margin and the meniscal posterior margin; and (e) the distance between the meniscal posterior margin and the posterior margin of the tibial plateau. Because of the morphological features of the DLM, the “b” and “d” measurements ultimately could not be obtained (Fig. 2a, b). In addition, the sagittal ratio was defined as the percentage of the sagittal length of the meniscus (sum from “b” to “d”) compared to the entire sagittal length (sum from “a” to “e”). Based on the MRI findings, the preoperative DLM was categorized according to shifting meniscus morphologies in the sagittal and coronal images as defined by Ahn et al. [17, 37]. The categories were characterized according to the following types: (I) anterocentral shift, (II) posterocentral shift, (III) central shift, and (IV) no shift.
Midbody image measurements in the sagittal plane are shown. a Lateral meniscal length and height in the sagittal plane are shown. The length measurements are defined as follows: (a) distance between the anterior margin of the tibial plateau and the meniscal anterior margin; (b) distance between the meniscal anterior margin and the meniscal anterior–inner margin; (c) distance between the meniscal anterior-inner margin and the meniscal posterior–inner margin; (d) distance between the meniscal posterior–inner margin and the meniscal posterior margin; and (e) distance between the meniscal posterior margin and the posterior margin of the tibial plateau. The yellow arrow indicates the height of the anterior and posterior horns of the meniscus. b Preoperative DLM length and height in the sagittal plane are shown. “b” and “d” could not be measured due to morphology. The yellow arrow also indicates the height of the anterior and posterior horns of the meniscus
This study was approved by the institutional review board of Kyung Hee University Hospital at Gangdong (institutional review board/protocol no. KHNMC2013-01-047) and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Statistical analysis
Data were analyzed using the SPSS version 20.0 for Windows software (IBM Corp., Armonk, NY, USA). The primary outcome measure of the study was to find the equivalence of the mean coronal widths of the midbody of the MM and remaining DLM after surgery. Because there were no previous reports with a novel reference for partial meniscectomy of DLM patients in this study, a pilot study was performed. An allocation ratio was set at 1:1 and a sample size calculation was performed based on a pilot study of 10 patients who enrolled this study. The mean difference and standard deviation in the pilot study was 0.3 mm ± 0.98, and the equivalence limit was set as 1.0 mm for this study. We accepted a two-sided α error of 5% and a β error of 20% to detect any significant differences. Based on these calculations, the required study size was at minimum 47 cases, with the assumption of a 10% follow-up loss.
The quantitative sizes of the preoperative and postoperative meniscus were compared using the paired t test and independence t test after the Shapiro–Wilks test for normality. For the categorical analysis, a Chi-squared test was performed. Age, gender, preoperative symptom duration, the presence of preoperative meniscal shift (+/−), type of shift,[17, 37] operative technique, and preoperative meniscal size measurements (Tables 1, 2) were obtained to identify associations between size, absolute extrusion, and RPE in the remaining postoperative DLM. Binary logistic regression analysis was used to evaluate predictive variables for the risk of less than 6 mm remaining DLM after surgery to ensure a more conservative result [23]. Stepwise logistic regression analysis with backward elimination was performed with the results of the AIC. A linear regression analysis with stepwise method was performed to find associated factors with RPE and with the width of the remaining DLM. Statistical significance was set at p ≤ 0.05. All radiographic studies were reviewed by two musculoskeletal radiologists and consensus diagnoses were made. Test–retest was performed at 2 weeks after the first inspection and the average values were used for continuous variables. The inter- and intraobserver reliability of the measurements were assessed using the intraclass correlation coefficient (ICC) with two-way random absolute agreement or consistency, which quantifies the proportion of variance due to variability.
Results
Patient characteristics
A total of 136 patients with DLM were enrolled in this study. After applying the exclusion criteria, 48 consecutive patients with complete DLM were included in this study. Thirty-two cases were excluded because of combined osteochondral injury or ligament injury, 38 cases were excluded after subtotal or total meniscectomy, 10 cases were excluded because of no definite unstable tear, and eight cases were excluded because of incomplete discoid meniscus. Participant demographics are summarized in Table 1.
MRI evaluation of DLM size and extrusion
The preoperative and postoperative sizes and extrusions of DLM are summarized in Table 2. The DLM width and height in the coronal plane images were significantly different between the preoperative and postoperative periods. However, there were no differences between the remaining lateral meniscus (LM) and MM widths postoperatively, which means that the partial meniscectomy that was referenced to the MM width was satisfactory (p = 0.659). Interestingly, the meniscal height was increased after surgery (p = 0.016), while the intruded DLM preoperatively was extruded postoperatively (RPE: p = 0.002; absolute LM extrusion: p = 0.005). In the sagittal plane images, the sagittal ratio and the meniscal length were increased and significantly different after surgery (Table 2), but the meniscal anterior horn and posterior horn heights were not.
Postoperative MRI evaluations according to the coronal width of the remaining DLM after surgery are summarized in Table 3. Although the partial meniscectomy was performed referencing the MM width, 25% (12/48) of patients had a remaining meniscus of less than 6 mm. If the coronal width of the remaining DLM was small, the sagittal length of the remaining DLM was also smaller than that of the large coronal width of the remaining DLM patients, even though the partial meniscectomy was performed with the same reference.
Factors associated with width and extrusion of the remaining DLM
Factors associated with the width of the remaining DLM are summarized in Table 4. The only associated factors were the presence of preoperative meniscal shift and its type of shift. The odds ratio (OR) of the preoperative meniscal shift was 13.0 (95% confidence interval (CI) 2.413–70.051, p = 0.002) in the “less than 6 mm remaining” DLM group.
The linear regression analyses of the preoperative predictive factors for the width, absolute extrusion, and RPE of the remaining DLM are summarized in Table 5. The remaining DLM width was associated with the postoperative sagittal length of the remaining DLM (b + c + d) and the presence of preoperative meniscal shift. From the analysis, when preoperative meniscal shift was present, the postoperative width of the remaining DLM was decreased (Fig. 3). The absolute extrusion of the remaining DLM was associated with the postoperative meniscal sagittal length (b + c + d), postoperative anterior subluxation (“a”), postoperative height of the remaining DLM, and the presence of preoperative meniscal shift. From our analysis, increased sagittal length of the remaining DLM (b + c + d); decreased value of postoperative anterior subluxation (“a”, which means increased anterior subluxation of remaining DLM clinically); increased remaining DLM height; and the presence of preoperative meniscal shift were all associated with increased absolute extrusion of the remaining DLM (Table 5). In addition, the postoperative RPE of the remaining DLM was associated with anterior meniscal length (“b”) and increased height of remaining DLM. However, there were no preoperative factors associated with the RPE of the remaining DLM. Decreased anterior meniscal length (“b”) and increased remaining DLM height were both associated with increased RPE of the remaining DLM (Table 5).
Using logistic regression analysis with backward elimination, the factors associated with remaining DLM widths of less than 6 mm are detailed in Table 6. In an analysis of remaining DLM widths of less than 6 mm, the presence of preoperative meniscal shift and increased preoperative LM height were significantly predictive factors. The presence of preoperative meniscal shift was the major factor associated with a smaller width of the remaining DLM (Table 6).
The ICC values for radiographic reliability ranged from 0.81 to 0.90, indicating that raters were in good agreement.
Discussion
The most important finding of this study was that the mean width of the remaining DLM after surgery was comparable to the MM width when a partial meniscectomy with or without repair was performed in reference to the width of the MM. However, there was still a risk of decreased remaining DLM width, especially in patients with preoperative meniscal shift. This study is the first to introduce MM width as a surgical reference for partial meniscectomy in DLM patients. This novel surgical reference, MM size, could be appropriate for sufficiently preserving the DLM, although risks for smaller remaining DLM width and more extrusion of the remaining DLM were present. Using this reference, the remaining DLM was increased in height and length postoperatively as compared with in the case of the preoperative values (Table 2; LM height and sagittal ratio values) and also the intruded DLM preoperatively was extruded postoperatively (Table 2; values of RPE and absolute LM extrusion). Moreover, patients with smaller remaining DLM widths had smaller remaining DLM anterior and posterior lengths (Table 3; “b” and “d” in the sagittal plane images) Of the potentially associated factors, preoperative meniscal shift was the major significant factor for smaller width and greater extrusion of the remaining DLM, regardless of shift type.
Total and subtotal meniscectomy have been performed for DLM for many years and have demonstrated good clinical outcomes in long-term follow-up [7, 15, 17, 37, 38]. However, in many long-term studies, degeneration and arthritis change of the knee joint were reported after total and subtotal meniscectomy in juvenile DLM patients even with good clinical outcomes [16, 39,40,41]. Therefore, surgical treatment of DLM has been changed to partial meniscectomy with or without repair rather than total or subtotal meniscectomy. Although the collagen morphology of the DLM central portion has been shown to be heterogeneous via transmission electron microscopy, the DLM peripheral area contains circumferential fibers similar to the normal meniscus [28]. Because partial meniscectomy with or without repair is more likely to result in normal anatomy than total or subtotal meniscectomy in DLM patients, such could theoretically restore improved force distribution within the joint. Thus, this would be worthwhile to preserve the peripheral rim in a DLM patient, similar to in reports of tears of normal meniscus, where partial meniscectomy showed better outcomes as compared with total meniscectomy [40, 42]. However, there has been no consensus as to how much peripheral rim of the DLM should be preserved during surgery to prevent a loss of function of the remaining DLM meniscus, and risk factors to be considered in an effort sufficiently preserve DLM with the same surgical reference have not been explored.
To the best of our knowledge, this is the first study to introduce a surgical reference for partial meniscectomy of the DLM and to assess risk factors for smaller remaining DLM width using this novel surgical reference. In this study, using the MM width as a reference for partial meniscectomy could sufficiently preserve DLM. Moreover, the shape of the remaining DLM was greater in height and length and more extruded than that which was observed in preoperative DLM, much like a loosened “bowstring.” It is possible that the abnormal central portion collagen network of the DLM tethered the peripheral rim and thus the remaining DLM shape was greater in height and length and more extruded with peripheral contracture after partial meniscectomy. Although using the overall size and extrusion of the remaining DLM as a reference would be acceptable, there is still a risk of smaller remaining DLM, which could lead to degenerative changes [23, 39,40,41]. A few previous studies have reported remaining DLM cutoff widths of 3 mm and 5 mm that otherwise could induce degeneration [19, 23]. In the study by Yamasaki et al. [23], the authors had found that a remaining meniscal width of less than 5 mm, male gender, and anterocentral meniscal shift represented risk factors for degeneration after surgery. Moreover, they also determined that meniscal extrusion defined as RPE was correlated with degenerated change via radiography. In our study, we identified the risk factors of smaller remaining DLM width and the presence of preoperative meniscal shift, regardless of type, as major factors for smaller remaining DLM width. Consistent with the findings of Yamasaki et al. [23] preoperative meniscal shift is a major factor for poor prognosis of partial meniscectomy in DLM, including increased risk of smaller remaining DLM width. Moreover, combined meniscus repair could not guarantee a smaller remaining DLM width and prevent the development of degenerative change.
The degree of meniscal extrusion defined as RPE has been previously reported as a risk factor of degenerative change [23, 24, 43,44,45]. A meniscal extrusion of greater than 3 mm or severe extrusion (RPE > 50%) were associated with meniscal tearing, chondral degeneration, and malalignment, which could induce osteoarthritis [24, 43,44,45]. The load distribution capacity of the meniscus would be diminished with meniscal extrusion, thus leading to decreased contact area and increased pressure on the joint, which could lead to a further progression in cartilage degeneration. However, there have been few reports of meniscal extrusion in DLM patients to date [22, 23], and the cutoff value of the RPE correlated with degenerative change has not been confirmed. In this study, the factors associated with absolute LM extrusion and RPE of the remaining DLM after surgery were investigated (Table 5). Interestingly, the evaluation of the anterior portion of the remaining DLM (postoperative “a” and “b”) was correlated with the RPE and absolute LM extrusion (Table 5). As compared with in the case of the normal meniscus, the DLM may be susceptible to the effects of meniscal extrusion because of abnormal collagen fibers,[3, 28] and this anterior shifting of the remaining DLM postoperatively, for instance into a “bowstring” form, could be a potential risk factor for extrusion of the remaining DLM and a cause of degenerative progression. However, excluding preoperative meniscal shift, there were no other preoperative factors for extrusion of the remaining DLM. In addition, the power of explanation defined with the adjusted R2 value in this study was also found to be low. Further research is needed to define the correlations between DLM extrusion and position and long-term follow-up data are also required to identify which factors affect degeneration more significantly.
There are limitations to this study. First, the number of patients enrolled was relatively small and the findings obtained from these individuals may not necessarily represent those in the general population. In particular, the number of cases in each preoperative meniscal shift type was very small. Thus, it could not be confirmed whether the type of preoperative meniscal shift could affect the remaining DLM width, which was reported as a meaningful factor in the study of Yamasaki et al. [23]. Second, a combined analysis of clinical outcomes and long-term follow-up to assess degenerative change would be needed to confirm that these factors are clinically relevant. Moreover, with results from long-term outcomes, especially for degenerative change, cutoff values could be determined. Third, a comparison of meniscal size from normal patients would be needed to confirm that a partial meniscectomy referenced to the MM width is acceptable. However, the postoperative sizes of the MM and the remaining DLM were not significantly different and, thus, this novel reference could be used to preserve the remaining DLM. Fourth, this study was performed involving symptomatic Asian DLM patients. There could be differences of collagen fibers between ethnic groups, so care should be taken when extrapolating these results to other groups. Fifth, the surgical techniques could also affect the outcomes, although no significant differences were found in logistic regression analysis of this study due to the small number of cases involving partial meniscectomy only. However, as additional meniscus repair was performed in severe cases, which included the combined tear and shift of the discoid meniscus, the outcomes of this study using the size of the MM midbody as a reference could be applied robustly.
The described information can be a reasonable guideline to determine a preserving peripheral rim in partial meniscectomy for complete DLM. When a preoperative shift of DLM in preoperative MRI exists, the possibility of a small width of the remaining meniscal tissue after surgery, which might not ensure the maintenance of appropriate function of the meniscus, should be explained to patients preoperatively.
Conclusion
The size of midbody of medial meniscus could be a reference for partial meniscectomy in symptomatic complete discoid meniscus. However, a significant risk of greater extrusion of the remaining DLM in both coronal and sagittal planes are observed. Preoperative meniscal shift represent a risk factor for decreased remaining meniscal width. These findings could be helpful in ensuring appropriate surgical planning and explaining poor prognostic factors.
References
Dickason JM, Del Pizzo W, Blazina ME, Fox JM, Friedman MJ, Snyder SJ (1982) A series of ten discoid medial menisci. Clin Orthop Relat Res 168:75–79
Fritschy D, Gonseth D (1991) Discoid lateral meniscus. Int Orthop 15:145–147
Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL (2007) Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med 35:475–478
Hayashi LK, Yamaga H, Ida K, Miura T (1988) Arthroscopic meniscectomy for discoid lateral meniscus in children. J Bone Jt Surg Am 70:1495–1500
Jose J, Buller LT, Rivera S, Carvajal Alba JA, Baraga M (2015) Wrisberg-variant discoid lateral meniscus: current concepts, treatment options, and imaging features with emphasis on dynamic ultrasonography. Am J Orthop (Belle Mead NJ) 44:135–139
Adachi N, Ochi M, Uchio Y, Kuriwaka M, Shinomiya R (2004) Torn discoid lateral meniscus treated using partial central meniscectomy and suture of the peripheral tear. Arthroscopy 20:536–542
Ahn JY, Kim TH, Jung BS, Ha SH, Lee BS, Chung JW et al (2012) Clinical results and prognostic factors of arthroscopic surgeries for discoid lateral menisci tear: analysis of 179 cases with minimum 2 years follow-up. Knee Surg Relat Res 24:108–112
Andrish JT (1996) Meniscal injuries in children and adolescents: diagnosis and management. J Am Acad Orthop Surg 4:231–237
Yoo WJ, Jang WY, Park MS, Chung CY, Cheon JE, Cho TJ et al (2015) Arthroscopic treatment for symptomatic discoid meniscus in children: midterm outcomes and prognostic factors. Arthroscopy 31:2327–2334
Aglietti P, Bertini FA, Buzzi R, Beraldi R (1999) Arthroscopic meniscectomy for discoid lateral meniscus in children and adolescents: 10-year follow-up. Am J Knee Surg 12:83–87
Kaplan EB (1957) Discoid lateral meniscus of the knee joint; nature, mechanism, and operative treatment. J Bone Jt Surg Am 39-A:77–87
Pellacci F, Montanari G, Prosperi P, Galli G, Celli V (1992) Lateral discoid meniscus: treatment and results. Arthroscopy 8:526–530
Smillie IS (1948) The congenital discoid meniscus. J Bone Jt Surg Br 30B:671–682
Aichroth PM, Patel DV, Marx CL (1991) Congenital discoid lateral meniscus in children. A follow-up study and evolution of management. J Bone Jt Surg Br 73:932–936
Lee YS, Teo SH, Ahn JH, Lee OS, Lee SH, Lee JH (2017) Systematic review of the long-term surgical outcomes of discoid lateral meniscus. Arthroscopy 33:1884–1895
Räber DA, Friederich NF, Hefti F (1998) Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Jt Surg Am 80:1579–1586
Ahn JH, Lee SH, Yoo JC, Lee YS, Ha HC (2008) Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow-up. Arthroscopy 24:888–898
Kim SJ, Chun YM, Jeong JH, Ryu SW, Oh KS, Lubis AM (2007) Effects of arthroscopic meniscectomy on the long-term prognosis for the discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc 15:1315–1320
Lee DH, Kim TH, Kim JM, Bin SI (2009) Results of subtotal/total or partial meniscectomy for discoid lateral meniscus in children. Arthroscopy 25:496–503
Vandermeer RD, Cunningham FK (1989) Arthroscopic treatment of the discoid lateral meniscus: results of long-term follow-up. Arthroscopy 5:101–109
Ahn JH, Lee SH, Yoo JC, Lee HJ, Lee JS (2010) Bilateral discoid lateral meniscus in knees: evaluation of the contralateral knee in patients with symptomatic discoid lateral meniscus. Arthroscopy 26:1348–1356
Choi NH (2006) Radial displacement of lateral meniscus after partial meniscectomy. Arthroscopy 22:575 e571–e574
Yamasaki S, Hashimoto Y, Takigami J, Terai S, Takahashi S, Nakamura H (2017) Risk factors associated with knee joint degeneration after arthroscopic reshaping for juvenile discoid lateral meniscus. Am J Sports Med 45:570–577
Choi CJ, Choi YJ, Lee JJ, Choi CH (2010) Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26:1602–1606
Kijowski R, Woods MA, McGuine TA, Wilson JJ, Graf BK, De Smet AA (2011) Arthroscopic partial meniscectomy: MR imaging for prediction of outcome in middle-aged and elderly patients. Radiology 259:203–212
Lee DH, Lee BS, Kim JM, Yang KS, Cha EJ, Park JH et al (2011) Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 19:222–229
Noyes FR, Barber-Westin SD (2015) A systematic review of the incidence and clinical significance of postoperative meniscus transplant extrusion. Knee Surg Sports Traumatol Arthrosc 23:290–302
Cui JH, Min BH (2007) Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy 23:635–641
Bloecker K, Guermazi A, Wirth W, Benichou O, Kwoh CK, Hunter DJ et al (2013) Tibial coverage, meniscus position, size and damage in knees discordant for joint space narrowing—data from the Osteoarthritis Initiative. Osteoarthr Cartil 21:419–427
Bloecker K, Wirth W, Hudelmaier M, Burgkart R, Frobell R, Eckstein F (2012) Morphometric differences between the medial and lateral meniscus in healthy men—a three-dimensional analysis using magnetic resonance imaging. Cells Tissues Organs 195:353–364
Bowers ME, Tung GA, Fleming BC, Crisco JJ, Rey J (2007) Quantification of meniscal volume by segmentation of 3T magnetic resonance images. J Biomech 40:2811–2815
Gupta M, Goyal PK, Singh P, Sharma A (2018) Morphology of intra-articular structures and histology of menisci of knee joint. Int J Appl Basic Med Res 8:96–99
Watanabe M, Ikeuchi H, Takeda S (1979) Atlas of arthroscopy, 3rd edn. Igaku-Shoin, Tokyo
Verdonk P, Depaepe Y, Desmyter S, De Muynck M, Almqvist KF, Verstraete K et al (2004) Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12:411–419
Kim NK, Bin SI, Kim JM, Lee CR (2016) Does lateral meniscal allograft transplantation using the keyhole technique restore the anatomic location of the native lateral meniscus? Am J Sports Med 44:1744–1752
Lee DH, Kim JM, Jeon JH, Cha EJ, Bin SI (2015) Effect of sagittal allograft position on coronal extrusion in lateral meniscus allograft transplantation. Arthroscopy 31:266–274
Ahn JH, Lee YS, Ha HC, Shim JS, Lim KS (2009) A novel magnetic resonance imaging classification of discoid lateral meniscus based on peripheral attachment. Am J Sports Med 37:1564–1569
Smuin DM, Swenson RD, Dhawan A (2017) Saucerization versus complete resection of a symptomatic discoid lateral meniscus at short- and long-term follow-up: a systematic review. Arthroscopy 33:1733–1742
Abdon P, Turner MS, Pettersson H, Lindstrand A, Stenstrom A, Swanson AJ (1990) A long-term follow-up study of total meniscectomy in children. Clin Orthop Relat Res 257:166–170
Manzione M, Pizzutillo PD, Peoples AB, Schweizer PA (1983) Meniscectomy in children: a long-term follow-up study. Am J Sports Med 11:111–115
Wroble RR, Henderson RC, Campion ER, el-Khoury GY, Albright JP (1992) Meniscectomy in children and adolescents. A long-term follow-up study. Clin Orthop Relat Res 279:180–189
Baratz ME, Fu FH, Mengato R (1986) Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med 14:270–275
Badlani JT, Borrero C, Golla S, Harner CD, Irrgang JJ (2013) The effects of meniscus injury on the development of knee osteoarthritis: data from the osteoarthritis initiative. Am J Sports Med 41:1238–1244
Crema MD, Roemer FW, Felson DT, Englund M, Wang K, Jarraya M et al (2012) Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the Multicenter Osteoarthritis study. Radiology 264:494–503
Magee T (2008) MR findings of meniscal extrusion correlated with arthroscopy. J Magn Reson Imaging 28:466–470
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This is approved by the institutional review board of Kyung Hee University Hospital at Gangdong (Institutional Review Board/protocol number, KHNMC2013-01-047.) and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Kim, S.H., Ahn, J., Kim, T.W. et al. Midbody of the medial meniscus as a reference of preservation in partial meniscectomy for complete discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc 27, 2558–2567 (2019). https://doi.org/10.1007/s00167-018-5268-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5268-9