Abstract
Purpose
Kinematic alignment technique for TKA aims to restore the individual knee anatomy and ligament tension, to restore native knee kinematics. The aim of this study was to compare parameters of kinematics during gait (knee flexion–extension, adduction–abduction, internal–external tibial rotation and walking speed) of TKA patients operated by either kinematic alignment or mechanical alignment technique with a group of healthy controls. The hypothesis was that the kinematic parameters of kinematically aligned TKAs would more closely resemble that of healthy controls than mechanically aligned TKAs.
Methods
This was a retrospective case–control study. Eighteen kinematically aligned TKAs were matched by gender, age, operating surgeon and prosthesis to 18 mechanically aligned TKAs. Post-operative 3D knee kinematics analysis, performed with an optoelectronic knee assessment device (KneeKG®), was compared between mechanical alignment TKA patients, kinematic alignment TKA patients and healthy controls. Radiographic measures and clinical scores were also compared between the two TKA groups.
Results
The kinematic alignment group showed no significant knee kinematic differences compared to healthy knees in sagittal plane range of motion, maximum flexion, abduction–adduction curves or knee external tibial rotation. Conversely, the mechanical alignment group displayed several significant knee kinematic differences to the healthy group: less sagittal plane range of motion (49.1° vs. 54.0°, p = 0.020), decreased maximum flexion (52.3° vs. 57.5°, p = 0.002), increased adduction angle (2.0–7.5° vs. − 2.8–3.0°, p < 0.05), and increased external tibial rotation (by a mean of 2.3 ± 0.7°, p < 0.001). The post-operative KOOS score was significantly higher in the kinematic alignment group compared to the mechanical alignment group (74.2 vs. 60.7, p = 0.034).
Conclusions
The knee kinematics of patients with kinematically aligned TKAs more closely resembled that of normal healthy controls than that of patients with mechanically aligned TKAs. This may be the result of a better restoration of the individual’s knee anatomy and ligament tension. A return to normal gait parameters post-TKA will lead to improved clinical outcomes and greater patient satisfaction.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of patients following total knee arthroplasty (TKA) do not experience a natural knee joint [9]. A systematic review of gait analysis following TKA demonstrated that patients walked with less total range of knee motion and significant kinematic discrepancies to normal controls [24]. This may be one of the reasons that up to 20% of TKA patients are dissatisfied [4] and over 50% may have residual symptoms [27].
When TKA was first introduced in the 1970s, instrument precision was poor and implantation errors were frequent. There were many pitfalls to overcome, hence the focus was on implant survivorship, rather than reproducing normal knee function [33]. To achieve this, surgeons introduced the mechanical alignment (MA) technique. By selecting a neutral femoral and tibial cut with femoral rotation adapted to create equal femoral and extension gaps, a simple and reproducible method for alignment was created. Recent studies, however, have shown that the MA technique frequently results in significant anatomical modifications with a wide range of complex collateral ligament imbalances, which are not correctable by collateral ligament release [1, 12]. It is, therefore, unsurprising that TKA patients walk with an unnatural gait.
Kinematic alignment (KA) technique was introduced as a possible solution to the high dissatisfaction following TKA. The KA technique aims to restore the pre-arthritic patient’s constitutional knee alignment. It is almost a pure bone procedure with only exceptional collateral ligament release, which has been shown to reliably position knee components [14, 15]. Previous studies have compared clinical outcomes of KA with MA procedures [6, 11, 23, 34, 36]. These studies, however, did not perform any objective gait analysis on the two groups.
The aim of this study was to compare kinematic parameters during gait (i.e. flexion–extension, abduction–adduction and internal–external rotation of the tibia relative to the femur, as well as the walking speed) of TKA patients operated by either KA or MA technique with a group of healthy controls. The primary hypothesis was that these four kinematic parameters, measured in patients treated with KA TKA would more closely resemble healthy controls that patients treated with MA TKA. A return to normal gait parameters post-TKA will lead to improved clinical outcomes [17]. If KA TKA restores knee kinematics to normal, in contrast to MA TKA [24], this should lead to greater patient satisfaction.
Materials and methods
This is a retrospective case–control study comparing kinematic parameters following MA or KA TKA.
All surgery was performed at a single institution by the same experienced arthroplasty surgeon (P.-A.V.). The MA TKAs were performed between December 2008 and February 2011 when the surgeon was exclusively performing MA TKAs. The KA TKAs were performed between May 2012 and April 2015 when the surgeon was exclusively performing KA TKAs. Patients were recruited by a research nurse: all patients under 80 years of age, presenting at a minimum of 12 months post-primary TKA for degenerative arthritis of the knee were eligible. Patients were excluded if they had any post-operative complications requiring a secondary surgical procedure, or if they could not commit to performing the kinematic gait assessment.
A total of 18 knees [15 patients, 5 men (1 bilateral), 10 women (2 bilateral)] were recruited in the KA group. These were matched by gender, age and surgeon to 18 MA TKAs implanted with the same prosthesis [17 patients, 6 men, 11 women (1 bilateral)] from our database containing patients with studies of knee kinematics. Our database has 728 studies, of which 64 are on TKA patients. Best match to the KA group by prosthesis, age and gender was performed by an investigator blinded to the knee kinematic study results. The opto-electric knee assessment was performed at a mean of 33.5 months (range 12–96) post-operatively.
A control group of 95 healthy subjects (170 knees, 43 men, 52 women) from a previous study was used for comparison purposes [8].
Surgical procedure
All patients received a cruciate-retaining, fixed bearing implant (Triathlon, Stryker, MI, US). An anterolateral skin incision and medial parapatellar arthrotomy were used, without a tourniquet. Coronal plane alignment was achieved using optical computer navigation (Orthomap ASM, Stryker, Michigan) for both groups. In the MA group, coronal plane alignment in both the femur and tibia aimed for a neutral (0°) alignment to the mechanical axis. Femoral external rotation was set at 3° to the femoral posterior condyles.
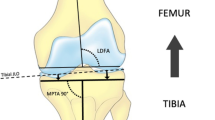
The KA technique used in the current study has been previously described as a “Restricted KA protocol” [1, 15]. The goal of the procedure is to resurface the knee according to each patient’s pre-arthritic anatomy, as closely as possible given the limitations of using standard implants. Distal femoral and proximal tibial cuts were adjusted to ensure an 8-mm resection on the intact femoral condyle and 9 mm on the tibial plateau, which represents the TKA implant thickness. On the worn side, fully exposed subchondral bone was considered to represent 2 mm of cartilage loss for females and 3 mm for males [20, 26]. The coronal resection angles were then adjusted to compensate. For example, in a female varus knee with full cartilage loss on the medial condyle and intact lateral side, medial resection would be 6 mm and lateral resection 8 mm. Secondary checks included calliper measurements of resected bone and comparison to pre-operative measurements performed on full-length weight-bearing lower limb radiographs of the lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA). Resections were modified from patient anatomy only if the measured angles fell outside a pre-defined “safe range” of either a combined coronal orientation within ± 3° of neutral and/or independent femoral or tibial cuts within ± 5° of neutral. Femoral external rotation was set at 0° to the femoral posterior condyles.
Kinematic data acquisition and processing
All patients underwent a 3D knee kinematic analysis with an opto-electric knee assessment device system (KneeKG®, Emovi Inc., Montreal, QC, Canada) [7, 13, 18, 22]. This device consists of a pelvic belt, a femoral harness, and a tibial plate, each mounted with three passive markers. The device measures 3D knee rotations with an accuracy of 0.4° for knee abduction/adduction, 2.3° for axial rotation, 2.4 mm for anteroposterior translation, and 1.1 mm for axial translation [30]. The repeatability ranges between 0.4 and 0.8° [13], and the reliability with intra-class coefficient (ICC) values ranges between 0.88 and 0.94 [18]. The device was applied to the operated limb of participants, who were asked to walk barefoot on a treadmill. After a period of habituation of 5 min, their comfortable walking speed was determined. It is then calibrated using a functional and anatomical procedure. The patients finally performed a 45-s walk routine, during which the motions of the device’s markers were recorded by a Polaris Spectra® camera (60-Hz). This protocol was repeated on the contralateral limb in cases of bilateral TKAs. After the tests, 3D knee kinematics were computed using software (Knee3D™, Emovi Inc., Montreal, Canada). Mean knee angles, i.e. flexion–extension in the sagittal plane, abduction–adduction in the frontal plane, and internal–external tibial rotation in the axial plane, of each patient were generated, as motion of the tibia relative to the femur, by keeping only the 15 most repeatable gait cycles.
Demographic and radiographic data
Demographic data including sex, age, height, weight and body mass index (BMI) were recorded. The Knee Injury and Osteoarthritis Outcomes Score (KOOS) was recorded pre-operatively and at the time of the kinematic assessment. The study groups’ data along with the normal controls’ data are presented in Table 1.
No significant differences were found, using a three-level one-way ANOVA, between MA and KA groups for any of the demographic measures or pre-operative KOOS score (p > 0.05). Significant differences were found between both TKA groups and the control group for age, weight and BMI (p < 0.001).
Radiographic measurements were performed on coronal full-length weight-bearing and short lateral radiographs by a single investigator using Impax software. Measurements included the hip–knee–ankle angle (HKA); joint line obliquity angle (JLOA); tibial and femoral component coronal alignment and; tibial and femoral component sagittal alignment.
Ethical approval was obtained from the research and ethics committee (CIUSSS de l’Est-de-l’Île-de-Montréal, Project number 2011-462), and all patients gave informed consent.
Statistical analysis
A sample size calculation was performed using data from our control group. The maximum knee flexion in swing phase was 57.5° (SD 6.0). A change of 5° was deemed to be clinically significant. Using a power of 80% and alpha < 0.05, 12 patients were required in each group. This was increased by 50% to 18, to allow for multiple comparisons.
Three-dimensional kinematic curves of MA, KA and control groups were compared at each point using a three-level one-way ANOVA, with a Bonferroni post hoc test. Comparisons of radiographic and demographic data were performed between the MA TKA and KA TKA groups using the unpaired Student’s T test. Significance was set at an alpha value of 0.05. All statistical analyses were undertaken with SPSS 21 (IBM Corp., Armonk, NY, USA).
Results
Range of motion of the knee, maximum knee flexion during swing phase, parameters in the sagittal plane
Figure 1 shows 3D knee kinematics for the MA, KA, and control groups. Compared to the healthy knee group, overall knee range of motion (ROM) and maximal swing phase knee flexion during normal gait were not significantly different in the KA group. These measures, however, were significantly decreased in the MA group (see Table 2). Comparing KA and MA, there was a significant difference in maximum flexion in swing phase with the MA group achieving less (52°) compared to the KA group (57°, p = 0.035).
Adduction parameter: a kinematic parameter in the coronal plane
Abduction–adduction curves for the KA group did not show any significant difference with the healthy knee group throughout the gait cycle. Significant differences were evident between the MA and control groups, with MA knees being more adducted than the healthy knees (2.0–7.5° vs. − 2.8–3.0°, p < 0.05) for most of the swing phase (66–94% of gait cycle).
Internal–external tibial rotation parameter
Internal–external tibial rotation curves for the KA group showed significant differences with the healthy knee group for a negligible portion of the initial swing phase (67–71% of gait cycle). KA knees displayed a peak of external tibial rotation while the healthy knees were in internal rotation (1.7–2.5° vs. − 1.9 to − 1.4°, p < 0.05). Conversely, MA internal–external tibial rotation was significantly different from healthy knees’ internal–external tibial rotation for various portions of the gait cycle. This included the loading response and mid-stance phases (3–22% of gait cycle), a portion of terminal stance (35–38% of gait cycle), the initial swing phase (65–73% of gait cycle), and the end of the terminal swing phase (90–94% of gait cycle). On average, the MA group had more knee external tibial rotation by 2.3 ± 0.7° during the whole gait cycle compared to the healthy knee group (p < 0.001).
Walking speed
There was no significant difference between the KA group and the control group in the walking speed (0.68 vs. 0.75 m/s, p = 0.063). The MA group, however, was significantly slower than the healthy knee group (0.65 vs. 0.75 m/s, p < 0.001).
Radiographic analyses
Radiographic outcomes are presented in Table 3. Significant differences between KA and MA groups are present in the JLOA, femoral and tibial component coronal alignment. There are no significant differences in the HKA and sagittal component alignment measures.
Clinical outcomes
The post-operative KOOS score was significantly higher in the KA group compared to the MA group (74 vs. 61, p = 0.034).
Discussion
The main finding of this study was that the knee kinematics of patients with KA TKAs more closely resembled that of normal healthy controls than that of patients with MA TKAs. The KA group showed no significant differences for sagittal plane range of motion, maximum flexion and abduction/adduction curves. They demonstrated a significant difference in the transverse plane for a negligible portion (< 5%) of the gait cycle, compared to 39% of the cycle for the MA group. The MA group displayed many significant differences to the control group: less sagittal plane range of motion. decreased maximum flexion, increased adduction angle, and increased external tibial rotation. These kinematic differences translated to a significantly better KOOS score in the KA TKAs compared to the MA TKAs (+ 13.5 points, p = 0.034).
TKA patients operated on using traditional MA technique have significant kinematic discrepancies during gait compared to normal healthy controls [24]. KA TKA may offer a solution to these gait abnormalities by restoring the femoral flexion axis, the longitudinal axis in the tibia about which it internally and externally rotates on the femur, and the transverse axis in the femur about which the patellar flexes and extends. There are only two other studies, of which we are aware, that have compared gait parameters between KA and MA TKAs [25]. McNair et al., comparing the gait in 15 MA patients with 14 KA patients, found a significantly greater internal rotation moment in the MA group from mid to late stance. Although there were differences in the other knee kinematics, the study was likely underpowered to reach significance. Furthermore, they did not have a healthy control group. Niki et al. in a similar matched study of KA and MA TKAs found an increased knee adduction moment in the MA group (3.83 vs. 2.89, p < 0.05) [28].
Evaluating the sagittal knee kinematics in the present study, the mean maximum flexion of the knee in the MA group (52°) was significantly less than both the healthy control group (57°) and the KA group (57°). There was also decreased range of motion (ROM) in the sagittal plane during gait for the MA group (49°) compared to both the healthy controls and the KA groups (54° for both), though statistical significance was only achieved for the former group. Decreased flexion during the swing phase of gait and decreased total ROM in the sagittal plane are consistent findings in gait analysis studies of patients following TKA surgery [24]. Increases in sagittal plane ROM and maximum knee flexion during gait are positively associated with patient’s satisfaction [32], functional abilities and level of physical activity post-TKA [3]. Therefore, the findings of this study might partly explain the better functional outcomes of KA TKAs over MA TKAs.
In the coronal plane, the KA group displayed no significant difference with the control group. However, the MA group had significantly increased adduction for most of the swing phase, whereas the control group was abducted. Evaluating HKA on long-standing films, there was no significant difference between KA and MA groups. The JLOA in the KA group, however, tended to be more parallel to the floor or slope down medially while the JLOA in MA group tended to slope down laterally. Interestingly, even with similar HKAs, we found that MA TKAs have a larger mean dynamic adduction angle during gait when compared to KA TKAs. Standing limb coronal alignment has been shown to be a poor predictor of the dynamic coronal alignment and adduction moments of MA TKAs [29]. Knee adduction angle through stance is correlated with the dynamic load on the medial compartment of the knee, with a greater angle resulting in a larger adduction moment, increased joint reaction force [5] and early TKA implant loosening [2]. Corroborating our results, Niki et al. similarly found an increased knee adduction moment in KA TKAs compared to MA TKAs [28]. They also concluded that this was likely a result of the effect of the differences in the JLOA between the two groups.
Regarding axial knee kinematics, the KA group displayed a minimal significant difference to the healthy control group at beginning of swing phase (for < 5% of the gait cycle), compared to the MA group with many significant differences throughout the gait cycle (3–22%, 35–38%, 53%, 65–73, 90–94%). Furthermore, the MA group had significantly more knee external tibial rotation by a mean of 2.3° throughout the whole gait cycle compared to the control group. Increased external tibial rotation has been shown to have an effect on polyethylene wear in knee simulator testing [16].
The improved knee kinematic profile of KA TKAs compared to MA TKAs may be explained by the fact that KA technique is an almost exclusively bony procedure [14, 15]. It aims to reproducibly restore the patient-specific femorotibial joint line orientation and native soft tissue balance, reducing the occurrence of knee balance-related complications and poor knee kinematics that traditionally affect MA TKAs. The significantly higher post-operative KOOS score seen in the KA group compared to the MA group may be a result of this improved knee kinematics. Three RCTs [6, 11, 23] and five meta-analyses [10, 19, 21, 31, 35] have also reported better clinical scores (KSS and WOMAC) with KA compared to MA TKAs.
A few limitations should be discussed that might affect generalisation of our findings. First, surgeries were performed by one surgeon, using a single implant and cannot be generalised to all TKAs. Second, the KA technique used does not represent true KA for 100% of the patients. Using a restricted KA protocol, it is estimated that 50% of the cases had their knee anatomy restored and the others needed minor corrections to fit the “safe range” of the restricted KA protocol [1]. Third, there is a high inter-individual variability in knee kinematics and gait pattern. Ideally, we should have compared the prosthetic knee kinematics with a healthy contralateral knee. Fourth, our sample size in the MA and KA groups was underpowered to reach significance for some of the differences detected between these two groups. Finally, this was not a randomised trial and the case–control design of the trial may introduce potential bias.
At present there is no long-term data on KA TKAs, so it is important to generate outcome data for patients that have undergone the procedure. One of the aims of KA TKA is to reproduce a more natural feeling joint. Therefore, the results of this study are promising, as it has demonstrated a more normal gait in KA TKAs than MA TKAs, compared to healthy controls.
Conclusion
The knee kinematics of patients with KA TKAs more closely resembled that of normal healthy controls than that of patients with MA TKAs. This may be the result of a better restoration of the individual’s knee anatomy and ligament tension.
References
Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli P-A (2017) The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplasty 32:2133–2140
Andriacchi TP, Stanwyck TS, Galante JO (1986) Knee biomechanics and total knee replacement. J Arthroplasty 1:211–219
Arnold JB, Mackintosh S, Olds TS, Jones S, Thewlis D (2015) Improvements in knee biomechanics during walking are associated with increased physical activity after total knee arthroplasty. J Orthop Res 33:1818–1825
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Butler RJ, Barrios JA, Royer T, Davis IS (2011) Frontal-plane gait mechanics in people with medial knee osteoarthritis are different from those in people with lateral knee osteoarthritis. Phys Ther 91:1235–1243
Calliess T, Bauer K, Stukenborg-Colsman C, Windhagen H, Budde S, Ettinger M (2017) PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 25:1743–1748
Clément J, de Guise JA, Fuentes A, Hagemeister N (2018) Comparison of soft tissue artifact and its effects on knee kinematics between non-obese and obese subjects performing a squatting activity recorded using an exoskeleton. Gait Posture 91:197–203
Clément J, Toliopoulos P, Hagemeister N, Desmeules F, Fuentes A, Vendittoli P-A (2018) Healthy 3D knee kinematics during gait: differences between women and men, and correlation with X-ray alignment. Gait Posture 64:198–204
Collins M, Lavigne M, Girard J, Vendittoli PA (2012) Joint perception after hip or knee replacement surgery. Orthop Traumatol Surg Res 98:275–280
Courtney PM, Lee GC (2017) Early outcomes of kinematic alignment in primary total knee arthroplasty: a meta-analysis of the literature. J Arthroplasty 32:2028–2032
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Jt J 96-B:907–913
Gu Y, Roth JD, Howell SM, Hull ML (2014) How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? AAOS exhibit selection. J Bone Jt Surg Am 96:e101
Hagemeister N, Parent G, Van de Putte M, St-Onge N, Duval N, de Guise J (2005) A reproducible method for studying three-dimensional knee kinematics. J Biomech 38:1926–1931
Howell SM, Howell SJ, Hull ML (2010) Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J Bone Jt Surg Am 92:98–104
Hutt JRB, LeBlanc MA, Massé V, Lavigne M, Vendittoli PA (2016) Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res 102:99–104
Johnson TSLM, Yao JQ, Gilbertson LN (2001) The effect of displacement control input parameters on tibiofemoral prosthetic knee wear. Wear 250:222–226
Kirschberg J, Goralski S, Layher F, Sander K, Matziolis G (2018) Normalized gait analysis parameters are closely related to patient-reported outcome measures after total knee arthroplasty. Arch Orthop Trauma Surg 138:711–717
Labbe DR, Hagemeister N, Tremblay M, de Guise J (2008) Reliability of a method for analyzing three-dimensional knee kinematics during gait. Gait Posture 28:170–174
Lee YS, Howell SM, Won YY, Lee OS, Lee SH, Vahedi H et al (2017) Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4558-y
Li G, Park SE, DeFrate LE, Schutzer ME, Ji L, Gill TJ et al (2005) The cartilage thickness distribution in the tibiofemoral joint and its correlation with cartilage-to-cartilage contact. Clin Biomech (Bristol Avon) 20:736–744
Li Y, Wang S, Wang Y, Yang M (2018) Does kinematic alignment improve short-term functional outcomes after total knee arthroplasty compared with mechanical alignment? A systematic review and meta-analysis. J Knee Surg 31:78–86
Lustig S, Magnussen RA, Cheze L, Neyret P (2012) The KneeKG system: a review of the literature. Knee Surg Sports Traumatol Arthrosc 20:633–638
Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R (2017) Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Jt J 99-B:640–646
McClelland JA, Webster KE, Feller JA (2007) Gait analysis of patients following total knee replacement: a systematic review. Knee 14:253–263
McNair PJ, Boocock MG, Dominick ND, Kelly RJ, Farrington BJ, Young SW (2017) A comparison of walking gait following mechanical and kinematic alignment in total knee joint replacement. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.09.031
Nam D, Lin KM, Howell SM, Hull ML (2014) Femoral bone and cartilage wear is predictable at 0 degrees and 90 degrees in the osteoarthritic knee treated with total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:2975–2981
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Jt J 96-B:96–100
Niki Y, Nagura T, Nagai K, Kobayashi S, Harato K (2018) Kinematically aligned total knee arthroplasty reduces knee adduction moment more than mechanically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1629–1635
Riviere C, Ollivier M, Girerd D, Argenson JN, Parratte S (2017) Does standing limb alignment after total knee arthroplasty predict dynamic alignment and knee loading during gait? Knee 24:627–633
Sati M, de Guise J, Larouche S, Drouin G (1996) Improving in vivo knee kinematic measurements: application to prosthetic ligament analysis. Knee 3:179–190
Takahashi T, Ansari J, Pandit HG (2018) Kinematically aligned total knee arthroplasty or mechanically aligned total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/s-0038-1632378
Turcot K, Sagawa Y Jr, Fritschy D, Hoffmeyer P, Suva D, Armand S (2013) How gait and clinical outcomes contribute to patients’ satisfaction three months following a total knee arthroplasty. J Arthroplasty 28:1297–1300
Vendittoli PA, Blakeney W (2017) Redefining knee replacement. Orthop Traumatol Surg Res 103:977–979
Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD (2016) The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Bone Jt J 98-B:1360–1368
Yoon JR, Han SB, Jee MK, Shin YS (2017) Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty: a meta-analysis. Medicine (Baltimore) 96:e8157
Young SW, Walker ML, Bayan A, Briant-Evans T, Pavlou P, Farrington B (2017) The Chitranjan S. Ranawat Award: no difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res 475:9–20
Funding
Research funds were provided by Maisonneuve-Rosemont Hospital Fundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the author have proprietary, financial, professional or other personal interest of any nature or kind of any product, service and/or company that could be construed as influencing the position presented in the manuscript.
Ethical approval
Ethical approval was obtained from the research and ethics committee (CIUSSS de l’Est-de-l’Île-de-Montréal, Project number 2011-462), and all patients gave informed consent.
Rights and permissions
About this article
Cite this article
Blakeney, W., Clément, J., Desmeules, F. et al. Kinematic alignment in total knee arthroplasty better reproduces normal gait than mechanical alignment. Knee Surg Sports Traumatol Arthrosc 27, 1410–1417 (2019). https://doi.org/10.1007/s00167-018-5174-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5174-1