Abstract
Purpose
The purpose of this review was to compare outcomes and complication profiles of anterior cruciate ligament reconstruction (ACL-R) between full thickness (FT-Q) and partial thickness (PT-Q) quadriceps tendon (QT) autografts.
Methods
As per PRISMA guidelines, PubMed, EMBASE, and MEDLINE were searched in September 2017 for English language, human studies of all levels of evidence on patients undergoing primary ACL-R with FT-Q or PT-Q. This search was repeated in March 2018 to capture additional articles. Data regarding postoperative outcomes and complications were abstracted. Due to heterogeneous reporting, data were not combined in meta-analysis and were summarized descriptively.
Results
Upon screening 3670 titles, 18 studies satisfied inclusion/exclusion criteria. The second search identified an additional two studies for a total of 20 studies (50% case–control, 50% case series). These studies examined 1212 patients (1219 knees) of mean age 29.8 years (range 15–59) followed a mean of 42.2 months (range 12–120). FT-Q and PT-Q autografts were used in eight studies (50.5% of knees), and thirteen studies (49.5% of knees), respectively. Only one study directly compared FT-Q to PT-Q. Instrumented laxity was less than 3 mm in 74.8 and 72.4% of the FT-Q and PT-Q groups, respectively. Postoperative IKDC Subjective Knee Form scores were similar between the FT-Q (82.5) and PT-Q (82.1) groups. Postoperative quadriceps strength, measured as a percentage of the contralateral side, were similar in the FT-Q (89.5%) and PT-Q (85.1%) groups. Graft failure rates for the FT-Q and PT-Q groups were 3.7 and 3.0%, respectively.
Conclusion
Across the 20 studies included in this review, there appeared to be no difference in outcomes or complications between either FT-Q or PT-Q in primary ACL-R. Moreover, primary ACL-R using QT autografts appears to have successful outcomes with a low rate of graft failure, irrespective of tendon thickness. While further comparative studies are needed to better delineate the optimal thickness of quadriceps tendon for primary ACL-R, these data suggest that, in primary ACL-R, either FT-Q or PT-Q is efficacious and, in the clinical setting, surgeons may be justified in using either graft thickness.
Level of evidence
IV, Systematic Review of Level III and IV studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous studies have found favorable results with the use of quadriceps tendon autografts (QT) during anterior cruciate ligament reconstruction (ACL-R) [13, 36]. Commonly cited benefits of QT over other commonly used autografts, including bone-patellar tendon-bone (BPTB) and hamstring (HS) autografts, include decreased graft-site morbidity, improved versatility, and predictability of size on pre-operative imaging [13, 16, 18, 28, 32, 36]. Compared to BPTB and HS, there are fewer studies investigating the optimal technique for performing ACL-R with QT, as exemplified by the finding in a 2010 study that only 2.7% of all reported autografts for ACL-R were QT [41]. Greater understanding of the benefits and drawbacks of various aspects of ACL-R with QT, including graft thickness, graft fixation, or the inclusion of a bone block, would assist clinicians in optimizing ACL-R with QT.
Techniques for ACL-R with QT have been described using both partial and full thickness quadriceps tendon grafts. Previous anatomic analyses of the quadriceps tendon have found the average thickness of the distal tendon to be approximately 8 mm with an average thickness of 16–18 mm at the patellar insertion [36, 44]. Techniques vary and have been described for harvesting either full thickness [1, 20] or partial thickness grafts, [15, 18, 28, 40] which range anywhere from 6 to 8 mm. Theoretical advantages of a full thickness graft include increased graft tensile strength, lower rates of graft failure, and improved stability, whilst theoretical drawbacks include increased graft site morbidity as well as the risk of entering the knee joint capsule or suprapatellar bursa during harvest. While one recent systematic review reported successful outcomes with ACL-R using QT, the authors did not specifically examine whether graft thickness influenced outcomes [36]. Previous studies of ACL-R with HS have found that increased graft size does correlate with reduced rates of graft failure requiring revision surgery and that a graft diameter less than 8 mm is specifically correlated with an increase revision rate [10, 30, 31, 39]. Given that reported techniques for partial thickness QT autografts report average graft thickness of 6–8 mm, [15, 18, 28, 40], a systematic investigation of graft thickness and outcomes is warranted. While there have been multiple published reviews of quadriceps tendon autografts in the last several years, [3, 19, 32, 36], none of these studies specifically examined the influence of graft thickness on outcomes. Consequently, there does not appear to be any consensus to guide surgeons in choosing whether to harvest a partial or full thickness QT during ACL-R. As evidence continues to come out in favor of the use of QT [3, 19, 33, 35] and as the use of QT grows in popularity [36], it will become increasingly important to optimize the technique for performing ACL-R with QT, specifically with regard to the clinical question of whether to harvest a partial or full thickness autograft.
Thus, the purpose of this systematic review was to compare the outcomes and complication profiles after primary ACL-R with either full or partial thickness QT. It was hypothesized that, across all studies, full thickness grafts, when compared to partial thickness grafts, would be associated with improved clinical outcomes, including improved scores on patient-reported outcome (PRO) measures, decreased anterior laxity, and decreased incidence of graft failure, but increased rates of complications, including anterior kneeling pain.
Materials and methods
Search strategy
To search for clinical studies addressing the surgical procedures, outcomes and complications of primary ACL-R with QT, three databases (i.e., PubMed, Ovid (MEDLINE), and EMBASE) were searched as per PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines on September 1, 2017. The search was conducted using the terms “quadriceps tendon,” “anterior cruciate ligament reconstruction,” and “autograft.” This search was repeated on March 31, 2018 to capture any additional or newly published articles. Appendix Fig. 1 in Supplementary material lists the detailed strategy used for the search. The PRISMA statement was used for the reporting of study selection.
Study screening
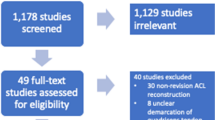
Two reviewers independently screened the titles, abstracts, and full-text articles in duplicate. The reviewers discussed all discrepancies to reach a consensus and a third senior reviewer was consulted as necessary when no consensus could be reached. The references of the included studies were subsequently searched by the reviewers to manually identify any articles that may have eluded the initial search (Fig. 1).
Assessment of study eligibility
The inclusion criteria were as follows: studies investigating primary anterior cruciate ligament reconstruction with quadriceps tendon autograft; English language studies; studies on humans of all ages; studies with reported clinical outcomes; and studies of all levels of evidence. Systematic reviews, conference abstracts, book chapters, and technical reports with no outcomes data were excluded.
Assessment of agreement
Inter-reviewer agreement for the title, abstract, and full-text articles was calculated with the kappa statistic (κ). The values were categorized a priori as follows: k of 0.81–0.99 was considered almost perfect agreement; k of 0.61–0.80, substantial agreement; k of 0.41–0.60, moderate agreement; k of 0.21–0.40, fair agreement; and k of 0.20 or less, slight agreement [29].
Quality assessment
The level of evidence of the included studies was assessed using the American Academy of Orthopaedic Surgeons classification system for the orthopaedic literature [43]. The MINORS (methodological index for non-randomized studies) checklist was used as well to assess the methodologic quality of the included studies.
Data extraction and analysis
Data were extracted from the included studies and recorded in a Microsoft Excel spreadsheet (version 2016; Microsoft, Redmond, WA). The recorded data included study characteristics as well as individual patient demographics, surgical techniques, and subjective/objective outcomes. If a paper stated in their methods section either that their graft thickness or diameter was 7 mm or greater or that the entire quadriceps tendon was harvested, it was classified as full thickness based on previous anatomic studies of the quadriceps tendon [38]. Alternatively, if the paper stated that their graft thickness or diameter was less than 7 mm or that part of the quadriceps tendon, such as the vastus intermedius, was left behind, then it was classified as partial thickness. If a study did not specifically report its graft thickness but stated, it used the technique of a previously published paper, that paper was reviewed, and the study of interest was classified based on the technique used in previously published paper. Because of limited and heterogeneous reporting, these data were not combined in a meta-analysis and were summarized descriptively. Descriptive statistics, including means, frequencies, standard deviations, and ranges, were calculated as appropriate for recorded data. All statistics were calculated by use of Minitab statistical software (version 17; Minitab, State College, PA).
Results
Search strategy
The initial search yielded a total of 3670 studies. After 2414 duplicates were removed, 1256 unique studies remained for assessment. Systematic screening of the titles, abstracts, and full-text articles was performed, resulting in 18 studies that met the inclusion criteria for evaluation in this review. An additional two studies were identified in the repeat search for a total of 20 studies (Fig. 1). There was substantial agreement between reviewers at the title (κ = 0.71) and almost perfect agreement between reviewers at the abstract (κ = 0.90) and full-text (κ = 0.97) screening stages.
Study quality
Twenty studies (50% case-control, 50% case series) satisfied all inclusion and exclusion criteria and were included in the final analysis [1, 2, 7,8,9, 15, 17, 18, 20, 21, 23,24,25,26,27,28,29, 33, 34, 40]. Only one of the included studies directly compared FT-Q to PT-Q [25]. The mean follow-up time was 42.2 months. The MINORS score for all studies are listed in Table 1.
Study characteristics
A total of 1212 patients (1219 knees) across 20 studies underwent primary ACL-R with a QT autograft. The mean age of patients was 29.8 years (range, 15–59). The average follow-up time was 42.2 months (range, 12–120). Table 2 shows a comparison of the patient characteristics of the pooled FT-Q and PT-Q cohorts. A detailed summary of the study characteristics is shown in Table 1. Concomitant injuries (significant articular cartilage erosion of more than grade II per the Outerbridge classification, concomitant posterior cruciate ligament reconstruction, posterolateral instability, medial collateral ligament injury, meniscal lesion that led to total meniscectomy) were reported in 11 studies. In three studies, such injuries were considered exclusion criteria [24, 25, 28].
Surgical management
Table 3 shows a detailed overview of the techniques used for each, including graft preparation, how graft thickness was determined, fixation technique, and drilling technique, i.e., transtibial versus anteromedial portal. The suprapatellar approach for graft harvesting was similar in all studies assessed. FT-Q autografts were used in eight studies (50.5% of knees), and PT-Q autografts were used in thirteen studies (49.5% of knees). In the one study that directly compared FT-Q and PT-Q autografts, double-bundle technique was used with FT-Q and single-bundle technique was used with PT-Q. Four studies used an isolated all-soft tissue tendon graft, and 16 used a tendon graft with an adjacent bone block. There were a variety of graft fixation methods used across studies, with most studies using interference screw fixation for both the tibial and femoral sides.
Outcomes
A detailed summary of the outcomes and complication profiles across all studies is shown in Table 4, and a comparison of a few selected outcomes between the FT-Q and PT-Q groups across all reported data is shown in Table 5. Instrumented laxity was noted to be less than 3 mm in 74.8% of the FT-Q group (four studies, 505 knees) and 72.8% of the PT-Q group (eight studies, 324 knees). Range of motion was restored within 5° of full extension for 95.1% of the FT-Q group (three studies, 308 knees) and 95.2% of the PT-Q group (four studies, 155 knees). Postoperative quadriceps strength, measured as a percentage of the contralateral side, was similar between both groups with reported means of 87.4 and 86.1% for FT-Q (two studies, 295 knees) and PT-Q (five studies, 333 knees), respectively.
Postoperative Lysholm scores were similar between both groups with means of 90.4 for FT-Q (four studies, 355 knees) and 91.0 for PT-Q (10 studies, 506 knees). Postoperative International Knee Documentation Committee Subjective Knee Form (IKDC-SKF) scores were also similar between groups with means of 82.5 for FT-Q (two studies, 78 knees) and 82.1 for PT-Q (four studies, 174 knees). Mean postoperative anterior knee pain was similar for FT-Q patients at rates of 5.2% (two studies, 227 knees) compared to PT-Q patients at 4.0% (five studies, 225 knees).
Complications
Only one study using FT-Q examined post-operative graft site numbness with a reported incidence of 1.0% (one study, 198 patients) [15]. Two cases of post-operative patellar fractures were reported for a total incidence of 0.7%; both occurred in cases using PT-Q (2 studies, 154 knees). Both were the result of mechanical falls: one case ultimately required osteosynthesis [17] and the other was treated nonoperatively [18, 28]. Both cases utilized a QT autograft with an adjacent bone block.
Standards for graft failure were different across studies, with some studies defining graft failure as an increase of 5 mm in the side-to-side difference in anterior laxity on instrumented testing [25] versus other studies which defined it as either arthroscopically confirmed graft rupture, positive pivot shift postoperatively, or an increased side-to-side difference in anterior laxity of greater than 5 mm on instrumented testing [15]. Using a broad definition of graft failure including graft rupture as well as symptomatic instability or increased anterior laxity, the overall rate of graft failure was 3.7% in FT-Q (three studies, 476 knees) and 3.0% in PT-Q (four studies, 230 knees), and 3.5% across all studies (seven studies, 706 knees).
Discussion
The most important finding of the present study was that there appears to be no difference in clinical outcomes or complication rates between either FT-Q or PT-Q autografts in primary ACL-R, thus disproving the hypothesis under study. There were no major differences in postoperative Lysholm or IKDC-SKF scores, range of motion, quadriceps strength, instrumented laxity, anterior knee pain, or incidence of graft failure between both graft types, although only one study directly compared FT-Q versus PT-Q. Moreover, based on the studies presented here, ACL-R with either FT-Q or PT-Q appears to have successful short-term outcomes. While statistical significance could not be assessed, it is worth noting that many of the differences, such as the differences in the Lysholm score and IKDC-SKF which were both less than 1 point, are well below the minimum detectable change (MDC) (IKDC-SKF, 8.8–16.4; Lysholm, 10.1) [4, 22] and, thus, highly unlikely to be of statistical or clinical significance. This finding is important for clinical practice as it suggests that either FT-Q or PT-Q are viable graft choices during ACL-R. Moreover, if FT-Q and PT-Q are equally efficacious in ACL-R, surgeons may choose to utilize the PT-Q given the inherent, albeit low, risks of FT-Q harvesting, such as violation of the joint capsule. Such complications were not reported in any studies and may be under-estimated or under-reported. While heterogenous reporting precluded combining data in a meta-analysis, this review nonetheless includes data from over 1200 patients. Moreover, demographics between the FT-Q and PT-Q cohorts were similar with respect to age, sex, and follow-up time, thus allowing for a valid comparison between the two cohorts.
Previous studies have yielded mixed findings regarding the relationship between graft size and outcomes. Multiple previous studies have found no statistically significant differences in re-rupture rate, clinical outcomes or biomechanical characteristics between 4- and 5-strand hamstring grafts for ACL-R [5, 6]. Another recent study analyzing the association between graft rupture rate and dichotomized graft size in HS and BPTB autografts reported that increasing autograft diameter did not lead to a reduction in revision ACL-R surgery [42]. However, another recent study found that an increase in the graft diameter between 7.0 and 10.0 mm resulted in a 0.86 times lower likelihood of revision surgery with every 0.5-mm increase [37]. Previous studies of ACL-R with HS autografts have found that increased graft size does correlate with reduced rates of graft failure requiring revision surgery, and that graft diameter less than 8 mm is specifically correlated with an increase revision rate [10, 30, 31, 39]. This disparity between studies may be explained by the notion that that the collagen content of a graft, rather than its diameter, may be the more important parameter [12]. As well, graft orientation, tension for fixation, and extremity position for fixation are but few of the multiple technical factors apart from graft thickness that can affect surgical outcomes. Given that certain graft preparation techniques have been shown to reduce graft diameter [12] without necessarily changing their collagen content, many of the above-mentioned studies may be confounded by differences in graft preparation techniques. Ultimately, larger, multi-center comparative studies or randomized controlled trials will be valuable in further investigating the role of graft thickness in ACL-R with QT autografts.
The graft failure across all patients in this study was 3.5%. However, the reporting of complications was limited across studies, exemplified by the fact that only 9 of 20 studies reported on the incidence of graft failure. Across available clinical data though, the overall failure rate is low in comparison to other common autograft sources. While mechanisms of graft failure were not uniformly reported, at least seven out of the 25 cases of graft failure (28%) were attributable to traumatic mechanisms. This rate compares favorably to a previous systematic review of 14 studies and 1532 patients with a minimum 10-year follow-up which found an ACL graft failure rate, including both graft rupture or increased anterior laxity, of 10.3% [11]. Given that the mean follow-up time in the present study was only 3.5 years, however, future long-term studies will be needed to better characterize the incidence of graft failure with QT autograft, in order to delineate any meaningful clinical differences FT-Q and PT-Q.
This study, which has a number of strengths including reporting several objective and PRO measures from a pooled cohort of 1212 patients and 20 studies, has numerous implications for clinical practice. Given that there appears to be no difference in the clinical outcome and complication profiles of FT-Q and PT-Q, surgeons may be justified in using either graft type based on their preference or experience with harvesting a particular graft type. Given the growing body of evidence supporting QT autografts over other autograft options [3, 14, 19, 33] as well as the growing popularity of QT autografts [36], these findings are particularly important as they may help reaffirm to clinicians that there is evidence to support primary ACL-R using QT, both full and partial thickness.
This review was limited by the quantity and quality of studies available on primary ACL-R with FT-Q or PT-Q autograft. Many of the included studies had significant methodologic flaws such as a low sample size, retrospective evaluation of data, limited reporting of technique such as the tools used to measure graft thickness, and lack of a control group for comparison. Only one of the included studies directly compared FT-Q to PT-Q. There was fairly significant heterogeneity in the included studies regarding graft preparation, graft fixation technique, and the reporting of outcomes and complications. Apart from functional scores, more data are needed to evaluate time to return to sport at preinjury level.
Conclusions
Across the 20 studies included in this review, there appeared to be no difference in outcomes or complications between either FT-Q or PT-Q in primary ACL-R. Moreover, primary ACL-R using QT autografts appear to have successful outcomes with a low rate of graft failure, irrespective of tendon thickness. While larger, multi-center comparative studies are needed to better delineate the optimal thickness of quadriceps tendon for primary ACL-R, these data suggest that, in primary ACL-R, either FT-Q or PT-Q is efficacious, and surgeons may be justified in using either graft thickness.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACL-R:
-
Anterior cruciate ligament reconstruction
- BPTB:
-
Bone-patellar tendon-bone
- FT-Q:
-
Full thickness quadriceps tendon autograft
- PT-Q:
-
Partial thickness quadriceps tendon autograft
- HS:
-
Hamstring
- QT:
-
Quadriceps tendon
References
Akoto R, Hoeher J (2012) Anterior cruciate ligament (ACL) reconstruction with quadriceps tendon autograft and press-fit fixation using an anteromedial portal technique. BMC Musculoskelet Disord 13:161
Akoto R, Muller-Hubenthal J, Balke M, Albers M, Bouillon B, Helm P, Banerjee M, Hoher J (2015) Press-fit fixation using autologous bone in the tibial canal causes less enlargement of bone tunnel diameter in ACL reconstruction—a CT scan analysis three months postoperatively. BMC Musculoskelet Disord 16:200
Belk JW, Kraeutler MJ, Marshall HA, Goodrich JA, McCarty EC (2018) Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction: a systematic review of comparative studies with minimum 2-year follow-Up. Arthroscopy 34:1699–1707
Briggs KK, Kocher MS, Rodkey WG, Steadman JR (2006) Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Joint Surg Am 88:698–705
Broadhead ML, Singla AA, Bertollo N, Broe D, Walsh WR (2017) A Biomechanical comparison of 4-strand and 5-strand anterior cruciate ligament graft constructs. Orthop Rev (Pavia) 9:6989
Calvo R, Figueroa D, Figueroa F, Vaisman A, Schmidt-Hebbel A, Morales N, Izquierdo G (2017) Five-strand hamstring autograft versus quadruple hamstring autograft with graft diameters 8.0 millimeters or more in anterior cruciate ligament reconstruction: clinical outcomes with a minimum 2-year follow-up. Arthroscopy 33:1007–1013
Cavaignac E, Coulin B, Tscholl P, Nik Mohd Fatmy N, Duthon V, Menetrey J (2017) Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am J Sports Med 45:1326–1332
Chen C-H, Chen W-J, Shih C-H (1999) Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. J Trauma Acute Care Surg 46:678–682
Chen CH, Chuang TY, Wang KC, Chen WJ, Shih CH (2006) Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon autograft: clinical outcome in 4–7 years. Knee Surg Sports Traumatol Arthrosc 14:1077–1085
Conte EJ, Hyatt AE, Gatt CJ, Dhawan A (2014) Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy 30:882–890
Crawford SN, Waterman BR, Lubowitz JH (2013) Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy 29:1566–1571
Cruz AI Jr, Fabricant PD, Seeley MA, Ganley TJ, Lawrence JTR (2016) Change in size of hamstring grafts during preparation for ACL reconstruction: effect of tension and circumferential compression on graft diameter. J Bone Jt Surg Am 98:484–489
DeAngelis JP, Fulkerson JP (2007) Quadriceps tendon—a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med 26:587–596
Fischer F, Fink C, Herbst E, Hoser C, Hepperger C, Blank C, Gföller P (2018) Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 26:418–425
Geib TM, Shelton WR, Phelps RA, Clark L (2009) Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy 25:1408–1414
Gorschewsky O, Klakow A, Putz A, Mahn H, Neumann W (2007) Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 15:1284–1292
Guimarães MV, Junior LHdC, Terra DL (2009) Reconstruction of the anterior cruciate ligament with the central third of the quadriceps muscle tendon: analysis of 10-year results. Rev Bras Ortop 44:306–312
Han HS, Seong SC, Lee S, Lee MC (2008) Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Clin Orthop Relat Res 466:198–204
Hurley ET, Calvo-Gurry M, Withers D, Farrington SK, Moran R, Moran CJ (2018) Quadriceps tendon autograft in anterior cruciate ligament reconstruction: a systematic review. Arthroscopy 34:1690–1698
Iriuchishima T, Ryu K, Okano T, Suruga M, Aizawa S, Fu FH (2017) The evaluation of muscle recovery after anatomical single-bundle ACL reconstruction using a quadriceps autograft. Knee Surg Sports Traumatol Arthrosc 25:1449–1453
Joseph M, Fulkerson J, Nissen C, Sheehan TJ (2006) Short-term recovery after anterior cruciate ligament reconstruction: a prospective comparison of three autografts. Orthopedics 29:243–248
Kanakamedala AC, Anderson AF, Irrgang JJ (2016) IKDC subjective knee form and Marx Activity Rating Scale are suitable to evaluate all orthopaedic sports medicine knee conditions: a systematic review. J ISAKOS 1:25–31
Kim S-J, Kumar P, Oh K-S (2009) Anterior cruciate ligament reconstruction: autogenous quadriceps tendon–bone compared with bone–patellar tendon–bone grafts at 2-year follow-up. Arthroscopy 25:137–144
Kim SJ, Chang JH, Kim TW, Jo SB, Oh KS (2009) Anterior cruciate ligament reconstruction with use of a single or double-bundle technique in patients with generalized ligamentous laxity. J Bone Jt Surg Am 91:257–262
Kim SJ, Jo SB, Kumar P, Oh KS (2009) Comparison of single- and double-bundle anterior cruciate ligament reconstruction using quadriceps tendon-bone autografts. Arthroscopy 25:70–77
Kwak Y-H, Lee S, Lee MC, Han H-S (2018) Anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone allograft: matched case control study. BMC Musculoskelet Disord 19:45
Lee JK, Lee S, Lee MC (2016) Outcomes of anatomic anterior cruciate ligament reconstruction: bone-quadriceps tendon graft versus double-bundle hamstring tendon graft. Am J Sports Med 44:2323–2329
Lee S, Seong SC, Jo CH, Han HS, An JH, Lee MC (2007) Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. J Bone Joint Surg Am 89(Suppl 3):116–126
Lee S, Seong SC, Jo H, Park YK, Lee MC (2004) Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy 20:795–802
Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE (2012) Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 28:526–531
Mariscalco MW, Flanigan DC, Mitchell J, Pedroza AD, Jones MH, Andrish JT, Parker RD, Kaeding CC, Magnussen RA (2013) The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a multicenter orthopaedic outcomes network (MOON) cohort study. Arthroscopy 29:1948–1953
Mulford JS, Hutchinson SE, Hang JR (2013) Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc 21:1882–1888
Runer A, Wierer G, Herbst E, Hepperger C, Herbort M, Gföller P, Hoser C, Fink C (2018) There is no difference between quadriceps-and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee Surg Sports Traumatol Arthrosc 26:605–614
Schulz AP, Lange V, Gille J, Voigt C, Fröhlich S, Stuhr M, Jürgens C (2013) Anterior cruciate ligament reconstruction using bone plug-free quadriceps tendon autograft: intermediate-term clinical outcome after 24–36 months. Open Access J Sports Med 4:243
Sheean AJ, Musahl V, Slone HS, Xerogeanes JW, Milinkovic D, Fink C, Hoser C (2018) Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: use it now, use it often. Br J Sports Med 52:698–701
Slone HS, Romine SE, Premkumar A, Xerogeanes JW (2015) Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy 31:541–554
Snaebjornsson T, Hamrin Senorski E, Ayeni OR, Alentorn-Geli E, Krupic F, Norberg F, Karlsson J, Samuelsson K (2017) Graft diameter as a predictor for revision anterior cruciate ligament reconstruction and KOOS and EQ-5D values: a cohort study from the swedish national knee ligament register based on 2240 patients. Am J Sports Med 45:2092–2097
Staeubli H-U, Bollmann C, Kreutz R, Becker W, Rauschning W (1999) Quantification of intact quadriceps tendon, quadriceps tendon insertion, and suprapatellar fat pad: MR arthrography, anatomy, and cryosections in the sagittal plane. AJR. Am J Roentgenol 173:691–698
Steiner M (2017) Editorial commentary: size does matter—anterior cruciate ligament graft diameter affects biomechanical and clinical outcomes. Arthroscopy 33:1014–1015
Theut PC, Fulkerson JP, Armour E, Joseph M (2003) Anterior cruciate ligament reconstruction utilizing central quadriceps free tendon. Orthop Clin North Am 34:31–39
van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH (2010) “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 26:S2–S12
Wernecke GC, Constantinidis A, Harris IA, Seeto BG, Chen DB, MacDessi SJ (2017) The diameter of single bundle, hamstring autograft does not significantly influence revision rate or clinical outcomes after anterior cruciate ligament reconstruction. Knee 24:1033–1038
Wright J (2005) Levels of evidence and grades of recommendations. AAOS Bulletin. http://www2.aaos.org/bulletin/apr05/fline9.asp. Accessed 15 Sept 2017
Xerogeanes JW, Mitchell PM, Karasev PA, Kolesov IA, Romine SE (2013) Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med 41:2392–2399
Funding
There was no external source of funding for this study.
Author information
Authors and Affiliations
Contributions
ACK, OAO performed the screening of all titles, abstracts, and full-texts. MEA and ACK performed the abstraction of all data. PBS and ACK drafted the original manuscript. DdS, ACK, BPL, and VM participated in the editing of the original manuscript. DdS, ACK, BPL, and VM participated in the conception and design of the original study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study confirm that they have no conflicts of interest related to this study.
Ethical approval
No IRB approval was required or obtained for this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
167_2018_5042_MOESM1_ESM.tiff
Appendix Figure 1: Detailed Flow Diagram of Search Strategy—Detailed description of search strategy for systematic literature review and screening process (TIFF 3954 KB)
Rights and permissions
About this article
Cite this article
Kanakamedala, A.C., de SA, D., Obioha, O.A. et al. No difference between full thickness and partial thickness quadriceps tendon autografts in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 27, 105–116 (2019). https://doi.org/10.1007/s00167-018-5042-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5042-z