Abstract
Purpose
The aim of this study was to compare the intraoperative kinematics of medial and lateral unicompartmental knee arthroplasty (UKA) with those of the native knee using a navigation system.
Methods
Six fresh-frozen cadaveric knees were included in the study. Medial UKA was performed in all right knees and lateral UKA was performed in all left knees. All UKA procedures were performed with a computerised navigation system. The tibial internal rotation angle and coronal alignment of the mechanical axis during passive knee flexion were assessed as rotational and varus/valgus kinematics before and after surgery using the navigation system.
Results
The rotation angles of the tibia in the early flexion phase of medial UKA were significantly larger than those of native knees (p = 0.008 at minimum knee flexion, p = 0.008 at 0° knee flexion). The rotational kinematics of lateral UKA was similar to those of the native knees throughout knee flexion. There were no significant differences in varus/valgus kinematics between native and UKA knees.
Conclusion
The rotational kinematics of the native knee was not restored after medial UKA but was preserved after lateral UKA. There were no significant differences in the varus/valgus kinematics after either medial or lateral UKA when compared with those of the native knees. Thus, the geometry of the medial tibial articular surface is a determinant of the ability to restore the rotational kinematics of the native knee. Surgeons and implant designers should be aware that the anatomical medial articular geometry is an important factor in restoration of the native knee kinematics after knee arthroplasty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) is a surgical alternative for patients with osteoarthritis and osteonecrosis in only one compartment of the knee [22]. Recent studies have reported that the long-term survival of UKA is similar to that of total knee arthroplasty (TKA) [5, 11, 17, 20]. There are also several reports of better functional outcomes after UKA than after TKA [2, 7, 9, 16, 28]. In particular, a recent report suggested that patients who undergo UKA are more likely to forget that they have an artificial joint in daily life than patients who undergo TKA [30]. This could be partly explained by the closer similarity in kinematics between the native knee and UKA, compared with TKA, because UKA enables preservation of the knee ligaments. In other words, this preservation might be a key factor in restoring the kinematics of the native knee after UKA. However, this remains controversial [14, 19, 23], and there have been a few reports on the kinematics of lateral UKA. A kinematic study of medial and lateral UKA would provide important information to address this controversy.
In addition, from another perspective, tibial surface geometry is reported to have considerable impact on rotational knee kinematics [25, 31]. Therefore, the hypothesis tested in this study was that the kinematics would be affected by isolated replacement of either the medial or lateral articular surface by UKA. To test this, a navigation system was used to compare the kinematics of the native knee with the kinematics of medial and lateral UKA knees in the same whole-body cadaveric specimen.
Materials and methods
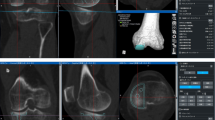
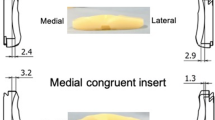
Six fresh-frozen cadavers stored at − 20 °C (2 males, 4 females; mean age at time of dissection 88.8 years, range 79–100 years) were obtained for this study. All the cadaveric specimens were macroscopically intact without gross deformity, arthritic change, contracture, or evidence of prior surgery. Preoperative computed tomography confirmed that none had osteoarthritis. The trial component was a flat-surfaced, fixed-bearing cemented UKA prosthesis (Tribrid, Kyocera Medical, Osaka, Japan) that was implanted in each specimen using an image-free knee navigation system (Stryker Navigation version 1.0, Stryker, Kalamazoo, MI, USA), infrared cameras, and light-emitting diodes. Medial UKA was performed in the right knee and lateral UKA in the left knee of each specimen.
Surgical procedure and evaluation of intraoperative kinematics
Each surgery was performed using the standard medial parapatellar approach. Soft-tissue release was not performed except for portions that required osteotomy. The anterior and posterior cruciate ligaments were preserved. Registration of the navigation system was performed for each case following the manufacturer’s protocol. After registration, the kinematics of the native knee was evaluated with intraoperative kinematic analysis.
Next, the proximal tibia was resected perpendicular to the mechanical axis on the coronal plane using an extramedullary rod with the navigation system. Tibial rotational alignment was directed along a line from the medial border of the tibial tubercle to the middle of the posterior cruciate ligament [1]. On the sagittal plane, the posterior tibial slope were set as 5° with the navigation system. The amount of bone resection was set to the component thickness. Following the manufacturer’s protocol, the distal femur was resected to create a total component thickness gap both at full knee extension and 90° of knee flexion using a spacer block. The patella was not resurfaced. A 9-mm polyethylene insert was used in all knees. After the trial component was assembled, intraoperative kinematic analysis was performed to evaluate the knee kinematics after UKA.
During evaluation of the intraoperative kinematics, the dissected fascia was sutured with nylon thread. For each knee, kinematic analysis was performed once by the same examiner using the navigation system. The knee was flexed by placing the specimen’s heel in the examiner’s open palm to allow for freedom of tibial rotation, while the examiner’s other hand was placed beside the specimen’s knee for support. Care was taken to avoid intentional rotation of the knee throughout flexion. The navigation system automatically recorded the rotation angle of the tibia (internal rotation as positive) as rotational kinematics and the coronal alignment of the lower limb (valgus alignment as positive) as varus/valgus kinematics at minimum flexion, at 10° intervals from 0° to 130° flexion, and at maximum flexion during passive knee motion. The data for both the rotation angle of the tibia and the coronal alignment of the lower limb were collected by the navigation system with a measurement accuracy of 0.5°. Therefore, the results are reported to one decimal place. An earlier study demonstrated that the repeatability and reproducibility of this methodology was statistically sufficient [26].
The institutional review board approved this prospective study (no. 2068-1). All procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Statistical analysis
The Mann–Whitney U test was used to evaluate differences in the rotation angle of the tibia and the coronal alignment of the lower limb at each knee flexion angle between the native knee and the UKA knee. All statistical analyses were performed using IBM SPSS statistical software (SPSS v.21.0 for Mac OS X; IBM Corp., Armonk, NY, USA). For all analyses, a p value < 0.05 was considered statistically significant. The results are presented as the median and range. Given the small number of subjects, a post hoc calculation of effect size (Cohen’s d) and statistical power was performed with G*power statistical software (version 3.1.9.2, Dusseldorf, Germany) [10]. The effect sizes were defined as small (d > 0.2), medium (d > 0.5), or large (d > 0.8), as described by Cohen’s d criteria [8, 18]. A sample size calculation based on the calculated effect size demonstrated that six specimens would be sufficient to detect statistically significant kinematic differences with a power of 0.8. The probability of type I error associated with this test is 0.05.
Results
Figures 1, 2 show the axial rotation angle of the tibia at each angle of knee flexion for the native and UKA knees. For medial UKA (Fig. 1), both native and medial UKA knees showed continuous tibial internal rotation during knee flexion. In contrast, medial UKA knees showed significantly larger tibial internal rotation angles during the early flexion phase (p = 0.008; effect size = 2.4 at minimum knee flexion, p = 0.008; effect size = 2.7 at 0° knee flexion) than native knees (with a statistical power of 0.9 at minimum knee flexion and 0.9 at 0° knee flexion). For lateral UKA (Fig. 2), both native and lateral UKA knees showed tibial internal rotation during knee flexion, including transient tibial external rotation at mid-flexion. Interestingly, the rotational kinematics were similar between the lateral UKA and native knees throughout passive knee flexion.
Figures 3, 4 show the coronal angle of the mechanical axis at each angle of knee flexion in native and UKA knees. The varus/valgus kinematics were similar between the lateral UKA and native knee throughout knee flexion (Fig. 4). In contrast, some kinematics differed between the medial UKA knees and the native knee as the flexion angle increased (Fig. 3), but the differences were not statistically significant.
Discussion
The most important finding in this study was that the internal rotation angles of the tibia in the early flexion phase of medial UKA were significantly larger than those of the native knee. The results indicate that the rotational kinematics of the native knee was not restored after medial UKA but was preserved after lateral UKA. There were no significant differences in varus/valgus kinematics before or after medial or lateral UKA. To the authors’ knowledge, this study is the first to evaluate the intraoperative kinematics of both medial and lateral UKA in the same whole-body cadaveric specimen.
The classic “screw-home” mechanism was reported as a sharp internal rotation near extension [12], and other studies have shown that the screw-home mechanism is coupled to internal tibial rotation as the femur flexes and to external tibial rotation as it extends [6, 27]. The proximal tibia normally rotates externally on the distal femur by about 15° during the final 20° of extension, with the screw-home mechanism serving to lock the knee in extension and limit anterolateral rotatory movement [4, 15, 29]. In the present study, the internal rotation angles of the tibia in the early flexion phase of medial UKA were significantly larger than those of the native knee, indicating that the screw-home mechanism of the native knee was not restored after medial UKA but was preserved after lateral UKA.
Whether UKA can restore the kinematics of the native knee has been the subject of some controversy. Patil et al. [23] studied six cadaveric human knees using a kinematic rig before and after medial UKA and reported no significant difference in axial tibial rotation between the native knee and the flat-surfaced, fixed-bearing UKA knee. However, they found that the tibia rotated internally during knee extension in both native and UKA knees. From the viewpoint of the screw-home mechanism, that finding indicates that the native knee kinematics was not preserved after UKA. Argenson et al. [3] evaluated the in vivo kinematics of 20 UKA knees and reported that 12 of 17 subjects who underwent medial UKA maintained normal axial rotation. Nevertheless, their results for the average axial rotation pattern suggested less than 3° of axial rotation angle in the early flexion phase. Although they did not evaluate the native knee, their finding that the angle of rotation was small is similar to the results for medial UKA in the present study. Thus, it seems that the screw-home mechanism of the native knee is not maintained after UKA. Heyse et al. [14] compared the difference between the native knee kinematics and the kinematics after medial flat-surfaced, fixed-bearing UKA using a kinematic rig in six cadaveric knees and concluded that the native knee kinematics was restored after medial UKA. However, they also reported that the internal rotation angle of the tibia after UKA tended to be larger than that of the native knee, especially in the early phase of knee flexion. That finding indicates that the screw-home mechanism of the native knee might not be preserved after UKA. In contrast with these reports, Mochizuki et al. [19] reported that the pattern of motion of 17 osteoarthritic knees before medial UKA was similar to that afterwards, but that both motion patterns were markedly different from those of the native knee. Their results are similar to the results of the present study in that the size of the angle of axial rotation near extension decreases after UKA to a greater extent than that found in the native knee, indicating that the screw-home mechanism was lost. These findings suggest that medial UKA influences the rotational kinematics of the native knee, especially in the early flexion phase.
The screw-home mechanism has been attributed to the function of the anterior cruciate ligament and asymmetry between the medial and lateral femoral condyles. However, in the present study, the mechanism was not restored after medial UKA despite preservation of the anterior cruciate ligament, but was restored after lateral UKA. Rajendran et al. [24] suggested that the workings of the screw-home mechanism involved the medial femoral condyle slipping or sliding against the upslope of the tibia as the knee extends, while the lateral femoral condyle suffers little or no interference as a result of flattening of the downward sloping anterior part of the lateral tibial condyle. The findings presented here indicate that changes in the articular surface geometry of the tibia in the medial compartment of the knee have a more significant impact on the screw-home mechanism than changes in the lateral compartment. In terms of the articular surface, the loss of the upslope of the tibia when a flat-surfaced, fixed-bearing type of UKA prosthesis was applied caused the changes in rotational kinematics after medial UKA, especially in the early flexion phase.
Several previous reports have suggested that tibial surface geometry has a considerable impact on the rotational kinematics of the knee. Using a knee simulator, Varadarajan et al. [25] demonstrated that a biomimetic implant with an anatomic articular geometry was able to mimic the activity-dependent kinematics of the normal knee more closely than contemporary implants in cruciate-retaining TKA. A recent dynamic computer simulation study by Zumbrunn et al. [31] demonstrated that a bicruciate-retaining TKA implant designed with biomimetic inserts mimicking the native tibial surface geometry achieved more marked kinematic improvement than cruciate-retaining TKA, contemporary bicruciate TKA, or bi-UKA. A recent cadaveric study by Hamada et al. [13] showed that the normal rotational kinematics are lost after tibial replacement in bicruciate-retaining TKA, and suggested that the surface geometry of the polyethylene insert is an important factor in the restoration of normal rotational kinematics. The present study also confirms the importance of preserving native geometry for restoration of the kinematics of the native knee when using a navigation system. Specifically, the present results show that preservation of the native geometry of the medial compartment is more important than preservation of that of the lateral compartment. This important finding suggests that the articular surface in knee arthroplasty should be considered further. However, approximating the tibial insert geometry to the native joint surface in UKA leads to increased strain. Therefore, further study is needed to evaluate the stress of the tibial component in the clinical setting.
This study had several limitations. First, it assessed only the internal rotation angle of the tibia and the coronal alignment of the mechanical axis during flexion. There is a lack of kinematic data for the anteroposterior, mediolateral, and superoinferior dimensions, because the knee kinematics had six degrees of freedom. Specifically, anterior–posterior translation should be examined to evaluate the kinematics of knee flexion; unfortunately, this could not be done with the navigation system used in this study. Second, tibial internal rotation was not assessed under weight-bearing conditions. Many previous studies have suffered from the same limitation of evaluating non-weight-bearing kinematics intraoperatively. However, a recent study reported that external femoral rotation with a medial pivot motion intraoperatively was associated with a deep knee flexion angle postoperatively [21]. Therefore, even in a non-weight-bearing situation, internal tibial rotation is an important parameter in terms of postoperative knee flexion. Although this study was performed using whole-body cadaveric specimens, the conditions were similar to those in clinical studies of patients under anaesthesia. Third, the reproducibility of the kinematic analysis was not evaluated; this may be problematic, because the analysis was performed manually. Nevertheless, a previous study found that intraoperative kinematic analysis had high reproducibility [26]. Therefore, the present data, which were obtained using the same method, are believed to have adequate reproducibility. Fourth, both the rotational and varus/valgus kinematics of native knees differed between the right and left knees. A possible cause of this phenomenon is a registration setting error. In this study’s methodology, manually registered transepicondylar and tibial axes were used to evaluate rotational kinematics and manually registered mechanical axes were used to evaluate varus/valgus kinematics. Therefore, the kinematics of medial and lateral UKA could not be compared directly. Thus, in the present study, the kinematics of the native knee were compared separately with the kinematics of the medial UKA knee and the lateral UKA knee. Finally, the sample size was small, because access to cadaveric specimens is limited and specimens with osteoarthritis were excluded. However, although only post hoc power analyses were performed, items with significant differences had adequate statistical power. Despite these limitations, the data generated in this study highlight the need to consider the articular surface to further improve the performance of UKA. These data also suggest that restoring the articular surface geometry leads to restoration of the kinematics of the native knee, not only in UKA but also in TKA.
Conclusion
The rotational kinematics of the native knee were not restored after medial UKA but were preserved after lateral UKA. There were no significant differences in the varus/valgus kinematics after either medial or lateral UKA when compared with those of the native knee. Thus, the geometry of the medial tibial articular surface is a determinant of the ability to restore the rotational kinematics of the native knee. Surgeons and implant designers should be aware that the anatomical medial articular geometry is an important factor in restoration of the native knee kinematics after knee arthroplasty.
Abbreviations
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicompartmental arthroplasty
References
Akagi M, Mori S, Nishimura S et al (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176
Argenson JN, Blanc G, Aubaniac JM et al (2013) Modern unicompartmental knee arthroplasty with cement. J Bone Jt Surg Am 95:905–909
Argenson JN, Komistek RD, Aubaniac JM et al (2002) In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplast 17:1049–1054
Asano T, Akagi M, Nakamura T (2005) The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplast 20:1060–1067
Berger RA, Meneghini RM, Jacobs JJ et al (2005) Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Jt Surg Am 87:999–1006
Blankevoort L, Huiskes R, de Lange A (1988) The envelope of passive knee joint motion. J Biomech 21:705–720
Burn E, Sanchez-Santos MT, Pandit HG et al (2016) Ten-year patient-reported outcomes following total and minimally invasive unicompartmental knee arthroplasty: a propensity score-matched cohort analysis. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-016-4404-7
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Hillsdale
Fabre-Aubrespy M, Ollivier M, Pesenti S et al (2016) Unicompartmental knee arthroplasty in patients older than 75 results in better clinical outcomes and similar survivorship compared to total knee arthroplasty. A matched controlled study. J Arthroplast 31:2668–2671
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Foran JRH, Brown NM, Della Valle CJ et al (2013) Long-term survivorship and failure modes of unicompartmental knee arthroplasty knee. Clin Orthop Relat Res 471:102–108
Hallén LG, Lindahl O (1966) The “screw-home” movement in the knee-joint. Acta Orthop Scand 37:97–106
Hamada D, Wada K, Takasago T et al (2018) Native rotational knee kinematics are lost in bicruciate-retaining total knee arthroplasty when the tibial component is replaced. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4842-5
Heyse TJ, El-Zayat BF, De Corte R et al (2014) UKA closely preserves natural knee kinematics in vitro. Knee Surg Sport Traumatol Arthrosc 22:1902–1910
Ishii Y, Terajima K, Terashima S et al (1997) Three-dimensional kinematics of the human knee with intracortical pin fixation. Clin Orthop Relat Res 343:144–150
Lim JW, Cousins GR, Clift BA et al (2014) Oxford unicompartmental knee arthroplasty versus age and gender matched total knee arthroplasty—functional outcome and survivorship analysis. J Arthroplast 29:1779–1783
Lisowski LA, Meijer LI, van den Bekerom MPJ et al (2016) Ten- to 15-year results of the Oxford Phase III mobile unicompartmental knee arthroplasty: a prospective study from a non-designer group. Bone Jt J 98-B:41–47
Maher JM, Markey JC, Ebert-May D (2013) The other half of the story: effect size analysis in quantitative research. CBE Life Sci Educ 12:345–351
Mochizuki T, Sato T, Blaha JD et al (2014) Kinematics of the knee after unicompartmental arthroplasty is not the same as normal and is similar to the kinematics of the knee with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 22:1911–1917
Naudie D, Guerin J, Parker DA et al (2004) Medial unicompartmental knee arthroplasty with the Miller-Galante prosthesis. J Bone Jt Surg Am 86-A:1931–1935
Nishio Y, Onodera T, Kasahara Y et al (2014) Intraoperative medial pivot affects deep knee flexion angle and patient-reported outcomes after total knee arthroplasty. J Arthroplast 29:702–706
Nwachukwu BU, McCormick FM, Schairer WW et al (2014) Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. J Arthroplast 29:1586–1589
Patil S, Colwell CW, Ezzet KA et al (2005) Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Jt Surg Am 87:332–338
Rajendran K (1985) Mechanism of locking at the knee joint. J Anat 143:189–194
Varadarajan KM, Zumbrunn T, Rubash HE et al (2015) Cruciate retaining implant with biomimetic articular surface to reproduce activity dependent kinematics of the normal knee. J Arthroplast 30:2149–2153
Wada K, Mikami H, Hamada D et al (2016) Measurement of rotational and coronal alignment in total knee arthroplasty using a navigation system is reproducible. Arch Orthop Trauma Surg 136:271–276
Wilson DR, Feikes JD, Zavatsky AB et al (2000) The components of passive knee movement are coupled to flexion angle. J Biomech 33:465–473
Wong T, Wang CJ, Wang JW et al (2014) Functional outcomes of uni-knee arthroplasty for medial compartment knee arthropathy in Asian patients. Biomed J 37:406
Wretenberg P, Ramsey DK, Németh G (2002) Tibiofemoral contact points relative to flexion angle measured with MRI. Clin Biomech (Bristol Avon) 17:477–485
Zuiderbaan HA, van der List JP, Khamaisy S et al (2017) Unicompartmental knee arthroplasty versus total knee arthroplasty: which type of artificial joint do patients forget? Knee Surg Sport Traumatol Arthrosc 25:681–686
Zumbrunn T, Varadarajan KM, Rubash HE et al (2015) Regaining native knee kinematics following joint arthroplasty: a novel biomimetic design with ACL and PCL preservation. J Arthroplast 30:2143–2148
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
KW carried out the kinematic measurements, performed the statistical analysis, and drafted the manuscript. DH participated in the design of the study and performed the UKA surgery. TT and AN assisted with the UKA surgery. IT and YT helped to coordinate the study. TG and KS helped to draft the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All performed procedures were approved by the institutional review board of Tokushima University Hospital (the ID number of approval was 2068-1) and done in accordance with the 1964 Declaration of Helsinki and its later amendments for comparable ethical standards.
Rights and permissions
About this article
Cite this article
Wada, K., Hamada, D., Takasago, T. et al. Native rotational knee kinematics is restored after lateral UKA but not after medial UKA. Knee Surg Sports Traumatol Arthrosc 26, 3438–3443 (2018). https://doi.org/10.1007/s00167-018-4919-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4919-1