Abstract
Purpose
(1) To determine the overall accuracy of synovial alpha-defensin, synovial C-reactive protein (sCRP), interleukin-6 (sIL-6), and leukocyte esterase (sLE) as diagnostic markers for periprosthetic joint infection (PJI) and (2) to independantly evaluate the accuracy of both the laboratory-based ELISA alpha-defensin test and the Synovasure™ alpha-defensin test kit.
Methods
An EMBASE and MEDLINE (PubMed) database search was performed using a set of professionally set search terms. Two independent reviewers rated eligible articles. Sensitivity and specificity were meta-analysed using a bivariate random-effects model.
Results
Accuracy values were extracted from 42 articles. Pooled sensitivity and specificity of the represented biomarkers were: alpha-defensin ELISA 0.97 (95% CI 0.91–0.99) and 0.97 (95% CI 0.94–0.98), respectively; Synovasure™ test kit assay 0.80 (95% CI 0.65–0.89) and 0.89 (95% CI 0.76–0.96), respectively; sLE 0.79 (95% CI 0.67–0.87) and 0.92 (95% CI 0.87–0.92), respectively; sIL-6 0.76 (95% CI 0.65–0.84) and 0.91 (95% CI 0.88–0.94), respectively; sCRP 0.86 (95% CI 0.81–0.91) and 0.90 (95% CI 0.86–0.93), respectively.
Conclusion
The labararory-based alpha-defensin ELISA test showed the highest ever reported accuracy for PJI diagnosis. However, this did not apply for the Synovasure™ alpha-defensin test, which was comparable in its overall diagnostic accuracy to sCRP, sIL-6 and sLE. The later biomarkers also did not yield an overall diagnostic accuracy higher than that previously reported for synovial white cell count (sWBC) or culture bacteriology. Based on current evidence, no synovial biomarker should be applied as a standalone diagnostic tool. Furthermore, the use of the laboratory-based alpha-defensin ELISA test should be encouraged, still, the Synovasure™ alpha-defensin test kit should be critically appreciated.
Lever of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A reliable establishment of early and correct diagnosis is crucial for effective management of periprosthetic joint infection (PJI). Early detection and subsequent management are warranted to control the systemic inflammatory response and to avoid biofilm formation on the implants. It also often allows for less aggressive surgical treatment [28].
In contrast to acute PJI, chronic PJI frequently presents with a more subtle clinical picture, and ‘conventional’ diagnostic methods are often unremarkable. Consequently, PJI may be misinterpreted as instability, aseptic loosening, or implant malposition. In fact, this clearly highlights the urgent need for accurate and reliable testing methods for the diagnosis of PJI.
Synovial fluid biomarkers are increasingly used in the diagnostic workup of PJI. The theoretical advantage is the direct measurement and prompt result of the affected joint. Synovial fluid biomarkers well described in association with PJI include Interleukin-6 [7], CRP [31], alpha-defensin [3], and leukocyte esterase [30]. Some previous studies have revealed a high accuracy of these biomarkers for detecting PJI. However, the reality is that lack of consensus currently persists, complicating the smooth translation of biomarker-based diagnostic tests to standard algorithms in clinical practice. This emphasizes the need for meta-analyses in the field that could compute the large pool of accuracy reports into comprehendible output values clinicians could employ with simplicity, ultimately easing the process of research translation and ensuring evidence-based practice.
The aim of the current meta-analysis was to (1) determine the overall accuracy of synovial alpha-defensin, synovial C-reactive protein (sCRP), interleukin-6 (sIL-6), and leukocyte esterase (sLE) as diagnostic markers for periprosthetic joint infection (PJI) and (2) to independently evaluate the accuracy of both the laboratory-based ELISA alpha-defensin test and the commercially available Synovasure™ test kit.
Materials and methods
Search strategy
A systematic literature search was conducted using the databases MEDLINE (PubMed) and OVID (EMBASE), including all publications from database inception until 21 August 2017. The search terms are provided in the supplementary material alongside the manuscript.
Eligibility criteria
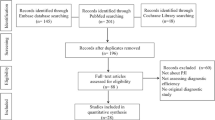
Potentially relevant publications were screened by two independent reviewers to ensure adherence to the following inclusion criteria: (1) test accuracy as a primary research question, (2) inclusion of quantitative accuracy information (sensitivity, specificity or likelihood ratios). Articles not focusing on diagnostic tests (e.g. on therapeutic or economic aspects) or not containing original quantitative values of sensitivity and specificity, systematic reviews or narrative reviews, guidelines, recommendations and expert opinions and case reports were excluded (Fig. 1).
Data extraction
Two authors worked independently to classify studies and extract data. Sensitivity, specificity, positive and negative likelihood ratios (LR), positive and negative predictive values as well as area under the curve (AUC) were extracted. Quality assessment of each study was also performed using the QUADAS (Quality Assessment of Diagnostic Accuracy Studies) tool [44].
Statistical analysis
Four biomarkers were analysed: alpha-defensin, CRP in synovial fluid, synovial interleukin-6 and leukocyte esterase. All calculations were performed using continuity-corrected cell counts. The continuity correction was added to the whole data as soon as one cell in one study was zero. Sensitivity and specificity were meta-analysed using the bivariate diagnostic random-effects model described by Reitsma et al. [33] and were estimated by restricted maximum likelihood (REML). For alpha-defensin, two different assay types were included (laboratory ELISA versus Synovasure™ lateral flow test kit) and analysed using a bivariate random-effects meta-regression with the assay type as covariate, or using two separate models. The combined, meta-analysed estimates for sensitivity and specificity were reported with 95% confidence intervals (95% CI). Combined estimates for postive and negative likelihood ratio (LR), and diagnostic odds ratio (DOR) were calculated using a sampling approach according to Zwinderman and Bossuyt [45]. A summary receiver operating characteristic curve (ROC) curve was constructed based on Monte Carlo simulations [11]. The area under the curve (AUC) was calculated using the trapezoidal rule also including the extrapolated points of the ROC curve. A sensitivty analysis was performed to assess the effect of the inclusion of more than one value of sensitivity/specificity from the same study. All analyses were performed using R (MADA package Boston, Massachusetts, USA).
This study did not involve experiments or direct analysis of patient data. No ethical approval was necessary.
Results
Four synovial biomarker groups were covered: alpha-defensin (n = 10 articles), synovial CRP (n = 9 articles), synovial leukocyte esterase (n = 12 articles) and synovial interleukin-6 (n = 11 articles) (Fig. 1). Articles were published between the years 2007 and 2017. A total of 3734 prosthetic joints were examined, of which 1107 were infected. The median (range) QUADAS-2 quality score was 13 (13; 14) for articles dealing with synovial CRP, 12 (12; 13) for articles dealing with IL-6, 12.5 (11; 14) for articles dealing with leukocyte esterase and 13 (12; 14) for articles dealing with alpha-defensin. This demonstrates the good quality of diagnostic studies included here, given that the maximum possible score of 14 points.
Diagnostic values and meta-analysed estimates
Characteristics of diagnostic studies with the corresponding pooled values from this analysis are illustrated in Tables 1, 2, 3 and 4. Forest plots showing the study-specific and meta-analysed estimates of sensitivity and specificity for each synovial fluid biomarker are seen in Figs. 2, 3, 4 and 5. Summary ROC curves constructed for all assays based on Monte Carlo simulations are shown in Fig. 6.
Summary receiver operating characteristic curve (ROC curve). The dashed part of the curve is extrapolated beyond the observed data range. Estimates of sensitivity and specificity for each study are indicated with open circles, and the meta-analysed summary estimate with a filled circle together with the 95% confidence region. AUC area under the curve
Discussion
The most important findings of this meta-analysis are: (1) the laboratory-based alpha-defensin enzyme-linked immunosorbent assay (ELISA) test demonstrated the highest ever reported accuracy for PJI diagnosis; (2) the accuracy of the Synovasure™ alpha-defensin test kit is markedly lower than that of the laboratory ELISA; (3) the Synovasure™ alpha-defensin test kit, synovial CRP, synovial Interleukin-6 and synovial leukocyte esterase showed an overall good and similar accuracy, however, not higher than the accuracy previously reported for synovial white cell count (sWBC) or culture bacteriology.
In clinical practice, the diagnostic workup of PJI is based on the initial assumption that every painful prosthetic joint is infected until proven otherwise [2]. From there, it is the responsibility of the clinician to provide arguments for the absence of an infection. It was previously mentioned that the majority of available tests show effectiveness in either excluding a PJI or confirming it, but not necessarily both [2]. A measure used for detecting the strengths of diagnostic tests in that regard is the likelihood ratio (LR), which incorporates both sensitivity and specificity, is simple to understand and allows for comparison between tests. It was utilized for result interpretation in this section of the manuscript [17].
It was shown in a survey published by the European Knee Associates (EKA) in 2016 that synovial biomarker testing was performed by less than 5% of surgeons [1]. This value is obviously low; however, the question of whether to increase the utility of those tests is only to be answered by current clinical evidence. The two well-established tests and commonly used tools will be referred to for comparison: (i) synovial fluid white cell count (sWBC) as an effective test for PJI exclusion and (ii) culture bacteriology as an effective tool for confirmation of PJI [2].
Firstly, it is important to underline the fact that based on the results of this meta-analysis, there is a difference between accuracy of the laboratory alpha-defensin ELISA test and the Synovasure™ test kit. The laboratory ELISA reports demonstrate the best ever reported overall accuracy compared to any other test, reflected in the efficacy in both ruling out an infection or confirming it with very high pooled sensitivity and specificity values of 97%. It is fair to note that only four studies were found and included in this meta-analysis. The Synovasure™ test kit on the other hand showed markedly lower accuracy values with a lower capacity to exclude a PJI than sWBC, and lower potency to confirm a PJI than culture bacteriology. The test could therefore be performed as an adjunct and should not serve as a standalone test. It should be encouraged to perform comparative controlled studies in an attempt to find the reason for the aforementioned discrepancy.
Regarding the remaining synovial biomarkers, synovial CRP showed a very high potency for ruling out a PJI, similar to sWBC count but not better. Regarding confirmation of PJI, it did not prove better than bacterial culture examinations. Both synovial leukocyte esterase and synovial interleukin-6 were inferior to sWBC for ruling out PJI and inferior to bacterial culture examinations for confirming it.
Limitations of the study included the fact that only four studies of alpha-defensin ELISA were found and included. Two of these four studies did not find any false negatives or positives (reported a sensitivity and specificity of 100%) and a continuity correction was applied which could lead to an underestimation of the true values. Secondly, some studies were included twice in the meta-analysis as they reported sensitivity and specificity at two different cutoffs. This procedure violates the independence assumption and may lead to the underestimation of the uncertainty in the meta-analysis. Therefore, sensitivity analyses with only one cutoff were included for each study. All possible combinations were analysed for each end point (e.g. two analyses for one duplicated study, four analyses for two duplicated studies and eight analyses for three duplicated studies). Differences for both point and interval estimates were very small, and the correlation between estimates from the same studies seems not to be a major concern.
The relevance of the results to clinical practice can be reflected in that biomarkers in synovial fluid are of significance and their use should be encouraged given the relatively high accuracy. However, they do not yet provide more powerful diagnostic tools than conventional synovial exam such as synovial white blood cell count, or tissue culture. They are still not to be seen as standalone diagnostic tests. Furthermore, all evidence is in favour of the laboratory-based ELISA alpha-defensin test and therefore its use should be encouraged.
Conclusion
The laboratory-based alpha-defensin ELISA test demonstrated the highest ever reported accuracy for PJI diagnosis. However, this does not apply to the Synovasure™ alpha-defensin test kit, which showed a markedly lower accuracy and should therefore be critically appreciated. Synovasure™ alpha-defensin, synovial CRP, synovial Interleukin-6 and synovial leukocyte esterase were not superior to synovial white cell count or culture bacteriology in the overall potency as diagnostic tools. Therefore, synovial biomarkers should not replace existing tools, but be used as diagnostic adjuncts.
References
Ahmad SS, Becker R, Chen AF, Kohl S (2016) EKA survey: diagnosis of prosthetic knee joint infection. Knee Surg Sports Traumatol Arthrosc 24:3050–3055
Ahmad SS, Shaker A, Saffarini M, Chen AF, Hirschmann MT, Kohl S (2016) Accuracy of diagnostic tests for prosthetic joint infection: a systematic review. Knee Surg Sports Traumatol Arthrosc 24:3064–3074
Bingham J, Clarke H, Spangehl M, Schwartz A, Beauchamp C, Goldberg B (2014) The alpha defensin-1 biomarker assay can be used to evaluate the potentially infected total joint arthroplasty. Clin Orthop Relat Res 472:4006–4009
Bonanzinga T, Zahar A, Dütsch M, Lausmann C, Kendoff D, Gehrke T (2017) How reliable is the alpha-defensin immunoassay test for diagnosing periprosthetic joint infection? A prospective study. Clin Orthop Relat Res 475:408–415
Buttaro MA, Martorell G, Quinteros M, Comba F, Zanotti G, Piccaluga F (2015) Intraoperative synovial C-reactive protein is as useful as frozen section to detect periprosthetic hip infection. Clin Orthop Relat Res 473:3876–3881
Colvin OC, Kransdorf MJ, Roberts CC, Chivers FS, Lorans R, Beauchamp CP et al (2015) Leukocyte esterase analysis in the diagnosis of joint infection: can we make a diagnosis using a simple urine dipstick? Skeletal Radiol 44:673–677
Deirmengian C, Hallab N, Tarabishy A, Della Valle C, Jacobs JJ, Lonner J et al (2010) Synovial fluid biomarkers for periprosthetic infection. Clin Orthop Relat Res 468:2017–2023
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Booth RE et al (2015) The alpha-defensin test for periprosthetic joint infection outperforms the leukocyte esterase test strip. Clin Orthop Relat Res 473:198–203
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J (2014) Combined measurement of synovial fluid α-defensin and C-reactive protein levels: highly accurate for diagnosing periprosthetic joint infection. J Bone Jt Surg Am 96:1439–1445
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J (2014) Diagnosing periprosthetic joint infection: has the era of the biomarker arrived? Clin Orthop Relat Res 472:3254–3262
Doebler P, Holling H, Böhning D (2012) A mixed model approach to meta-analysis of diagnostic studies with binary test outcome. Psychol Methods 17:418
Frangiamore SJ, Gajewski ND, Saleh A, Farias-Kovac M, Barsoum WK, Higuera CA (2016) α-Defensin accuracy to diagnose periprosthetic joint infection—best available test? J Arthroplast 31:456–460
Frangiamore SJ, Saleh A, Grosso MJ, Kovac MF, Higuera CA, Iannotti JP et al (2015) α-Defensin as a predictor of periprosthetic shoulder infection. J Shoulder Elbow Surg 24:1021–1027
Frangiamore SJ, Saleh A, Grosso MJ, Kovac MF, Zhang X, Daly TM et al (2017) Neer Award 2015: analysis of cytokine profiles in the diagnosis of periprosthetic joint infections of the shoulder. J Shoulder Elbow Surg 26:186–196
Frangiamore SJ, Saleh A, Kovac MF, Grosso MJ, Zhang X, Bauer TW et al (2015) Synovial fluid interleukin-6 as a predictor of periprosthetic shoulder infection. J Bone Jt Surg Am 97:63–70
Frangiamore SJ, Siqueira MB, Saleh A, Daly T, Higuera CA, Barsoum WK (2016) Synovial cytokines and the MSIS criteria are not useful for determining infection resolution after periprosthetic joint infection explantation. Clin Orthop Relat Res 474:1630–1639
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM (2003) The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 56:1129–1135
Gollwitzer H, Dombrowski Y, Prodinger PM, Peric M, Summer B, Hapfelmeier A et al (2013) Antimicrobial peptides and proinflammatory cytokines in periprosthetic joint infection. J Bone Jt Surg Am 95:644–651
Guenther D, Kokenge T, Jacobs O, Omar M, Krettek C, Gehrke T et al (2014) Excluding infections in arthroplasty using leucocyte esterase test. Int Orthop 38:2385–2390
Jacovides CL, Parvizi J, Adeli B, Am Jung K (2011) Molecular markers for diagnosis of periprosthetic joint infection. J Arthroplasty 26:99–103
Kasparek MF, Kasparek M, Boettner F, Faschingbauer M, Hahne J, Dominkus M (2016) Intraoperative diagnosis of periprosthetic joint infection using a novel alpha-defensin lateral flow assay. J Arthroplast 31:2871–2874
Kheir MM, Ackerman CT, Tan TL, Benazzo A, Tischler EH, Parvizi J (2017) Leukocyte esterase strip test can predict subsequent failure following reimplantation in patients with periprosthetic joint infection. J Arthroplast 32:1976–1979
Koh IJ, Han SB, In Y, Oh KJ, Lee DH, Kim TK (2017) The leukocyte esterase strip test has practical value for diagnosing periprosthetic joint infection after total knee arthroplasty: a multicenter study. J Arthroplast 32:3519–3523
Lenski M, Scherer MA (2014) Synovial IL-6 as inflammatory marker in periprosthetic joint infections. J Arthroplasty 29:1105–1109
Nelson GN, Paxton ES, Narzikul A, Williams G, Lazarus MD, Abboud JA (2015) Leukocyte esterase in the diagnosis of shoulder periprosthetic joint infection. J Shoulder Elbow Surg 24:1421–1426
Nilsdotter-Augustinsson Å, Briheim G, Herder A, Ljunghusen O, Wahlström O, Öhman L (2007) Inflammatory response in 85 patients with loosened hip prostheses: a prospective study comparing inflammatory markers in patients with aseptic and septic prosthetic loosening. Acta Orthop 78:629–639
Omar M, Ettinger M, Reichling M, Petri M, Guenther D, Gehrke T et al (2015) Synovial C-reactive protein as a marker for chronic periprosthetic infection in total hip arthroplasty. Bone Jt J 97:173–176
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM et al (2013) Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56:1–10
Parvizi J, Jacovides C, Adeli B, Am Jung K, Hozack WJ (2012) Mark B. Coventry award: synovial C-reactive protein: a prospective evaluation of a molecular marker for periprosthetic knee joint infection. Clin Orthop Relat Res 470:54–60
Parvizi J, Jacovides C, Antoci V, Ghanem E (2011) Diagnosis of periprosthetic joint infection: the utility of a simple yet unappreciated enzyme. J Bone Jt Surg Am 93:2242–2248
Parvizi J, McKenzie JC, Cashman JP (2012) Diagnosis of periprosthetic joint infection using synovial C-reactive protein. J Arthroplast 27:12–16
Randau TM, Friedrich MJ, Wimmer MD, Reichert B, Kuberra D, Stoffel-Wagner B et al (2014) Interleukin-6 in serum and in synovial fluid enhances the differentiation between periprosthetic joint infection and aseptic loosening. PLoS One 9:e89045
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58:982–990
Ronde-Oustau C, Diesinger Y, Jenny J-Y, Antoni M, Gaudias J, Boeri C et al (2014) Diagnostic accuracy of intra-articular C-reactive protein assay in periprosthetic knee joint infection—a preliminary study. Orthop Traumatol Surg Res 100:221–224
Shafafy R, McClatchie W, Chettiar K, Gill K, Hargrove R, Sturridge S et al (2015) Use of leucocyte esterase reagent strips in the diagnosis or exclusion of prosthetic joint infection. Bone Jt J 97:1232–1236
Sigmund I, Holinka J, Gamper J, Staats K, Böhler C, Kubista B et al (2017) Qualitative α-defensin test (Synovasure) for the diagnosis of periprosthetic infection in revision total joint arthroplasty. Bone Jt J 99:66–72
Suda AJ, Tinelli M, Beisemann ND, Weil Y, Khoury A, Bischel OE (2017) Diagnosis of periprosthetic joint infection using alpha-defensin test or multiplex-PCR: ideal diagnostic test still not found. Int Orthop 41(7):1307–1313
Tarabichi M, Fleischman AN, Shahi A, Tian S, Parvizi J (2017) Interpretation of leukocyte esterase for the detection of periprosthetic joint infection based on serologic markers. J Arthroplast 32(9S):S97–S100.e1
Tetreault MW, Wetters NG, Moric M, Gross CE, Della Valle CJ (2014) Is synovial C-reactive protein a useful marker for periprosthetic joint infection? Clin Orthop Relat Res 472:3997–4003
Tischler EH, Cavanaugh PK, Parvizi J (2014) Leukocyte esterase strip test: matched for musculoskeletal infection society criteria. J Bone Jt Surg Am 96:1917–1920
Vanderstappen C, Verhoeven N, Stuyck J, Bellemans J (2013) Intra-articular versus serum C-reactive protein analysis in suspected periprosthetic knee joint infection. Acta Orthop Belg 79:326–330
Wang C, Li R, Wang Q, Duan J, Wang C (2017) Leukocyte esterase as a biomarker in the diagnosis of periprosthetic joint infection. Med Sci Monit 21 23:353–358
Wetters NG, Berend KR, Lombardi AV, Morris MJ, Tucker TL, Della Valle CJ (2012) Leukocyte esterase reagent strips for the rapid diagnosis of periprosthetic joint infection. J Arthroplasty 27:8–11
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Zwinderman AH, Bossuyt PM (2008) We should not pool diagnostic likelihood ratios in systematic reviews. Stat Med 27:687–697
Funding
The study was financed by acquired independent research funds, and was not financed by a specific grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
This study dealt with published data only, no ethical approval was needed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ahmad, S.S., Hirschmann, M.T., Becker, R. et al. A meta-analysis of synovial biomarkers in periprosthetic joint infection: Synovasure™ is less effective than the ELISA-based alpha-defensin test. Knee Surg Sports Traumatol Arthrosc 26, 3039–3047 (2018). https://doi.org/10.1007/s00167-018-4904-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4904-8