Abstract
Purpose
Notwithstanding the importance of the tibial slope (TS) for anterior tibial translation, little information is available regarding the implications on posterior laxity, particularly in healthy subjects. It was hypothesized that increased TS is associated with decreased posterior tibial translation (PTT) in healthy knees.
Methods
A total of 124 stress radiographs of healthy knees were enrolled in this study. Tibial slope and the posterior tibial translation were evaluated using a Telos device with a 150-N force at 90° of knee flexion. Two blinded observers reviewed independently on two different occasions.
Results
One hundred and twenty-four patients [35 females and 89 males; 41 (range 18–75) years] were enrolled in this study, with a mean PTT of 2.8 mm (±1.9 mm; range 0–8 mm) and a mean TS of 8.6° (±2.6°; range 1°–14°). Pearson correlation showed a significant correlation between the PTT and TS in the overall patient cohort (P < 0.0001) with r = 0.76 and R 2 = 0.58. There was no statistical difference between female and male patients regarding the PTT or the TS. Subgrouping of the patient cohort (four groups with n = 31) according to their TS (groups I < 7°; II = 7°–8.5°; III = 9°–10.5°; IV ≥ 11°) revealed significant differences between each subgroup, respectively. Furthermore, there was a weak but significant correlation between age and PTT (P = 0.004, r = 0.26).
Conclusion
In addition to the substantial variance in tibial slope and posterior laxity among healthy knees, high tibial slope significantly correlates with increased posterior tibial translation. Increasing age is further associated with a greater magnitude of posterior tibial translation. Consequently, knowledge of the tibial slope facilitates simple estimation of posterior knee laxity, which is mandatory for PCL reconstruction and knee arthroplasty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The contributions of soft tissue restraints on posterior knee laxity, such as the posterior cruciate ligament, the posterolateral corner and the meniscus, are highly acknowledged, albeit the importance of the bony geometry of the underlying tibial plateau is less well understood.
There is an emerging consensus that the dorsal inclination of the tibial plateau has a direct influence on the kinematics of the knee [6, 8, 11, 21, 22, 29, 41, 42]. This includes anteroposterior laxity, the centre of rotation and loading of the cruciate ligaments.
Specifically, an increased tibial slope (TS) has been shown to result in greater anterior tibial translation during simple weight-bearing activities [8]. Current scientific literature supports a moderate-to-strong association in predisposing an individual to an increased risk of ACL or ACL graft injury [22, 41, 42].
In contrast, it has been reported that an increased TS may avoid mechanical overload of the graft after reconstruction of the posterior cruciate ligament (PCL) and thus may be beneficial for long-term knee stability [10]. This might elucidate why current surgical approaches have been ineffective in consistently restoring knee stability to its original state [3, 35, 38, 43].
However, there is still scientific paucity of the impact of tibial slope on posterior laxity. By implication, the present study is the first to evaluate the association between tibial slope and posterior tibial translation in healthy knees. As measurement of the tibial slope on lateral knee radiographs or cross-sectional imaging can easily be implemented in clinical routine, it might facilitate estimation of posterior knee laxity. This could lead to a better understanding of knee kinematics and could yield important implications for knee surgery, such as PCL reconstruction or implant choice in knee arthroplasty. The tested hypothesis was that an increased tibial slope is associated with a smaller magnitude of posterior knee laxity in healthy knees, irrespective of gender or age.
Materials and methods
The ethics committee of Charité-Universitaetsmedizin Berlin (EA1/003/16) approved the current study. A retrospective analysis was conducted on patients, who underwent bilateral posterior stress radiographs, within a 2-year period (May 2014–May 2016).
Care was taken, that only radiographs of the uninjured, contralateral knees were included, as assessed by the patients’ history. If this was not recorded in detail, the patient was further interviewed by telephone. The exclusion criteria comprised patients with bilateral injuries, combined lower extremity fractures or prior surgery to the uninvolved knee or missing clinical data.
Two blinded observers evaluated the posterior tibial slope and the posterior tibial translation by using a PACS workstation (Centricity RIS-I 4.2 Plus, GE Healthcare, Milwaukee, WI, USA). Each observer measured both parameters separately. Mean values for the TS and the PTT were calculated, respectively.
The tibial slope is defined as the angle formed at the intersection of a line parallel to posterior inclination of the tibial plateau and a line perpendicular to the diaphyseal shaft axis of the tibia. TS was measured according to Dejour et al. [8]. As the medial contour of the tibial plateau is usually superimposed on lateral radiographs, it was chosen to measure the medial TS. The diaphyseal shaft axis was measured by two mid-points between the anterior and posterior tibial cortex at 5 cm below the tibial tuberosity and 15 cm below the tibial joint line. Subsequently, the tibial slope is determined between the tangent line to the respective medial tibial plateau and the perpendicular to the established diaphyseal axis. In case of multiple radiographs of the same patient, the TS was measured on the radiograph, which contained of the longest diaphyseal axis and the best true lateral view of the tibia.
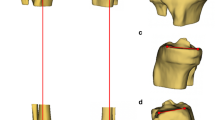
Posterior tibial translation was measured by the use of conventional stress radiographs at 90° of flexion using a Telos device, with a posteriorly directed force of 150 N at the level of the tibial tubercle. Posterior tibial translation was determined according to the technique described by Jacobsen [16] as well as Schulz and Strobel [32, 33] using peripheral bony landmarks. Perpendicular to the tangent of the joint line, the mid-points between the most posterior contours of the medial and lateral femoral condyles and tibial plateaus were created. The distance between these two points was regarded as the posterior tibial translation (Fig. 1).
Statistical analysis
Subgrouping between female and male patients was made to examine gender differences. Additionally, four subgroups were formed based on the tibial slope.
Statistical analysis was performed using Prism Version 6 (GraphPad Software Inc., San Diego, CA) and SPSS Version 24 (IBM Corp., USA). The average PTS and PTT are reported as mean with upper and lower 95% CIs. A normal distribution of data was confirmed using D’Agostino and Pearson omnibus normality tests. The comparison of the parametric data was made with a t test, and a Pearson correlation was performed in order to establish an association between tibial slope/posterior tibial translation and patients age/posterior tibial translation, assessing r and R 2.
The intraclass correlation coefficient (ICC) was used to evaluate intra- and interrater reliability. Intraobserver reliability was assessed by a repeat measurement of each observer on a random sample of 25 images selected from the total cohort. The interval between measurements of the same observer was 2 weeks. Notably, values of an ICC of 0.5–0.6 are regarded as moderate agreement, whereas 0.7–0.8 indicate a strong agreement. P < 0.05 was considered statistically significant.
Power analysis based on the correlation between the PTT and TS revealed the need for a minimum of eleven subjects to establish 80% power to protect against the undue rejection of the null hypothesis. To further account for the correlation between age and PTT, post hoc power analysis revealed a power greater than 0.84 with α = 0.05 in a total sample size of 124 patients.
Results
A total of 124 patients (35 females and 89 males) at a mean age of 41 (range 18–75) years met our inclusion criteria and were enrolled in this study. ICC between the observers was 0.82 for the tibial slope and 0.78 for the posterior tibial translation, indicating a high interrater agreement. Intrarater agreement was 0.87 for the tibial slope and 0.85 for the posterior tibial translation for reader one and 0.88 as well as 0.80 for reader two.
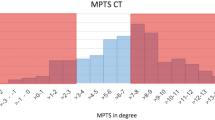
Radiographic assessment revealed a mean posterior tibial translation of 2.8 mm (±1.9 mm; range 0–8 mm) and a mean tibial slope of 8.6° (±2.6°; range 1°–14°). Pearson correlation analysis showed a significant correlation between the PTT and TS in the overall patient cohort (P < 0.0001) with r = 0.76 and R 2 = 0.58 (Fig. 2).
Additionally, a comparative analysis was performed comparing the tibial slope and posterior tibial translation in female (n = 35) versus male (n = 89) patients. There were no significant differences regarding the PTT (2.7 ± 2.0 mm vs. 2.8 ± 1.9 mm; n.s.). Likewise, there was no statistical difference in TS between female and male patients (7.9 ± 2.8 vs. 8.8° ± 2.5°; n.s.).
In order to improve comparability, subdivision of the patient cohort (four groups with 31 patients each) according to their tibial slope (group I < 7°; II = 7°–8.5°; III = 9–10.5°; IV ≥ 11°) was conducted. Group I showed a significantly lower posterior tibial translation when compared to group II (0.9 ± 0.8 vs. 1.8 ± 1.3 mm; P = 0.008). Accordingly, group II had a significantly lower posterior translation when compared to group III (1.8 ± 1.3 vs. 3.8 ± 1.1 mm; P < 0.0001) and group III to group IV (3.8 ± 1.1 vs. 4.8 ± 1.2 mm; P = 0.001), respectively (Fig. 3).
Finally, Pearson correlation revealed a significant correlation between age and posterior tibial translation (P = 0.004, r = 0.26). While this finding illustrates that PTT significantly increases with age, correlation coefficients of this magnitude only represent a weak correlation. Creating two equal subgroups of the patient cohort according to their age (group A: 30.7 ± 6.7 years vs. group B: 51.4 ± 6.3 years) showed a significantly higher PTT for group B (3.2 ± 1.9 vs. 2.5 ± 1.9 mm; P = 0.04).
Discussion
The most important finding of the present study was that increased tibial slope significantly correlates with higher values of posterior tibial translation in healthy knees. In contrast to patients’ gender, increasing age was further associated with a greater magnitude of posterior tibial translation.
Notwithstanding the importance of the TS for anterior laxity, little information is available regarding the implications on posterior laxity. An increased tibial slope has been acknowledged to result in greater anterior translation of the tibia and increased strain on the anterior cruciate ligament [5, 8, 36, 40]. Vice versa, an increased tibial slope will decrease the in situ forces of the posterior cruciate ligament, which is in accordance with our prior results [11]. At the beginning of the last century, Wilhelm Roux stated “an organ will adapt itself structurally to an alteration, quantitative or qualitative in function” [31]. This has been demonstrated in regard to knee kinematics, both clinically and in in vitro studies [20, 26, 28]. Ochi et al. [28] illustrated in patients with PCL deficiency that the ACL lost its functional tension and consequently underwent decreased stress shielding. This resulted in direct morphological changes of the ACL as shown in a reduced number and diameter of its collagen fibrils.
Taking these findings into account, the present study suggests that patients with an increased tibial slope undergo decreased PCL strain during simple weight-bearing activities and are prone to an increased physiological posterior laxity.
Consequently, the study shows that there is substantial variance not only in the TS but also in the PTT among healthy knees. Knowledge of these individual differences can lead to a more accurate replication of physiological knee kinematics after implantation of a total (TKA) or unicompartmental knee arthroplasty (UKA). There are several studies, which suggest that the tibial slope should be recreated in TKA and UKA [7, 13, 37]. Exemplarily, Singh et al. [37] stated that “using a standardized posterior tibial slope cutting angle results in a change in the soft-tissue balance and envelope of laxity of the knee”. Notably, this “functional soft tissue envelope of the knee” needs to be restored according to the authors. However, it has not yet been further specified.
To the best of our knowledge, the current study is the first to demonstrate a direct correlation between the tibial slope and posterior knee laxity and thus might explain the superior outcome of TKA surgery, which aims to recreate the preoperative tibial slope.
Furthermore, achieving proper posterior soft tissue tension is mandatory in cruciate-retaining TKAs to enable proper femoral rollback, which determines the range of motion [25]. Thus, overloading due to a tight and unbalanced PCL is believed to result in a decreased range of motion, excessive posterior polyethylene wear and its associated complications [4, 9, 23, 30, 34, 39]. Partial PCL release is advocated in these cases, even though this technique has not been investigated thoroughly and may lead to a mismatch between the extension and flexion gaps [2, 17, 22]. The presented results suggest that the underlying geometry of the operated knee and its posterior laxity can be estimated preoperatively on lateral radiographs by measurement of the tibial slope. This can help to detect at-risk patients; thus, surgeons may encounter unexpected PCL tension less likely during surgery. Vice versa, posteriorly stabilized implant designs have to be considered in patients with a high tibial slope. Posteriorly stabilized implants attempt to substitute the function of the posterior cruciate ligament using a polyethylene post and femoral cam that interact to prevent posterior tibial translation, while ensuring a more stable component interface than cruciate-retaining designs. Taking the results of the current study into account, it might be advisable in patients with a high tibial slope and thus an assumable increased posterior laxity to use posteriorly stabilized implants, as they have been advocated to result in decreased posterior tibial translation under weight-bearing conditions [44]. However, future clinical studies are needed to further delineate this matter.
As far as UKA surgery is concerned, tibial slope is commonly modified due to the implant design and surgical technique, targeting a TS of 5°–7° [7, 12, 27]. Taking our results into account, this approach will fail to recreate native knee kinematics in a large percentage of patients.
Posterior stress radiographs have been acknowledged to provide a high accuracy for an objective quantification of the posterior tibial translation, without soft tissue interference in patients with potential PCL deficiency [18, 32]. Our results underline the importance of a bilateral clinical examination or of bilateral stress radiographs to detect PCL injuries, as physiological posterior laxity shows considerable individual variance. Notably, knowledge of the tibial slope can help to estimate the amount of physiological posterior laxity and to enable comparisons against pathological laxity in patients, in which the contralateral side cannot serve as a physiological comparison.
Notably, there are several limitations to the study. Demographic data, such as height, weight, body mass index and ethnicity, were not available for review. Thus, correlations between these factors were not delineated.
Another drawback is that the impact of the tibial slope on anterior laxity in healthy knees has not been specified in the current study. This is due to the fact that anterior stress radiographs in 90° of flexion do not accurately display anterior laxity [15].
Finally, the tibial slope was measured on lateral radiographs, thereby ignoring a potential asymmetry of the medial and lateral, as well as of the chondral or meniscal slope. As the medial slope is usually superimposed on lateral radiographs, we chose to measure the medial slope, as proposed in the literature [1].
Precise measurement of the tibial slope usually requires a lateral radiograph, displaying the knee as well as the ankle joint, as measurements are easily overestimated the shorter the depicted tibial axis [10]. To mitigate this concern and to ensure comparability, only stress radiographs were included, as the Telos device predefines the tibial length. We further excluded radiographs, which did not include a true lateral view of the tibia as determined by proper superimposition of the femoral condyles, as rotation of the tibial shaft has been demonstrated to lead to an inaccurate assessment of the TS [19].
Notably, there is still little consensus on the ideal reference to measure the tibial slope [1]. Moore and Harvey [24] introduced a method as a line congruent with the anterior tibial cortex, but this method is likely to introduce inaccuracy due to the high variability of the tibial tuberosity. Dejour et al. [8] proposed an alternative diaphyseal tibial axis using two mid-points between the anterior and posterior tibial cortex, one below the tibial tubercle and the other 15 cm below the tibial joint line. Overall, the complex geometry of the femur and tibia cannot be completely represented by one-dimensional lateral radiographs. Thus, future cross-sectional imaging studies should devote more attention to an individual analysis of the medial and lateral compartment to further clarify the effect of the bony morphology on posterior laxity with more definitive information. Nevertheless, Hudek et al. [14] described a high inter- and intraobserver accordance for the aforementioned method by Dejour et al. [8], a high reproducibility and a good correlation between the medial tibial slope on radiographs and MRI.
Conclusion
The findings of the present study indicate that there is a substantial variance not only of tibial slope but also of posterior laxity among healthy knees. More specifically, an increment in tibial slope significantly correlates with an increase in posterior tibial translation. In contrast to patients’ gender, increasing age is further associated with a greater magnitude of posterior tibial translation. Consequently, knowledge of the tibial slope facilitates simple estimation of posterior knee laxity, which is mandatory in PCL reconstruction and knee arthroplasty.
References
Ahmad R, Patel A et al (2016) Posterior tibial slope: effect on, and interaction with, knee kinematics. JBJS Rev 4:31–36
Arima J, Whiteside LA et al (1998) Effect of partial release of the posterior cruciate ligament in total knee arthroplasty. Clin Orthop Relat Res 353:194–202
Barrett GR, Savoie FH (1991) Operative management of acute PCL injuries with associated pathology: long-term results. Orthopedics 14:687–692
Bellemans J, Robijns F et al (2005) The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 13:193–196
Beynnon BD, Fleming BC et al (2002) Chronic anterior cruciate ligament deficiency is associated with increased anterior translation of the tibia during the transition from non-weightbearing to weightbearing. J Orthop Res 20:332–337
Cantin O, Magnusson RA et al (2015) The role of high tibial osteotomy in the treatment of knee laxity: a comprehensive review. Knee Surg Sports Traumatol Arthrosc 23:3026–3037
Chatellard R, Sauleau V et al (2013) Medial unicompartmental knee arthroplasty: does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res 99:S219–S225
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76:745–749
D’Lima DD, Patil S et al (2007) An ABJS best paper: dynamic intraoperative ligament balancing for total knee arthroplasty. Clin Orthop Relat Res 463:208–212
Faschingbauer M, Sgroi M et al (2014) Can the tibial slope be measured on lateral knee radiographs? Knee Surg Sports Traumatol Arthrosc 22:3163–3167
Gwinner C, Weiler A et al (2017) Tibial slope strongly influences knee stability after posterior cruciate ligament reconstruction: a prospective 5- to 15-year follow-up. Am J Sports Med 2:355–361
Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 86-A:506–511
Hoffman AA, Bachus KN et al (1991) Effect of the tibial cut on subsidence following total knee arthroplasty. Clin Orthop Relat Res 269:63–69
Hudek R, Schmutz S et al (2009) Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res 467:2066–2072
Iversen BF, Stürup J et al (1989) Implications of muscular defense in testing for the anterior drawer sign in the knee. Am J Sports Med 17:409–413
Jacobsen K (1976) Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand 47:335–344
Jojima H, Whiteside LA, Ogata K (2004) Effect of tibial slope or posterior cruciate ligament release on knee kinematics. Clin Orthop Relat Res 426:194–198
Jung TM, Reinhardt C et al (2006) Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc 14:1116–1121
Kessler MA, Burkart A et al (2003) Development of a 3-dimensional method to determine the tibial slope with multislice-CT. Z Orthop Ihre Grenzgeb 141:143–147
Lee DH, Park SC et al (2016) Effect of soft tissue laxity of the knee joint on limb alignment correction in open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 24:3704–3712
Lee SY, Lim HC et al (2017) Sagittal osteotomy inclination in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 25:823–831
Li Y, Hong L et al (2014) Are failures of anterior cruciate ligament reconstruction associated with steep posterior tibial slopes? A case control study. Chin Med J (Engl) 127:2649–2653
Lu H, Mow CS, Lin J (1999) Total knee arthroplasty in the presence of severe flexion contracture: a report of 37 cases. J Arthroplasty 14:775–780
Moore TM, Harvey JP (1974) Roentgenographic measurement of tibial-plateau depression due to fracture. J Bone Joint Surg Am 56:155–160
Morberg P, Chapman-Sheath P et al (2002) The function of the posterior cruciate ligament in an anteroposterior-gliding rotating platform total knee arthroplasty. J Arthroplasty 17:484–489
Murao T, Ochi M et al (1997) The adverse effects of sectioning the posterior cruciate ligament in rabbits. Changes in the structural and morphological properties of the femur-anterior cruciate ligament-tibia complex. Arch Orthop Trauma Surg 116:1–5
Nunley RM, Nam D et al (2014) Extreme variability in posterior slope of the proximal tibia: measurements on 2395 CT scans of patients undergoing UKA? J Arthroplasty 29:1677–1680
Ochi M, Murao T et al (1999) Isolated posterior cruciate ligament insufficiency induces morphological changes of anterior cruciate ligament collagen fibrils. Arthroscopy 15:292–296
Ozel O, Yucel B et al (2017) Changes in posterior tibial slope angle in patients undergoing open-wedge high tibial osteotomy for varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc 25:314–318
Pagnano MW, Cushner FD, Scott NW (1998) Role of the posterior cruciate ligament in total knee arthroplasty. J Am Acad Orthop Surg 6:176–187
Roux W (1905) Die Entwicklungsmechanik; ein neuer Zweig der biologischen Wissenschaft, vols I & II. Ed. Wilhelm Engelmann, Leipzig
Schulz MS, Russe K et al (2005) Reliability of stress radiography for evaluation of posterior knee laxity. Am J Sports Med 33:502–506
Schulz MS, Steenlage ES et al (2007) Distribution of posterior tibial displacement in knees with posterior cruciate ligament tears. J Bone Joint Surg Am 89:332–338
Scott RD, Chmell MJ (2008) Balancing the posterior cruciate ligament during cruciate-retaining fixed and mobile-bearing total knee arthroplasty: description of the pull-out lift-off and slide-back tests. J Arthroplasty 23:605–608
Sekiya JK, West RV et al (2005) Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy 21:1042–1050
Shoemaker SC, Markolf KL (1986) The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. Effects of partial versus total excision. J Bone Joint Surg Am 68:71–79
Sing G, Tan JH et al (2013) Restoring the anatomical tibial slope and limb axis may maximise post-operative flexion in posterior-stabilised total knee replacements. Bone Joint J 10:1354–1358
Song EK, Park HW et al (2014) Transtibial versus tibial inlay techniques for posterior cruciate ligament reconstruction: long-term follow-up study. Am J Sports Med 42:2964–2971
Swany MR, Scott RD (1993) Posterior polyethylene wear in posterior cruciate ligament-retaining total knee arthroplasty: a case study. J Arthroplasty 8:439–446
Torzilli PA, Deng X, Warren RF (1994) The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med 22:105–112
Webb JM, Salmon LJ et al (2013) Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med 41:2800–2804
Wordeman SC, Quatman CE et al (2012) In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med 40:1673–1681
Yang JH, Yoon JR et al (2012) Second-look arthroscopic assessment of arthroscopic single-bundle posterior cruciate ligament reconstruction: comparison of mixed graft versus achilles tendon allograft. Am J Sports Med 40:2052–2060
Yoshida S, Matsui N et al (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20:777–783
Acknowledgements
We thank the Institute for Radiology and Nuclear Medicine of the Charité-University Medicine Berlin, for their continuous support and image allocation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The authors confirm that no funding was received for this study.
Ethical approval
The ethics committee of Charité-Universitaetsmedizin Berlin (EA1/003/16) approved the current study. A retrospective analysis was conducted on patients, who underwent bilateral posterior stress radiographs, within a 2-year period (May 2014–May 2016).
Rights and permissions
About this article
Cite this article
Schatka, I., Weiler, A., Jung, T.M. et al. High tibial slope correlates with increased posterior tibial translation in healthy knees. Knee Surg Sports Traumatol Arthrosc 26, 2697–2703 (2018). https://doi.org/10.1007/s00167-017-4706-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4706-4