Abstract
Purpose
To assess the role of preoperative magnetic resonance imaging (MRI) on the eligibility for arthroscopic primary anterior cruciate ligament (ACL) repair.
Methods
All patients undergoing ACL surgery between 2008 and 2017 were included. Patients underwent arthroscopic primary repair if sufficient tissue length and quality were present, or they underwent single-bundle ACL reconstruction. Preoperative MRI tear locations were graded with the modified Sherman classification: type I (>90% distal remnant length), type II (75–90%), or type III (25–75%). MRI tissue quality was graded as good, fair, or poor. Arthroscopy videos were reviewed for tissue length and quality, and final treatment.
Results
Sixty-three repair patients and 67 reconstruction patients were included. Repair patients had more often type I tears (41 vs. 4%, p < 0.001) and good tissue quality (89 vs. 12%, p < 0.001). Preoperative MRI tear location and tissue quality predicted eligibility for primary repair: 90% of all type I tears and 88% of type II tears with good tissue quality were repaired, while only 23% of type II tears with fair tissue quality, 0% of type II tears with poor tissue quality, and 14% of all type III tears could be repaired.
Conclusions
This study showed that tear location and tissue quality on preoperative MRI can predict eligibility for arthroscopic primary ACL repair. These findings may guide the orthopaedic surgeon on the preoperative assessment for arthroscopic primary repair of proximal ACL tears.
Level of evidence
Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first surgical treatment of anterior cruciate ligament (ACL) injuries consisted of open primary repair [22,23,24,25, 27, 35]. The initial short-term outcomes in the 1970s and 1980s were promising [8, 9, 16], but Feagin and Curl were the first to note a deterioration of these results at mid-term follow-up [10]. Despite many improvements, such as using non-absorbable sutures [18, 19], the results remained unpredictable at mid-term follow-up [13], and the technique was ultimately abandoned [35].
At the end of the primary repair era, in 1991, Sherman et al. [28] attempted to find an explanation for the deterioration of their results at mid-term follow-up by performing an extensive subgroup analysis. They categorized ACL tears by tear location and tissue quality and noted that better outcomes were associated with proximal (type I) tears and good tissue quality compared to mid-substance tears and poor tissue quality. Subsequently, several authors reported excellent outcomes of open primary repair when selectively treating patients with proximal tears and good tissue quality [4, 11, 37]. Despite these results, reconstructive surgery had become the standard operative treatment for all ACL injuries [35].
More recently, there has been a renewed interest in primary ACL repair using arthroscopy. DiFelice et al. were the first to report excellent outcomes of arthroscopic primary repair in patients with proximal (type I) tears and good tissue quality [7], and others confirmed these findings [1, 3, 29, 38]. These studies, similar to the study of Sherman et al. in 1991, emphasized that patient selection is critical for good results of arthroscopic primary ACL repair [1, 3, 6, 7, 29, 38]. With the usage of magnetic resonance imaging (MRI), a preoperative assessment can be made for which patients might be eligible for arthroscopic primary repair, but knowledge on the predictive role of MRI is currently lacking.
Therefore, the goal of this study was to assess the predictive role of preoperative MRI on the eligibility for arthroscopic primary repair of proximal ACL tears. The research questions were (I) what tear types were seen on preoperative MRI in patients that were eligible and not eligible for primary repair, and (II) can a preoperative assessment for arthroscopic primary ACL repair be made using MRI. The hypotheses were that (I) different tear location and tissue quality were seen on preoperative MRI in patients eligible and not eligible for primary repair, and (II) preoperative MRI could be used to predict eligibility for primary repair. Findings in this study may help the orthopaedic surgeon in making a preoperative assessment of the eligibility of primary repair and provide insight into the incidence of repairable ACL tears.
Materials and methods
A retrospective search was performed in the database of the senior author (Gregory S. DiFelice) for patients undergoing ACL surgery between April 2008 and January 2017. Patients were excluded if preoperative MRI was unavailable or of insufficient quality (n = 72), arthroscopy images and videos were unavailable or of insufficient quality (n = 12), or both were unavailable or of insufficient quality (n = 7). Furthermore, patients were excluded when time between injury and MRI was >3 months (n = 11), or time between MRI and arthroscopic surgery was >3 months (n = 18). Finally, patients were excluded for distal bony avulsion tears (n = 3), as this study focused on proximal ACL repair eligibly. A total of 130 patients met the exclusion and inclusion criteria and could be included.
Baseline characteristics of included patients
Included patients had a median age of 31 years (range 14–66 years) and BMI of 25 kg/m2 (range 18–44 kg/m2). Most patients were males (60%) and had right-sided injuries (57%). Sixty-three patients (48%) underwent arthroscopic primary repair, and 67 (52%) patients underwent reconstruction. No significant differences between the repair group and reconstruction group were found with regard to age, BMI, gender, side of injury, injury mechanism, or time from MRI to surgery, although repair patients had shorter time from injury to MRI than the reconstruction patients (5 vs. 9 days, p = 0.015) (Table 1).
Surgical techniques
During this period, all included patients preoperatively agreed to the same treatment algorithm: patients would undergo primary ACL repair if sufficient length and tissue quality were noted intraoperatively, or they would undergo single-bundle ACL reconstruction. All surgeries were performed by the senior author (Gregory S. DiFelice). Arthroscopic primary repair was performed with suture anchor fixation of both the anteromedial and posterolateral bundle, as previously described [5, 38]. An InternalBrace (Arthrex, Naples, FL, USA) was added to the repair in 62% of patients since the availability of this technique to protect the healing of the ligament, as previously described [17]. Single-bundle anatomical ACL reconstruction was performed in the reconstruction group using soft tissue autografts (21%), allografts (58%) or hybrid (autograft/allograft, 3%), or bone–patellar tendon–bone autografts (18%).
Data collection
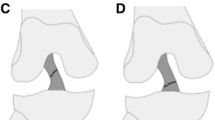
First, general data were collected, including date of birth, date of injury, date of MRI, date of surgery, age, gender, BMI, side of injury, and injury mechanism. Then, tear location and tissue quality of all patients were reviewed on preoperative MRI using the modified Sherman classification by van der List et al. [39]. On the axial, coronal, and sagittal views, the ACL was reviewed and the exact tear location was determined. Using a ruler, the length of the tibial and femoral remnants was measured and the tear location was classified as one of the following tear types (Table 2): type I proximal avulsion tear (distal remnant length >90%; Fig. 1), type II proximal tear (75–90%; Figs. 2, 3, 4), or type III mid-substance tear (middle 25–75%; Fig. 5) [21, 33, 34]. This method has been shown to have substantial interobserver (Kappa 0.670) and substantial to nearly perfect intra-observer reliability (Kappa 0.741–0.934) [39]. Tissue quality was graded as one of the following grades using the classification of Sherman et al. [28] (Table 1): good (when (nearly) all fibres were running in the same direction and the signal was homogenous; Figs. 1 and 2, fair (when part of the fibres was running in same direction and the signal was mildly heterogeneous; Figs. 3, 5), or poor tissue quality (when most fibres were running in different directions and the signal as heterogeneous; Fig. 4).
Sagittal T1 (a) and T2 (b) views show a type I proximal avulsion tear (arrows) with good tissue quality, characterized by homogeneous dark signal of fibres running in the same direction on T2 views (b). With arthroscopy, the tissue quality (asterisks) is confirmed (c), and probing of the ligament (d) shows a proximal type I tear with sufficient tissue length and an empty femoral wall (asterisks), although some scar tissue is found between the remnant and the wall (arrow). Primary repair was performed without the need of an InternalBrace
Sagittal T1 (a) and T2 (b) views show a type II proximal tear (arrows) with good tissue quality (asterisks). Arthroscopy with probing (asterisks) confirms that sufficient tissue length for primary repair is present (c). Some fibres of the posterolateral bundle are present on the femoral wall (d, arrow), which explains the discrepancy between a type II tear on MRI and a type I proximal avulsion tear on arthroscopy (asterisks). Primary repair was performed, and an InternalBrace was added
Sagittal T1 (a) and T2 (b) views show a type II proximal tear (arrows) with fair tissue quality (asterisks in a) and some fibres on the femoral wall (asterisks in b). Arthroscopy with probing (C) confirms that some fibres are present on the femoral wall (asterisks) and that most of the ligament has sufficient tissue quality (d, arrow) but is not perfect (asterisks). This ligament could be repaired and was reinforced with an InternalBrace
Sagittal T1 (a) and T2 (b) views show a type II proximal tear (arrows) with poor tissue quality (asterisks) and partially flipped ligament (arrowhead). Arthroscopy (c) confirms the proximal tear (asterisks) with poor and unrepairable tissue quality (arrow) and partially flipped ligament (arrowhead), after which ACL reconstruction (d) is performed
Next, the arthroscopic videos of all patients were reviewed, blinded for the MRI grading. Intraoperatively, the senior author recorded the assessment of tissue length and tissue quality using video in all patients. Tissue length was assessed by inspection of the tear location, probing the ligament, and tensioning the distal remnant proximally with a grasper. It was noted whether the tissue length was sufficient, or insufficient, for reinsertion onto the femoral wall. Tissue quality was assessed by inspection, by probing the ligament, and during suture passage. It was noted if the tissue quality was sufficient, or insufficient, for suture passage and tensioning towards the femoral wall. Finally, the ultimate treatment (repair or reconstruction) was assessed and noted. Institutional Review Board approval was obtained from the Hospital for Special Surgery (IRB #16006).
Statistical analysis
Statistical analysis was performed using SPSS Version 24 (SPSS Inc., Armonk, NY, USA). Independent t tests were used to compare continuous data, and Chi-square tests were used to compare nominal data. A flowchart was created to assess what percentage of patients could ultimately be repaired based on the tear location and tissue quality based on preoperative MRI. Continuous data were presented in mean ± standard deviation (SD). All tests were two-sided, and a difference of p < 0.05 was considered statistically significant. Sample size calculation revealed that 34 patients were needed in both groups in order to show a 20% difference with a power of 0.80 and a p value of 0.05.
Results
Preoperative MRI findings
In the total cohort, 22% of patients had a type I tear, 55% a type II tear, and 22% a type III tear. Most patients had good tissue quality (49%), while 28% had fair and 23% had poor tissue quality. The most commonly observed combinations of tear location and tissue quality were type I tears with good tissue quality (20%; Fig. 1), type II with good tissue quality (26%; Fig. 2), type II with fair tissue quality (17%; Fig. 3), type II with poor tissue quality (14%; Fig. 4) (Table 3).
Type I tears were more commonly seen in repair patients (41 vs. 4%, p < 0.001), and type III tears were more commonly seen in reconstruction patients (37 vs. 6%, p < 0.001), while there was no difference in incidence of type II tears in repair and reconstruction patients (52 vs. 58%, respectively, p = n.s.). In the repair group, significantly more patients had good tissue quality compared to reconstruction patients (89 vs. 12%, p < 0.001), while reconstruction patients had more often fair (43 vs. 11%, p < 0.001) or poor (44 vs. 0%, p < 0.001) tissue quality than repair patients.
Predictive role of tear location on MRI
It was noted that 90% of all MRI type I tears, 47% of MRI type II tears, and 14% of MRI type III tears were eligible for and treated with primary repair (Fig. 1). One patient with an MRI type II tear was found eligible for primary repair but was converted to reconstruction after a significant gap was noted between the femoral wall and the repaired ligament after InternalBrace tensioning (Table 3).
Predictive role of combination of tear location and tissue quality on MRI
It was noted that all patients with type I tears with good tissue quality were repaired. Of all patients with type II tears, it was noted that 88% of patients with good tissue quality, 23% of patients with fair tissue quality, and 0% of patients with poor tissue quality were repaired. Finally, it was noted that 33% (2/6) patients with type III tears with good tissue quality, 15% of patients with type III tears with fair tissue quality, and no patients with type III tears and poor tissue quality were repaired (Fig. 6).
Discussion
The main findings of this study were that preoperative MRI provided important predictive information on the eligibility and possibility of arthroscopic primary repair of the proximal ACL tears. In this cohort, 90% of type I tears and 46% of type II tears could be repaired, while only 14% of type III tears were repairable. Using tear location and tissue quality on preoperative MRI, it was noted that 93% of patients with the combination of type I or II tears and good tissue quality could be repaired. These data can significantly aid the orthopaedic surgeon in making a preoperative assessment of arthroscopic primary repair of proximal ACL tears.
Sherman et al. [28] were the first to note the role of tear location and tissue quality on the outcomes of open primary ACL repair in 1991. Following their study, several authors reported on treating of proximal (type I) tears with open primary [4, 11] or augmented repair [12, 14]. Genelin et al. [11] published the mid-term outcomes of open primary repair of proximal ACL tears and found no deterioration of outcomes at mid-term follow-up in this selective group, as opposed to several studies that noted deterioration at mid-term follow-up when performing primary repair in all tear types [10, 13, 30]. In these years, MRI was not widely available, and therefore, no historical studies assessed the role of preoperative MRI on patient selection for primary repair of proximal ACL tears [20, 31, 40]. At the time that MRI became widely available, the operative treatment of ACL injuries had already shifted towards ACL reconstruction for all tear types, and thus, there was no clinical need for the assessment of tear location and tissue quality.
In 2015, twenty years after the last original studies on primary repair, DiFelice et al. [7] renewed the interest in primary repair using arthroscopic surgery. The authors reported excellent clinical outcomes at mean 3.5-year follow-up on the first 11 patients treated by arthroscopic suture anchor repair of proximal tears, with only one early failure (9%). Subsequently, others have reported similar promising outcomes of arthroscopic primary repair in adult [1] and paediatric patients [3, 29]. With the recent resurgence of interest in ACL preservation [21, 33, 34], and especially primary ACL repair [1, 3, 7, 29, 36], and the modern availability of MRI, MRI can assist orthopaedic surgeons in making a preoperative assessment regarding the eligibility of arthroscopic primary ACL repair.
In this study, the classification system for tear location and tissue quality was partially based on recent publications on ACL preservation and primary ACL repair [21, 33, 34] and partially on the historical study by Sherman et al. [28] A recent review summarized the available treatment options of ACL preservation using the same tear-type classification, in which primary repair was discussed for type I tears, and primary repair or augmented repair for type II tears [33, 34]. Furthermore, Murray et al. recently started a clinical trial with primary ACL repair with an additional biologic scaffold in patients with type III tears (<75% of distal remnant length). In a previous study, van der List et al. [39] showed substantial interobserver reliability (Kappa 0.670) and substantial to nearly perfect intra-observer reliability (Kappa 0.741–0.934) using this classification. For tissue quality, a similar approach was used as the study by Sherman et al. [28], in which the tear types were also graded in three categories.
When only taking preoperative MRI tear location into account, it was noted that 90% of patients with type I tears could be treated with primary repair. Achtnich et al. [1] recently compared the outcomes of arthroscopic primary repair with ACL reconstruction. They included 22 patients in the repair group that all had type I tears on preoperative MRI, and performed primary repair in 21 patients (95%) that had sufficient tissue quality, which is similar to the percentage of patients with MRI type I tears that underwent primary repair in our cohort (90%). Of all patients with MRI type II tears, 46% were treated with primary repair. Taking a closer look at this 50:50 group in Table 3, it can be noted that 88% of the patients with MRI type II tears with good tissue quality could be repaired, while only 13% (5/40) of MRI type II tears with fair or poor tissue quality could be repaired. Reviewing these subgroups, the data suggest that the distal remnants of type II tears have sufficient length to be reinserted on the femoral wall, and that the possibility for primary repair mainly depends on the tissue quality. A possible reason for the finding that the distal remnant length of type II MRI tears was sufficient for primary repair is that some fibres from the posterolateral bundle are torn slightly more distal, which leaves some fibres attached on the femoral wall and this leads to a type II appearance on MRI. This tear pattern was frequently seen (Fig. 2) and suggests that MRI can underestimate the distal remnant length. The finding that 88% of type II tears with good tissue quality was repaired indicates that the tissue length of type II MRI tears is sufficient for reinsertion, and that repair of these tears mainly depends on tissue quality.
Another explanation for the finding that type II tears with good tissue quality on MRI can be repaired is that sagittal images are likely not transecting the ligament along its anatomical course, and therefore, they are not accurately displaying the location of the tear. In 22 patients, sagittal oblique and/or coronal oblique views were available, and in four of these cases, the tear type changed from type III (n = 1) or type II (n = 3) to a type I tear (example in Fig. 7). Over the last decade, some studies have assessed the role of sagittal oblique and coronal oblique imaging for ACL injuries and concluded that these can have additional value in the diagnosis for ACL tears [2, 15, 26]. Interestingly for primary repair, Kosaka et al. [15] highlighted that especially the femoral attachment can be clearly visualized with these views. The findings in this current study show that obtaining sagittal oblique and coronal oblique views have additional value for assessing eligibility for arthroscopic primary ACL repair.
Sagittal T1 view (a) shows a type II proximal tear, but sagittal oblique ACL view (b) shows a type I proximal avulsion tear. Arthroscopy (c) confirms sufficient tissue quality for repair (although not optimal), and proximal type I avulsion type tear (d) with an empty wall (arrow) and avulsed distal remnant (asterisks). Primary repair was performed, and an InternalBrace was not needed
One patient in the MRI type II group with good tissue quality was graded as eligible for primary repair but was ultimately not repaired (Fig. 6). In this patient, an internal brace was added to the primary repair after the ACL was repaired to the femoral wall with suture anchors. Because the internal brace was inserted at the proximal end of the ACL remnant and was tensioned through the ligament, this resulted in the repaired ligament pulling off the femoral wall, and this resulted in a gap forming between the ligament and the femoral wall. A decision was made to convert the patient to an ACL reconstruction, as it was expected that healing would not occur due to this gap [32].
Limitations are present in this study. First of all, the numbers in this study cannot be used for a true assessment of the tear-type incidence, as patients are referred to the practice of the senior author for primary ACL repair surgery. Studies assessing the incidence of the different tear types in a cohort of consecutive patients are necessary. Secondly, it is currently not known if the differences in tissue quality affect the outcomes of primary repair at longer-term follow-up. However, the goal of this study was to assess the correlation of tear location and tissue quality on MRI with arthroscopy. Follow-up studies are necessary if differences in outcomes exist between these different groups. Thirdly, this study is a retrospective cohort study, and the nature of this study increases the risk of bias. A similar study using a prospective design is necessary to confirm these findings. Nonetheless, the data in this study are valuable for the orthopaedic surgeon and provide information for preoperative assessment on the possibility of primary ACL repair.
The findings in this study can guide the orthopaedic surgeon in making a preoperative assessment on whether primary ACL repair can be successfully performed. Patients with tears in the proximal quarter and good tissue quality can be informed that it is likely that arthroscopic primary repair can be performed and the advantages and disadvantages of the procedure should be explained in this subgroup of patients.
Conclusion
This study showed that tear location and tissue quality on preoperative MRI could be used to predict the eligibility of primary ACL repair. More specifically, it was noted that 93% of patients with a type I or II tear (i.e. tear located at proximal 25% of ligament) and with good tissue quality were repairable. Furthermore, it was noted that sagittal and coronal oblique views provided additional information on tear location.
References
Achtnich A, Herbst E, Forkel P, Metzlaff S, Sprenker F, Imhoff AB, Petersen W (2016) Acute proximal anterior cruciate ligament tears: outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy 32:2562–2569
Barberie JE, Carson BW, Finnegan M, Wong AD (2001) Oblique sagittal view of the anterior cruciate ligament: comparison of coronal vs. axial planes as localizing sequences. J Magn Reson Imaging 14:203–206
Bigoni M, Gaddi D, Gorla M, Munegato D, Pungitore M, Piatti M, Turati M (2017) Arthroscopic anterior cruciate ligament repair for proximal anterior cruciate ligament tears in skeletally immature patients: surgical technique and preliminary results. Knee 24:40–48
Bram J, Plaschy S, Lutolf M, Leutenegger A (1994) The primary cruciate ligament suture—is the method outdated? Results in follow-up of 58 patients. Z Unfallchir Versicherungsmed 87:91–109
DiFelice GS, van der List JP (2016) Arthroscopic primary repair of proximal anterior cruciate ligament tears. Arthrosc Tech 5:E1057–E1061
DiFelice GS, van der List JP (2017) Regarding “Acute Proximal Anterior Cruciate Ligament Tears: outcomes After Arthroscopic Suture Anchor Repair Versus Anatomic Single-Bundle Reconstruction”. Arthroscopy 33:693–694
DiFelice GS, Villegas C, Taylor SA (2015) Anterior cruciate ligament preservation: early results of a novel arthroscopic technique for suture anchor primary anterior cruciate ligament repair. Arthroscopy 31:2162–2171
England RL (1976) Repair of the ligaments about the knee. Orthop Clin North Am 7:195–204
Feagin JA, Abbott HG, Rokous JR (1972) The isolated tear of the anterior cruciate ligament. J Bone Jt Surg Am 54:1340–1341
Feagin JA Jr, Curl WW (1976) Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 4:95–100
Genelin F, Trost A, Primavesi C, Knoll P (1993) Late results following proximal reinsertion of isolated ruptured ACL ligaments. Knee Surg Sports Traumatol Arthrosc 1:17–19
Grontvedt T, Engebretsen L (1995) Comparison between two techniques for surgical repair of the acutely torn anterior cruciate ligament. A prospective, randomized follow-up study of 48 patients. Scand J Med Sci Sports 5:358–363
Kaplan N, Wickiewicz TL, Warren RF (1990) Primary surgical treatment of anterior cruciate ligament ruptures. A long-term follow-up study. Am J Sports Med 18:354–358
Kdolsky R, Kwasny O, Schabus R (1993) Synthetic augmented repair of proximal ruptures of the anterior cruciate ligament. Long-term results of 66 patients. Clin Orthop Relat Res 295:183–189
Kosaka M, Nakase J, Toratani T, Ohashi Y, Kitaoka K, Yamada H, Komura K, Nakamura S, Tsuchiya H (2014) Oblique coronal and oblique sagittal MRI for diagnosis of anterior cruciate ligament tears and evaluation of anterior cruciate ligament remnant tissue. Knee 21:54–57
Liljedahl SO, Lindvall N, Wetterfors J (1965) Early diagnosis and treatment of acute ruptures of the anterior cruciate ligament; a clinical and arthrographic study of forty-eight cases. J Bone Jt Surg Am 47:1503–1513
Mackay GM, Blyth MJ, Anthony I, Hopper GP, Ribbans WJ (2015) A review of ligament augmentation with the InternalBrace: the surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int 26:239–255
Marshall JL, Warren RF, Wickiewicz TL (1982) Primary surgical treatment of anterior cruciate ligament lesions. Am J Sports Med 10:103–107
Marshall JL, Warren RF, Wickiewicz TL, Reider B (1979) The anterior cruciate ligament: a technique of repair and reconstruction. Clin Orthop Relat Res 143:97–106
Mink JH, Levy T, Crues JV 3rd (1988) Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology 167:769–774
Murray MM, Flutie BM, Kalish LA, Ecklund K, Fleming BC, Proffen BL, Micheli LJ (2016) The bridge-enhanced anterior cruciate ligament repair (BEAR) procedure: an early feasibility cohort study. Orthop J Sports Med 4:2325967116672176
O’Donoghue DH (1950) Surgical treatment of fresh injuries to the major ligaments of the knee. J Bone Jt Surg Am 32(A):721–738
O’Donoghue DH (1955) An analysis of end results of surgical treatment of major injuries to the ligaments of the knee. J Bone Jt Surg Am 37:1–13
Palmer I (1938) On the injuries to the ligaments of the knee joint. Acta Orthop Scand 53:41–56
Palmer I (2007) On the injuries to the ligaments of the knee joint: a clinical study. Clin Orthop Relat Res 454:17–22
Park HJ, Lee SY, Park NH, Ahn JH, Chung EC, Kim SJ, Cha JG (2016) Three-dimensional isotropic T2-weighted fast spin-echo (VISTA) knee MRI at 3.0 T in the evaluation of the anterior cruciate ligament injury with additional views: comparison with two-dimensional fast spin-echo T2-weighted sequences. Acta Radiol 57:1372–1379
Robson AW (1903) VI. Ruptured crucial ligaments and their repair by operation. Ann Surg 37:716–718
Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I (1991) The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med 19:243–255
Smith JO, Yasen SK, Palmer HC, Lord BR, Britton EM, Wilson AJ (2016) Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc 24:1845–1851
Straub T, Hunter RE (1988) Acute anterior cruciate ligament repair. Clin Orthop Relat Res 227:238–250
Turner DA, Prodromos CC, Petasnick JP, Clark JW (1985) Acute injury of the ligaments of the knee: magnetic resonance evaluation. Radiology 154:717–722
van der List JP, DiFelice GS (2016) Gap formation following primary repair of the anterior cruciate ligament: a biomechanical evaluation. Knee 24:243–249
van der List JP, DiFelice GS (2016) Preservation of the anterior cruciate ligament: a treatment algorithm based on tear location and tissue quality. Am J Orthop (Belle Mead NJ) 45:E393–E405
van der List JP, DiFelice GS (2016) Preservation of the anterior cruciate ligament: surgical techniques. Am J Orthop (Belle Mead NJ) 45:E406–E414
van der List JP, DiFelice GS (2017) Primary repair of the anterior cruciate ligament: a paradigm shift. Surgeon 15:161–168
van der List JP, DiFelice GS (2017) Range of motion and complications following primary repair versus reconstruction of the anterior cruciate ligament. Knee. doi:10.1016/j.knee.2017.04.007
van der List JP, DiFelice GS (2017) Role of tear location on outcomes of open primary repair of the anterior cruciate ligament: a systematic review of historical studies. Knee. doi:10.1016/j.knee.2017.05.009
van der List JP, DiFelice GS (2017) Successful arthroscopic primary repair of a chronic anterior cruciate ligament tear 11 years following injury. HSS J 13:90–95
van der List JP, Mintz DN, DiFelice GS (2017) The location of anterior cruciate ligament tears: a prevalence study using magnetic resonance imaging. Orthop J Sports Med 5:2325967117709966
Widhalm HK, Surer L, Kurapati N, Guglielmino C, Irrgang JJ, Fu FH (2016) Tibial ACL insertion site length: correlation between preoperative MRI and intra-operative measurements. Knee Surg Sports Traumatol Arthrosc 24:2787–2793
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jelle P. van der List declares he has no conflict of interest. Gregory S. DiFelice is a paid consultant for Arthrex (Naples, FL).
Funding
No funding has been received for this study.
Ethical approval
IRB approval obtained (Hospital for Special Surgery IRB number 16006).
Informed consent
Informed consent was obtained for all patients in the study.
Rights and permissions
About this article
Cite this article
van der List, J.P., DiFelice, G.S. Preoperative magnetic resonance imaging predicts eligibility for arthroscopic primary anterior cruciate ligament repair. Knee Surg Sports Traumatol Arthrosc 26, 660–671 (2018). https://doi.org/10.1007/s00167-017-4646-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4646-z