Abstract
Purpose
The purpose of this study was to investigate if the type of approach [medial parapatellar approach (MPA) versus lateral parapatellar approach with tibial tubercle osteotomy (LPA)] influences rotation of femoral and/or tibial component and leg axis in total knee arthroplasty (TKA). It was the hypothesis that MPA leads to an internally rotated tibial TKA component.
Methods
This study included 200 consecutive patients in whom TKA was performed using either a parapatellar medial (n = 162, MPA) or parapatellar lateral approach with tibial tubercle osteotomy (n = 38, LPA). All patients underwent clinical follow-up, standardized radiographs and computed radiography (CT). TKA components’ position and the whole leg axis were assessed on 3D reconstructed CT scans (sagittal, coronal and rotational). Mean values of TKA component position and the whole leg alignment of both groups were compared using a t test. The tibial component was graded as internally rotated (<3° of external rotation (ER)), neutral rotation (equal or between 3° and 6° of ER) and externally rotated (>6° ER). The femoral component was graded as internally rotated [>3° of internal rotation (IR)], neutral rotation (equal or between −3° IR and 3° of ER) and externally rotated (>3° ER).
Results
There was no significant difference in terms of whole leg axis after TKA between both groups (MPA: 0.2° valgus ± 3.4; LPA: 0.0° valgus ± 3.5). Means of tibial component rotation were 2.7° ER ± 6.1 (MPA) and 7.6° ER ± 5.4 (LPA). Patients of group LPA presented a significantly less internally rotated (LPA: 18.4%; MPA: 48.8%) and more externally rotated (LPA: 52.6%; MPA: 22.8%) tibial component (p < 0.001). No significant differences were seen for the femoral component position, tibial valgus/varus and tibial slope.
Conclusion
The type of approach (medial versus lateral) significantly influenced tibial TKA component rotation. It appears that a MPA tends to internally rotate the tibial TKA component and a LPA tends to externally rotate the tibial TKA. The anterior cortex should not be used as landmark for tibial TKA component placement when using the lateral approach with tibial tubercle osteotomy.
Level of Evidence
Retrospective comparative study, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tibial and femoral component rotations are considered as a key factor for successful outcomes after total knee arthroplasty (TKA) [11, 39]. Suboptimal rotational TKA position severely alters knee kinematics leading to patellar maltracking and overloading [1, 2, 26], flexion instability [2], synovial and soft tissue impingement [2], accelerated inlay wear [26, 40] or stiffness [36]. Typically, internal rotation of the femoral TKA component results in an increased lateral flexion gap and causes overloading on the lateral patellar facet [5, 23]. An externally rotated femoral component leads to a medial lift-off in flexion [13]. An internally rotated tibial component is associated with medial compartment pain and limited knee flexion [5, 23]. Combined internal rotation of the femoral and tibial component is reported to increase the risk of patellar dislocation and anterior knee pain [4, 6, 8].
There is a variety of different TKA approaches the surgeon can choose from. Among those, the medial parapatellar approach (MPA) and the lateral parapatellar approach with tibial tubercle osteotomy (LPA) are commonly used for varus or valgus knees. The MPA is most frequently used, in both varus and valgus knees as it is less demanding [20, 31]. However, it violates the vascular supply of the patella and some authors suggest using a lateral subvastus approach combined with a tibial tubercle osteotomy particularly in valgus-deformed knees [3, 19]. The main risk associated with MPA in valgus knees is an excessive release of medial collateral ligament and other medial structures. Furthermore, it provides a poorer access to the posterolateral corner, limiting the release of lateral soft tissues under direct view. On the other side, a LPA allows a better visualization of lateral soft tissue structures. The lateral release, which is a necessary part in most valgus knees, is already included into the approach [10, 34, 35]. Following LPA, a better patellar vascularization, improved quadriceps strength and a better patellar tracking have been reported [12, 24]. However, this approach is more technical demanding, less familiar to most of the surgeons and causes a higher rate of complications [16, 22, 41]. In addition, the surgery time is longer than with MPA [16].
The purpose of this study was to investigate whether and how the choice of the approach (MPA or LPA) in primary TKA affects the rotation of the femoral and tibial TKA components and the entire leg axis. The hypothesis was that there is a tendency to internally rotate the tibial component in MPA and to externally rotate the tibial component in LPA.
Materials and methods
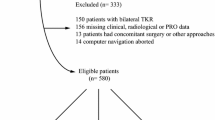
A consecutive series of 200 patients who underwent a computed tomography (CT) after primary TKA from 2013 to 2016 as clinical routine follow-up or because of knee pain in a university-affiliated hospital were prospectively collected and retrospectively analysed. Indication for TKA was end-stage osteoarthritis. A team of two senior surgeons performed the surgeries using either cruciate retaining or posterior stabilized TKA. The decision to perform a CR or PS TKA was based on the integrity of the posterior cruciate ligament and was done independently from alignment (varus versus valgus knees). The tibial TKA components were all of symmetrical shape.
The landmarks used for femoral and tibial TKA rotation were surgical transepicondylar axis, anteroposterior trochlear line, posterior femoral condyle line and medial third of the tibial tubercle, second metatarsal, Akagi’s line, anterior tibial marginal line, respectively. Femoral rotation for each TKA was based on a 3° external rotation with regard to the posterior condylar line and parallel to the anatomical transepicondylar axis.
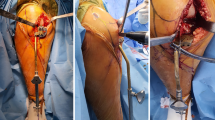
Patients were divided into two groups with regard to the used surgical approach. Group LPA included thirty-eight patients (male/female = 14:24; 67.5 ± 10.4 years), who underwent TKA using a lateral parapatellar approach combined with tibial tubercle osteotomy. The lateral parapatellar approach with tibial tubercle was done in standardized Bruderholz technique. A lateral curved skin incision from the distal lateral thigh to the lateral tibia was performed towards the tibial tubercle. The subcutaneous layer was bluntly prepared, and the iliotibial tract as well as the anterior tibial muscle fascia was incised. Then, a lateral subvastus approach to the knee joint and a tibial tubercle osteotomy was performed.
Group MPA included one-hundred sixty-two patients (male/female = 56:106; 67.2 ± 9.8 years) who underwent TKA using a medial parapatellar approach.
All patients underwent standardized clinical and radiological examination including radiographs and CT scans according to a previously published protocol [32]. Data were processed by interactive reconstruction, and images were displayed in axial, coronal and sagittal planes. Femoral and tibial TKA position was assessed on 3D reconstructed CT as previously published [32]. Measurements were taken by a musculoskeletal radiologist with more than ten-year experience using a customized analysis software (OrthoExpert©, London, UK) (Fig. 1). A good-to-excellent inter- and intra-observer reliability for the measurements of TKA position on 3D reconstructed CT was shown [15].
For the femoral component, the external (+) and internal (−) rotation on the transversal plane was measured as an angle between the surgical femoral transepicondylar axis and a tangent line of the femoral component surface at the internal part of the anterior flange. Varus (+) and valgus (−) inclination on the coronal plane was measured as an angle between the perpendicular line to the femoral mechanical axis and a distal tangent line on the distal femoral condyles. Flexion (+) and extension (−) on the sagittal plane was measured as an angle between the femoral mechanical axis and a tangent line to the internal flat side of the anterior flange.
For the tibial component, external (+) and internal (−) component rotation on the transversal plane was measured as an angle between the tangent line to the posterior tibial component and the tibial posterior condylar axis. Varus (+) and valgus (−) inclination on the coronal plane was measured as an angle between a perpendicular line to the tibial mechanical axis and a line parallel to the tibial TKA component. Posterior (+) and anterior (−) slope on the sagittal plane was measured as an angle between a perpendicular line to the tibial mechanical axis and a tangent line put on the tibial TKA component. Varus (+) and valgus (−) alignment of the whole leg on the coronal plane was measured as the hip-knee-ankle angle.
Femoral TKA component rotation was graded as internally rotated for measured angles lower than −3°, neutrally rotated for angles between −3° and +3° and externally rotated for angles greater than +3°. Tibial TKA component rotation was graded as internally rotated for measured angles lower than +3°, neutrally rotated for angles between +3 and +6° and externally rotated for angles greater than +6°. This grading is based on our previous experience with those landmarks and measurement protocol.
Ethical approval was obtained from the Ethikkommission Nordwest- und Zentralschweiz (EKNZ, Basel). All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Statistical analysis
All data were analysed by an independent professional statistician using IBM SPSS version 22.0 (Armonk, NY: IBM Corp.). Continuous data were described as mean and standard deviation (SD) while categorical data were presented as frequencies and proportions. For basic comparison of groups in terms of age a t test and of gender and side a Chi-square test were used. For comparison between groups in terms of TKA component orientation and whole leg axis a t test was used. The difference of classified rotations between the groups was tested with Chi-square tests (Table 1). A two-tailed p < 0.05 was considered statistical significant. Post hoc power analysis was performed with G*Power version 3.1.9 (University of Düsseldorf, Germany). A post hoc power analysis of the main result (external vs. internal rotation in the tibia) showed a large effect size of 0.84 which corresponds to a power (1-beta) of 99.6%.
Results
The two groups did not differ with regard to the age (n.s.), gender (n.s.) and knee side (n.s.). Means, standard deviations and p values of TKA component position of both groups are presented in Table 2. A significant difference between the two groups was seen for the rotation of the tibial component on the transversal plane (p < 0.001) (Table 2). No significant differences were seen for the position of the tibial and femoral component on others planes (n.s.) (Table 2). The graded measurements of femoral and tibial TKA component are presented in Tables 3 and 4.
The femorotibial axis was almost neutral in both groups (group MPA: −0.16 ± 3.368; group LPA: 0.04 ± 3.458) without a significant difference (n.s.) (Table 2).
The percentages of neutrally orientated tibial TKA components were similar in both groups (LPA: 28.9%; MPA: 28.4%). In group LPA, more than twofold externally (p < 0.001) and less than half internally (p < 0.001) rotated tibial TKA components were found. In group LPA, almost 15% more neutrally orientated femoral components (LPA: 71.1%; MPA: 55.6%) (n.s.) and almost 15% less internally rotated tibial femoral components (LPA: 28.9%; MPA: 43.8%) were seen when compared to group MPA (n.s.) (Table 3).
Discussion
The most important result of the present study was that the type of approach significantly affected the resulting tibial component rotation after TKA. The tibial component was more externally rotated in group LPA and more internally rotated in group MPA; hence, the starting hypothesis of the authors was confirmed.
The findings are in agreement with Passeron et al. who, using the self-adjustment method for the tibial component positioning, reported similar results in a small-sized prospective study using measurement on transverse CT slices (2D). They found that LPA led to significantly more external rotation in tibial TKA components [28]. However, in here the Berger method was used, which is considered as less reliable than measurements on 3D reconstructed CT [18, 32].
MPA and LPA provide the surgeon with less or more access to the lateral corner structures. Within the LPA, a lateral release is done leading to an internal rotation of the tibia during TKA surgery. In contrast, MPA includes a medial approach and medial release, which comes along with an externally rotated tibia. However, this tibial position during TKA surgery has a significant influence on the surgeon’s perspective and explains finding of the present study. In addition, with a tibial tubercle osteotomy done in LPA, also the local bony anatomy of the proximal tibia changes, which might be another reason for a tendency to externally rotate the tibial TKA component. In contrast, the lateral eversion/subluxation of the patella performed in MPA limits the direct view on the lateral corner structures [21, 29, 30, 33, 34]. The present study did not take into account the postoperative clinical outcomes. While an internally rotated tibial component is known to be a major cause of pain, reduced knee flexion and higher rates of revision TKA [4, 5, 23, 25, 27], an externally rotated tibial component seems to improve the patellofemoral tracking [28]. Hirschmann et al. compared the clinical outcomes at a two-year follow-up of 143 patients who undergone TKA with LPA (n = 76) and MPA (n = 67). The LPA group presented higher scores at the visual analogue scale (VAS) and at knee society score (KSS), more patients’ satisfaction and increased pain-free walking distance [16]. However, in this group of patients, a higher TKA revision rate, due to a secondary proximal migration of the tibial tubercle was seen (LPA: 4%; MPA: 1.5%) [16]. Teng et al. in a meta-analysis collected 940 primary TKAs (LPA: 482; MPA: 458) and found better KSS scores in the LPA group at 4-, 6-week and 1-year follow-up [37]. The ROM at 1-year follow-up was similar in both groups [37]. Matsueda et al. found no differences between LPA and MPA at 6-month follow-up with regard to the KSS and ROM; however, a better patellar tracking in the LPA group was reported [24].
Terashima et al. [38] showed that externally rotated femoral components lead to better patellofemoral tracking which might be explained by lower patellofemoral contact stress. This present study showed a higher rate of neutrally orientated and a smaller rate of internally rotated femoral components in the LPA group. However, the finding was not significantly different to the MPA group.
Another finding of the present study was that there was no other significant difference in terms of TKA component position, except tibial component rotation. Also, there was no significant difference in terms of mechanical leg axis, which was almost neutral in all patients. Restoration of a neutral leg axis is one of the most important factors for a successful TKA [9, 11]. Medial collapse and ligament instability have been reported to be cause of TKA failure, respectively, in valgus and varus malaligned legs [7, 14]. In accordance with the present study, other also did not find any significant difference between patients who underwent TKA using LPA or MPA [16, 22].
The study bears a considerable number of limitations. This is a retrospective analysis of prospectively collected data. The retrospective nature bears a selection bias, which is, however, limited due the prospective data collection. The sample size is well balanced for the question to be answered.
The postoperative functional scores have not been considered. The choice of only one observer to assess the TKA component position and leg axis on CT images could be criticized; however, Figueroa et al. [15] reported a good inter- and intra-observer reliability for the CT on this type of measurements. Furthermore, 3D-CT reconstructed images have been used for the present study and these have been assessed as more reliable than 2D-CT images for TKA component measurements [17, 18, 32].
Clinically, all orthopaedic surgeons should be aware of the fact that MPA has the tendency to result in internally rotated tibial TKA components. This can only be avoided if a combination of landmarks is used for determination of TKA position.
Conclusion
The different knee exposure in MPA or LPA affects tibial TKA component rotation differently; MPA led to internal rotation and LPA external rotation. A meticulous selection and combination of tibial landmarks are recommended to overcome these tendencies.
Abbreviations
- TKA:
-
Total knee arthroplasty
- LPA:
-
Lateral parapatellar subvastus approach with tibial tubercle osteotomy
- MPA:
-
Medial parapatellar approach
- CT:
-
Computed tomography
- ER:
-
External rotation
- IR:
-
Internal rotation
- EKNZ:
-
Ethikkommission Nordwest- und Zentralschweiz
- VAS:
-
Visual analogue scale
- KSS:
-
Knee society score
References
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Apostolopoulos AP, Nikolopoulos DD, Polyzois I, Nakos A, Liarokapis S, Stefanakis G, Michos IV (2010) Total knee arthroplasty in severe valgus deformity: interest of combining a lateral approach with a tibial tubercle osteotomy. Orthop Traumatol Surg Res 96(7):777–784
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Bédard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469(8):2346–2355
Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B, Blyth M, McLean A (2012) Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee 21(1):272–277
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Boonen B, Schotanus MG, Kerens B, van der Weegen W, van Drumpt RA, Kort NP (2013) Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: a multicentre, randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 21(10):2206–2212
Buechel FF (1990) A sequential three-step lateral release for correcting fixed valgus knee deformities during total knee arthroplasty. Clin Orthop Relat Res 260:170–175
Choong PF, Dowsey MM, Stoney JD (2009) Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplast 24(4):560–569
Cila E, Güzel V, Ozalay M, Tan J, Simşek SA, Kanatli U, Oztürk A (2002) Subvastus versus medial parapatellar approach in total knee arthroplasty. Arch Orthop Trauma Surg 122(2):65–68
Dennis DA, Komistek RD, Walker SA, Cheal EJ, Stiehl JB (2001) Femoral condylar lift-off in vivo in total knee arthroplasty. J Bone Jt Surg Br 83(1):33–39
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplast 24(6 Suppl):39–43
Figueroa J, Guarachi JP, Matas J, Arnander M, Orrego M (2016) Is computed tomography an accurate and reliable method for measuring total knee arthroplasty component rotation? Int Orthop 40(4):709–714
Hirschmann MT, Hoffmann M, Krause R, Jenabzadeh RA, Arnold MP, Friederich NF (2010) Anterolateral approach with tibial tubercle osteotomy versus standard medial approach for primary total knee arthroplasty: does it matter? BMC Musculoskelet Disord 11:167
Hirschmann MT, Iranpour F, Konala P, Kerner A, Rasch H, Cobb JP, Friederich NF (2010) A novel standardized algorithm for evaluating patients with painful total knee arthroplasty using combined single photon emission tomography and conventional computerized tomography. Knee Surg Sports Traumatol Arthrosc 18(7):939–944
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Jt Surg Br 93(5):629–633
Kayler DE, Lyttle D (1988) Surgical interruption of patellar blood supply by total knee arthroplasty. Clin Orthop Relat Res 229:221–227
Keblish PA (1991) The lateral approach to the valgus knee. Surgical technique and analysis of 53 cases with over 2-year follow-up evaluation. Clin Orthop Relat Res 271:52–62
Khan H, Grob K, Milne LP, Kuster MS (2016) Tibial tubercle osteotomy to improve exposure in complex knee fractures: a cadaveric study and case series. Injury 47(10):2331–2338
Langen S, Gaber S, Zdravkovic V, Giesinger K, Jost B, Behrend H (2016) Lateral subvastus approach with tibial tubercle osteotomy for primary total knee arthroplasty: clinical outcome and complications compared to medial parapatellar approach. Eur J Orthop Surg Traumatol 26(2):215–222
Maderbacher G, Baier C, Springorum HR, Maderbacher H, Birkenbach AM, Benditz A, Grifka J, Keshmiri A (2016) Impact of axial component alignment in total knee arthroplasty on lower limb rotational alignment: an in vitro study. J Knee Surg. doi:10.1055/s-0036-1592148
Matsueda M, Gustilo RB (2000) Subvastus and medial parapatellar approaches in total knee arthroplasty. Clin Orthop Relat Res 371:161–168
Meccia B, Komistek RD, Mahfouz M, Dennis D (2014) Abnormal axial rotations in TKA contribute to reduced weightbearing flexion. Clin Orthop Relat Res 471(1):248–253
Nagamine R, Whiteside LA, White SE, McCarthy DS (1994) Patellar tracking after total knee arthroplasty. The effect of tibial tray malrotation and articular surface configuration. Clin Orthop Relat Res 304:262–271
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Jt Surg Br 92(9):1238–1244
Passeron D, Gaudota F, Boisrenoulta P, Falletb L, Beaufilsa P (2009) Does lateral versus medial exposure influence total knee tibial component final external rotation? A CT based study. Orthop Traumatol Surg Res 95(6):420–424
Punwar SA, Fick DP, Khan RJ (2016) Tibial tubercle osteotomy in revision knee arthroplasty. J Arthroplast. doi:10.1016/j.arth.2016.08.029
Radulescu R, Badila A, Nutiu O, Japie I, Terinte S, Radulescu D, Manolescub R (2013) Extended exposure in difficult total knee arthroplasty using tibial tubercle osteotomy. Maedica (Buchar) 8(4):380–383
Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S (2005) Total knee arthroplasty for severe valgus deformity. J Bone Jt Surg Am 87(Suppl 1(Pt 2)):271–284
Rasch H, Falkowski AL, Forrer F, Henckel J, Hirschmann MT (2013) 4D-SPECT/CT in orthopaedics: a new method of combined quantitative volumetric 3D analysis of SPECT/CT tracer uptake and component position measurements in patients after total knee arthroplasty. Skelet Radiol 42(9):1215–1223
Sanna M, Sanna C, Caputo F, Piu G, Salvi M (2013) Surgical approaches in total knee arthroplasty. Joints 1(2):34–44
Segur JM, Vilchez-Cavazos F, Martinez-Pastor JC, Macule F, Suso S, Acosta-Olivo C (2014) Tibial tubercle osteotomy in septic revision total knee arthroplasty. Arch Orthop Trauma Surg 134(9):1311–1315
Sekiya H, Takatoku K, Takada H, Sugimoto N, Hoshino Y (2014) Lateral approach is advantageous in total knee arthroplasty for valgus deformed knee. Eur J Orthop Surg Traumatol 24(1):111–115
Su EP, Su SL, Della Valle AG (2010) Stiffness after TKR: how to avoid repeat surgery. Orthopedics 33(9):658
Teng Y, Du W, Jiang J, Gao X, Pan S, Wang J, An L, Ma J, Xia Y (2012) Subvastus versus medial parapatellar approach in total knee arthroplasty: meta-analysis. Orthopedics 35(12):e1722–e1731
Terashima T, Onodera T, Sawaguchi N, Kasahara Y, Majima T (2015) External rotation of the femoral component decreases patellofemoral contact stress in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(11):3266–3272
Valkering KP, Breugem SJ, van den Bekerom MP, Tuinebreijer WE, van Geenen RC (2015) Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop 86(4):432–439
Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG (1994) Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 299:31–43
Zonnenberg CB, Lisowski LA, van den Bekerom MP, Nolte PA (2010) Tuberositas osteotomy for total knee arthroplasty: a review of the literature. J Knee Surg 23(3):121–129
Author information
Authors and Affiliations
Contributions
Author contributions
FFS collected and analysed the data and prepared the manuscript. FA carried out the statistical analysis and helped drafting the manuscript. MTH designed the study, helped with the analysis of data and prepared and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
There was no financial conflict of interest with regards to this study.
Ethical approval
Ethical approval was obtained from the Ethikkommission Nordwest- und Zentralschweiz (EKNZ, Basel). All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Schiapparelli, FF., Amsler, F. & Hirschmann, M.T. Medial parapatellar approach leads to internal rotation of tibial component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26, 1564–1570 (2018). https://doi.org/10.1007/s00167-017-4586-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4586-7