Abstract
Purpose
Atraumatic microinstability of the hip is felt to be a cause of intra-articular pathology, particularly tears of the anterior labrum. The purpose of this study is to evaluate a consecutive series of patients with atraumatic hip microinstability that resulted in anterior labral and cartilage pathology, treated with hip arthroscopy and capsular plication without any associated bony procedures.
Methods
Thirty-two patients underwent hip arthroscopy and suture capsular plication for the treatment of hip instability without concomitant bony resections of the acetabulum or proximal femur between November 2009 and November 2012 and were followed for a minimum of 12 months. Patients were clinically evaluated preoperatively and again at 3, 6, 12, 24, and 36 months postoperatively with the modified Harris hip score (mHHS) and iHOT score in some patients (as this was introduced late in the study). Comparison was made evaluating centre-edge angle, Tönnis angle, physical examination findings, and demographics on outcome.
Results
There was significant improvement in the mean mHHS from 67 (SD = 8.7) to 97 (SD = 4.7) and iHOT score from 41 (SD = 18.3) to 85 (SD = 10.1) at final follow-up. When comparing patients with mild hip dysplasia to patients without hip dysplasia, there was no significant difference in clinical outcome at any point in follow-up. There was no significant association between patient age, duration of preoperative symptoms, previous ipsilateral hip arthroscopy, nature of onset of symptoms, centre-edge angle, Tönnis angle, or preoperative physical examination findings with clinical outcome at final follow-up.
Conclusion
Isolated arthroscopic suture capsular plication performed for the treatment of hip instability resulted in improved patient pain and function at a minimum of 1-year follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hip instability is generally defined as extraphysiologic hip motion that causes pain with or without symptoms of hip joint unsteadiness [22]. The diagnosis and treatment of gross hip instability as a result of trauma or iatrogenic injury has been well described. Symptomatic hip microinstability, however, is poorly defined and less dramatic in clinical presentation. Hip microinstability has only recently emerged as a significant cause of pain and disability in younger patients [4, 22].
Treatment options for symptomatic hip microinstability consist of strengthening of the dynamic stabilizers of the hip with physical therapy and surgically addressing the underlying structural abnormalities. In the absence of significant abnormal bony anatomy, however, treatment options focus on the hip capsuloligamentous complex. Several techniques have been described to shrink or reduce hip capsular volume in the treatment of hip microinstability [9, 10, 18, 21]. However, there are few reports on the clinical results of these surgical interventions, especially in the context of hip arthroscopy.
The purpose of this study is to report the results of a consecutive series of patients with symptomatic atraumatic hip microinstability that resulted in anterior or lateral labrum and chondral pathology, treated with hip arthroscopy and suture capsular plication without any associated bony procedures. With clinical improvement, this may help confirm that hip microinstability is a real clinical entity, as there is no current objective measure of joint laxity. The hypothesis is that patients undergoing arthroscopic hip capsular plication for the treatment of hip microinstability would experience clinical improvement with few complications and a low reoperation rate.
Materials and methods
All hip arthroscopy procedures performed by the senior author (MRS) between 2009 and 2013 were retrospectively reviewed. The explicit inclusion criteria were an age of less than 50 years old, diagnosis of hip instability based on preoperative and intra-operative findings, symptoms refractory to non-operative management, clinical follow-up of ≥12 months, pain relief >50% with image-guided intra-articular local anaesthetic injection, and performance of arthroscopic suture capsular plication. The explicit exclusion criteria were an age of 50 years or more, presence of Tönnis grade ≥2 degenerative changes, severe hip dysplasia (CEA < 18°), history of Legg–Calve–Perthes disease, clinical follow-up of <12 months, associated acetabular or proximal femoral fracture, and performance of any arthroscopic osseous resections including resection of a femoral cam lesion (cheilectomy) and/or resection of an acetabular pincer lesion (acetabuloplasty). The study was approved by the institutional review board (Stanford University, protocol approval number 28502).
All patients were prospectively assessed using the modified Harris hip score (mHHS) [7, 13, 14]. A score was obtained preoperatively and then reassessed postoperatively at 3, 6, 12, 24, and 36 months. Additionally, eight patients in the study were prospectively assessed using the iHOT score, as the final version of this score was introduced late in the study [16].
Clinical evaluation
The diagnosis of hip instability was based on patient history and physical examination. Special attention was given to a history of pain or apprehension brought on by activities requiring repetitive hip rotation and axial loading. Duration of symptoms before arthroscopic surgery was recorded as well as any history of previous ipsilateral hip surgery. The onset of symptoms was noted and defined as follows: “traumatic” involved a major injury such as violent impact or simple hip dislocation; “acute” signified a twisting episode or other well-defined event precipitating the acute onset of symptoms; and “insidious” meant absence of injury or precipitating event but a gradual onset of worsening symptoms [6].
Physical examination of the hip included routine range of motion and strength testing. Hip internal and external rotation was measured in the supine position with the hip at 90° of flexion. The FABERE test, assessing the distance between the lateral knee and table with the patient’s leg in a figure-of-4 position, was recorded. The presence of generalized ligamentous laxity/hypermobility was assessed using the Beighton criteria [2]. The anterior impingement and labral stress tests were used to detect the presence of intra-articular pathology, such as a labral tear [17]. In addition, two specific provocative manoeuvres were performed to detect for hip instability—the log roll test and anterior apprehension test. The log roll test is performed with the patient in the supine position [22]. External rotation greater than the contralateral side is a positive test. The anterior apprehension test (hyper-extension-external rotation test) is performed with the patient in the supine position with the buttocks just over the edge of the table—the affected lower extremity is then extended and externally rotated [22]. A positive test reproduces pain and/or apprehension.
Radiographs included supine anteroposterior pelvis and cross-table lateral views. All radiographs were assessed by the senior author on a PACS system (McKesson Horizon Rad Station 11.6, San Francisco, CA). The presence of acetabular dysplasia was evaluated based on the lateral centre-edge angle (CEA) and the Tönnis angle. CEA > 25° was defined as normal, CEA 18°–25° was defined as dysplastic, and CEA < 18° was defined as severely dysplastic. A Tönnis angle ≤10° was defined as normal, and an angle >10° was defined as dysplastic. Radiographs were also evaluated for degenerative changes, and patients with Tönnis grade 2 changes or greater were excluded from the study [24]. All patients underwent a magnetic resonance arthrogram (MRA) preoperatively for assessment of labral and chondral damage. An intra-articular injection of local anaesthetic, either with the MRA or in isolation, was performed preoperatively in all patients to confirm an intra-articular source of symptoms.
Surgical technique
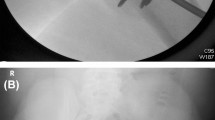
Hip arthroscopy was performed with the patient in the supine position on a traction table with a well-padded perineal postlateralized to the operative hip. “Fine traction” was applied by the screw distraction mechanism of the traction table. The number of “turns” needed to distract the joint 7–10 mm was noted, with less than 10 “turns” suggesting hip instability and ligamentous laxity. It should be noted that some patients had a few millimetres of joint opening before “fine traction” was applied, and this also was strongly suggestive of hip instability and ligamentous laxity (Fig. 1). Access to the joint was gained through a standard anterolateral portal placed under fluoroscopic visualization, followed by mid-anterior and posterolateral portals placed under direct visualization. A capsulotomy between portals was not performed in an attempt to maintain the integrity of the hip capsular ligaments [23].
Intra-operative fluoroscopic image of a patient where just manual “gross traction” (using body weight, but no “fine traction” applied using fracture table) resulted in femoral head distraction of a few millimetres. This is consistent with hip instability. This patient had a capsular plication and labral repair, with complete resolution of her symptoms
The specifics of the surgical procedure were dictated by the pathology encountered. No bony resections, either of the acetabulum (acetabuloplasty/rim resection) or of the proximal femur (cheilectomy/femoroplasty), were performed on any patient in the study.
Capsular plication was performed in the region of the capsule that does not have ligamentous thickenings [23]. This was accomplished with a suture shuttling technique meant to tighten the hip in a manner analogous to a rotator interval closure in the shoulder. After traction was released, a proximal anterolateral portal was created 3–4 cm proximal to the anterolateral portal. A 30° arthroscopic lens was placed in the anterolateral portal, directly against the capsule at the femoral head–neck junction. A shaver was then placed in the proximal anterolateral portal and triangulated to the tip of the arthroscope, using fluoroscopy to assist with localization. An anterolateral partial capsulectomy approximately 8–10 mm in width (proximal–distal) and 15 mm in length (anterior–posterior) was then performed with a shaver in the “bare area” between the iliofemoral and ischiofemoral ligaments until the femoral head–neck region was clearly visualized (Fig. 2) [23]. A suture shuttling technique was then utilized to perform the capsulorrhaphy, essentially closing the ligament “bare area” with 3 to 5 sutures depending on the size of the defect (Figs. 3, 4). Postoperatively, patients remained foot flat 20 lb weight bearing in an abduction brace with range of motion limited from 0° to 90° of hip flexion for a period of 2 weeks.
Statistical analysis
Results at baseline and postoperatively were compared using a paired t test. Significance was set at p < 0.05. All analyses were conducted in SPSS (version 20, IBM Inc., Armonk, NY, USA).
Results
Thirty-two patients (25%) underwent hip arthroscopy and suture capsular plication without any associated bony resection by the senior author between November 2009 and November 2012. One patient was lost to follow-up, leaving 31 patients (94%) available for analysis. Median follow-up was 20 months (range 12–46 months).
The study group was entirely female (100%) with a median age of 27 years (range 14–49 years). Eleven patients (35%) in the study group were collegiate or professional athletes. The median duration of symptoms before arthroscopy was 24 months (range 2–120 months). The onset of symptoms was traumatic in two patients (7%), acute in 11 cases (35%), and insidious in 18 cases (58%). Six patients (19%) had undergone previous ipsilateral hip arthroscopy at a median of 16 months before initial presentation (range 12–20). None of these six patients (0%) had undergone a previous capsular plication procedure. On physical examination, 15 patients (48%) demonstrated a Beighton score of ≥1 during preoperative clinical evaluation, and ten patients (29%) demonstrated a score of ≥2. No patients had a diagnosis of an underlying connective tissue disorder. The log roll test was positive in 16 patients (52%), and the anterior apprehension test was positive in 24 patients (77%). On radiographic evaluation, the median CEA was 28° (range 18°–37°). Twenty-two patients (71%) were categorized as non-dysplastic and nine patients (29%) were categorized as dysplastic. No patients had severe dysplasia (CEA < 18°).
Capsular plication was performed in all 31 patients (100%). Labral repair was performed in 19 patients (61%), and partial labrectomy was performed in seven patients (23%). Chondroplasty was performed in 25 patients (81%), ligamentum teres debridement was performed in 28 patients (90%), microfracture was performed in five patients (16%), and loose body removal was performed in four patients (13%).
The median preoperative mHHS was 67 (range 43–81), and the median postoperative mHHS at final follow-up was 97 (range 79–100) (p < 0.001). The preoperative iHOT score was available for eight patients, as it was introduced late in the study. The median preoperative iHOT score was 41 (range 21–73), and the median postoperative iHOT score in these eight patients at final follow-up was 85 (range 73–97) (p < 0.001).
Based on the radiographic CEA, there was no significant difference in the mean mHHS at any point in follow-up (3-, 6-, 12-month, and final follow-up) between patients with hip dysplasia (nine patients, 29%) and those without dysplasia (22 patients, 71%). Based on the radiographic Tönnis angle, there was no significant difference in the mean mHHS at any point in follow-up (3-, 6-, 12-month, and final follow-up) between patients with hip dysplasia (14 patients, 45%) and those without dysplasia (17 patients, 55%).
There was no significant difference in the mean mHHS at any point in follow-up (3-, 6-, 12-month, and final follow-up) between patients treated with labral repair (19 patients, 61%) and patients treated with partial labrectomy (seven patients, 23%).
There was no statistically significant association between patient age, duration of preoperative symptoms, previous ipsilateral hip arthroscopy, nature of onset of symptoms, CEA, Tönnis angle, or preoperative physical examination findings with clinical outcome based on mHHS or iHOT score at final follow-up. Nine of the 11 patients (82%) who were collegiate or professional athletes returned to their previous sport at the preoperative level of competition.
There was also no significant difference between preoperative and postoperative hip range of motion. Median preoperative hip flexion was 118° (range 90°–145°), and mean postoperative hip flexion was 122° (range 105°–145°) (n.s.). Median preoperative hip internal rotation was 40° (range 5°–70°), and median postoperative hip internal rotation was 37° (range 10°–70°) (n.s.). Median preoperative hip external rotation was 62° (range 30°–90°), and median postoperative hip external rotation was 60° (range 30°–90°) (n.s.).
There were no perioperative complications. One patient underwent revision hip arthroscopy at 14 months postoperatively for treatment of symptomatic hip stiffness after an extensive course of physical therapy. At the time of arthroscopy, she was noted to have anterior capsular adhesions with loss of the normal cleft between the labrum and hip capsule. This was treated with a capsulotomy and lysis of adhesions. At the time of most recent follow-up, the patient had regained all of her preoperative hip external rotation.
Discussion
The most important finding of this study is that symptomatic hip microinstability may be a real clinical entity that may be successfully managed with hip arthroscopy and suture capsular plication when non-operative management has failed. Although there are no objective criteria to define hip laxity, nor the amount of required plication, the authors feel this study is important to confirm the concept of hip microinstability, by reporting the results of capsular plication without concomitant bony procedures. The purpose of this study is to report the clinical outcomes of patients treated with hip arthroscopy and suture capsular plication without concomitant osseous surgery for the treatment of symptomatic hip microinstability. The results of the present study demonstrate significant clinical improvement in patients treated with hip arthroscopy and capsular plication. In addition, there were no significant differences in clinical outcomes between patients with and without radiographic evidence of lesser degrees of acetabular dysplasia. To our knowledge, this is the first study to report the results of patients with symptomatic atraumatic microinstability of the hip treated with hip arthroscopy and suture capsular plication without any associated FAI bony resections.
In this study, there was significant improvement in clinical outcomes following hip arthroscopy and suture capsular plication for the treatment of symptomatic atraumatic hip microinstability. Similar results have been reported using a variety of open and arthroscopic techniques. Bellabarba et al. [3] reported a single case of atraumatic hip instability treated successfully with open suture capsulorrhaphy. Philippon et al. [18] reported the results of arthroscopic thermal capsulorrhaphy in a series of 12 patients with hip instability. All patients experienced improvement in their mHHS at both 6 weeks and 6 months postoperatively. In addition, eight patients in Philippon’s series were professional athletes and all returned to their pre-injury level of competition, similar to the results presented in this series. Thermal capsulorrhaphy in the shoulder has been associated with thermal necrosis, chondrolysis, and capsular attenuation, although these complications have not been reported in the hip. Regardless, concern for these potential complications has led to arthroscopic hip capsular plication using sutures becoming more commonly used for treating hip capsular laxity and microinstability. Although more technically demanding, this technique allows control of plication tension and can easily be used during concomitant cartilage, labrum, or FAI procedures. Several authors have reported success with a variety of arthroscopic suture plication techniques; however, most of these reports consist of small case series of patients treated with suture plication along with associated bony resections [11, 19, 20].
Although good results have been reported with a variety of arthroscopic suture plication techniques, the technique used by the senior author in this study is unique in that it avoids iatrogenic injury to the iliofemoral ligament [1, 9, 10, 22]. Several described plication techniques involve transection of the iliofemoral ligament, either longitudinally during the vertical limb of a T-capsulotomy or transversely in an attempt to perform an inferior capsular shift [1, 9, 10]. When suture plication is then performed, there is a potential for overtightening of the iliofemoral ligament. This may result in hip stiffness and loss of range of motion, particularly loss of external rotation. The plication technique performed by the senior author in this study, however, consists of a capsulotomy and plication in the capsular “bare area” or “rotator interval” between the iliofemoral and ischiofemoral ligaments [23]. Plication of this “rotator interval” theoretically avoids overtightening of a single capsular ligament. Given that there is no quantitative way to measure hip instability or a consensus on how much capsular plication is necessary to treat instability, the senior author feels that it is safer to close this capsular interval rather than directly tightening a specific capsular ligament. In this study, we found no significant difference between preoperative and postoperative hip range of motion, although one patient did complain of hip stiffness requiring arthroscopic lysis of adhesions. Domb et al. [10] recently reported the results of patients with borderline hip dysplasia treated with arthroscopic capsular plication. The authors performed a transverse transection of the iliofemoral ligament followed by a “shift” of the inferior capsule proximally, essentially shortening the iliofemoral ligament. They reported favourable clinical results at 2-year follow-up; however, there was a statistically significant loss of hip external rotation. This loss of hip range of motion may have a negative effect in patients participating in certain sports requiring extreme hip range of motion. It has been shown in the shoulder, for example, that loss of glenohumeral internal rotation in overhead athletes and pitchers results in abnormal mechanics and an increased risk of injury, while a loss of external rotation can affect the velocity of the ball [5, 8, 15]. Similarly, loss of hip range of motion may also potentially affect energy transfer and the kinetic chain during certain movements, and for sports such as ballet, range of motion is critical to performance of their activity [12].
No difference was noted between patients with mild acetabular dysplasia and patients without acetabular dysplasia in terms of clinical function and pain at final follow-up. For patients with hip microinstability in the presence of acetabular dysplasia, the role of hip arthroscopy and capsular plication is not well defined. Byrd et al. [6] reported the results of 48 patients with acetabular dysplasia or borderline dysplasia treated with hip arthroscopy. At a minimum follow-up of 1 year, there was significant improvement in clinical outcomes. As a result, the authors concluded that the presence of hip dysplasia is not a contraindication to hip arthroscopy, nor is it an indicator of poor outcome. Similar results were noted among the dysplastic patients, with a mean mHHS improvement of 28 points. It should be noted that none of the dysplastic patients in the previously mentioned report were diagnosed with hip instability and no patients underwent capsular plication, making comparisons between the studies difficult. Domb et al. [10] recently reported the 2-year results of patients with borderline hip dysplasia treated with arthroscopic capsular plication. They noted significant improvement in all patient-reported outcome scores at final follow-up, once again consistent with the results of our dysplastic patient population. It should also be noted that 41% of the patients in this study underwent a concomitant bony resection of the proximal femur.
Atraumatic hip microinstability can also be seen in patients with non-dysplastic hip joints, but there is very little literature available on the clinical results of capsulorrhaphy/capsular plication in the treatment of symptomatic atraumatic instability in these patients. In the previously mentioned report by Philippon, the author treated a series of 12 patients with arthroscopic thermal capsulorrhaphy [18]. All patients experienced clinical improvement postoperatively and all professional athletes in the series were able to return to their pre-injury level of competition. In a subsequent study, the same author reported the results of revision hip arthroscopy [19]. Of the 37 reported cases, 13 patients underwent capsular plication or thermal capsulorrhaphy for treatment of previously unaddressed hip instability and experienced significant improvement in their symptoms. It should be noted, however, that 34 of the 37 patients in this latter Philippon study also underwent concomitant bony resection of the acetabular rim or proximal femur for treatment of previously unaddressed or undertreated FAI. To our knowledge, there are no other studies that report the results of patients with symptomatic atraumatic microinstability of the hip treated with hip arthroscopy and suture capsular plication without any associated FAI bony resections.
The present study has several limitations. First, the clinical outcomes were evaluated with the mHHS and iHOT scores. Both clinical patient outcome scores have been validated in the literature; however, they may not be sensitive enough to detect subtle changes in pain and function, especially in the context of atraumatic hip microinstability [13, 14, 16]. Although we did note significant improvement in patient pain and function at each point in follow-up and the vast majority of patients participating in preoperative competitive sport were able to return to their preoperative level of competition, the development of a more sensitive hip instability-specific rating system may be helpful for elucidating subtle functional differences. Second, there is no objective way to assess for hip laxity, the degree of hip laxity, or the resolution of this symptomatic laxity/instability. However, hip microinstability is being diagnosed more frequently, and surgery performed more often for this diagnosis. The authors felt that the outcomes of this group of patients who underwent capsuloligamentous plication without bony surgery help support the concept that this diagnosis is a valid clinical entity, though objective measures still elude us. Third, there were a relatively small number of patients in the study cohort, even though a minimum of 12-month follow-up was available for 31 of the 32 patients (94%). This smaller cohort may be a result of relatively few patients actually suffering from hip microinstability as well as the challenging nature of diagnosing this sometimes subtle condition. Even so, a larger series of patients may have potentially elucidated significant correlations between patient age, duration of symptoms, previous hip arthroscopy, nature of onset of symptoms, CEA, Tönnis angle, or preoperative physical examination findings with clinical outcome. Fourth, the available patient follow-up (mean 20 months) may not be adequate to provide perspective on longer-term clinical outcomes. Only longer follow-up can give us information on the durability of this intervention, particularly for those patients with relative bony deficiency (acetabular dysplasia). Lastly, this study lacks a control group. In an attempt to minimize potential confounding variables, patients who underwent concomitant bony surgery at the time of arthroscopy were excluded, and the results of patients with and without acetabular dysplasia were also separately analysed. Regardless, there was still substantial variability in the surgical treatment of labral tears, ligamentum teres tears, and chondral lesions. As a result, it is difficult to definitively state that suture capsular plication is the sole reason for the improved clinical outcomes in this cohort.
Conclusion
The results of this study suggest that symptomatic hip microinstability may be a real clinical entity and may be successfully managed with hip arthroscopy and suture capsular plication when non-operative management has not resolved the patient’s symptoms.
References
Bedi A, Galano G, Walsh C et al (2011) Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy 27:1720–1731
Beighton P (1988) Hypermobility scoring. Br J Rheumatol 27:163
Bellabarba C, Sheinkop M, Kuo K (1998) Idiopathic hip instability: an unrecognized cause of coxa saltans in the adult. Clin Orthop Relat Res 355:261–271
Boykin R, Anz A, Bushnell B et al (2011) Hip instability. J Am Acad Orthop Surg 19:340–349
Burkhart S, Morgan C, Kibler W (2003) The disabled throwing shoulder: spectrum of pathology. Arthroscopy 19:404–420
Byrd J, Jones K (2003) Hip arthroscopy in the presence of dysplasia. Arthroscopy 19:1055–1060
Byrd J, Jones K (2000) Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy 16:578–587
Dines J, Frank J, Akerman M et al (2009) Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med 37:566–570
Domb B, Philippon M, Giordano B (2013) Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy 29:162–173
Domb B, Stake C, Lindner D et al (2013) Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med 41:2591–2598
Epstein D, Rose D, Philippon M (2010) Arthroscopic management of recurrent low-energy anterior hip dislocation in a dancer: a case report and review of literature. Am J Sports Med 38:1250–1254
Fleisig G, Barrentine S, Escamilla R et al (1996) Biomechanics of overhand throwing with implications for injuries. Sports Med 21:421–437
Harris W (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am 51:737–755
Harris-Hayes M, McDonough C, Leunig M et al (2013) Clinical outcomes assessment in clinical trials to assess treatment of femoroacetabular impingement use of patient-reported outcome measures. J Am Acad Orthop Surg 21(Suppl 1):39–46
Kibler W, Wilkes T, Sciascia A (2013) Mechanics and pathomechanics in the overhead athlete. Clin Sports Med 32:637–651
Mohtadi N, Griffin D, Pedersen M et al (2012) The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the international hip outcome tool (iHOT-33). Arthroscopy 28:595–605
Nunley R, Prather H, Hunt D et al (2011) Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Jt Surg Am 93(Suppl 2):17–21
Philippon M (2001) The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med 20:817–829
Philippon M, Schenker M, Briggs K et al (2007) Revision hip arthroscopy. Am J Sports Med 35:1918–1921
Ranawat A, McClincy M, Sekiya J (2009) Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Jt Surg Am 91:192–197
Shindle M, Ranawat A, Kelly B (2006) Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med 25:309–326
Shu B, Safran M (2011) Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med 30:349–367
Telleria J, Lindsey D, Giori N et al (2011) An anatomic arthroscopic description of the hip capsular ligaments for the hip arthroscopist. Arthroscopy 27:628–636
Tönnis D, Heinecke A (1999) Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Jt Surg Am 81:1747–1770
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding was received for this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Formal consent is not required for the study.
Rights and permissions
About this article
Cite this article
Kalisvaart, M.M., Safran, M.R. Hip instability treated with arthroscopic capsular plication. Knee Surg Sports Traumatol Arthrosc 25, 24–30 (2017). https://doi.org/10.1007/s00167-016-4377-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4377-6