Abstract
Purpose
To inventory the examination methods available to assess antero-medial rotational laxity (AMRL) of the knee following medial collateral ligament injury.
Methods
Searches were conducted in accordance with the PRISMA guidelines and using four online databases: WEB OF SCIENCE, MEDLINE, EMBASE, and AMED. The Critical Appraisal Skills Programme guidelines for Diagnostic Test Studies were used for the quality assessment of the articles.
Results
A total of 2241 articles were identified from the database searches. From this, four articles were included in the final review. All were case–control studies, considered a combined ACL/MCL injury and had small study populations. Specialised equipment was required in all studies, and one needed additional imaging support before measurements could be taken. Two employed commercially available measuring equipment as part of the assessment process.
Conclusion
Clinical assessment of AMRL in relation to a MCL injury remains challenging. Although methods have been developed to support clinical examination, they are limited by a number of factors, including the need for additional time in the clinical environment when setting up equipment, the need for specific equipment to produce and measure rotational movement and imaging support. In addition, there are patient safety concerns from the repeated imaging. A reliable and valid clinical examination remains to be found to truly assess antero-medial rotational laxity of the knee.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Knee stability, key for successful locomotion, is achieved through static and dynamic structures working synergistically to maintain knee integrity against destabilising forces [34]. Static structures include the menisci, cruciate and collateral ligaments, and joint capsule. Dynamic structures include the quadriceps, hamstring, and calf muscles traversing the joint [18, 44]. Often, there is a fine balance between the different elements, particularly those on the medial and lateral aspects of the knee [35].
Knee injuries commonly cause morbidity, and the medial collateral ligament (MCL) is most frequently traumatised [15, 32, 46]. The MCL is the primary restraint to knee valgus movement throughout flexion, but also limits external rotation, functioning as a secondary restraint anterior displacement with the Anterior cruciate ligament (ACL) [6, 41, 51, 54, 56].
O’Donoghue [40] identified two components to the MCL, the superficial (sMCL) and deep (dMCL). The larger sMCL runs from the medial femoral condyle, inserts on the tibia anteriorly, and resists valgus stress [45]; studies have suggested it sustains forces of up to 557.1 ± 55.4 N [57]. The dMCL is reported as the primary restraint for antero-medial rotational laxity (AMRL) at all ranges of knee flexion [9, 10, 23] and tolerates forces up to 100.5 ± 10.3 N [8, 54]. Due to its close association with the joint and fibrous attachments to the medial meniscus (MM), concurrent dMCL/MM pathologies often occur [5, 47, 50]. Moreover, there is also load sharing between the dMCL/sMCL and dMCL/ACL complexes; injury to one component confers additional stabilising responsibilities to the other [7, 19, 45, 58].
With its relative vulnerability from rotational forces, dMCL disruption should be frequently anticipated. Injuries to the dMCL have been reported to prevent patients returning to sporting activities due to persistent symptoms, and therefore, focused interventions are necessary to restore function [25, 43].
Three degrees of MCL injury are recognised, based on gapping and perceived end-point feel [33]. This is assessed with valgus forces in straight leg (sMCL) and in 30° degrees flexion (dMCL). Valgus–varus assessment does not fully assess rotatory knee stability, due to the lack of rotational stressors, and hence dMCL disruption might be missed [31]. In general, grade I/II injures improve with conservative measures and traditionally grade III was thought to require surgical correction. However, the availability of bracing and rehabilitation techniques has made surgical intervention less common [8, 14, 17].
Slocum and Larson [49] described AMRL along the long axis of the knee, speculating that this may be a limiting factor for athletes participating in sports requiring sudden changes in direction or rotational movements. While routine examinations assess valgus and varus knee stability [27], Slocum and Larson’s [49] work prompted anatomical investigations of the MCL and methods to clinically evaluate AMRL [13]. While methods to assess rotational movement of the knee in vitro have been considered in the past [32], this review aims to inventory the available methods, including diagnostic tests, which can be applied in the clinical setting to assess rotational laxity in the context of a dMCL injury. This will support practicing clinicians by providing them with up to date information to enable an informed choice when choosing a method to assess this pathology.
Materials and methods
Search strategy
The PRISMA statement was used as a guideline to conduct the review [37]. A systematic computerised search was conducted using WEB OF SCIENCE, MEDLINE, PubMed, and EMBASE from inception until August 2016, including the following keywords:
-
Knee.
-
(Medial AND collateral AND ligament) OR MCL OR (Deep and medial AND collateral AND ligament) OR dMCL.
-
Antero-medial OR External.
-
Rotatory OR Rotational OR Laxity.
-
Physical OR Clinical OR Examination OR Assessment.
Eligibility criteria
The following inclusion criteria were applied to select relevant papers:
-
The study included human subjects over 18 years old.
-
The investigation focused on assessing knee AMRL with MCL injury either in isolation or with another concurrent pathology.
-
The study was published in English.
Articles were excluded if they were:
-
Not peer-reviewed.
-
Reviews.
-
Cadaveric or anatomical studies.
-
Did not include an MCL injury.
Review process
Articles were imported into Endnote X7.5 (Thomson Reuters, CA, USA). Duplicates were removed before two authors (DS; EP) independently screened the titles and abstracts of articles retrieved from the databases searches. The full texts of the remaining articles were then reviewed to check for eligibility. Disagreements were resolved by consensus discussion. References of relevant papers were checked for additional studies that the database searches may have overlooked.
Study analysis
An adapted Critical Appraisal Skills Programme for Diagnostic Test Studies was used to extract information including population, methodology, outcome measures, gold standard applied, and study findings [12]. Quality assessment of studies, including assessment of population bias and clinical applicability, was based on the QUADAS-2 checklist for diagnostic studies [55].
Results
Search findings
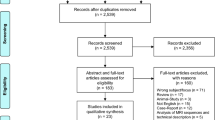
The article selection process is shown in Fig. 1. The search identified 2241 articles, and 2 were identified from other sources. Examination of titles and abstracts produced 182 remaining articles. Following application of the eligibility criteria, the full text revision yielded 4 studies to be included in the subsequent review processes of quality assessment and data extraction. Reasons for exclusion of the other 178 articles are shown in Fig. 1.
Quality assessment
Table 1 shows the quality assessment scores, based on the QUADAS-2 [55] checklist, of the 4 included studies, indicating potential sources of bias. Three articles had population bias [28, 30, 36], and all [28, 30, 36, 39] were of questionable applicability. No articles excluded subjects from analysis.
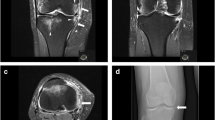
Study characteristics
Table 2 summarises the data extracted from the included studies. All studies adopted a case–control design and considered combined ACL/MCL injuries [28, 30, 36, 39]. None considering an MCL injury in isolation were available for inclusion. Three studies also included healthy controls for comparison [28, 30, 36]. All four employed specialised medical devices to assess knees [28, 30, 36, 39], but two also employed the KT-1000 arthrometer (MEDmetric, San Diego, CA), either as part of their experimental method for assessing AMRL [36] or as a validation tool [39]. The KT-1000 arthrometer is commonly employed as a tool for quantifying anterior laxity following ACL injury and not for rotational assessments. One study employed Computerised tomography (CT) to produce images from which measurements were taken [39], while the remaining three relied on non-imaging modalities [28, 30, 36]. None employed a physical/clinical examination technique to assess AMRL.
Devices used for assessment and related findings
Kennedy and Fowler [28] developed a clinical stress machine to produce rotational movement around the knee using a gas-driven footplate controlled with rolling drums. Most medial movement (mm) was identified in subjects with an ACL/MCL injury, whereas it was less in healthy subjects and negligible with isolated ACL injuries (Table 2).
The ‘Laxitester’ [36] produces rotational torque along the long axis of a flexed knee (Fig. 2). No significant difference in rotational (°) movement was identified between the study groups, but anterior displacement (mm) in the externally rotated position was greatest in subjects with an ACL/MCL injury (Table 2).
Laxitester produced rotational movement at the foot and measured the maximal angle (°) of movement. Simultaneously, an anterior force was applied using the KT-1000 to measure anterior displacement (mm) in the rotated position [36]
Kurimura et al. [30] used a foot-level rotating plate and electronic displacement sensors to measure displacement (mm) and stiffness [angle (°)] around the knee (Fig. 3). In subjects with an ACL/MCL injury, displacement (20°: 5.0 ± 2.4 mm, 90°: 3.5 ± 1.8 mm) and stiffness (20°: −28.7 ± 36.2°, 90°: −18.0 ± 10.1°) increase significantly compared to healthy subjects and those with an isolated ACL injury (Table 2).
Rotational device using electronic displacement system employed by Kurimura et al. [30]. Their devices enabled differing degrees of knee flexion and produced rotational movement at the foot. Electronic displacement devices placed along the tibia and at the patella detected movement (mm)
Nordt et al. [39] used a modified force transduction apparatus (Telos Co., Hungen-Obbornhofen, Germany) and Computerised tomography (CT) imaging (Fig. 4) to study post-operative patients with unilateral ACL or ACL/MCL injuries. Displacement (°), measured from CT images, was significantly greater for combined ACL/MCL injuries in a neutral and anteriorly displaced conditions compared to healthy knees and those with an isolated ACL pathology (Table 2).
Force translation apparatus used by Nordt et al. [39]; it produced an anterior force behind the knee while an external rotation moment was produced at the foot. CT images were obtained and from these external rotation (°) of the knee was calculated
Discussion
The most important finding of the present study was the absence of an easily applicable method for clinically assessing AMRL in the context of a dMCL injury. This systematic review aimed to examine methods for assessing the AMRL in vivo following a medial knee injury, but as none were available, those who studied a combined ACL/MCL pathology were included.
The search yielded four studies, all of which employed specialised medical equipment to produce rotational forces and record movements. This included a gas-driven system [28], the ‘Laxitester’ [36], customised frames [28, 30], and torque wrench systems [39]. In addition, some utilised more conventional systems such as the KT-1000 [36, 39] and CT imaging [39] to analyse the movements.
While the authors report that their individual systems provide a method for assessing rotational laxity in the knee, a glaring drawback is the need for specialised equipment that may not be commercially available. Without being more widely accessible, it almost negates any generalizable benefits from each of these examinations and leaves their methods only applicable in the respective institution. Equally, needing time to set up, calibrate, and then analyse the results limits the practical applicability of these systems in a real-world fast-paced clinical setting where real-time feedback would be also preferable. With consultation time pressures and clinical loads, time taken to use these systems would require specialised clinical settings or personnel; otherwise, they remain only an option in research environments. Moreover, in situations where repeated CT imaging [39] is needed, it brings patients’ safety issues into question with repeated high-dose radiation.
A key limitation of the studies included in the review is the small population sample sizes, particularly the subjects with an ACL/MCL injury. This implies that the generalizability of the findings to situations where only the dMCL is affected is particularly challenging, but given the paucity of studies examining this phenomenon, an exclusion criterion for study power could not be set. As such, while the combined ACL/MCL injury subjects did demonstrate greater movement than healthy knees and those with an isolated ACL pathology, it is a significant assumption that the MCL injury was the contributing factor. Further studies involving isolated MCL injured patients are needed to address this question.
Another limitation of the systems employed is the rotational movement being generated at the foot and taken to represent the rotated position of the knee [30, 36]. In a cadaveric study of ankle-level knee AMRL measurements, foot and tibial recordings taken to represent knee movement were analysed using inclinometers at 30° and 90° knee flexion. Significantly, greater movement was recorded at the ankle level at both positions [1]. Given that rotational positions of the foot were taken to represent those at the knee, an element of error is certainly possible in the methods reviewed. Indeed, similar studies in the past that have focussed exclusively on ACL pathologies and measured knee rotational laxity at the ankle have also made this same assumption, bringing into question the outcomes of otherwise more applicable systems [3, 4, 16, 25, 26].
Equally, a further limitation of the studies reviewed were the physical parameters measured; some recorded movement in mm [28, 30, 36], while others took angular measurements [36, 39]. This limits direct comparison of the studies, and also, for an individual patient assessed by one method, reassessment via an alternative might produce different results.
During the review process, it was evident that several studies have considered AMRL in the context of an isolated ACL injury. While these were excluded from the review process based on the eligibility criteria, several of these also employed a medical device to produce rotational movement [2–4, 16, 20, 21, 25, 26, 29, 30, 36, 39, 48, 53], used imaging modalities to record movements [3, 16, 20–22, 25, 26, 39, 41, 42, 52, 53] or attempted to perform this assessment functionally [11, 22].
As with the studies included in the review process, many of these methods required specialised medical apparatus, most of which are not commercially available, technical expertise, extensive time, and patients’ exposure to radiation. Some, such as the Vermont knee laxity device (VKLD), was used in repeated studies to determine the degree of rotational movement in healthy [48, 53], ACL-deficient [20], and post-ACL repair subjects [29]. This implies that it was available to different groups for research purposes and that also the design held a degree of versatility, such that a non-metallic version could be manufactured and applied in another study [20]. However, it still remains impractical in the clinical setting due to time taken in setting up the system; moreover, it was only tested in patients with an isolated ACL injury.
The generalizability and results of this review are limited by the paucity and quality of studies focussing on the MCL/dMCL and its role in controlling for AMRL. One of the challenges is in the variability of methodology in recording the rotational movement and the actual measurement taken as displacement in mm or angular displacement in degrees, making direct comparison and extrapolation of results more challenging. The exclusion of studies that were not in vivo or did not consider an MCL injury limited the number of studies included in the review process. While AMRL could have been considered more generally, with the aim of the review being to assess AMRL in the context of an MCL pathology, it would not have been in keeping with the review process. However, it does not mean that these studies could not have been applied in the situations of suspected MCL injury, either in isolation or as a combined pathology.
Moreover, the following limitations should be acknowledged about this review: agreement statistics were not included as part of the methods, as on only one occasion did authors disagree. Only studies published in English were considered due to unavailability of translated sources, representing a language bias to study selection.
Rotational laxity of the knee associated with a dMCL injury can cause a delayed return to activity for professional and amateur athletes and those in physically challenging professions [24, 38]. The aim of being able to effectively assess this in the clinical setting would be to limit the impact this injury has on performance and increase participation in activities. Moreover, by having a readily applicable assessment method, it could highlight the need for focussed treatments at an earlier stage, rather than when there was a failure to progress.
Conclusion
Deep MCL injury and AMRL remain an enigma in medicine that is not routinely examined by clinicians. While we understand more about the anatomical subtleties of this structure, this knowledge is of limited use without a reliable clinical assessment. This review highlights the paucity of methodologies when examining AMRL in association with a medial ligament injury. Even when investigated, specialised equipment was needed to generate rotational movement or record movements produced. Further work is clearly required to identify a clinically valid and reproducible examination technique.
Abbreviations
- AMRL:
-
Antero-medial rotational laxity
- CT:
-
Computerised tomography
- ACL:
-
Anterior cruciate ligament
- MCL:
-
Medial collateral ligament
- sMCL:
-
Superficial medial collateral ligament
- dMCL:
-
Deep medial collateral ligament
- MM:
-
Medial meniscus
- VKLD:
-
Vermont knee laxity device
References
Alam M, Bull AMJ, Thomas R et al (2011) Measurement of rotational laxity of the knee: in vitro comparison of accuracy between the tibia, overlying skin, and foot. Am J Sports Med 39(12):2575–2581
Alam M, Bull AMJ, Thomas R et al (2013) A clinical device for measuring internal–external rotational laxity of the knee. Am J Sports Med 41(1):87–94
Almquist PO, Arnbjörnsson A, Zätterström R et al (2002) Evaluation of an external device measuring knee joint rotation: an in vivo study with simultaneous roentgen stereometric analysis. J Orthop Res 20(20):427–432
Almquist PO, Ekdahl C, Isberg PE et al (2013) Knee rotation in healthy individuals related to age and gender. J Orthop Res 31(1):23–28
Ambrose HC, Simonian PT, Sims WF (2001) Arthroscopic localization of medial collateral ligament injury: report of 2 cases in adults. Arthroscopy 17(5):E21
Amis AA, Bull AMJ, Gupte CM et al (2003) Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Truamatol Arthrosc 11(5):271–281
Athwal KK, Daou HE, Kittl C et al (2016) The superficial medial collateral ligament is the primary medial restraint to knee laxity after cruciate-retaining or posterior-stabilised total knee arthroplasty: effects of implant type and partial release. Knee Surg Sports Traumatol Arthrosc 24(8):2646–2655
Ballmer PM, Jakob RP (1988) The non operative treatment of isolated complete tears of the medial collateral ligament of the knee. Arch Orthop Trauma Surg 107:273–276
Branch TP, Stinton SK, Siebold R et al (2015) Assessment of knee laxity using a robotic testing device: a comparison to the manual clinical knee examination. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3935-7
Cavaignac E, Carpentier K, Pailhe R et al (2015) The role of the deep medial collateral ligament in controlling rotational stability of the knee. Knee Surg Sports Truamatol Arthrosc 23(10):3101–3107
Chouteau J, Testa R, Viste A et al (2012) Knee rotational laxity and proprioceptive function 2 years after partial ACL reconstruction. Knee Surg Sports Truamatol Arthrosc 20(4):762–766
Critical Appraisal Skills Program (CASP) (Diagnostic checklist). http://www.casp-uk.net/casp-tools-checklists. Accessed Aug. 2016
Csintalan RP, Ehsan A, McGarry MH et al (2006) Biomechanical and anatomical effects of an external rotational torque applied to the knee: a cadaveric study. Am J Sports Med 34(10):1623–1629
Edson CJ (2006) Conservative and postoperative rehabilitation of isolated and combined injuries of the medial collateral ligament. Sports Med Arthrosc 14(2):105–110
Ellis BJ, Lujan TJ, Dalton MS et al (2006) Medial collateral ligament insertion site and contact forces in the ACL-deficient knee. J Orthop Res 24(4):800–810
Espregueira-Mendes J, Pereira H, Sevivas N et al (2012) Assessment of rotatory laxity in anterior cruciate ligament-deficient knees using magnetic resonance imaging with Porto-knee testing device. Knee Surg Sports Truamatol Arthrosc 20(4):671–678
Fetto JF, Marshall JL (1978) Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res 132:206–218
Flandry F, Hommel G (2011) Normal anatomy and biomechanics of the knee. Sports Med Arthrosc 19(2):82–92
Haimes JL, Wroble RR, Grood ES et al (1994) Role of the medial structures in the intact and anterior cruciate ligament-deficient knee. Am J Sports Med 22(3):402–409
Haughom BD, Souza R, Schairer WW et al (2012) Evaluating rotational kinematics of the knee in ACL-ruptured and healthy patients using 3.0 Tesla magnetic resonance imaging. Knee Surg Sports Truamatol Arthrosc 20(4):663–670
Hemmerich A, van der Merwe W, Batterham M et al (2012) Knee rotational laxity: an investigation of bilateral asymmetry for comparison with the contralateral uninjured knee. Clin Biomech 27(6):607–612
Hoshino Y, Fu FH, Irrgang JJ et al (2013) Can joint contact dynamics be restored by anterior cruciate ligament reconstruction? Clin Orthop Relat Res 471(9):2924–2931
Iizawa N, Mori A, Majima T et al (2015) Influence of the medial knee structures on valgus and rotatory stability in total knee arthroplasty. J Arthroplasty 31(3):688–693
Jones L, Bismil Q, Alyas F et al (2009) Persistent symptoms following non operative management in low grade mcl injury of the knee—the role of the deep MCL. The Knee 16:64–68
Kärrholm J, Elmqvist L-G, Selvik G et al (1989) Chronic anterolateral instability of the knee. A roentgen sterophotogrammetric evaluation. Am J Sports Med 17(4):555–563
Kärrholm J, Selvik G, Elmqvist LG et al (1988) Three-dimensional instability of the anterior cruciate deficient knee. J Bone Joint Surg Br 70(5):777–783
Kastelein M, Wagemakers HP, Luijsterburg PA et al (2008) Assessing medial collateral ligament knee lesions in general practice. Am J Med 121(11):982–988
Kennedy JC, Fowler PJ (1971) Medial and anterior instability of the knee: an anatomical and clinical study using stress machines. J Bone Joint Surg Am 53(7):1257–1270
Kothari A, Haughom B, Subburaj K et al (2012) Evaluating rotational kinematics of the knee in ACL reconstructed patients using 3.0 Tesla magnetic resonance imaging. The Knee 19(5):648–651
Kurimura M, Matsumoto H, Fujikawa K et al (2004) Factors for the presence of anteromedial rotatory instability of the knee. J Orthop Sci 9(4):380–385
Kurzweil PR, Kelley ST (2006) Physical examination and imaging of the medial collateral ligament and posteromedial corner of the knee. Sports Med Arthrosc 14(2):67–73
Lam MH, Fong DT, Yung PS et al (2012) Biomechanical techniques to evaluate tibial rotation. a systematic review. Knee Surg Sports Truamatol Arthrosc 20(9):1720–1729
Lubowitz JH, Bernardini BJ, Reid JB (2008) Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med 36(3):577–594
Marchant MH, Tibor LM, Sekiya JK et al (2011) Management of medial-sided knee injuries, part 1: medial collateral ligament. Am J Sports Med 39(5):1102–1113
Matsuzaki T, Matsuoto T, Kubo S et al (2014) Tibial internal rotation is affected by lateral laxity in cruciate-retaining total knee arthroplasty: an intraoperative kinematic study using a navigation system and offset-type tensor. Knee Surg Sports Truamatol Arthrosc 22(3):615–620
Mayr HO, Hoell A, Bernstein A et al (2011) Validation of a measurement device for instrumented quantification of anterior translation and rotational assessment of the knee. Arthroscopy 27(8):1096–1104
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269
Narvani A, Mahmud T, Lavelle J et al (2010) Injury to the proximal deep medial collateral ligament. A problematic subgroup of injuries. J Bone Joint Surg Br 92(7):949–953
Nordt WE, Lotfi P, Plotkin E et al (1999) The in vivo assessment of tibial motion in the transverse plane in anterior cruciate ligament-reconstructed knees. Am J Sports Med 27(5):611–616
O’Donoghue DH (1950) Surgical treatment of fresh injuries to the major ligaments of the knee. J Bone Joint Surg Am 32-A(4):721–738
Okazaki K, Miura H, Matsuda S et al (2007) Assessment of anterolateral rotatory instability in the anterior cruciate ligament-deficient knee using an open magnetic resonance imaging system. Am J Sports Med 35(7):1091–1097
Okazaki K, Tashiro Y, Izawa T et al (2012) Rotatory laxity evaluation of the knee using modified Slocum’s test in open magnetic resonance imaging. Knee Surg Sports Truamatol Arthrosc 20(4):679–685
Robinson JR, Bull AMJ, Thomas RR et al (2006) The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med 34(11):1815–1823
Robinson JR, Sanchez-Ballester J, Bull AMJ et al (2004) The posteromedial corner revisited: an anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Joint Surg Br 86(5):674–681
Schafer KA, Tucker S, Griffith T et al (2016) Distribution of force in the medial collateral ligament complex during simulated clinical tests of knee stability. Am J Sports Med 44(5):1203–1208
Schaffer DJ (1981) Knee ligament injuries induced by skiing. Ann Emerg Med 10(9):472–475
Shelbourne D, Nitz PA (1991) The O’Donoghue triad revisited. Am J Sports Med 19(5):474–477
Shultz SJ, Shimokochi Y, Nguyen AD et al (2007) Measurement of varus–valgus and internal–external rotational knee laxities in vivo–Part II: relationship with anterior–posterior and general joint laxity in males and females. J Orthop Res 25(8):989–996
Slocum DB, Larson RL (1968) Rotatory instability of the knee: its pathogenesis and a clinical test to demonstrate its presence. J Bone Joint Surg Am 50(2):211–225
Stein G, Koebke J, Faymonville C et al (2011) The relationship between the medial collateral ligament and the medial meniscus: a topographical and biomechanical study. Surg Radiol Anat 33(9):763–766
Sullivan D, Levy M, Sheskier S et al (1984) Medical restraints to anterior-posterior motion of the knee. J Bone Joint Surg Am 66(6):930–936
Tashiro Y, Okazaki K, Miura H et al (2009) Quantitative assessment of rotatory instability after anterior cruciate ligament reconstruction. Am J Sports Med 37(5):909–916
Un BS, Beynnon BD, Churchill DL et al (2001) A new device to measure knee laxity during weightbearing and non-weightbearing conditions. J Orthop Res 19(6):1185–1191
Wang X, Malik A, Bartel DL, et al. (2014) Asymmetric varus and valgus stability of the anatomic cadaver knee and the load sharing between collateral ligaments and bearing surfaces. J Biomech Eng 136(8)
Whiting PF, Rutjes AWS, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536
Wijdicks CA, Ewart DT, Nuckley DJ et al (2010) Structural properties of the primary medial knee ligaments. Am J Sports Med 38(8):1638–1646
Wijdicks CA, Griffith CJ, Johansen S et al (2010) Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am 92(5):1266–1280
Wijdicks CA, Griffith CJ, LaPrade RF et al (2009) Medial knee injury: part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med 37(9):1771–1776
Authors’ contribution
DS conceived the review, participated in designing and conducting the review, drafted the manuscript, and took it through the final editing process. EP participated in designing and conducting the review, drafted the manuscript, and took it through the final editing process. ET conceived the review, participated in designing and conducting the review. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sirisena D, Papi E, and Tillett E declare that they have no conflict of interest.
Funding
No funding was received for this study.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This was a systematic review and there were no participants included.
Rights and permissions
About this article
Cite this article
Sirisena, D., Papi, E. & Tillett, E. Clinical assessment of antero-medial rotational knee laxity: a systematic review. Knee Surg Sports Traumatol Arthrosc 25, 1068–1077 (2017). https://doi.org/10.1007/s00167-016-4362-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4362-0