Abstract
Objective
To evaluate the degree of correlation between MRI and clinical gradings of medial collateral ligament (MCL) injuries and assess for associated structures on MRI which may influence the clinical perception of MCL laxity.
Materials and methods
All knee MRIs with acute MCL injuries between 2016 and 2020 at our centre were retrospectively reviewed by two blinded musculoskeletal radiologists. The clinic notes were reviewed for clinical gradings.
Results
One hundred and nineteen MRIs included. Forty-eight percent (57/119) agreement between MRI and clinical gradings (κ = 0.21, standard error (SE) 0.07). MRI grades: I 29% (34/119), II 50% (60/119), III 21% (25/119). Clinical grades: I 67% (80/119), II 26% (31/119), III 7% (8/119). In patients with clinical grade III MCL injury, there was waviness of the superficial MCL on MRI in 100% (8/8), deep meniscofemoral ligament tear in 75% (6/8), anterior cruciate ligament (ACL) partial or complete tear in 75% (6/8) and posteromedial corner (PMC) injury in 100% (8/8); compared with 0% (0/111), 34% (38/111), 44% (49/111) and 41% (46/111) respectively in clinical grade I or II injuries (p < 0.05).
Conclusion
Agreement between MRI and clinical gradings of MCL injuries was only ‘fair’, with MRI almost always overestimating the grade of the injury when there was a mismatch. Waviness of the superficial MCL and injuries to the deep MCL, ACL and PMC correlate with clinical instability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The medial collateral ligament (MCL) forms part of the capsuloligamentous complex of the medial knee [1]. The superficial component of the MCL is the largest and principle stabilising structure of the medial knee joint, measuring approximately 10 cm in length [2]. It originates at the posterior aspect of the medial femoral condyle and inserts onto the medial tibia, 5 to 7 cm below the knee joint line [3]. The deep component of the MCL is comprised of a meniscofemoral ligament (MFL) proximally and a meniscotibial ligament (MTL) distally, each measuring approximately 26 mm and 9 mm respectively [2].
MRI can accurately detect the presence of acute MCL injury in clinically diagnosed patients [4]. The three-part MRI grading system for MCL injury severity takes into account only the appearances of the superficial component of the MCL and is the same as that applied to many other ligaments. The MRI grading criteria are intended to correspond directly with the three clinical grades of MCL injury, which are based upon clinical MCL instability [5]. To our knowledge, the only previous evaluation of the accuracy of the MRI grading system was conducted in 1995 and the authors did not make direct comparison between clinical and MRI grades, nor did they analyse coronal fluid-sensitive sequences as is recommended by the grading system [5, 6]. However, their work did show that the MRI gradings were unexpectedly inversely related to clinical MCL instability [6]. This suggested that there was a need for a better MRI grading system than the current, which has remained unaltered to the present day.
Grading of MCL injuries is important for guiding treatment. Management normally involves conservative non-steroidal anti-inflammatory medication, rest and physical therapy for grade I injuries, with the addition of a knee brace for grade II and stable grade III injuries. Operative repair is indicated for acute grade III injuries with valgus alignment, MCL displacement over pes anserinus or bony avulsion [7].
In this study, we aim to (i) evaluate the correlation between MRI and clinical gradings of MCL injuries and (ii) assess for associated MRI features including other injured or intact structures which may influence clinical perception of MCL instability. We hypothesise that there are other features beyond the signal and continuity of the superficial MCL fibres which can be included in the MRI evaluation of MCL injuries for more concordance with clinical gradings than the current system provides.
Materials and methods
The study was approved by the local Research and Development Office and the committee confirmed that ethical opinion was not required.
Study participants
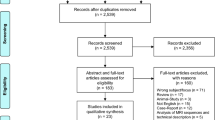
We conducted a retrospective observational study at our teaching hospital, which provides specialist tertiary referral orthopaedic services. The Picture Archiving and Communication System (PACS) was searched for all knee MRIs with a report containing the terms ‘MCL’ or ‘medial collateral ligament’ between December 2016 and December 2020. This captured all reports where the requesting clinician stated the word ‘MCL’ or ‘medial collateral ligament’ in the clinical history section or where the radiologist dictated that the findings were consistent with a ‘MCL injury’ or ‘medial collateral ligament injury’. Patients with MRI reports stating that the MCL was normal or that the MCL injury was chronic were excluded. When a patient had more than one MRI scan during the timeframe, we included only the MRI and clinical assessment which were performed closest to the time of initial injury.
The clinical notes for all included patients were reviewed to obtain the following information: age, sex, date of injury, mechanism of injury, clinical grade of MCL and injury management.
MRI technique and evaluation
All participants were scanned with a 1.5 T Magnetom Avanto or Avanto-Fit scanner (Siemens Healthcare, Germany), using a dedicated knee coil. The imaging protocols included standard knee sequences: proton density (PD) turbo spin echo (TSE) sagittal, T2-weighted fat-suppressed (FS) TSE sagittal, PD TSE axial, PD FS TSE coronal and T1-weighted spin echo coronal.
All included scans were reviewed by both a musculoskeletal radiology consultant and fellow with a combined 15 years of subspecialty experience, who were blinded from the clinical gradings. The appearances of each superficial MCL were given a grading reached by consensus between the two observers, defined according to the system which is currently used in radiological practise:
-
Grade I (low-grade sprain): high signal on fluid-sensitive sequences is seen superficial to the ligament, which itself looks normal.
-
Grade II (high-grade sprain/partial tear): high signal on fluid-sensitive sequences is seen superficial to the ligament, with high intrinsic signal or partial disruption of the ligament.
-
Grade III (high-grade tear): complete disruption of the ligament [5]
The appearances of the structures defined in Tables 2 and 3 were also recorded. The location of each anterior cruciate ligament (ACL) tear and whether partial or complete were specified. A medial meniscus tear was defined as high intrameniscal signal extending to an articular surface seen on at least two slices [8]. The configuration of the medial meniscal tear was also recorded and classified as a ‘ramp’ lesion if it involved the peripheral meniscocapsular attachments of the posterior horn [9]. A posteromedial corner (PMC) injury was defined as oedema, intrinsic high signal or discontinuity of any of the following structures: the posterior oblique (POL), oblique popliteal ligament(OPL), all five insertional tendon components of the semimembranosus, the posteromedial capsule and posterior horn of the medical meniscus [10,11,12].
Clinical evaluation
MCL injuries at our institution are categorised into three different clinical grades according to the Hughston standardisation of the AMA classification [13]. Injury severity is determined by the extent of tenderness and amount of medial joint opening when a valgus load is applied at 20 to 30 degrees of knee flexion, with less than a 3-mm medial joint line widening considered physiological:
-
Grade I (tear involving a few fibres): localised tenderness, no laxity, firm end point.
-
Grade II (tear involving more fibres but no instability): generalised tenderness, laxity with a firm end point.
-
Grade III (complete ligament disruption): generalised tenderness, laxity with no end point [13]
In those patients with a clinical grade III injury, the knee was also examined in extension to confirm a high-grade injury. The contralateral knee was examined in all cases as a baseline to compare with the injured knee.
Statistical analysis
Data was recorded and analysed using Microsoft Excel computer software. The agreement between the MRI and clinical gradings overall was described by percentage and weighted kappa (κ) with 95% CI. The following kappa cut-of values were used: ≤ 0.20 is slight agreement, 0.21–0.40 fair, 0.41–0.60 moderate, 0.61–0.80 substantial and 0.81–1 almost perfect [14]. Fisher’s exact test was used for measuring the statistical significance of differences in rates of associated injuries between grading categories. Statistical significance was set at p < 0.05.
Results
In the study period, a total of 315 MRI reports were identified as containing the relevant search terms. After applying the exclusion criteria, 119 cases were included for review. The MRI images for these were retrieved from PACS and the clinical notes were obtained. The clinical MCL injury gradings were specified or provided in clear descriptive terms in the clinic notes of all included cases.
The mean duration of time between the dates of clinical examinations and subsequent MRI scans was 14 days.
Thirty-eight percent of patients were female (45/119). Ages ranged between 11 to 79 years, with a mean of 41 years of age.
The most frequent injury mechanisms were sports related, comprising 75% (89/119). Of these, the most common were football 37% (33/89), skiing 24% (21/89) and rugby 9% (7/89). The second overall most frequent mechanisms of injury related to motor vehicle accidents 6% (7/119).
All grade II and III MCL injuries were treated with a hinged knee brace as per protocol in our unit to protect MCL healing. Cases of a concomitant posterior cruciate ligament (PCL) injury were treated with a PCL brace if a high-grade injury. ACL injuries were only treated with a brace if there was a concomitant MCL grade II or grade III injury. Surgical management was considered in those patients with grade III injuries in the setting of a multi-ligament knee injury. Surgical repair of the MCL was performed in 3% (4/119) of all patients, the remainder were managed conservatively. All four of these patients had concomitant ACL and PCL injuries.
MRI vs. clinical gradings of the MCL injuries
There was a 48% overall agreement rate (57/119) between the MRI and clinical gradings, κ = 0.21, standard error (SE) 0.07. See Table 1.
Half of all cases had a grading mismatch. The frequencies of findings on the MRIs of all patients with acute MCL injury and in those with each combination of grading disparity are provided in Table 2. The findings among patients with matching gradings are displayed in Table 3.
MCL injuries with a higher MRI than clinical grading
The MRI grading was higher than the clinical grading 15 times more frequently than it was lower. In the cases with the highest MRI grade (III) but lowest clinical grading (I), the ACL and PMC were almost twice as likely to be intact and medial meniscal tears were also less common compared with among those with a matching MRI and clinical grade III, possibly contributing to the increased stability clinically.
MCL injuries with a lower MRI than clinical grading
All cases with a lower MRI than clinical grading were MRI grade I and clinical grade II. In this group, injuries of all the additional structures that we assessed were more common than in those with a matching MRI and clinical grade I, possibly attributing to the decreased stability clinically (Table 3).
The four patients for which the MRI grading was lower than the clinical grading (MRI I vs. clinical II) are referred to below as patients a–d and more detail is provided on the accompanying injuries present on MRI for each of these individual patients:
-
Patient a: MFL oedema, PMC injury (specifically POL tear), medial meniscus tear and complete mid-substance tear of the ACL.
-
Patient b: MFL tear only.
-
Patient c: complete mid-substance tear of the ACL only.
-
Patient d: MFL oedema, MTL oedema, contusion in the posterior horn of the medial meniscus and complete mid-substance tear of the ACL.
MRI findings with increasing clinical severity of MCL injury
The frequencies of associated injuries on MRI in each clinical grading category are detailed and compared in Table 4.
An MRI grade III in combination with waviness involving all or part of the superficial MCL had total correlation with grade III instability clinically. Furthermore, in patients with a clinical grade III MCL injury, deep MFL tears, ACL tears and PMC injuries were all approximately twice as common on MRI than among patients with clinical grade I or grade II injuries (Table 4).
Discussion
The main findings of our study were two-fold. Firstly, there was a ‘fair’ rate of agreement between MRI and clinical gradings, with the most common and most polarised mismatches being those where the MRI grading was higher than the clinical. Secondly, waviness involving the superficial MCL and injuries to the deep MCL, ACL and PMC were all more frequent on MRI as the clinical gradings increased. The implications for clinical practise are clear: the current MRI grading system, which is based on the appearances of the superficial MCL, cannot always be relied upon to prognosticate the clinical grading. We discuss the findings in the cases we reviewed which may enable greater correlation between MRI evaluation and clinical MCL instability.
The superficial MCL is the most commonly injured ligament of the knee, torn in 8% of all knee injuries and involved in 60% of skiing knee injuries [3, 7, 15,16,17,18]. The mechanism of injury is most often valgus stress, which may be in combination with internal rotational force and direct impact particularly in athletes [19]. In our cohort, waviness involving all or part of the superficial MCL secondary to loss of tension was present exclusively in all clinical grade III injuries, all of which had matching MRI gradings (Figs. 1, 2 and 3) [20, 21]. The deep MFL was additionally torn on MRI in the majority of patients with clinical grade III MCL injury compared with only a third of those with a clinical grade I or II injury (p < 0.05) (Table 4) (Figs. 1, 2 and 3). Likewise, tear of the deep MTL was far less common in those with lower clinical MCL injury gradings. This is consistent with the role that the deep MCL components have in providing reinforcement against valgus and rotational forces [2]. The deep MCL also plays a part in preventing anterior tibial translation in ACL deficiency [4].
A 35-year-old female with clinical grade III MCL tear. Proton density fat saturated coronal images (a, b) demonstrate a complete tear of the middle third of the superficial MCL with retraction and wavy contour of the distal torn end (thick arrows), tear and avulsion of the deep MTL at its tibial attachment (thin arrow), and associated traumatic bone marrow oedema consistent with a valgus injury mechanism laterally and deep MCL entheseal traction injury medially (arrow heads). Proton density fat saturated axial image (c) shows high-grade tear of the POL (thick arrow). Anteroposterior plain radiograph (d) reveals a displaced bony avulsion fragment originating from the deep MTL insertion at the medial tibial plateau (reverse Segond fracture). The PCL was partially torn proximally and the ACL remained intact. Treatment was surgical
A 22-year-old male with clinical grade III MCL tear. Proton density fat saturated coronal images (a, b) and proton density coronal image (c) demonstrate complete tearing of the superficial MCL with disruption at both the proximal femoral and distal tibial attachments and a wavy contour proximally (thick arrows). There is complete tear of the deep MFL and MTL which also have a wavy contour (arrow heads), and complete tear and avulsion of the POL at its medial femoral attachment (thin arrow). There was a complete tear of the ACL proximally and the PCL was partially torn. Management was non-surgical involving functional rehabilitation with a knee brace
A 26-year-old male with clinical grade III MCL tear. Proton density fat saturated coronal images (a, b) demonstrate complete tear of the superficial MCL at the tibial attachment and a wavy contour (thick arrow). There is high-grade injury of the deep MCL (arrow head) and tear of the POL at its tibial attachment (thin arrow). Proton density fat saturated coronal image (c) shows high-grade injury of the POL (thin arrow). The ACL and PCL remained intact. Management was conservative with a knee brace and physical therapy
An MCL partial or complete tear may occur in isolation, however, as supported by our findings, injuries to the ACL and medial meniscus are classically associated—together known as ‘O’Donoghue’s Triad’ [22]. We found that among patients with clinical grade III complete MCL tears the ACL was concomitantly torn to some degree on MRI in approximately the same percentage as quoted in the current literature, which is 80% [23]. Furthermore, the ACL was almost twice as frequently torn in patients with the highest clinical gradings (III) compared with those with the lowest (I) (p > 0.05), likely reflecting the severity of injury mechanisms (Table 4). Ramp lesions were also more frequent with higher clinical gradings, though the difference was not statistically significant (Table 4).
Other findings on MRI related to MCL injuries can involve the PMC and less commonly the lateral collateral ligament (LCL), lateral meniscus and posterior cruciate ligament [12, 24]. We quantified that the PMC was injured in almost half of all patients with acute MCL injury who underwent MRI and over twice as commonly in those with a clinical grade III MCL injury compared with grade I or II (p < 0.05) (Table 4) (Figs. 1, 2 and3). The five main components of the PMC are the POL, OPL, semimembranosus and its tendinous expansions (inserting at the infraglenoid tubercle of the posteromedial tibial condyle, the medial margin of the tibia, the fascia over the popliteus muscle, and the lateral femoral condyle where it forms much of the OPL), the posteromedial capsule and posterior horn of the medical meniscus. There is controversy in the literature regarding whether the POL exists as a separate entity or is instead a part of the MCL or posteromedial joint capsule. Nevertheless, the POL provides added restraint against valgus and rotational stress and its load is substantially increased after MCL tear [12]. In addition, the semimembranosus serves as a dynamic restraint to valgus force with the knee extended and restricts rotation when the knee is flexed [11]. Accompanying injury of the PMC may therefore have an effect on clinical perception of MCL instability. Almost all patients treated surgically for combined ACL and MCL injuries have a concomitant POL tear or complete PMC rupture [25].
The Cohen’s kappa coefficient suggests that the 48% rate of agreement between the radiologist and clinical raters was ‘fair’, relative to the probability of agreement occurring by chance. Other published work on this topic is from over 25 years ago. It was then shown that when radiologists considered other features in addition to the superficial MCL on MRI, they could predict the clinical classification of an MCL injury with a moderately higher 65% rate of accuracy [4]. In another study from that time, a high degree of agreement was shown between MRI grading and clinical varus-valgus laxity testing when an accompanying deep MCL tear was required to constitute an MRI grade III [26]. However, in both of these previous studies, the deep MCL was not routinely seen on MRI and image quality has since improved, also allowing more detailed characterisation of the superficial MCL [4, 26]. Increased MRI sensitivity for intrinsic signal change representing grade II partial tears may be a contributing factor to the higher rate of discrepancies between today’s clinical and MRI gradings, which we found were mainly in the MRI II vs. clinical I category (Table 1). On this note, it is also known that high signal superficial to the MCL mimicking oedema may occur due to unrelated causes, such as meniscal injury or osteoarthritis, thus increased MRI sensitivity for this high signal creates more potential for overcalling grade I MCL injury [27].
Only a small number of patients in our study had a lower radiological than clinical grading (Table 1). It is these cases which are most helpful for exploring what other features on MRI apart from the appearances of the superficial MCL might play a role in increasing the clinical grading. These cases were all MRI grade I and clinical grade II, there were none with an MRI grade I or II and a clinical grade III. The implication is that there can be perceived MCL laxity constituting a clinical grade II without the presence of intrinsic signal change within the superficial MCL which is required to raise the MRI grading from I to II. All the associated injuries we assessed for were more frequent in these patients compared with those with matching MRI and clinical gradings of I; however, the group size was not great enough for differences to be significant (Table 3). In a larger sample, this would raise the possibility that a higher energy mechanism of injury and deficiency of these ancillary structures culminates in a greater amount of instability during clinical examination of the MCL than that which would be expected based upon the MRI appearances of the superficial MCL alone. Alternatively, healing of these clinically grade II MCL injuries may have occurred during the interval between the examination and MRI scan, with subsequent resolution of the intrinsic ligamentous high signal. In comparison, more surprisingly, the previous evaluation of the accuracy of the MRI grading system found that clinical valgus instability (degree of valgus not defined) was actually most frequent among MRI grade I tears and least common in MRI grade III tears. The authors deemed that this was most likely because MCL injuries are not accurately graded with MRI imaging. Furthermore, they reported that swelling and tenderness clinically were both more prevalent in MRI grade II than grade III MCL injuries [6]. Conversely, half of all our patients had a higher MRI than clinical MCL injury grade. The majority of these were MRI grade II and clinical grade I; however, a considerable proportion were MRI grade III and clinical grade I (Table 1). It is incumbent on physicians to be aware that partial and complete tears can be present on MRI despite a clinically stable MCL, as these patients will not be appropriately put into a knee brace if management is based on examination alone. We found that the main significant difference between associated injuries on MRI in patients with MRI grade I and clinical grade I compared with MRI grade II and clinical grade I MCL injury was the higher rate of deep MFL injuries in the latter group (Table 4). Whilst this contradicts our other finding of deep MFL injuries being twice as common in clinical grade III compared to grade I MCL injuries, the variability may be because the deep MFL alone is thought to play a relatively minor role in resisting valgus strain [2]. Needless to say, it is cases with the greatest degree of grading disagreement from which there is likely the most to be learned. Among the nine with oppositely higher MRI vs. clinical grades, the main observation was that there were around half as many ACL tears and PMC injuries in these patients compared with the group that had clinical gradings matching the grade III on MRI. There was also a low proportion of medial meniscus tears in this group compared with all patients overall (Table 2). It could be speculated that the maintained integrity of these structures reduced the degree of clinical laxity which would have been expected given the complete tear of the superficial MCL demonstrated on MRI. The previous authors postulated that, as well as the inaccuracy of the MRI grading system, this type of grading disparity could be due to guarding and oedema limiting passive instability at the time of clinical examination [6].
A limitation of our study for making inferences regarding additional injuries on MRI which may predict greater or lesser instability during clinical assessment of the MCL is the small number of cases captured with disagreement between radiologist vs. clinical gradings. In particular, there were only eight patients with matching MRI and clinical grade III MCL injuries and only four patients with a lower MRI vs. clinical grading, which were all grade I vs. II respectively. Larger multicentre samples with comparisons between radiological and clinical raters are needed to better understand the meaning of our observations. A further limitation of this study is that all included cases were considered to be acute based upon the clinical history provided with the first MRI scan performed in our network and the presence of imaging features indicating recent trauma. While reasonably inferable, these factors do not guarantee that all cases were indeed an acute primary injury.
To conclude, the available data shows limited correlation between MRI and clinical gradings of acute MCL injuries when the current MRI grading system is used. We suggest that radiologists instead report the appearances of the superficial MCL on MRI using descriptive terms (‘intact’, ‘partial tear’ or ‘complete tear’) and comment on its contour, in particular any waviness as this implies loss of tension. Injuries to the deep MCL, ACL and PMC must also be assessed, because these correlate with clinical instability.
References
Andrews K, Lu A, Mckean L, Ebraheim N. Review: Medial collateral ligament injuries. J Orthop. 2017. https://doi.org/10.1016/j.jor.2017.07.017.
Liu F, Yue B, Gadikota HR, et al. Morphology of the medial collateral ligament of the knee. J Orthop Surg Res. 2010. https://doi.org/10.1186/1749-799x-5-69.
LaPrade RF, Engebretsen AH, Ly T V, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Jt Surg - Ser A. 2007. https://doi.org/10.2106/JBJS.F.01176.
Yao L, Dungan D, Seeger LL. MR imaging of tibial collateral ligament injury: comparison with clinical examination. Skeletal Radiol. 1994. https://doi.org/10.1007/BF00223082.
Major NM, Helms CA, Anderson MW, Kaplan PA, Dussault R. Musculoskeletal MRI. Musculoskelet. MRI. 2019. https://doi.org/10.1016/C2013-0-18906-4.
Schweitzer ME, Tran D, Deely DM, Hume EL. Medial collateral ligament injuries: Evaluation of multiple signs, prevalence and location of associated bone bruises, and assessment with MR imaging. Radiology. 1995. https://doi.org/10.1148/radiology.194.3.7862987.
Encinas-Ullán CA, Rodríguez-Merchán ECEC. Isolated medial collateral ligament tears: an update on management. EFORT Open Rev. 2018. https://doi.org/10.1302/2058-5241.3.170035.
Helms CA. The meniscus: Recent advances in MR imaging of the knee. Am J Roentgenol. 2002. https://doi.org/10.2214/ajr.179.5.1791115.
Chahla J, Dean CS, Moatshe G, et al. Meniscal Ramp Lesions: Anatomy, Incidence, Diagnosis, and Treatment. Orthop J Sport Med. 2016;4(7). https://doi.org/10.1177/2325967116657815.
Sandalcidi D, Dommerholt J. Deep dry needling of the hip, pelvis and thigh muscles. Trigger Point Dry Needling An Evid Clin Approach. 2013. https://doi.org/10.1016/B978-0-7020-4601-8.00010-4.
House CV, Connell DA, Saifuddin A. Posteromedial corner injuries of the knee. Clin Radiol. 2007. https://doi.org/10.1016/j.crad.2006.11.024.
Lundquist RB, Matcuk GR, Schein AJ, et al. Posteromedial corner of the knee: the neglected corner. Radiographics. 2015. https://doi.org/10.1148/rg.2015140166.
Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Jt Surg - Ser A. 1994. https://doi.org/10.2106/00004623-199409000-00008.
Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33(1). https://doi.org/10.2307/2529310.
Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006. https://doi.org/10.1016/j.knee.2006.01.005.
Paletta GA, Warren RF. Knee injuries and alpine skiing: treatment and rehabilitation. Sport Med Eval Res Exerc Sci Sport Med. 1994. https://doi.org/10.2165/00007256-199417060-00006.
LaPrade RF, Bernhardson AS, Griffith CJ, MacAlena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. 2010. https://doi.org/10.1177/0363546509349347.
Memarzadeh A, Melton JT. Medial collateral ligament of the knee: anatomy, management and surgical techniques for reconstruction. Orthop Trauma. 2019. https://doi.org/10.1016/j.mporth.2019.01.004.
LaPrade RF, Wijdicks CA. The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther. 2012. https://doi.org/10.2519/jospt.2012.3624.
Boutin RD, Fritz RC, Walker REA, Pathria MN, Marder RA, Yao L. Tears in the distal superficial medial collateral ligament: the wave sign and other associated MRI findings. Skeletal Radiol. 2020;49(5). https://doi.org/10.1007/s00256-019-03352-4.
Taketomi S, Uchiyama E, Nakagawa T, et al. Clinical features and injury patterns of medial collateral ligament tibial side avulsions: “Wave sign” on magnetic resonance imaging is essential for diagnosis. Knee. 2014;21(6). https://doi.org/10.1016/j.knee.2014.08.019.
Shelbourne KD, Nitz PA. The O’Donoghue triad revisited. Am J Sports Med. 1991. https://doi.org/10.1177/036354659101900509.
Tandogan NR, Kayaalp A. Surgical treatment of medial knee ligament injuries: Current indications and techniques. EFORT Open Rev. 2016;1(2). https://doi.org/10.1302/2058-5241.1.000007.
Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006.
DeLong JM, Waterman BR. Surgical Repair of Medial Collateral Ligament and Posteromedial Corner Injuries of the Knee: A Systematic Review. Arthrosc - J Arthrosc Relat Surg. 2015;31(11). https://doi.org/10.1016/j.arthro.2015.05.010.
Rasenberg EIJ, Lemmens JAM, van Kampen A, et al. Grading medial collateral ligament injury: comparison of MR imaging and instrumented valgus-varus laxity test-device. A prospective double-blind patient study. Eur J Radiol. 1995. https://doi.org/10.1016/0720-048X(95)00660-I.
Bergin D, Keogh C, O’Connell M, et al. Atraumatic medial collateral ligament oedema in medial compartment knee osteoarthritis. Skeletal Radiol. 2002. https://doi.org/10.1007/s002560100418.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethics committee review was not required for this retrospective observational study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watura, C., Morgan, C., Flaherty, D. et al. Medial collateral ligament injury of the knee: correlations between MRI features and clinical gradings. Skeletal Radiol 51, 1225–1233 (2022). https://doi.org/10.1007/s00256-021-03949-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03949-8