Abstract
Purpose
It is still controversial whether anteroposterior (AP) translation magnitude after total knee arthroplasty (TKA) affects clinical outcomes, particularly range of motion (ROM). This study examined the following two questions: (1) are AP translations at the mid- and long-term follow-up different for knees within the same patient treated with posterior cruciate ligament-retaining (PCLR) versus posterior cruciate ligament-substituting (PCLS) mobile-bearing TKA prosthesis designs? (2) Is the ROM at the mid- and long-term follow-up for knees treated with PCLR and PCLS designs correlated with the AP translation?
Methods
Thirty-seven patients undergoing sequential bilateral TKA for osteoarthritis were prospectively enrolled. Patients received a PCLR implant in one knee and a PCLS implant in the other and were followed-up for an average 9.8 ± 3.2 years. The AP translations at 30° and 75° of knee flexion and the ROM of both knees were assessed.
Results
The implant design (p < 0.001), but not flexion angle (n.s.), had a significant effect on AP translation. AP translation values were larger in PCLR knees than in PCLS knees at both flexion angles (p < 0.0001). The ROM at the final follow-up in the two implant designs was similar (both 115°, n.s.). There was a weak correlation between ROM and AP translation at 30° in the PCLR knees (r = 0.397, p = 0.015), but no correlation at 75° or in the PCLS knees.
Conclusions
Differently constrained prosthesis designs resulted in significantly different AP translational values within the same patient. This indicates that achieving good clinical outcomes and ROM after TKA may not be strongly influenced by the specifics of each patient’s anatomical characteristics, but instead by knee constrainment. Clinically, this means that surgeons should familiarize themselves with the AP translation of the implant being used, as this may be the most important factor for optimizing outcomes after mobile-bearing TKA.
Level of evidence II, prospective, comparative study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is still controversy over whether the magnitude of anteroposterior (AP) translation after total knee arthroplasty (TKA) affects clinical outcomes, particularly the range of motion (ROM) and maximum flexion [2, 9, 12, 14, 15, 20, 22–24, 26, 28]. This is because it is unclear whether AP translations that allow femoral rollback or sliding relative to the tibial component help prevent early impingement after roll- or slide forward between the femoral and tibial components. However, adequate AP translation values have been reported for a number of TKA prosthesis designs, as evaluated by various arthrometers under different applied forces and knee flexion angles. AP translations between 3 and 10 mm generally lead to good short- and midterm clinical outcomes after TKA [6, 7, 9, 10, 14, 16, 18, 20, 22–24, 26–28].
Because the posterior cruciate ligament (PCL) is important for controlling AP translation after TKA, many studies have compared the magnitudes of translation achieved with PCL-retaining (PCLR) and PCL-substituting (PCLS) designs [3, 6, 11, 16, 19, 25, 26]. Some studies have reported larger AP translation in PCLR designs [3, 6, 19, 25, 26], while others reported no difference [6, 11, 16]. However, all previous research on AP translation was performed on heterogeneous groups of patients. In such study designs, it is difficult to account for the variability introduced by differences in sex, age, soft tissue structures other than the PCL and PCL tension, all of which can affect post-operative AP translation. To minimize confounding biases between patients, it is important to compare the AP translations that occur after PCLR and PCLS TKA within the same patient.
Thus, the present study investigated a population in which each patient was treated with a PCLR in one knee and a PCLS in the other knee. The purpose of the present study was to determine: (1) the effect of the changes in constraint on within-patient AP translation at the mid- and long-term follow-up, and (2) whether the AP translation affects the ROM after mobile-bearing TKA using PCLR and PCLS implant designs. This is the first investigation into the effect of AP translation on ROM after mobile-bearing TKA using PCLR versus PCLS implant designs in the same patient; hence, this study will involve less confounding biases than previous reports.
Materials and methods
This prospective study was performed at our institute. Informed consent, including a description of the protocol and potential arthrometer-related complications, was obtained from all patients. There were 65 eligible patients (130 knees) who underwent bilateral, scheduled, staged TKAs with a PCLR design on one side and a PCLS design on the other using the LCS® Total Knee System (DePuy, Warsaw, IN, USA) between 1998 and 2011. Study participation was declined by 23 eligible patients, and five eligible patients were dead at the time of this study. Hence, the final total was 37 patients (74 knees).
Participants
A total of 37 patients (74 knees) were analysed, with a median follow-up time of 9.7 years (range 5.0–17.6 years) in the PCLR knees and 9.5 years (range 5.2–16.5 years) in the PCLS knees. The median interval between surgeries was 11 months (range 4–59 months), and the median patient age at the time of the last follow-up was 81 years (range 69–96 years). The preoperative diagnosis for all patients was osteoarthritis. All patients were followed for a minimum of 5 years after both knee surgeries. Patients who were treated with revision arthroplasties, previous tibial osteotomies, or for rheumatoid arthritis were excluded.
Randomization
Each patient chose which knee would undergo TKA first. The timing of the second TKA was also determined solely by the patient based on their perceived ability to tolerate the additional pain and limitations to their activities of daily living during the post-operative period. The order of implant design used was quasi-randomized: patients with even medical record numbers received the PCLR implant first, while those with odd medical record numbers received the PCLS implant first.
Treatment
The two prosthesis designs had the same geometry in the coronal plane; however, the PCLR design had non-constrained AP and rotational movement, while the PCLS design had only non-constrained rotational movement. The PCLR meniscal-bearing knee prosthesis incorporates separate medial and lateral mobile polyethylene bearings sliding independently in circularly arced keyways running anterior–posterior in the metal tibial component. This design allows unrestrained AP translation and axial rotation of the femur relative to the tibia, limited only by the periarticular tissues. Sacrifice of the PCL necessitates the use of a translationally constrained prosthesis with a single polyethylene bearing rotating in the transverse plane without constraint. The LCS® femoral component had an anatomical articulating surface, and the radius of curvature decreased posteriorly. The LCS® femoral and tibial components were fully conforming in the sagittal plane from full extension to 30° flexion and less conforming at greater flexion angles because of the decreasing radii of curvature of the femoral posterior condyles.
A single surgeon performed all of the TKA surgeries using a standardized technique, including the necessary release of soft tissues to ensure proper balance. The surgical technique and rehabilitation protocol used were described in detail in a previous paper [8]. In the flexion gap first technique, also called the balanced flexion gap technique, the proximal tibial osteotomy was performed first. Although it was not quantified intraoperatively, proper intraoperative AP stability was confirmed manually. All of the TKAs were categorized as clinically successful (Hospital for Special Surgery scores greater than 90 and the new Knee Society Knee Scoring System scores greater than 130) [1, 21] at the final follow-up. The radiographs were evaluated in accordance with the recommendations of the Knee Society [4]. The clinical characteristics of the patients are summarized in Table 1.
Outcome measures and bias
AP translation was measured using a KT-2000 arthrometer (MEDmetric Corporation, San Diego, CA, USA) following a standard protocol at 30° and 75° of knee flexion, which was confirmed with a goniometer. An anterior force of 133 N [6, 7, 9, 10, 15, 18, 19, 28] and a posterior force of 89 N [6, 7, 9, 10, 14, 15, 18, 19] were applied). All patients were instructed to relax their quadriceps and hamstrings to minimize voluntary muscular defence. The same observer performed all of the tests to eliminate interobserver variation. Total AP translation was measured three times, and the average value of the three measurements was used for analysis. The intraclass correlation coefficients (ICCs) were calculated to address test–retest reliability. The ICCs for PCLR were 0.989 (95 % CI 0.982–0.994) at 30° and 0.960 (95 % CI 0.933–0.978) at 60° of knee flexion, and the ICCs for PCLS were 0.963 (95 % CI 0.937–0.979) at 30° and 0.959 (95 % CI 0.931–0.979) at 60° of flexion.
One independent physical therapist (TS) measured the ROM of all patients using a standard hand-held goniometer with 38-cm arms. The patient rested in the supine position on the table, and the physical therapist determined the maximum passive extension and flexion under non-weight-bearing conditions. The lateral femoral condyle was used as a landmark to centre the goniometer. The proximal limb was directed towards the greater trochanter and the distal limb towards the lateral malleolus. The physical therapist then measured and recorded the angle magnitude to the nearest 5°. Finally, the ROM was calculated as the range between the extension and flexion angles. Approval for this study was obtained from the Research Board of Healthcare Corporation Ashinokai, Gyoda, Saitama, Japan (ID number: 2015-2).
Statistical analysis
A two-way ANOVA with repeated measures was used to evaluate the differences among TKA implant designs and knee flexion angles. Post-operative ROM, tibial posterior slope, and the differences between the PCLR and PCLS designs in AP translation at 30° and 75° of flexion at the final follow-up were compared using paired t tests. Additionally, Pearson correlation coefficients were used to evaluate the relationships between AP translation and the ROM at both 30° and 75° of flexion in both designs at the final follow-up. A sample size estimation was performed for the Pearson’s correlation coefficient prior to the study with a medium effect size of 0.3, an α-error of 0.05, and a power of 0.8. The minimum required sample size was estimated to be 41. Since the acquired sample size was small, we performed post hoc power analysis to evaluate the power. All values are expressed as median (25th percentile, 75th percentile). The statistical analyses were performed using IBM SPSS version 23 software (SPSS, Tokyo, Japan). p values <0.05 were considered statistically significant.
Results
There was no difference in tibial posterior slope between the designs (n.s.; Table 1). The two-way ANOVA with repeated measures showed that TKA implant design effect (p < 0.001), but not knee angle effect (n.s.), had a significant effect on AP translation. At both 30° and 75° of flexion, the AP translation values for PCLR were significantly larger than those for PCLS designs (p < 0.001 at 30°, p < 0.001 at 75°). Additionally, the differences between the PCLR and PCLS values at 30° of flexion were significantly larger than those at 75° (p = 0.006) (Table 2). Within individual knees, there were no significant differences between the AP translation magnitudes at 30° and 75° of flexion in the PCLR implants (n.s.) or the PCLS implants (n.s.) (Table 2).
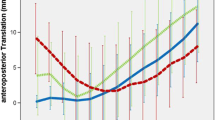
The median ROM at the final follow-up was 115° (110°, 120°) in the PCLR knees and 115° (105°, 125°) in the PCLS knees, and there was no difference between the two groups (n.s.) (Table 1). There was weak correlation between the ROM and AP translation at 30° in the PCLR knees (r = 0.397, p = 0.015), but no correlation in the PCLS knees (n.s.) (Fig. 1a, b). Similarly, there was no correlation between the ROM and AP translation at 75° in the PCLR knees (n.s.) and the PCLS knees (n.s.) (Fig. 2a, b). The post hoc power analysis for the Pearson correlation coefficient test based on a moderate effect size (r = 0.300) revealed that the power of the test was 85 % (α = 0.05).
Discussion
There were three important findings in the present study. First, good mid- and long-term clinical results indicate that mean AP translations of 7–12 mm are appropriate in both PCLR and PCLS mobile-bearing TKA design prostheses. Second, AP translation may not be strongly determined by each patient’s anatomical characteristics, but instead by the knee constrainment after TKA regardless of flexion angle; even within the same patient, higher constrainment led to less AP translation and lower constraint led to more AP translation. Third, ROM and AP translations of 7–12 mm were only significantly correlated for the PCLR knees at 30°. Moreover, while the AP translation in the PCLR knees at 30° was weakly correlated with ROM, the correlation was not significant at 75° of flexion or at either 30° or 75° in the PCLS knees.
The appropriate post-operative AP translations for a number of TKA implant designs have been reported as approximately 3–10 mm [6, 7, 9, 10, 14, 16, 18, 20, 22–24, 26–28]. The median AP translations in cases with good outcomes are consistently 7–8 mm for PCLS and 11–12 mm for PCLR implants, regardless of measurement angle. The PCLR design had non-constrained AP and rotational movement between the tibial insert and component, whereas the PCLS design had only non-constrained rotational movement between them. Additionally, because the conformity between the two components in the sagittal plane in both designs decreases with increasing flexion and the functional PCL in the PCLR design tightens with flexion [5], the AP translation may be mainly limited by the tensed PCL in the PCLR design, while the loss of conformity may be the major limitation in the PCLS design at 75° of flexion. The differences in AP translation between the PCLR and PCLS knees were significantly smaller at 75° compared with those at 30° of flexion.
Many studies have compared the AP translations among prostheses with different designs [3, 6, 11, 17, 19, 20, 25, 26], but all were based on data from heterogeneous patient populations, and hence may include unwanted bias in the measurements. AP translation can be affected by the joint geometry, soft tissue structures, and PCL tension. In contrast with previous work, the differences in AP translation recorded here are likely solely the result of the differences in the degree of constrainment provided by the two designs for the tibial insert and tray and/or retention of the PCL, as the non-PCL soft tissue structures are likely very similar within the same patient. The present results indicate that the amount of AP translation may be determined primarily by the constrainment of the knee after TKA, because the AP translation values were significantly different for the two designs within individual patients at both angles. A previous kinematics study [17] using the same designs supports our results; within-patient comparisons revealed that the AP translations in meniscal-bearing knees were larger than those in rotating-platform knees under different dynamic conditions [17].
AP translation in this study did not correlate with the ROM at the mid- and long-term follow-up, except in PCLR knees at 30° of flexion, the case with the least constraint on the soft tissues. The effects of muscular defence of the hamstrings during anterior drawer testing [13] and the tension of the retained PCL [5] are reduced at lower flexion angles. Although the AP translation in PCLR knees at 30° of approximately 12 mm were weakly correlated with the ROM, the effect was not significant at 75° or in PCLS knees. These results were obtained in patients whose TKAs were generally stable, with consistent AP translations of approximately 7–8 mm in PCLS and 11–12 mm in PCLR knees regardless of flexion angle. Therefore, our results do not indicate that larger AP translation is important to obtain better ROM. To the contrary, proper knee stability after TKA is important for good long-term post-operative knee function with both designs. Several previous studies support this result [14, 22, 23]. AP translations of 5–10 mm were reported as optimal for obtaining good functional outcomes [14, 22], and stable knees with AP translations ≤10 mm have a good functional outcome and less reduction in flexion after TKA compared with those with >10 mm [23].
There are several limitations to this study. First, the results cannot be generalized to all patients with knee arthroplasties because the study participants were patients with osteoarthritis who had stable knees, with very few outliers for either ROM or AP translations. Additionally, the sample size was relatively small, although the numbers were sufficient as indicated by the post hoc power analysis. Second, the effects of differences in geometry or soft tissue structures on AP translation through the assessment of fixed-bearing designs or single radius designs were not investigated because the scope of this study was limited to the analysis of the effects of the retention of the PCL in mobile-bearing designs. Third, there may be confounding effects of voluntary and involuntary contractions on the measured AP translations because we did not use electromyography monitoring to confirm the degree of muscle relaxation. Finally, only AP translation was measured. Although the arthrometer in this study can be used to separately measure the anterior and posterior translations, the starting position of the femoral component in relation to the tibial component varied and was not easily identifiable. In addition, this arthrometer cannot separately measure the medial and lateral translations. The assessment of ROM under load-bearing conditions may provide a better understanding of the factors influencing clinical performance during activity. However, this arthrometer is reliable, noninvasive, and widely used to evaluate AP translation. One major strength of the present study is that a single experienced surgeon treated all of the patients using the same instrumentation.
Conclusions
Differently constrained prosthesis designs resulted in significantly different AP translational values within the same patient; this indicates that achieving good clinical outcomes including ROM after TKA may not be strongly influenced by the specifics of each patient’s anatomical characteristics, but instead by knee constrainment. The findings of the current study indicate that the knee constrainment may play a more important role in AP translation than each patient’s anatomical characteristics and suggests that surgeons should recognize the optimal AP translations of the implants they typically use to optimize clinical outcomes.
References
Alicea J (2001) Scoring systems and their validation for the arthritic knee. In: Insall JN, Scott WN (eds) Surgery of the knee, vol 2, 3rd edn. Churchill Livingstone, New York, pp 1507–1515
Chouteau J, Lerat JL, Testa R, Moyen B, Banks SA (2009) Sagittal laxity after posterior cruciate ligament-retaining mobile-bearing total knee arthroplasty. J Arthroplasty 24:710–715
Dejour D, Deschamps G, Garotta L, Dejour H (1999) Laxity in posterior cruciate sparing and posterior stabilized total knee prostheses. Clin Orthop Relat Res 364:182–193
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Girgis FG, Marshall JL, Monajem A (1975) The cruciate ligaments of the knee joint: anatomical, functional and experimental analysis. Clin Orthop Relat Res 106:216–231
Ishii Y, Matsuda Y, Ishii R, Sakata S, Omori G (2005) Sagittal laxity in vivo after total knee arthroplasty. Arch Orthop Trauma Surg 125:249–253
Ishii Y, Noguchi H, Takeda M, Sato J, Sakurai T, Toyabe S (2014) In vivo anteroposterior translation after meniscal-bearing total knee arthroplasty: effects of soft tissue conditions and flexion angle. Eur J Orthop Surg Traumatol 24:967–971
Ishii Y, Noguchi H, Takeda M, Sato J, Toyabe S (2011) Prediction of range of motion 2 years after mobile-bearing total knee arthroplasty: PCL-retaining versus PCL-sacrificing. Knee Surg Sports Traumatol Arthrosc 19:2002–2008
Ishii Y, Noguchi H, Takeda M, Sato J, Toyabe S (2014) Anteroposterior translation does not correlate with knee flexion after total knee arthroplasty. Clin Orthop Relat Res 472:704–709
Ishii Y, Noguchi H, Takeda M, Kiga H, Toyabe SI (2011) Effect of voluntary soft tissue tension and articular conformity after total knee arthroplasty on in vivo anteroposterior displacement. Knee 18:11–14
Ishii Y, Terajima K, Koga Y, Takahashi HE, Bechtold JE, Gustilo RB (1995) Comparison of knee joint functional laxity after total knee replacement with posterior cruciate-retaining and cruciate-substituting prostheses. Knee 2:195–199
Itokazu M, Masuda K, Wada E, Ohno T, Yoshida M, Takatu T (2000) Influence of anteroposterior and mediolateral instability on range of motion after total knee arthroplasty: an ultrasonographic study. Orthopedics 23:49–52
Iversen BF, Sturup J, Jacobsen K, Andersen J (1989) Implications of muscular defense in testing for the anterior drawer sign in the knee: a stress radiographic investigation. Am J Sports Med 17:409–413
Jones DP, Locke C, Pennington J, Theis JC (2006) The effect of sagittal laxity on function after posterior cruciate-retaining total knee replacement. J Arthroplasty 21:719–723
Matsuda S, Miura H, Nagamine R, Urabe K, Matsunobu T, Iwamoto Y (1999) Knee stability in posterior cruciate ligament retaining total knee arthroplasty. Clin Orthop Relat Res 366:169–173
Matsuda Y, Ishii Y (2004) In vivo laxity of low contact stress mobile-bearing prostheses. Clin Orthop Relat Res 419:138–143
Mikashima Y, Ishii Y, Takeda M, Noguchi H, Momohara S, Banks SA (2013) Do mobile-bearing knee arthroplasty motions change with activity? Knee 20:422–425
Mizu-Uchi H, Matsuda S, Miura H, Nabeyama R, Okazaki K, Iwamoto Y (2006) Anteroposterior stability in posterior cruciate ligament-retaining total knee arthroplasty. J Arthroplasty 21:592–598
Nabeyama R, Matsuda S, Miura H, Kawano T, Nagamine R, Mawatari T, Tanaka K, Iwamoto Y (2003) Changes in anteroposterior stability following total knee arthroplasty. J Orthop Sci 8:526–531
Schuster AJ, von Roll AL, Pfluger D, Wyss T (2011) Anteroposterior stability after posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1113–1120
Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN (2012) The new knee society knee scoring system. Clin Orthop Relat Res 470:3–19
Seah RB, Pang HN, Lo NN, Chong HC, Chin PL, Chia SL, Yeo SJ (2012) Evaluation of the relationship between anteroposterior translation of a posterior cruciate ligament-retaining total knee replacement and functional outcome. J Bone Joint Surg Br 94:1362–1365
Seon JK, Park SJ, Yoon TR, Lee KB, Moon ES, Song EK (2010) The effect of anteroposterior laxity on the range of movement and knee function following a cruciate-retaining total knee replacement. J Bone Joint Surg Br 92:1090–1095
Seon JK, Song EK, Yoon TR, Bae BH, Park SJ, Cho SG (2007) In vivo stability of total knee arthroplasty using a navigation system. Int Orthop 31:45–48
Walker PS, Ambarek MS, Morris JR, Olanlokun K, Cobb A (1995) Anterior-posterior stability in partially conforming condylar knee replacement. Clin Orthop Relat Res 310:87–97
Warren PJ, Olanlokun TK, Cobb AG, Walker PS, Iverson BF (1994) Laxity and function in knee replacements: a comparative study of three prosthetic designs. Clin Orthop Relat Res 305:200–208
White SH, O’Connor JJ, Goodfellow JW (1991) Sagittal plane laxity following knee arthroplasty. J Bone Joint Surg Br 73:268–270
Yamakado K, Kitaoka K, Yamada H, Hashiba K, Nakamura R, Tomita K (2003) Influence of stability on range of motion after cruciate-retaining TKA. Arch Orthop Trauma Surg 123:1–4
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ishii, Y., Noguchi, H., Sato, J. et al. Anteroposterior translation and range of motion after total knee arthroplasty using posterior cruciate ligament-retaining versus posterior cruciate ligament-substituting prostheses. Knee Surg Sports Traumatol Arthrosc 25, 3536–3542 (2017). https://doi.org/10.1007/s00167-016-4257-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4257-0