Abstract
Purpose
Allografts are frequently used for anterior cruciate ligament (ACL) reconstruction. However, due to the inherent risk of infection, a method that achieves complete sterilization of grafts is warranted without impairing their biomechanical properties. Fractionation of electron beam (FEbeam) irradiation has been shown to maintain similar biomechanical properties compared to fresh-frozen allografts (FFA) in vitro. Therefore, aim of this study was to evaluate the biomechanical properties and early remodelling of grafts that were sterilized with fractionated high-dose electron beam irradiation in an in vivo sheep model.
Methods
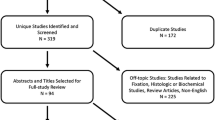
ACL reconstruction was performed in 18 mature merino mix sheep. Sixteen were reconstructed with allografts sterilized with FEbeam irradiation (8 × 3.4 kGy) and two with FFA. Eight FFA from prior studies with identical surgical reconstruction and biomechanical and histological analyzes served as controls. Half of the animals were sacrificed at 6 and 12 weeks, and biomechanical testing was performed. Anterior–posterior laxity (APL) was assessed with an AP drawer test at 60° flexion, and load to failure testing was carried out. Histological evaluation of mid-substance samples was performed for descriptive analysis, cell count, crimp and vessel density. For statistical analysis a Kruskal–Wallis test was used for overall group comparison followed by a Mann–Whitney U test for pairwise comparison of the histological and biomechanical parameters.
Results
Biomechanical testing showed significantly decreased stiffness in FEbeam compared to FFA at both time points (p ≤ 0.004). APL was increased in FEbeam compared to FFA, which was significant at 6 weeks (p = 0.004). Median of failure loads was decreased in FEbeam grafts, with 12 reconstructions already failing during cyclic loading. Vessel density was decreased in FEbeam compared to FFA at both time points, with significant differences at 12 weeks (p = 0.015). Crimp length was significantly shorter in FEbeam compared to FFA at both time points (p ≤ 0.004) and decreased significantly in both groups from 6 to 12 weeks (p ≤ 0.025).
Conclusion
ACL reconstruction with fractionated Ebeam sterilization significantly alters the biomechanical properties and the early remodelling process of treated grafts in vivo. Therefore, this sterilization method cannot be recommended for clinical application. As substantial changes in the remodelling are inherent in this study, care in the rehabilitation of even low-dose sterilized allografts, used for ACL reconstruction, is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction is a common procedure in orthopaedic practice. One of the most important decisions for the surgeon to make is the right choice of graft. Although autografts have proven capable and showed good clinical outcomes, graft harvest can cause persistent pain at the harvest site and limit range of motion [16, 17]. Therefore, allograft use has significantly increased in the last decade, since it eliminates donor-site morbidity [4, 19, 36], and albeit its use is associated with higher costs it remains a viable option, especially in revision cases [10]. Of note higher failure rates of allografts have been reported especially in young patients, which seems to be predominantly due to the sterilization process as some studies reported similar failure rates comparing fresh-frozen allografts and autografts [33, 36]. Other studies showed poorer results in sterilized compared with fresh-frozen allografts [19]. One important concern of allograft use is the risk of disease transmission [18]. Unsterilized allografts have been reported as one risk factor for septic arthritis following ACL reconstruction [34]. Furthermore, the rate of postoperative infections has been reported to be significantly higher if aseptically processed allografts are used compared to irradiated allografts or autografts [6].
This highlights the need for an effective sterilization technique that provides complete pathogen inactivation, while maintaining the graft’s mechanical competence. Currently, irradiation is the most commonly used sterilization method for tendon allografts, while different irradiation sources like gamma or electron beam (Ebeam) are available [7, 8, 30]. However, clinical as well as animal studies have shown significantly reduced biomechanical properties of grafts treated with gamma or Ebeam irradiation at the levels of more than 25 kGy [27, 29], which are necessary to effectively inactivate all pathogens including resistant viruses like HIV [9, 20]. Furthermore, inferior results following ACL reconstruction were also reported after low-dose gamma irradiation, which is currently used for allograft processing [19].
The impairment of biomechanical properties is thought to be caused by collagen crosslink breaks and collagen fragmentation due to free radicals also known as direct and indirect effects of irradiation [7]. As the number of formed radicals increases with increase in the irradiation dose, fractionation of a 34 kGy dose into 10 fractions of 3.4 kGy was evaluated, which preserved the biomechanical properties of human patellar tendon grafts in vitro [13]. Additionally oxygen-free conditions at low temperatures have been advocated to reduce radical density in vitro and hence reduce the break of crosslinks in the collagen structure and diminish the reaction with water molecules, respectively [7].
However, to our knowledge, no data exist on the in vivo performance of grafts sterilized with this method. Therefore, as the next logical step, the aim of the current study was to analyze the mechanical properties and remodelling of the ACL allograft treated with fractionated Ebeam (FEbeam) irradiation during short-term healing in an in vivo sheep model. We hypothesized that FEbeam treatment can provide complete tissue sterility without impairing the biomechanical properties of the grafts.
If proven effective, this new sterilization technique could be used clinically in future and not only provide ACL grafts with significantly reduced infection rates, but also eliminate the complications of the donor-site morbidity, effectively leading to the more cost-effective and clinically sound medical treatment.
Materials and methods
In this study, ACL replacement was performed in 18 mature female merino sheep minimum 2.5 years of age. All animals were checked for age by dental status and general health by a veterinarian doctor.
Sixteen sheep received a FEbeam 8 × 3.4 kGy sterilized ACL allograft and were sacrificed after 6 or 12 weeks (each n = 8). Two animals received an ACL replacement with non-sterilized fresh-frozen allograft (FFA) and were sacrificed after 12 weeks. Additional 18 FFA results from previous studies (each time point n = 9) were included as control group [25, 27].
All experiments were approved by our national authorities (G 0023/12) and carried out according to the policies and procedures established by the Animal Welfare Act, the NIH Guide for Care and Use of Laboratory Animals, and the national welfare guidelines.
Graft harvesting and sterilization
We used M. flexor digitales superficialis tendons for ACL reconstruction as a model for human hamstring tendons as described in our previous studies [25, 27]. Grafts were harvested aseptically under operation room conditions from sheep of previous studies with matching age, weight and sex. After sterile harvesting, grafts were rinsed with saline, individually packaged in gas-impermeable sterilization bags in an accredited authorized tissue bank facility (DIZG German Institute of Cell and Tissue Replacement, Berlin, Germany) and stored frozen at −80 °C until sterilization. Before sterilization graft packages were filled with CO2 to create nearly oxygen-free conditions (concentration ≤2 %). Sterilization was performed in polystyrene boxes on dry ice maintaining a temperature of −78 °C using eight serial cycles of 3.4 kGy Ebeam at an authorized irradiation facility (Synergy Health Radeberg GmbH, Radeberg, Germany) (Fig. 1) [13]. Average duration of each irradiation cycle was 30 s. Grafts were then stored at −20 °C until the day of surgery, when they were thawed at room temperature, prepared with baseball-stitch technique and soaked in sterile isotonic NaCl as described before [27].
ACL replacement
General anaesthesia was initiated with an intravenous injection of thiopental (Trapanal 15 mg/kg). After intubation, anaesthesia was maintained with isoflurane and nitric oxide. Due to the missing analgesic impact of isoflurane, fentanyl was administered intravenously as bolus injection (5 µg/kg each 30–45 min) for pain relief. Furthermore, animals received single-shot antibiotic treatment (Unacid®; ampicillin + sulbactam 3 g) and fluid administration (Sterofundin®). The flexor tendons were harvested from all animals before the ACL reconstruction, according to the established protocol from previous studies [25, 27].
For ACL replacement, an open arthrotomy was performed using a medial parapatellar approach. The ACL was cut at its femoral and tibial insertion sites and harvested for histological evaluation. Femoral and tibial insertion sites were identified, and the bone tunnels were placed in the middle of anteromedial and posterolateral bundle. Femoral attachment was achieved with an Endobutton (Smith and Nephew, Andover USA), and tibial fixation was achieved with sutures knotted over a bone bridge. After femoral fixation, knees were flexed and extended several times under maximum tension, to achieve proper bone contact to the Endobutton. Finally, the tibial fixation was performed at full extension under maximum manual tension. After joint lavage, the correct positioning of the graft was checked, the wound was closed in layers and the leg was bandaged for the first 3 days.
Postoperative treatment
Animals were examined daily for the first week, and general condition, body temperature and gait pattern were documented. For pain relief, animals received a fentanyl patch (2 µg/(kg*h)) and Finadyne® (flunixin 1.5 mg/kg s.c.) for the first 3 days. Full weight bearing was allowed from the first day after surgery, although animals were housed in smaller cages in groups of two for the first 3 days to reduce activity. After 14 days, the stitches were removed and animals were housed at an outdoor facility.
Sacrifice, graft harvesting and evaluation
After 6 and 12 weeks, animals each were sacrificed with an intravenous injection of an overdose of thiopental and potassium chloride. Gait pattern, macroscopic joint appearance and range of motion were evaluated prior to sacrifice. After macroscopic evaluation, the joint was opened and examined for adhesions, swelling, effusion or other signs of inflammation. Afterwards, biomechanical testing was performed using biomechanical testing machine (model 1455, Zwick, Germany) as described previously [25]. Briefly, the femur and tibia were potted in poly-methylmethacrylate and mounted on aluminium clamps for fixation in the mechanical testing machine. Two loading conditions were simulated: anterior–posterior laxity (APL) was assessed with an AP drawer test at 60° flexion, during sub-maximal cyclic loading (±50 N) applied perpendicular to the longitudinal axis of the tibia for 10 cycles with a strain rate of 120 mm/min. Load to failure testing (LFT) was carried out with the load applied in line with the ACL graft, and stiffness (ST) was calculated from the load to failure curve.
After biomechanical evaluation, midsubstance samples of an intraarticular part of the graft were harvested for histological analysis. Samples were fixed in formalin 4 %, automatically dehydrated and embedded in paraffin. Cross and longitudinal 4-µm sections were prepared and stained with haematoxylin–eosin following standard histological protocols for descriptive analysis, cell counting and crimp evaluation (longitudinal sections). For descriptive analysis, samples were analyzed with light and polarized microscopy with 5×, 10×, 20× and 40× magnification. Cells were counted in longitudinal sections in 10 randomly chosen representative regions of interest distributed over all parts of the graft (peripheral, middle and central) with a magnification of 20×, and the cell number/mm2 was calculated. To analyze the tertiary collagenous structure, the collagen crimp (wavelength of collagen fibrils) was analyzed under polarized light using the same regions of interest as those used for the cell counting. The distance between two consecutive peaks of the respective fibrils was defined as crimp length, which was reported as an average of all crimp lengths measured. For vessel detection, cross sections were stained with a factor VIII antibody as described elsewhere [23]. Vessels were counted in 14 regions of interest representing the subsynovial, the midsubstance and central region of the grafts with magnification 20×, and vessel density (vessels/mm2) was calculated. Additionally to the two control animals for 12 weeks time point, results from fresh-frozen allografts (FFA) from a previous study served as controls [25]. All animal procedures were conducted according to the guidelines of the National Institute of Health for the use of laboratory animals. The experiments were approved by our national authorities (Langesamt für Gesundheit und Soziales, Berlin, Germany, reference number: G 0023/12).
Statistical analysis
Due to nonparametric data distribution, Kruskal–Wallis test was used for overall group comparison followed by a Mann–Whitney U test for pairwise comparison of the histological (cellularity, vessel density, crimp) and biomechanical parameter (stiffness, AP laxity) between FEbeam and fresh-frozen allografts of the respective time points (6 and 12 weeks) and between both time points in one group. Data were corrected by Bonferroni–Holm correction. Statistical significance level was set at p < 0.05. The number of specimens used in this study was determined by performing a power analysis on preliminary data to estimate the required sample size to ensure 80 % power (α = 0.05; β = 0.2).
Results
All animals tolerated the surgeries well. No infections or other complications were observed after surgery. On the day of sacrifice, all animals showed a physiological gait pattern and full range of joint motion as well as unremarkable surgical wounds.
Biomechanical testing showed significantly decreased stiffness in FEbeam compared to FFA at both time points (p ≤ 0.004). APL was increased in FEbeam compared to FFA which was significant after 6 weeks (p = 0.004) (Fig. 2).
Although macroscopically grafts appeared mature and intact, load to failure test after 6 weeks was only possible in three out of eight grafts in FEbeam, due to early failure of five grafts during cyclic loading, whereas full testing was possible in FFA in all animals. Median of the failure load of the three grafts was decreased in FEbeam compared to the FFA group (Table 1).
After 12 weeks, all grafts failed due to intraligamentous rupture (Fig. 3). Just as with 6-weeks grafts, in FEbeam most specimens failed during cyclic loading test, so only one specimen underwent load to failure testing, which showed less than half of the failure load compared to FFA group after 12 weeks where testing was completed in all animals (Table 1).
Histological evaluation revealed predominant tissue necrosis after 6 weeks in both investigation groups. Fresh-frozen allografts showed a beginning repopulation of cells and ingrowth of small blood vessels starting from the subsynovial region. In the FEbeam group, variable results were observed. While in some samples the whole tissue was necrotic, others showed an increased cellularity compared to the FFA at this time point. Collagen orientation was mainly irregular especially in regions with higher cell density. Cell nuclei were mostly spindle shaped in both groups.
After 12 weeks, an ongoing remodelling was visible in both groups. In FFA, cells and vessels mainly were embedded in strands of connective tissue which grew in from peripheral to central parts of the grafts. However, central parts of the grafts still remained acellular. In FEbeam, cellularity was more homogenous also in central parts of the graft with some ovoid- but mostly spindle-shaped cells. Collagen orientation was mainly irregular in both groups in all regions of the tissue.
Cell counting (Fig. 4) revealed a significantly increased cell density from 6 to 12 weeks in both groups (p ≤ 0.048), which was more pronounced in FEbeam as in the FFA.
H&E staining after 6 weeks showed a beginning of repopulation in FEbeam (a) as well as in FFA (c). From 6 to 12 weeks, cell density significantly increased in both groups, which was more pronounced in FEbeam (b) compared to FFA (d). Magnification ×20. Mann–Whitney U test, Bonferroni–Holm correction, p ≤ 0.05, #means significant to FFA of the resp. time point, *means significant to other timepoint of same group
Vessel density (Fig. 5) was decreased in FEbeam compared to FFA at both time points, which was significant after 12 weeks (p = 0.015). While vessel density significantly increased in FFA from 6 to 12 weeks (p = 0.026), only a slight increase was seen in FEbeam.
Factor VIII vessel detection showed a beginning of revascularization from the periphery in FEbeam (a) as well as in FFA (c) after 6 weeks with lower vessel density in FEbeam. After 12 weeks, vessel density in FFA (d) was significantly increased and vessels were found up to the central parts of the grafts whereas in FEbeam grafts (b) only a small increase in vessel density with predominant large vessels was found. Magnification ×20/×10 (c)
Crimp length (Fig. 6) was significantly shorter in FEbeam compared to FFA after both time points (p ≤ 0.004) and decreased significantly in both groups from 6 to 12 weeks (p ≤ 0.025).
Analysis with polarized light showed a mainly irregular collagen crimp in the peripheral regions in both groups after 6 weeks (a, c). After 12 weeks, collagen crimp became more orientated in both groups (d FFA) with great variances in the FEbeam group (b) showing well-orientated regions as well as highly disorganized structure in more cellularized regions of the grafts (c). In general, crimp was shorter in FEbeam compared to FFA. Magnification ×20
Discussion
The most important finding of this study was that the use of fractionated Ebeam irradiation for ACL reconstruction resulted in significant impairment of biomechanical properties compared to fresh-frozen allografts during the early remodelling.
Significant impairment has been reported for high irradiation dosages >30 kGy; therefore, current sterilization methods utilize low-dose irradiation between 10 and 20 kGy [20]. Additionally, tissue banks use specific donor screening, aseptic handling, antibiotic solutions or irradiation to reduce the risk of disease transmission or infection. However, since these treatment options cannot assure graft sterility, governmental regulations restrict allograft use in many countries, thereby limiting supply of appropriate material for ACL surgeries [21].
As a consequence, significant efforts have been made to develop alternative sterilization methods that achieve complete graft sterility without affecting biomechanical properties [22, 24, 31, 32, 35].
Ebeam irradiation has been shown to be an effective alternative to gamma radiation, as dosages can be more accurately controlled and irradiation time is significantly decreased, while achieving similar efficacy of pathogen inactivation [8, 28]. Ebeam irradiation has also been shown to have less detrimental effects on the biomechanical properties of soft tissue grafts compared to gamma irradiation, even though significant reduction is still inherent with high-dose irradiation [8, 14, 15]. Furthermore, fractionation of dosages to decrease tissue damage, similar to irradiation of tumours in oncology, has been used for soft tissue grafts and has shown to retain biomechanical properties in vitro, while achieving sterility of grafts [13, 28, 35].
A possible explanation for this effect is the decrease in radical formation due to fractionation, as the number of primary radicals is directly related to the irradiation dose and the material-specific number of charged molecules per 100 eV absorbed energy [5]. Free oxygen radicals that are released during tissue radiation break collagen crosslinks and trigger chemical reactions leading to structural changes of polymers [7]. Both direct and indirect radiation effects might account for the slightly decreased mechanical properties in vitro [14].
The effect of radicals was confirmed by a study of Seto et al. [31] who found improved biomechanical properties of 50 kGy Ebeam or gamma-irradiated tendons after pretreatment with a radical scavenger compared to untreated controls. However, since radical scavengers might influence the sterilization process [1], reduction in radical formation and hence undesired chemical side reactions with oxygen and water were achieved by adapting the sterilization parameter in the current study. Sterilization at low temperature (−79 °C) in the absence of oxygen reduces the mobility of molecules, and fractionated dose application yields in reduced radical formation which finally should decrease the breakage of polymer graft-links and crosslinks and therefore help to maintain mechanical graft properties [3].
It is well known that radicals can be trapped at low temperature. In the case of polymers, this effect occurs if the irradiation and the sample storage were done at temperatures below the glass transition temperature. It is possible that after specimens were thawed, some residual radicals were present and reacted with sterile isotonic NaCl, water or other molecules. These post-sterilization reactions might result in additional structural changes (degradation, break of crosslinks, etc.) of the biomolecules influencing the biomechanical properties of the grafts.
Seto et al. [32] evaluated the impact of radioprotection on functional mechanics in a sheep model. They also found delayed healing with an increased cellularity and decreased biomechanical properties in radioprotected grafts and attributed this to prolonged graft healing in the bone tunnel [32].
Although we did not analyze tendon to bone healing histologically, we have to assume that predominantly intraarticular graft healing was affected by the irradiation as after 12 weeks all grafts failed due to intraligamentous rupture in this study, similar to the findings of previous studies for autografts and fresh-frozen allografts [25].
However, we also found increased cell density as well as a decreased crimp length in FEbeam compared to FFA at both time points, with significant differences for crimp pattern at 6 weeks. This was also found by Scheffler et al. [23] using the same animal model. They analyzed the effect of thermal shrinkage on the remodelling of an elongated ACL and found a similar crimp pattern accompanied by an increased cell density in their grafts [23]. They assumed that this could be due to an accelerated but immature remodelling process, which caused the reduced biomechanical properties of those grafts [23]. Macroscopically, the grafts in our study appeared smooth and weak after 12 weeks indicating a loss of tissue structure. The reduced vessel density also confirms the delayed remodelling process.
In the current study, the number of cells increased twofold in irradiated grafts at 12 weeks, but collagen orientation was irregular. Therefore, further reasons for alterations in the remodelling might be a more pronounced apoptosis of cells leading to a higher amount of tissue necrosis. Also an irregular orientation of collagen might inhibit an organized repopulation and remodelling of cells, which further decreases the biomechanical strength. Amiel et al. [2] demonstrated predominant collagen type III fibrils during the first 6 weeks in ACL autograft reconstruction, while the normal ACL consists predominantly of type I collagen. The relative proportion of collagen I/III increased after 30 weeks implying a slow maturation of collagen. Also, distribution of larger and smaller collagen fibres and higher crosslink rates have been proposed to indicate collagen maturation and hence increased biomechanical properties [11]. As crosslinks are destroyed due to irradiation, this process might be delayed in irradiated allografts. This is consistent with other studies, which reported a restoration of the inherent initial impairment of tensile strength [12]. However, as we only evaluated graft healing at 6 and 12 weeks without evaluation of crosslink density, we were not able to conclude whether restoration of graft properties would be observed at extended healing times. Further research on the effects of radiation on the remodelling process is needed to clarify the underlying mechanisms.
There are some more limitations to this study, as we only performed H&E staining, which did not allow for differentiation between inflammatory cells, cytokines or other cell types. Therefore, the cause of the increased cell count in this study cannot be identified. Also, time-dependent differences exist in soft tissue remodelling between sheep and humans and, therefore, the results might be different in humans [26]. Furthermore, controls from a different study might yield different results. However, both studies were performed under the same settings and methodology, so that differences should be minimized. Despite these limitations, our results show that sterilization using a fractionated dose application for irradiation does not prevent allograft tissue damage.
With current rehabilitation protocols for ACL reconstruction aiming for immediate return to full weight bearing and restoration of full range of motion to achieve normal lower extremity function, loading of the graft tissue must be expected that might not be sustained by the impaired biomechanical properties found in this study.
As most allografts in clinical use are at least low-dose-sterilized, it has to be assumed that similar changes in the remodelling are existent in these grafts as well. Therefore, it should be taken into account for the rehabilitation protocol after ACL replacement with sterilized allografts, especially in the first 12 weeks.
To our knowledge, this is the first study to report about in vivo application of fractionated sterilization. Although previous in vitro testing showed significantly better biomechanical results after fractionated compared to single high-dose Ebeam irradiation, both treatments significantly altered the biomechanical properties of soft tissue allograft during the early remodelling in an in vivo sheep model. Thus, further investigations are required in order to study post-sterilization effects in FEbeam sterilization.
Conclusion
Based on the results of the present study, even fractionated high-dose Ebeam irradiation cannot be recommended for sterilization of soft tissue grafts in ACL reconstruction due to the substantial impairment of graft’s mechanical properties during the early remodelling.
References
Akkus O, Belaney RM, Das P (2005) Free radical scavenging alleviates the biomechanical impairment of gamma radiation sterilized bone tissue. J Orthop Res 23:838–845
Amiel D, Kleiner JB, Akeson WH (1986) The natural history of the anterior cruciate ligament autograft of patellar tendon origin. Am J Sports Med 14:449–462
Bailey AJ, Rhodes DN, Cater CW (1964) Irradiation-induced crosslinking of collagen. Radiat Res 22:606–621
Bottoni CR, Smith EL, Shaha J, Shaha SS, Raybin SG, Tokish JM, Rowles DJ (2015) Autograft versus allograft anterior cruciate ligament reconstruction: a prospective, randomized clinical study with a minimum 10-year follow-up. Am J Sports Med 43:2501–2509
Burton M (1947) Effects of high-energy radiation on organic compounds. J Phys Colloid Chem 51:786–797
Crawford C, Kainer M, Jernigan D, Banerjee S, Friedman C, Ahmed F, Archibald LK (2005) Investigation of postoperative allograft associated infections in patients who underwent musculoskeletal allograft implantation. Clin Infect Dis 41:195–200
Dziedzic-Goclawska A, Kaminski A, Uhrynowska-Tyszkiewicz I, Stachowicz W (2005) Irradiation as a safety procedure in tissue banking. Cell Tissue Bank 6:201–219
Elenes EY, Hunter SA (2014) Soft-tissue allografts terminally sterilized with an electron beam are biomechanically equivalent to aseptic, nonsterilized tendons. J Bone Joint Surg Am 96:1321–1326
Fideler BM, Vangsness CT Jr, Moore T, Li Z, Rasheed S (1994) Effects of gamma irradiation on the human immunodeficiency virus. A study in frozen human bone-patellar ligament-bone grafts obtained from infected cadavera. J Bone Joint Surg Am 76:1032–1035
Genuario JW, Faucett SC, Boublik M, Schlegel TF (2012) A cost-effectiveness analysis comparing 3 anterior cruciate ligament graft types: bone-patellar tendon-bone autograft, hamstring autograft, and allograft. Am J Sports Med 40:307–314
Goertzen MJ, Buitkamp J, Clahsen H, Mollmann M (1998) Cell survival following bone-anterior cruciate ligament-bone allograft transplantation: DNA fingerprints, segregation, and collagen morphological analysis of multiple markers in the canine model. Arch Orthop Trauma Surg 117:208–214
Goertzen MJ, Clahsen H, Burrig KF, Schulitz KP (1995) Sterilisation of canine anterior cruciate allografts by gamma irradiation in argon. Mechanical and neurohistological properties retained one year after transplantation. J Bone Joint Surg Br 77:205–212
Hoburg A, Keshlaf S, Schmidt T, Smith M, Gohs U, Perka C, Pruss A, Scheffler S (2011) Fractionation of high-dose electron beam irradiation of BPTB grafts provides significantly improved viscoelastic and structural properties compared to standard gamma irradiation. Knee Surg Sports Traumatol Arthrosc 19:1955–1961
Hoburg A, Keshlaf S, Schmidt T, Smith M, Gohs U, Perka C, Pruss A, Scheffler S (2015) High-dose electron beam sterilization of soft tissue grafts maintains significantly improved biomechanical properties compared to standard gamma treatment. Cell Tissue Bank 16:219–226
Hoburg AT, Keshlaf S, Schmidt T, Smith M, Gohs U, Perka C, Pruss A, Scheffler S (2010) Effect of electron beam irradiation on biomechanical properties of patellar tendon allografts in anterior cruciate ligament reconstruction. Am J Sports Med 38:1134–1140
Kartus J, Magnusson L, Stener S, Brandsson S, Eriksson BI, Karlsson J (1999) Complications following arthroscopic anterior cruciate ligament reconstruction. A 2–5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc 7:2–8
Kartus J, Movin T, Karlsson J (2001) Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 17:971–980
Mroz TE, Joyce MJ, Steinmetz MP, Lieberman IH, Wang JC (2008) Musculoskeletal allograft risks and recalls in the United States. J Am Acad Orthop Surg 16:559–565
Park SS, Dwyer T, Congiusta F, Whelan DB, Theodoropoulos J (2015) Analysis of irradiation on the clinical effectiveness of allogenic tissue when used for primary anterior cruciate ligament reconstruction. Am J Sports Med 43:226–235
Pruss A, Kao M, Gohs U, Koscielny J, von Versen R, Pauli G (2002) Effect of gamma irradiation on human cortical bone transplants contaminated with enveloped and non-enveloped viruses. Biologicals 30:125–133
Pruss A, von Versen R (2007) Influence of European regulations on quality, safety and availability of cell and tissue allografts in Germany. Handchir Mikrochir Plast Chir 39:81–87
Raviraj J, Bokkasam VK, Kumar VS, Reddy US, Suman V (2014) Radiosensitizers, radioprotectors, and radiation mitigators. Indian J Dent Res 25:83–90
Scheffler S, Chwastek H, Schonfelder V, Unterhauser F, Hunt P, Weiler A (2005) The impact of radiofrequency shrinkage on the mechanical and histologic properties of the elongated anterior cruciate ligament in a sheep model. Arthroscopy 21:923–933
Scheffler SU, Gonnermann J, Kamp J, Przybilla D, Pruss A (2008) Remodeling of ACL allografts is inhibited by peracetic acid sterilization. Clin Orthop Relat Res 466:1810–1818
Scheffler SU, Schmidt T, Gangey I, Dustmann M, Unterhauser F, Weiler A (2008) Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy 24:448–458
Scheffler SU, Unterhauser FN, Weiler A (2008) Graft remodeling and ligamentization after cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 16:834–842
Schmidt T, Hoburg A, Broziat C, Smith MD, Gohs U, Pruss A, Scheffler S (2012) Sterilization with electron beam irradiation influences the biomechanical properties and the early remodeling of tendon allografts for reconstruction of the anterior cruciate ligament (ACL). Cell Tissue Bank 13:387–400
Schmidt T, Hoburg AT, Gohs U, Schumann W, Sim-Brandenburg JW, Nitsche A, Scheffler S, Pruss A (2012) Inactivation effect of standard and fractionated electron beam irradiation on enveloped and non-enveloped viruses in a tendon transplant model. Transfus Med Hemother 39:29–35
Schwartz HE, Matava MJ, Proch FS, Butler CA, Ratcliffe A, Levy M, Butler DL (2006) The effect of gamma irradiation on anterior cruciate ligament allograft biomechanical and biochemical properties in the caprine model at time zero and at 6 months after surgery. Am J Sports Med 34:1747–1755
Seto A, Gatt CJ Jr, Dunn MG (2008) Radioprotection of tendon tissue via crosslinking and free radical scavenging. Clin Orthop Relat Res 466:1788–1795
Seto A, Gatt CJ Jr, Dunn MG (2009) Improved tendon radioprotection by combined cross-linking and free radical scavenging. Clin Orthop Relat Res 467:2994–3001
Seto AU, Culp BM, Gatt CJ Jr, Dunn M (2013) Radioprotection provides functional mechanics but delays healing of irradiated tendon allografts after ACL reconstruction in sheep. Cell Tissue Bank 14:655–665
Tejwani SG, Chen J, Funahashi TT, Love R, Maletis GB (2015) Revision risk after allograft anterior cruciate ligament reconstruction: association with graft processing techniques, patient characteristics, and graft type. Am J Sports Med 43:2696–2705
Wee J, Lee KT (2014) Graft infection following arthroscopic anterior cruciate ligament reconstruction: a report of four cases. J Orthop Surg 22:111–117
Wei W, Liu Y, Yang X, Tian S, Liu C, Zhang Y, Xu Z, Hu B, Tian Z, Sun K (2013) Fractionation of 50 kGy electron beam irradiation: effects on biomechanics of human flexor digitorum superficialis tendons treated with ascorbate. J Biomech 46:658–661
Zeng C, Gao SG, Li H, Yang T, Luo W, Li YS, Lei GH (2016) Autograft versus allograft in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy 32(1):153–163e18
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmidt, T., Grabau, D., Grotewohl, J.H. et al. Does sterilization with fractionated electron beam irradiation prevent ACL tendon allograft from tissue damage?. Knee Surg Sports Traumatol Arthrosc 25, 584–594 (2017). https://doi.org/10.1007/s00167-016-4240-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4240-9