Abstract
Purpose
To investigate the effectiveness of isolated eccentric versus conventional exercise therapy in patients with rotator cuff tendinopathy.
Methods
Thirty-six patients with rotator cuff tendinopathy, diagnosed by an orthopaedic surgeon, were included and randomly allocated to an isolated eccentric exercise (EE) group (n = 20, mean age = 50.2 ± 10.8 years) or a conventional exercise (CG) group (n = 16, mean age = 48.6 ± 12.3 years). Both groups fulfilled a 12-week daily home-based exercise programme and received a total amount of nine treatment sessions. The Constant Murley score was used to evaluate both objective (e.g. range of motion and strength) and subjective measures (e.g. pain and activities of daily living). A visual analogue scale (VAS) was used to evaluate pain during daily activities. As secondary outcomes, shoulder range of motion and isometric abduction strength in 45° in the scapular plane were evaluated. All measurements were taken at baseline, at 6, 12 and 26 weeks.
Results
After 26 weeks, both groups showed a significant increase in the Constant Murley score and a significant decrease in VAS scores. No difference was found between the groups, for any of the evaluated outcome measures.
Conclusion
A 12-week-isolated eccentric training programme of the rotator cuff is beneficial for shoulder function and pain after 26 weeks in patients with rotator cuff tendinopathy. However, it is no more beneficial than a conventional exercise programme for the rotator cuff and scapular muscles. Based on the results, clinicians should take into account that performing two eccentric exercises twice a day is as effective as performing six concentric/eccentric exercises once a day in patients with rotator cuff tendinopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shoulder pain is a common complaint in primary care in the Netherlands. The incidence has been estimated to be 19 per 1000 persons per year [14].
Rotator cuff tendinopathy (RC tendinopathy) is often referred to as “subacromial impingement syndrome”, which is a commonly used term for patients presenting with anterior shoulder pain [19]. Neer introduced the term impingement in the early 70s in order to describe a clinical condition in which shoulder pain was believed to derive from bony compression of the tendons of the rotator cuff (RC) and bursa in the subacromial space [2]. However, in recent literature, several authors recommend to use the term “anterior shoulder pain” or “subacromial pain syndrome” (SAPS) instead of impingement, since the anatomical explanation seems insufficient to describe this painful, complex condition that involves both intrinsic and extrinsic mechanisms of RC tendinopathy [5, 11, 18].
Extrinsic mechanisms of RC tendinopathy in the painful shoulder consist of both anatomical and biomechanical factors [13]. Anatomical factors are decreased acromiohumeral distance, shape of the acromion, presence of large subacromial spurs, thickening of the coracoacromial ligament and arthritic changes in the acromioclavicular joint [2, 23].
Biomechanical factors are changes in glenohumeral and scapula-thoracic muscle performance, altered shoulder kinematics, poor posture, tightness of posterior shoulder tissues and the pectoralis minor muscle [7, 20], and myofascial trigger points associated with altered kinematics of the glenohumeral and scapula-thoracic joint [6].
Intrinsic mechanisms of RC tendinopathy comprise tendon morphology and performance that might result in degeneration, poor vascularity, altered biology and inferior mechanical properties [26, 30]. Both extrinsic and intrinsic mechanisms can overlap, particularly in patients with chronic RC tendinopathy. For example, patients with an intrinsic RC tendinopathy based on degenerative changes may develop decreased RC and scapular muscle performance and altered kinematics in the glenohumeral and scapula-thoracic joints [30].
Exercise therapy is an accepted treatment for patients with various tendinopathies [15, 22]. Previous studies have shown that eccentric training was effective in terms of symptom reduction and improved function in patients with Achilles and patellar tendinopathy, but it may also restore tendon tissue structure [1, 24]. Moreover, recent literature concerning Achilles tendinopathy indicates that one of the underlying potential mechanisms for eccentric training is a change in neuromuscular output [25]. The changes necessary for benefit may include increased muscle tendon unit stiffness, increased strength and shifts in the length tension curve. It is possible that these neuromuscular changes reduce the load on the tendon by “smoothing muscle contractions” (force fluctuations) and thereby reduce maximal or accumulative tendon strain. This may affect tendon homeostasis [25].
Several studies have investigated the effectiveness of eccentric training in patients with RC tendinopathy, but to our knowledge none of these studies used an isolated eccentric exercise (EE) protocol compared with a control group. Moreover, none of the previous studies followed the participants for more than 12 weeks. Therefore, we investigated whether isolated eccentric training of the RC could be more effective than conventional exercises in patients with RC tendinopathy with a long-term follow-up of 26 weeks. The aim of this study was to compare the effectiveness of an isolated eccentric training programme combined with stretching with a conventional exercise programme, including scapular stabilization exercises, concentric RC strengthening exercises and stretching. It was hypothesized that eccentric training would be of superior value compared to conventional exercises in this population.
Materials and methods
This study was a prospective randomized participant (single)-blinded controlled trial. Randomization was performed by an independent statistician before hand using a computer generated randomization table. Equal numbers of the two treatment groups were then concealed in opaque envelopes. After inclusion and baseline assessment by the principal investigator (BD), an independent employee chose an envelope to randomly allocate the participant to one of the two treatment groups and handed the concealed envelop to the supervising therapist. Data collection and treatment sessions were performed by the principle investigator (BD), who has 17 years of experience in musculoskeletal rehabilitation and who was not blinded for group allocation at the Sports Medical Center Papendal, Arnhem, the Netherlands. Analysis of data was performed by a blinded researcher. Written informed consent was acquired for all participants prior to their participation. The study protocol was approved by the Regional Ethical Committee (Independent Review Board Nijmegen) 2007/174.
Study population
Participants were recruited from the orthopaedic department, Rijnstate Hospital, Arnhem, the Netherlands. Initially, they were referred by their general practitioner. At Rijnstate Hospital, they attended a multidisciplinary shoulder consultation during which they were successively assessed by a physiotherapist and an orthopaedic surgeon. After this consultation, the participants were referred to a musculoskeletal radiologist for X-rays and ultrasound imaging using previously reported protocols [29]. Participants suspected with RC tendinopathy were subsequently referred to the principal investigator (BD), who screened them for their eligibility. The inclusion and exclusion criteria are presented in Table 1.
Intervention
All the participants of both treatment groups performed the exercises at home on a daily basis for a total of 12 weeks. In concurrence with protocols of previous literature, the EE group performed two different exercises twice a day [16, 17]. In order to minimize differences in the total amount of exercises/repetitions, the control group (CG) performed eight different exercises once daily. Both groups attended one physiotherapy session per week during the first 6 weeks and three sessions during the last 6 weeks. The content of these physiotherapy sessions was similar for both groups and solely consisted of rehearsing the exercises and adjusting the load if possible. After 12 weeks, both groups were instructed to cease the exercises and return to perform their habitual daily activities.
The EE group performed two exercises. First, a supine lying eccentric exercise for the external rotators, with an elastic band (Duraband, Servofit) wrapped around the homolateral foot at one side and held by the patient’s hand. The shoulder was in 90° of abduction and external rotation. The participant was then asked to bend the knee, externally rotate the shoulder, and subsequently to extend the knee and to internally rotate the forearm at a speed of 6–8 s (s) per repetition. Secondly, participants performed an empty-can abduction exercise in the scapular plane. Participants elevated their arm passively with a pulley until 90° of abduction. Then, they were asked to lower their arm actively at a speed of 6–8 s per repetition. Pain during the exercise was accepted if it did not exceed a pain score of 5 on a 0–10 numerical pain rating scale [16]. If exercises could be performed without pain, load was increased by adding a dumbbell weight of 1 kg. In addition to the eccentric strengthening exercises, participants from the EE group performed stretching exercises for the pectoralis minor muscle and the cross-body adduction stretch for the posterior shoulder muscles and capsular structures (which were similar to the CG) [10].
The exercises of the CG group consisted of a dumbbell full-can abduction exercise in the scapular plane until 90° of abduction, external and internal rotation in 0° of abduction using an elastic band (Duraband, Servofit), shoulder shrugs, knee push-up with a plus, prone horizontal abduction with external rotation, stretching exercises for the pectoralis muscles and the cross-body adduction stretch [10, 12].
Both groups completed a daily journal to record their pain on a numeric pain rating scale (NPRS; range 0–10), their training compliance and/or any remarks on the exercises. Initially, exercises were performed in both groups with three sets of eight repetitions. The load was changed by first increasing the number of repetitions (to a maximum of 15 repetitions) and then subsequently by increasing resistance of the elastic band or dumbbell [17].
Outcome measures
The primary outcome measure was shoulder function as measured with the CM score [9]. The CM score has four subscales: pain (15 points), activities of daily living (20 points), range of motion (ROM) (40 points) and strength (25 points). The maximum CM score is 100 points, indicating excellent shoulder function. Research has shown that the CM score can be used in clinical and research settings and has acceptable reliability (Spearman’s ρ ≥ 0.90) [28]. However, Rocourt et al. [27] stated that this is not unconditionally.
Average pain during daily activities was measured with the visual analogue scale (VAS), which is a 100-mm horizontal line with two anchors. The left anchor represents “no pain at all”, whereas the right anchor represents “the most severe pain”. The VAS is a reliable form of measuring patient’s perceived pain level (intraclass correlation coefficient [ICC] 0.97–0.99) [31].
Other outcome measures were ROM for active forward flexion–elevation, abduction–elevation, external rotation and isometric strength measurements of the shoulder abductors. For ROM measurements, participants were seated in an active upright position without back support, with their feet on the ground and they were asked to move their humerus to the maximal range as outlined above. A goniometer was placed after the movement was performed and end-range was achieved. During abduction–elevation, the goniometer was placed at the lateral margin of the spina scapulae. The stationary arm was aligned parallel to the spine and the moving arm along the shaft of the humerus. During forward flexion–elevation, the goniometer was placed at the greater tuberosity. The stationary arm was aligned parallel to the spine and the moving arm along the shaft of the humerus. During external rotation, the olecranon was used as punctum fixum. The humerus was positioned at 0° of abduction. The goniometer then was cantered at the olecranon with the moving arm aligned with the shaft of the ulna and the stationary arm held in the sagittal plane.
Isometric strength of the shoulder abductors measured with a hand-held dynamometer (HHD; CompuFET; Hoggan Health Industries Inc, UT, USA) according to a previously reported method [21] and using the “make test” [8]. During this reliable measurement (ICC > 0.94) [3], participants were seated on a treatment bench, without back support and with their feet on the ground. They grasped the under surface of the treatment bench with their contralateral hand. The HHD was then placed distally on the humerus, and participants were asked to abduct their shoulder to 45° in the scapular plane [21]. A maximal voluntary contraction was asked during 5 s, three times in succession with a 30 s rest interval between each repetition. Peak force of each trial was registered, and the average of three trials was used for data analysis [21]. All outcome measures were performed at baseline, and after 6, 12 and 26 weeks.
This study protocol has been approved by the Independent Review Board Nijmegen, Regional Ethical Committee (registration number CMO/2007/174) and was registered in the Dutch Trial Register (number: NTR 4427).
Statistical analysis
Data were analysed on intention-to-treat basis, and missing data were imputed using the last value carried forward method. Continuous data were checked for normal distribution using PP plots and the Shapiro–Wilk test. Differences in baseline characteristics were analysed with an independent t test for continuous data and the Fisher exact test for nominal data. Differences in the CM and VAS scores from baseline to 26-week follow-up were analysed using a two-way repeated measures analysis of variance (treatment × time), with duration of symptoms as a covariate. As Mauchly’s test of sphericity was violated, the Greenhouse–Geisser correction was used. Post hoc analyses were performed to investigate the progression of the CM and VAS over time, using Bonferroni corrections. Differences in ROM and isometric strength values at 26 weeks were analysed with a paired t test for differences within each group and an independent t test for differences between the groups. All statistical analyses were performed with SPSS 22.0, with statistical significance set at α = 0.05.
Sample size calculation
Previous research has shown a mean increase of 15 points on the Constant Murley (CM) score following a 12-week eccentric exercise programme for the RC [16, 17]. Sample size was calculated a priori, using G*Power 3.1. Assuming α (two-sided) = 0.05 and 1−β = 0.80, fourteen participants were required in each group in order to detect a difference of 15 points on the CM score between the two groups.
Results
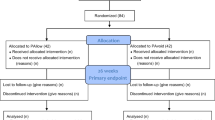
A flow diagram of the study participants, showing the inclusion process, is demonstrated in Fig. 1. A total of 41 participants were screened for eligibility, of which five did not meet the inclusion criteria. Thirty-six participants were randomly allocated to either the EE group (n = 20) or the CG group (n = 16). After 6 weeks, 36 patients were reassessed. Thirty-four participants completed the 12-week and 26-week follow-up measurements (EE group: n = 19; CG group: n = 15). Reasons for discontinuing the study were a severe car accident (n = 1) and lack of time (n = 1). These two patients did not attend the last three therapy sessions. Missing data for these participants were handled using the last value carried forward method. The compliance rate of the performed home exercise programme for the EE group was 92 % and for the CG group 91 %.
Baseline characteristics of both groups are shown in Table 2. No significant differences were found between the groups for any of the baseline variables measured.
Table 3 shows the mean ± SD values of the main outcome parameters CM and VAS over time. After 26 weeks, the CM score was significantly increased in both exercise groups (EE: 14.4 points, P < 0.001 and CG: 9.8 points, P < 0.001). However, no significant difference was found between these 2 groups (4.6 points, n.s.; see Fig. 2a). Furthermore, the VAS score significantly decreased in both groups from baseline to 26 weeks (EE: −19.9 mm, P < 0.001 and CG: −22.3 mm, P < 0.0001), but there was no significant difference between these groups (2.4 mm, n.s.; see Fig. 2b). This indicates that both treatment programmes yield similar improvements from baseline to 26 weeks.
Post hoc analyses showed a significant improvement in the CM score in the EE group between 6 and 12 weeks (78.4 vs. 87.3, P < 0.001), whereas the CG group showed a significant improvement between baseline and 6 weeks (78.9 vs. 84.9, P = 0.006). For the VAS scores, the post hoc analyses in the EE group showed a significant decrease between baseline and 6 weeks (39.0 vs. 23.5 mm, P = 0.015) and between 6 and 12 weeks (23.5 vs. 9.4 mm, P = 0.003), whereas no significant difference was found for any of the post hoc tests for the VAS scores in the CG. In the EE group, there was a slight deterioration in both CM (87.3 points vs. 86.9 points) and VAS scores (9.4 mm vs. 19.1 mm) between 12 and 26 weeks (Table 3), but this did not reach statistical significance.
The progress of the ROM values and isometric strength values is shown in Fig. 2c–f. Although there was a slight improvement in these variables for both groups from baseline to 26 weeks, these differences did not reach statistical significance, neither within nor between the groups.
Discussion
The main finding of the present study is that both isolated eccentric and conventional training programmes of the RC yield significant improvement in shoulder function (CM score) and pain (VAS) after 26 weeks. However, no significant difference was found between the two groups. Additionally, isometric strength and ROM were not improved over time, either between or within the groups. Based on these results, we have to reject our hypothesis that eccentric training is of superior value compared to conventional exercises in this study population. Furthermore, previous literature does not support that the statistically significant differences we found on the CM score also mean that they are clinically relevant.
Although eccentric training results in a significant improvement in VAS-pain scores (between baseline 6 weeks and between 6–12 weeks; post hoc analysis), the clinical relevance is limited as no between-group difference was found at 26 weeks. Interestingly, both groups showed almost no improvement in the CM score between 12 weeks (i.e. cessation of intervention) and 26 weeks of follow-up. The EE group even showed a slight non-significant deterioration in CM score and an increase in the VAS score in this period, which might indicate that a 12-week exercise programme is too short in this patient population. This is in line with the recommendations by Bohm et al. [4], who state that exercise programmes with a duration of more than 12 weeks are more beneficial compared to shorter ones in terms of tendon adaptation.
In this study, no significant improvement was found for isometric strength within or between the groups after 26 weeks. This could be explained by the fact that participants performed low-load endurance training rather than high-load resistance training. Although there was a slight increase in ROM values for forward flexion, abduction and external rotation, these differences were not significant within and between both groups.
To our knowledge, this is the first study investigating an isolated eccentric exercise programme with a follow-up period of 26-weeks in patients with RC tendinopathy. Therefore, comparison of the long-term results to other studies is difficult. Nonetheless, our results at 12-weeks follow-up are in agreement with other studies, investigating EE in patients with RC tendinopathy. Jonsson et al. [17] showed decreased pain and improved function after 12 weeks of eccentric training of the RC. In contrast to Jonsson’s study, participants in the current study were also asked to perform EE for the external rotators of the shoulder twice daily. Although the decrease in VAS scores for the EE group of Jonsson’s study was slightly better than for our EE group, conclusions should be interpreted with caution, as the Jonsson study used a relatively small sample size (i.e. n = 9) and lacked a control group. On the contrary, Maenhout et al. [21] investigated the value of adding 12 weeks of heavy load eccentric training to resisted internal and external rotation exercises in 61 patients with subacromial pain compared to a control group. They concluded that adding heavy load eccentric training to a traditional RC training was not superior to traditional RC training alone for decreasing pain (VAS) or improving function (measured with the shoulder pain and disability index). Finally, Holmgren et al. [16] investigated the effects of a 12-week-specific EE programme for the RC and concentric–eccentric exercises for the scapula stabilizers compared to unspecific movement exercises. In contrast to our study and the study of Maenhout [21], Holmgren et al. [16] showed a significant between-group difference for pain and function after 12 weeks in favour of the eccentric training group. This difference may be caused by the fact that their control group performed unspecific exercises such as neck retraction, shoulder retraction, shoulder abduction and stretching exercises that do not specifically load the RC.
A strength of this study is that it is the first study assessing patients until 26-week follow-up using an isolated eccentric training programme.
However, some important limitations should be addressed. Firstly, the investigator who was responsible for collecting data was also involved in the treatment of the study participants. This may have biased the study results. Secondly, our sample size calculation was based on an expected difference of 15 points on the CM score, which was based on the change score reported in two previous studies [16, 17]. However, Jonsson et al. [17] did not use any control group in their study, and the study of Holmgren et al. [16] compared eccentric loading to a control group that did not load the RC. Since both groups in our study performed RC exercises, the expected difference of 15 points may have been an overestimation and therefore our study may have lacked sufficient power to detect a significant difference between the groups. Finally, the CM score, which was our primary outcome measure, shows to have some methodological flaws. Rocourt et al. [27] state that the major problem of various CM score protocols used throughout Europe is the imprecise and different standardization. Despite these methodological shortcomings, they have stated that the intratester reliability of the CM score is acceptable [27].
Conclusion
This study shows that a 12-week-isolated eccentric training programme of the RC is beneficial for shoulder function and pain after 26 weeks in patients with RC tendinopathy. However, it is no more beneficial than a conventional exercise programme for the RC and scapular muscles. Based on the results, clinicians should take into account that performing two eccentric exercises twice a day is as effective as performing six concentric/eccentric exercises once a day in patients with RC tendinopathy.
References
Alfredson H, Lorentzon R (2003) Intratendinous glutamate levels and eccentric training in chronic Achilles tendinosis: a prospective study using microdialysis technique. Knee Surg Sports Traumatol Arthrosc 11:196–199
Bigliani LU, Cofield RH, Flatow EL, Fukuda HA, Hawkins RJ, Matsen FA 3rd, Morrison DS Jr, Rockwood CA, Warren RF (2009) Charles Neer: on the giant of the shoulder. J Shoulder Elbow Surg 18:333–338
Bohannon RW (1997) Reference values for extremity muscle strength obtained by hand-held dynamometry from adults aged 20 to 79 years. Arch Phys Med Rehabil 78:26–32
Bohm S, Mersmann F, Arampatzis A (2015) Human tendon adaptation in response to mechanical loading: a systematic review and meta-analysis of exercise intervention studies on healthy adults. Sports Med Open 1(1):1
Braman JP, Zhao KD, Lawrence RL, Harrison AK, Ludewig PM (2014) Shoulder impingement revisited: evolution of diagnostic understanding in orthopedic surgery and physical therapy. Med Biol Eng Comput 52:211–219
Bron C, Wensing M, Franssen JL, Oostendorp RA (2007) Treatment of myofascial trigger points in common shoulder disorders by physical therapy: a randomized controlled trial [ISRCTN75722066. BMC Musculoskelet Disord 5:107
Bullock MP, Foster NE, Wright CC (2005) Shoulder impingement: the effect of sitting posture on shoulder pain and range of motion. Man Ther 10:28–37
Conable KM, Rosner AL (2011) A narrative review of manual muscle testing and implications for muscle testing research. J Chiropr Med 10:157–165
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Cools AM, Johansson FR, Cagnie B, Cambier DC, Witvrouw EE (2012) Stretching the posterior shoulder in subjects with internal rotation deficit: comparison of two stretching techniques. Shoulder Elbow 4:56–63
Diercks R, Bron C, Dorrestijn O, Meskers C, Naber R, de Ruiter T, Willems J, Winters J, van der Woude HJ, Association Dutch Orthopaedic (2014) Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop 85:314–322
Ellenbecker TS, Cools A (2010) Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: an evidence-based review. Br J Sports Med 44:319–327
Graichen H, Hinterwimmer S, von Eisenhart-Rothe R, Vogl T, Englmeier KH, Eckstein F (2005) Effect of abducting and adducting muscle activity on glenohumeral translation, scapular kinematics and subacromial space width in vivo. J Biomech 38:755–760
Greving K, Dorrestijn O, Winters JC, Groenhof F, van der Meer K, Stevens M, Diercks RL (2012) Incidence, prevalence, and consultation rates of shoulder complaints in general practice. Scand J Rheumatol 41:150–155
Habets B, Van Cingel REH (2015) Eccentric exercise training in chronic mid-portion Achilles tendinopathy: a systematic review on different protocols. Scand J Med Sci Sports 25:3–15
Holmgren T, Bjornsson Hallgren H, Oberg B, Adolfsson L, Johansson K (2012) Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. BMJ 344:e787
Jonsson P, Wahlstrom P, Ohberg L, Alfredson H (2006) Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc 14:76–81
Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD (2013) Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med 47:877–885
Lewis J, McCreesh K, Roy JS, Ginn K (2015) Rotator Cuff Tendinopathy: navigating the diagnosis-management conundrum. J Orthop Sports Phys Ther 43:236–241
Ludewig PM, Reynolds JF (2009) The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther 39:90–104
Maenhout AG, Mahieu NN, De Muynck M, De Wilde LF, Cools AM (2013) Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg Sports Traumatol Arthrosc 21:1158–1167
Malliaras P, Barton C, Reeves N, Langberg H (2013) Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med 43:267–286
Ogawa K, Yoshida A, Inokuchi W, Naniwa T (2005) Acromial spur: relationship to aging and morphologic changes in the rotator cuff. J Shoulder Elbow Surg 14:591–598
Ohberg L, Lorentzon R, Alfredson H (2004) Eccentric training in patients with chronic Achilles tendinosis: normalised tendon structure and decreased thickness at follow up. Br J Sports Med 38:8–11
O’Neill S, Watson PJ, Barry S (2015) Why are eccentric exercises effective for achilles tendinopathy? Int J Sports Phys Ther 10:552–562
Riley GP, Harrall RL, Constant CR, Chard MD, Cawston TE, Hazleman BL (1994) Tendon degeneration and chronic shoulder pain: changes in the collagen composition of the human rotator cuff tendons in rotator cuff tendinitis. Ann Rheum Dis 53:359–366
Rocourt MH, Radlinger L, Kalberer F, Sanavi S, Schmid NS, Leunig M, Hertel R (2008) Evaluation of intratester and intertester reliability of the Constant-Murley shoulder assessment. J Shoulder Elbow Surg 17:364–369
Roy JS, MacDermid JC, Woodhouse LJ (2010) A systematic review of the psychometric properties of the Constant-Murley score. J Shoulder Elbow Surg 19:157–164
Rutten MJ, Jager GJ, Kiemeney LA (2010) Ultrasound detection of rotator cuff tears: observer agreement related to increasing experience. AJR Am J Roentgenol 195:W440–W446
Seitz AL, McClure PW, Finucane S, Boardman ND 3rd, Michener LA (2011) Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clin Biomech (Bristol, Avon) 26:1–12
Williamson A, Hoggart B (2005) Pain: a review of three commonly used pain rating scales. J Clin Nurs 14:798–804
Acknowledgments
The authors would like to thank Peer Konings and Nicky van Melick for their assistance in the development of the study protocol and recruitment of study participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Dejaco, B., Habets, B., van Loon, C. et al. Eccentric versus conventional exercise therapy in patients with rotator cuff tendinopathy: a randomized, single blinded, clinical trial. Knee Surg Sports Traumatol Arthrosc 25, 2051–2059 (2017). https://doi.org/10.1007/s00167-016-4223-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4223-x