Abstract
Purpose
The study reports the 2-year follow-up results of patients with valgus osteoarthritis undergoing total knee arthroplasty (TKA) with a standardized soft-tissue release.
Methods
Between 2008 and 2013, 222 TKAs were performed for valgus osteoarthritis by a single surgeon. A total of 181 TKAs in 164 patients were available for a minimum 2-year follow-up (range 24–87 months). Preoperative and postoperative range of motion (ROM), mechanical alignment, the postoperative medial proximal tibial angle (MPTA), Western Ontario and McMaster Universities Arthritis Index (WOMAC), VF-12 score, visual analogue pain scale (VAS), and the actual UCLA activity score, desired UCLA score, ligamentous stability (medial collateral ligament) and complications and revision rates were recorded.
Results
The ROM increased from a preoperative flexion contracture of 4.7° (range 0–40) and flexion of 110° (range 35–135) to a postoperative mean flexion contracture of 0.1° (range −5 to 10) and flexion of 128° (range 100–140). The mean hip–knee–ankle alignment was changed from 8.4° of mechanical valgus (range 5.3–25.4) to 0.02° of varus alignment (range −2.9 to 4.1). Tibia component angle (MPTA) was 90.4° (range 86.1–93.7). The WOMAC score, VF-12, UCLA and VAS significantly improved after surgery (p < 0.05). Two patients (1.1 %) underwent revision surgery for instability.
Conclusion
The described standardized soft-tissue release (release of the iliotibial band and posterolateral corner) provided excellent clinical results at a minimum 2-year follow-up and can be used safely for a “cook-book” approach to the valgus knee with up to 25° mechanical valgus alignment.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 15 % of patients requiring a total knee arthroplasty (TKA) have a valgus deformity of the knee [21]. The valgus knee is characterized by a contracted posterolateral capsule, a contracted iliotibial band (ITB), a contracted lateral collateral ligament (LCL), a contracted posterior cruciate ligament (PCL), medial collateral ligament laxity, osseous deficiency of the posterior lateral femoral condyle and/or posterolateral tibial plateau, external rotation of the distal femur and patellar maltracking [6, 11, 14, 25].
Based on the degree of medial laxity, valgus knees can be classified into three groups (Ranawat type I–III) [14]. The most advanced variant (type III) with insufficiency of the medial soft-tissue constraints (MCL), pronounced contracted lateral structures and marked osseous deficiency of both the lateral femoral condyle and lateral tibia plateau might require a constrained insert or hinged implant. Less advanced deformities (type I and II) can usually be treated with a posterior-stabilized TKA.
Multiple surgical techniques have been described to balance the soft tissues in a valgus knee. Insall and Easley [8] describe a release of the iliotibial band (ITB) of Gerdy’s tubercle. Miyasaka et al. [18] recommend a so-called “pie-crusting” technique to lengthen the ITB. A “pie-crusting” of the ITB and a release of the posterolateral capsule using electrocautery are preferred by Ranawat et al. [25]. Whiteside [31] reported a selective ligament release depending on the presence of tightness in flexion or extension. Although multiple techniques have been described, all current techniques require surgical experience to identify the anatomical structures that need to be released. In addition, outcome data on large patient cohorts are rare.
The aim of the current study is to report the clinical and radiographic outcome as well as the complication rate of TKA for valgus OA of the knee utilizing a standardized soft-tissue release (release of the iliotibial band and posterolateral corner). It is hypothesized that releasing the same structures (“cook-book” approach to the valgus knee) in every patient shows the same excellent outcomes as other techniques that rely on the surgeons’ judgment to determine the level of lateral soft-tissue release.
Materials and methods
Between 2008 and 2013, the senior author performed 222 TKAs in patients with a valgus osteoarthritis. Thirty-nine patients were lost to follow-up (17.6 %), and two patients (0.9 %) underwent TKA for posttraumatic osteoarthritis with valgus alignment and were excluded, leaving 181 TKAs (81.5 %) in 164 patients with a minimum follow-up of 2 years. There were 34 male (20.7 %) and 130 female (79.3 %) patients (17 bilateral TKAs). Mean age at time of surgery was 67 years (range 40–89). The mean BMI was 29.7 kg/m2 (range 18.6–57.9). The mean follow-up was 40 months (range 24–87). A total of 144 (79.6 %) posterior-stabilized tibial inserts (126 Genesis II, Smith & Nephew, Memphis, TN, USA; 10 Balanced Knee System, Ortho Development, Draper, UT, USA; 7 PFC Sigma, DePuy Synthes, West Chester, PA, USA; 1 NexGen, Zimmer, Warsaw, IN, USA) and 37 (20.4 %) constrained inserts were used (Genesis II, Smith & Nephew, Memphis, TN, USA).
Surgical techniques
Epidural hypotensive anaesthesia with intravenous sedation was used routinely. The tourniquet was inflated from the time of incision until implants were cemented. A medial parapatellar approach was used. Using an intramedullary guide, the distal femoral cut was done in 5° routinely. An extramedullary jig was used to perform the tibial cut at 90°, and posterior tibial slope was set according to the manufacturer’s recommendation. Care was taken to minimize the tibial resection in knees with evidence of medial joint space opening (Ranawat type II and III). Femoral component rotation was determined based on the transepicondylar axis and Whiteside’s line. Before the soft-tissue release was performed, appropriate alignment of the distal femur and tibia cut was confirmed using a spacer block with alignment rods. The soft-tissue release starts with a horizontal cut through the ITB using electrocautery at the level of the joint line. Afterwards, the posterolateral corner (PLC) was released starting at the posterior boarder of the ITB continuing to the lateral boarder of the popliteus tendon. This release includes the LCL (in its mid-substance) and anterior lateral ligament (ALL). Usually a “pop” is felt with a successful release. Lamina spreaders are used during the release to apply tension to the soft tissues (Fig. 1a–c). The popliteus tendon that the senior author considers a dynamic stabilizer was preserved in all patients. Now the extension and flexion gap was evaluated using a spacer block. If remaining medial laxity required a constrained insert, alignment was changed to slight varus by taking 1–2 mm of bone off the distal medial femoral condyle to assure that the knee is not left in valgus. All patients underwent patella replacement using a cemented all-polyethylene patellar button.
a After femoral and tibial cuts are done, an asymmetric extension gap occurs due to tightness of the posterolateral structures. The tibial cut aligns perpendicular to the tibial shaft axis; the distal femoral cut is done 5° of the anatomical axis of the femur (intramedullary alignment). b The soft-tissue release starts with a horizontal cut through the ITB using electrocautery (“bovie”) at the level of the joint line. c The lateral release is completed by continuing the release beginning at the posterior boarder of the ITB continuing to the lateral boarder of the popliteus tendon. The release includes following structures: ITB, posterolateral capsule, the LCL (in its mid-substance) and ALL. The popliteal tendon as dynamic stabilizer is preserved
Clinical and radiological evaluation
Clinical data including pre- and postoperative (minimum follow-up of 24 months) range of motion (ROM), degree of MCL laxity (manual examination in 20° flexion pre- and postoperative), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score (Likert scale 0–96) [1, 32], UCLA activity score (1–10) [28], desired UCLA activity score (1–10), visual analogue pain scale (VAS) (100 mm) [28], the VF-12 score (RAND) [29, 30] with subgroups “mental component summary” (MCS) and “physical component summary” (PCS), and postoperative complication and revision rates were recorded. Ligamentous stability was reported on a 4-grade scale with grade 1: having 0°–2° opening, grade 2: 3°–5° opening, grade 3: 6°–10° opening and grade 4: more than 10° opening.
Weight-bearing full-leg radiographs were obtained pre- and postoperatively with the patients standing barefoot with the patella oriented forward [22]. Femoral mechanical and anatomical (shaft) axis, tibial mechanical axis [19] and medial proximal tibial angle (MPTA) were measured according to the criteria defined by Cooke et al. [5]. The centre of the hip, defined by a concentric circle, and the centre of femoral condyles were connected [5] to reconstruct the mechanical axis of the femur. The femoral anatomical axis combines two mid-points of the mediolateral width of the femur (10 cm above the condyles and at the middle of the craniocaudal femur length). The tibial axis was constructed between the mid-width of the talus and the mid-point of the mediolateral tibia plateau [23]. The postoperative measurements were performed in the same fashion. The intersection between the tibial axis, as mentioned above, and the tibial baseplate represents the medial proximal tibial angle (MPTA). The degree of deformity was determined as the angle between the mechanical axis of the femur and the tibia. Five pre- and postoperative datasets of full-leg radiographs had to be excluded not meeting the above-mentioned Cooke criteria [5]. An investigator did repeated measurements on 30 pre- and postoperative radiographs to detect the intraobserver reliability (intraclass correlation, ICC). Another independent observer measured 30 pre- and postoperatively radiographs to identify the inter observer reliability (ICC). Sectra PACS software package (IDS7) was used for all measurements (Sectra AB, Linköping, Sweden).
The study received IRB approval by the institutional review board at the authors’ institution (Hospital for Special Surgery, New York, 10021 NY, USA; IRB number: 11051).
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics software version 23 (Armonk, NY: IBM Corp.). For all variables, descriptive statistics with means and range or standard deviation were reported. A Kolmogorov–Smirnov test and a Welch test were used to identify normal distribution of variables. The paired t test (metric and normally distributed variables) or the Wilcoxon test (ordinal scaled variables) were used to determine the significance of clinical parameters (ROM, MCL grade instability, WOMAC, VF-12 with subgroup MCS and PCS, UCLA, desired UCLA, VAS) and changes in the radiographic measurements. A possible correlation between change in WOMAC score and valgus alignment was analysed using bivariate correlation analyses (Kendall’s tau). Independent two-sided t test or χ 2-test was used to detect possible significant differences concerning WOMAC, VF-12, VAS, and ROM between types of used implants (posterior-stabilized or constrained TKA). A p value of less than 0.05 was considered to be statistically significant. A sample size calculation was done with the goal of a minimum 80 % power-analysis and an alpha failure of 0.05. Following this calculation, the study population should include a minimum of 83 patients (ClinCalc LLC, www.clincalc.com, 2015). The “intraclass correlation coefficient” (ICC) was used to measure inter- and intrarater reliability. The ICC was very high concerning the measurements “mechanical axis” and “anatomical axis” (0.91–0.96) and high for the measurement “MPTA” (intrarater 0.71, interrater 0.69).
Results
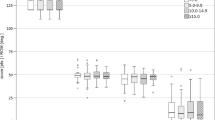
The overall functional improvements and pain relief are reported in Table 1. All functional and pain scores showed a statistically significant improvement after surgery. Preoperative Ranawat classification [25] and our own clinical rating scale are shown in Table 2. Postoperatively, five patients (2.8 %) showed a laxity of the MCL grade 2, two of them showed a mid-flexion instability grade 3. No postoperatively instability in anteroposterior direction occurred within 181 knees.
No statistically significant difference concerning functional and pain outcome (WOMAC, UCLA, VAS, VF-12, ROM) were shown between each type of insert (constrained versus posterior-stabilized TKA). A statistically significant correlation between Δ WOMAC score and Δ valgus alignment was not found.
Radiographic analyses (mechanical and anatomical alignment, tibia component angle, maximum values) pre- and postoperatively are shown in Table 3. One outlier was observed with 7.1° of postoperative mechanical valgus alignment (revision see below).
In five cases (2.8 %), “mobilization under anaesthesia” was performed for postoperative ROM of less than 90° at 4 weeks.
No permanent peroneal nerve injury was reported in 222 TKAs with the current lateral soft-tissue release technique. One temporary nerve palsy occurred in a patient with 25° of valgus alignment preoperatively; a full recovery of the nerve was observed at 6 months after the surgery. There was no deep venous thrombosis. There were two infections: a superficial wound infection was treated with a wound debridement and a consecutive vacuum-assisted closure therapy. The patient remained infection free during a 2-year follow-up. The second patient developed a deep implant infection and underwent a 2-stage revision. An additional four patients underwent further surgery: one patient underwent an arthroscopic synovectomy for restricted ROM and pain after an extensive work up (excluding infection, allergy, etc.) was done. One patellar button (0.6 %) had to be revised because of loosening, and two knees were revised for instability (1.1 %). One patient received an insert exchange (9-mm “high-flex” insert to 15-mm constrained insert) after three knee dislocations. The second patient (postoperative mechanical valgus alignment of 7.1°) required a revision 4 years after index procedure because of medial instability. During the initial surgery, a 15-mm constrained insert was used; however, ultimately the patient required a second revision to a hinged TKA.
Discussion
The most important finding of the current study is that excellent clinical and radiographic outcomes can be achieved after TKA utilizing the same standardized lateral soft-tissue release for all patients with valgus alignment up to 25°.
Although approximately 100,000 TKAs are performed for valgus osteoarthritis in the USA every year, there is an ongoing debate about the best lateral soft-tissue release technique to balance the valgus knee during TKA. The following lateral release techniques have been described: Whiteside [31] reported a selective release depending on lateral tightness in flexion and extension, which includes a release of the LCL, ITB, posterolateral capsule and popliteus tendon in a stepwise fashion. Krackow et al. [12] recommend to first release the ITB and the LCL, and if necessary to add a release of the popliteus tendon and the posterolateral capsule. Ranawat et al. [25] reported an “inside-out” technique with a release of the posterolateral capsule using the electrocautery and a “pie-crusting” of the ITB. The ITB is described as an effective lateral stabilizer only in full extension until 30° of flexion [9]. A higher rate of lateral instability in the clinical examination (varus stress in full extension and 30°) was not observed in the current study cohort. All patients in the current study underwent the same lateral release technique including a release of the ITB and posterolateral capsule using electrocautery. This technique is very reproducible and resulted in excellent functional outcomes at 2 years after surgery.
The study has the following limitations. First, the retrospective nature of the study could have impacted data collection. Second, although patients from the first 12 months in practice were excluded, the study might still be affected by the surgeon’s initial learning curve coming out of fellowship training. However, over the years, the senior author has continued the current soft-tissue release technique without modifications. The evaluation of postoperative soft-tissue balance is examiner dependent, but all patients were examined by the senior author during the follow-up period. Finally, a 2-year follow-up does not allow drawing long-term conclusions.
Clarke et al. [4] reported about a mean flexion after TKA in valgus knee of 121° (n = 24, mean follow-up 54 months). The current patient cohort shows an average flexion range of motion of 128° and is in line with data reported on posterior-stabilized TKA. It suggests that despite an extensive soft-tissue release in valgus knees, similar flexion range of motion can be achieved as in varus knees [13].
Roh et al. [26] described a preoperative WOMAC score of 58.4 (SD ± 22) and a postoperative WOMAC score of 17 (SD ± 10.7) in a randomized controlled study (RCS) performing posterior-stabilized TKAs (n = 44). Clarke et al. [3] reported a postoperative WOMAC score of 22.8 (SD ± 35.4) in a RCS also using posterior-stabilized implants at 2-year follow-up. Kim and Kim [10] evaluated 86 patients retrospectively using 57 (66 %) posterior-stabilized TKAs and 29 (34 %) constrained TKAs. Utilizing a similar implant mix as the current study, WOMAC scores improved from 79 (range 78–96) preoperatively to 34.4 (range 5–68) after surgery. In the current patient group, slightly decreased postoperative WOMAC score (14.4 points) and an increased change in WOMAC score were noted. Since most studies on TKA in valgus osteoarthritis did not report WOMAC scores, comparative data are not available [6, 25, 31]. UCLA activity scores and SF12 data are within the range reported in the literature for patients undergoing TKA [2, 7, 20, 27].
Comparative outcome studies on different release techniques do not exist. Most techniques require intraoperative judgment by the surgeon regarding the extent of the release and make these techniques somewhat dependent on surgeon experience. The current paper describes a surgical technique that was applied in exactly the same fashion during all surgeries. We believe that the technique therefore holds advantages for the low-volume surgeons and provides a “cook-book” approach to the valgus knee. In addition, most current papers consider a popliteus tendon release as a surgical release option. Our paper shows that excellent results can be achieved without touching the popliteus tendon. The authors consider the popliteus muscle a dynamic stabilizer, which in contrast to tight ligaments (LCL, ITB) and capsule will stretch out over time. Its release increases the chance of flexion instability [17] and according to the current study is not required to balance the valgus knee. The LCL and the ALL [16, 24] were also released during the procedure. Although the LCL is described as a major stabilizer throughout the arc from 0° to 90° flexion [9, 15], no lateral instability was observed in the current study. Luring et al. [15] showed a flexion instability after releasing the LCL. However, the stepwise release [17] which was used by Luring et al., always included a prior release of the popliteus tendon. The function of the ALL in terms of stability is still discussed controversially [16, 24]; an essential stabilization effect of the ALL has not been confirmed yet. The authors also prefer a posterior-stabilized insert in valgus knees. First, in the author’s experience, it is easier to balance the valgus knee if the PCL is released, and secondly, cruciate retaining knees require restoration of the joint line, which by definition is not possible in a valgus knee after a lateral release (the released space will be filled by an increased tibial insert height elevating the joint line).
The current study suggests that doing exactly the same release for all patients with valgus OA regardless of the extend of the deformity is a feasible approach to patients with valgus alignment. This gives less experienced surgeons a “cook-book” approach to the valgus knee.
Conclusion
The current study reports on a standardized lateral soft-tissue release for all patients with valgus alignment. It eliminated intraoperative judgment to select which structure needs to be released. Instability requiring revision surgery occurred in 1.1 % of patients and was primarily caused by valgus alignment of the femoral component. The current release appears to be a very reliable treatment option for valgus knees with up to 25° of mechanical deformity utilizing posterior-stabilized or constrained components.
References
Bellamy N (2002) WOMAC: a 20-year experiential review of a patient-centered self-reported health status questionnaire. J Rheumatol 29(12):2472–2476
Bourne RB, McCalden RW, MacDonald SJ, Mokete L, Guerin J (2007) Influence of patient factors on TKA outcomes at 5 to 11 years followup. Clin Orthop Relat Res 464:27–31
Clark CR, Rorabeck CH, MacDonald S, Swafford J, Cleland D (2001) Posterior-stabilized and cruciate-retaining total knee replacement. Clin Orthop Relat Res 392:208–212
Clarke HD, Fuchs R, Scuderi GR, Scott WN, Insall JN (2005) Clinical results in valgus total knee arthroplasty with the “pie crust” technique of lateral soft tissue releases. J Arthroplasty 20(8):1010–1014
Cooke TD, Sled EA, Scudamore RA (2007) Frontal plane knee alignment: a call for standardized measurement. J Rheumatol 34(9):1796–1801
Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS (2004) Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 86(12):2671–2676
Harato K, Bourne RB, Victor J, Snyder M, Hart J, Ries MD (2008) Midterm comparison of posterior cruciate-retaining versus -substituting total knee arthroplasty using the Genesis II prosthesis. A multicenter prospective randomized clinical trial. Knee 15(3):217–221
Insall JN, Easley ME (2001) Surgical Techniques and instrumentation in total knee arthroplasty. In: Insall JN, Scott WN (eds) Surgery of the Knee, Vol 2. 3rd edn. New York, Churchill Livingstone, p 1553–1620
Kanamiya T, Whiteside LA, Nakamura T, Mihalko WM, Steiger J, Naito M (2002) Effect of selective lateral ligament release on stability in knee arthroplasty. Clin Orthop Relat Res 404:24–31
Kim YH, Kim JS (2009) Does TKA improve functional outcome and range of motion in patients with stiff knees? Clin Orthop Relat Res 467(5):1348–1354
Koninckx A, Schwab PE, Deltour A, Thienpont E (2014) The minimally invasive far medial subvastus approach for total knee arthroplasty in valgus knees. Knee Surg Sports Traumatol Arthrosc 22(8):1765–1770
Krackow KA, Jones MM, Teeny SM, Hungerford DS (1991) Primary total knee arthroplasty in patients with fixed valgus deformity. Clin Orthop Relat Res 273:9–18
Li N, Tan Y, Deng Y, Chen L (2014) Posterior cruciate-retaining versus posterior stabilized total knee arthroplasty: a meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc 22(3):556–564
Lombardi A, Dodds K, Berend K, Mallory T, Adams J (2004) An algorithmic approach to total knee arthroplasty in the valgus knee. J Bone Joint Surg Am 86:62–71
Luring C, Oczipka F, Grifka J, Perlick L (2008) The computer-assisted sequential lateral soft-tissue release in total knee arthroplasty for valgus knees. Int Orthop 32(2):229–235
Lutz C, Sonnery-Cottet B, Niglis L, Freychet B, Clavert P, Imbert P (2015) Behavior of the anterolateral structures of the knee during internal rotation. Orthop Traumatol Surg Res 101(5):523–528
Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB (1999) Soft tissue release in total knee arthroplasty. Clin Orthop Relat Res 366:264–273
Miyasaka KC, Ranawat CS, Mullaji A (1997) 10- to 20-year followup of total knee arthroplasty for valgus deformities. Clin Orthop Relat Res 345:29–37
Moon YW, Kim JG, Han JH, Do KH, Seo JG, Lim HC (2013) Factors correlated with the reducibility of varus deformity in knee osteoarthritis: an analysis using navigation guided TKA. Clin Orthop Surg 5(1):36–43
Nam D, Park A, Stambough JB, Johnson SR, Nunley RM, Barrack RL (2016) The Mark Coventry Award: custom cutting guides do not improve total knee arthroplasty clinical outcomes at 2 years followup. Clin Orthop Relat Res 474(1):40–46
Nikolopoulos D, Michos I, Safos G, Safos P (2015) Current surgical strategies for total arthroplasty in valgus knee. World J Orthop 6(6):469–482
Paley D, Pfeil J (2000) Prinzipien der kniegelenknahen Deformitätenkorrektur. Orthopäde 29:18–38
Paternostre F, Schwab PE, Thienpont E (2014) The difference between weight-bearing and non-weight-bearing alignment in patient-specific instrumentation planning. Knee Surg Sports Traumatol Arthrosc 22(3):674–679
Pomajzl R, Maerz T, Shams C, Guettler J, Bicos J (2015) A review of the anterolateral ligament of the knee: current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy 31(3):583–591
Ranawat A, Ranawat C, Elkus M, Rasquinha V, Rossi R, Babhulkar S (2005) Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 87:271–284
Roh YW, Jang J, Choi WC, Lee JK, Chun SH, Lee S, Seong SC, Lee MC (2013) Preservation of the posterior cruciate ligament is not helpful in highly conforming mobile-bearing total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc 21(12):2850–2859
Shan L, Shan B, Suzuki A, Nouh F, Saxena A (2015) Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Am 97(2):156–168
Terwee CB, Bouwmeester W, van Elsland SL, de Vet HC, Dekker J (2011) Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthr Cartil 19(6):620–633
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Ware JE, Kosinski M, Dewey J (2000) How to score version two of the SF-36 health survey. QualityMetric Inc., Lincoln
Whiteside LA (1999) Selective ligament release in total knee arthroplasty of the knee in valgus. Clin Orthop Relat Res 367:130–140
Woolacott NF, Corbett MS, Rice SJ (2012) The use and reporting of WOMAC in the assessment of the benefit of physical therapies for the pain of osteoarthritis of the knee: findings from a systematic review of clinical trials. Rheumatology (Oxford) 51(8):1440–1446
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We certify that we have not signed any agreement with commercial interest related to this study, which would in any way limit publication of any and all data generated for the study or to delay publication for any reason. Dr. Boettner reports personal fees from Smith & Nephew, personal fees from Ortho Development Corporation, personal fees from DePuy Synthes, outside the submitted work. Dr. Faschingbauer reports personal fees from Deutsche Forschungsgemeinschaft (Research Fellowship, FA 1271/1-1, www.dfg.de), during the conduct of the study.
Ethical standard
The authors’ institutional review board approved this study.
Rights and permissions
About this article
Cite this article
Boettner, F., Renner, L., Arana Narbarte, D. et al. Total knee arthroplasty for valgus osteoarthritis: the results of a standardized soft-tissue release technique. Knee Surg Sports Traumatol Arthrosc 24, 2525–2531 (2016). https://doi.org/10.1007/s00167-016-4054-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4054-9