Abstract
Introduction
Advanced valgus osteoarthritis (OA) is one of the most challenging indications for total knee arthroplasty (TKA). There is no information in the literature about the optimal timing of surgery. The current study investigates the impact of the preoperative deformity and degree of arthritis on postoperative outcome after TKA.
Material and methods
The study evaluated 133 knees in 107 patients with valgus OA that failed nonoperative treatment with a minimum 2-year follow-up. Mechanical alignment, Kellgren and Lawrence (K/L) score, and minimal joint space width (minJSW) were measured on AP- and hip-to-ankle radiographs. All knees had advanced OA (i.e., K/L grades 3 or 4 and less than 50% minJSW). Pre- and postoperative WOMAC, VR-12, UCLA, VAS, ROM were recorded.
Results
There was no difference in clinical outcome (WOMAC, UCLA, VR-12, VAS or ROM) between patients with different degrees of valgus deformities (< 5.0 deg., 5.0–9.9 deg., 10.0–14.9 deg., ≥ 15.0 deg.). There was also no correlation between K/L score or minimal joint space width and any of the outcome parameters.
Conclusions
The degree of valgus deformity and the grade of osteoarthritis do not predict the outcome of TKA in patients with valgus OA. Since the risk of complication and the need for implant constraint increases with increasing deformity and instability of the knee, surgery appears to be justified in patients with advanced OA that failed nonoperative treatment, regardless of the degree of deformity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The indication for total knee arthroplasty (TKA) in osteoarthritis (OA) is based on the multiple factors, including pain, functional limitations, physical examination, and radiographic evidence of OA [1, 2]. It is often assumed that patients with more severe preoperative arthritis have better postoperative results and that early surgery should be avoided [1, 3]. This also is in line with the guidelines of the American health insurance industry (CG-SURG-54). However, it remains controversial whether the degree of joint space narrowing is correlated with postoperative outcomes [3,4,5,6,7,8].
Progressive valgus deformities are often accompanied with increased medial knee laxity and make balancing the knee during TKA more difficult [9]. In addition, pronounced mechanical malalignment in combination with a flexion contracture (tri-planar deformity) increases the risk of peroneal nerve injury [10, 11].
The current paper analyzes the following research question: Does the degree of the mechanical deformity or the grade of the osteoarthritis at the time of surgery impact the clinical outcome of TKA in patients with valgus OA who failed nonoperative treatment?
Materials and methods
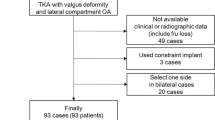
For the current study, 167 TKA in 135 patients (108 females and 27 males) with a minimum of 2-year follow-up were available. TKA was only indicated for advanced osteoarthritis (Kellgren and Lawrence (K/L) grades 3 or 4 and less than 50% of the remaining minimal joint space width (minJSW)). TKA in patients with mild valgus deformity (< 5 degree (deg.), 48 knees) were only indicated after failed nonoperative treatment (Table 1).
Patients underwent the same standardized soft-tissue release regardless of the extend of the deformity as described by the senior author [9]. Depending on the level of instability after the release of the iliotibial band and the posterolateral corner, either a posterior stabilized (PS, n = 98)—or constrained (n = 35) insert was used. Hinged knee systems, or additional correction-osteotomies were not needed in any of the cases. Implants used were n = 123 (92.5%) Genesis II (Smith & Nephew, Memphis, Tennessee, USA), n = 7 (5.3%) BKS (OrthoDevelopment, Draper, Utah, USA) and n = 3 (2.3%) Sigma (DePuy Synthes, Warsaw, Indiana, USA).
Of the 167 knees, 2 (1.2%) had to be excluded because not all X-rays were available, 2 (1.2%) because postoperative range of motion (ROM) was not recorded and 30 (18.0%) because not all outcome scores were available. In total 34 knees had to be excluded leaving 133 (79.6%) knees in 107 patients for enrollment in the current study. There were 23 men with 25 TKAs and 84 women with 108 TKAs. The mean age at the time of surgery was 68.3 years (range 44–89). The mean BMI was 30.6 kg/m2 (range 19.7–58.7 kg/m2). The minimum follow-up was 2 years (mean: 43.9 months, range 24–120 months).
Clinical evaluation
The data collection included pre- and postoperative range of motion (ROM), degree of flexion contracture, Western Ontario and McMaster University Osteoarthritis index (WOMAC) score (Likert scale 0–96), desired—and actual UCLA activity score (1–10), visual analogue pain scale (VAS) (100 mm) and the VR-12 score (RAND) with the subgroups: “mental component summary” (MCS, 0–100) and “physical component summary” (PCS, 0–100).
Radiographic evaluation
All patients underwent a series of preoperative radiographs. The standard bilateral weight-bearing anterior to posterior view of the fully-extended knee (AP view) and the weight-bearing hip-to-ankle (HA) radiograph.
Mechanical and anatomic alignment were determinate using HA radiographs [12]. The knees were divided into groups based on the degree of mechanical malalignment: group 1 (< 5.0 deg.), group 2 (5.0–9.9 deg.), group 3 (10.0–14.9 deg.) and group 4 (≥ 15.0 deg.). The minimal joint space width (minJSW) was defined as the macroscopic smallest distance between the femoral condyle and the articulating tibial plateau in mm. It was measured for the medial and lateral compartment using digital, calibrated AP- and PA-flexed radiographs [13]. Malpositioned radiographs (2, 1.2%) can compromise minJSW measurement and were excluded [14]. OA was graded on AP radiographs based on the Kellgren and Lawrence classification (K/L 1–4) [15]. One investigator repeated measurements on 20 preoperative AP views and HA radiographs for intraobserver reliability (intraclass correlation coefficient, ICC, range 0.79—0.94). Another investigator repeated measurements on 20 preoperative AP view and HA radiographs for inter observer correlation (ICC, range 0.78—0.92). All measurements were obtained in SECTRA PACS software package IDS7 (Sectra AB, Linkoeping, Sweden). The study received IRB approval by the institutional review board at the authors institution (IRB number: 2017—0418).
Statistical analysis
Descriptive statistics were performed to describe means and range and standard deviation for all variables. Kolmogorov–Smirnov was used to identify normal distribution of variables. Levene test was used to test for homogeneity of variances. Paired t test or ANOVA test (for metric and normally distributed variables; ΔWOMAC, minJSW, mechanical and anatomic alignment) or the Wilcoxon Rank Sum or Kruskal–Wallis test (for independent, nonparametric variables; WOMAC, UCLA, desired-UCLA, VAS, VR-12, ROM, gender, age at time of surgery, BMI) were performed to identify significance. Statistical analysis was performed for a 95% confidence interval. The results with p values less than 0.05 were considered statistically significant.
Standard deviation for WOMAC was previously calculated to be 17.6 [9]. Power calculation for an alpha failure of α = 0.05, an effect size of 0.57 to detect a difference in 10 points and an aimed power (1–β) of 80% required a sample size of 100 knees. The “intraclass correlation coefficient” (ICC) (minJSW measurements) or Cohen’s Kappa (Kellgren and Lawrence score) test were applied to measure inter- and intraobserver reliability. All statistical analyzes were performed using IBM SPSS® Statistics software version 26.0.0.0 (SPSS Inc., Chicago, Il, USA). Power calculation was performed with G*Power, version 3.1.9.2 (University of Duesseldorf, Duesseldorf, Germany) [16].
Results
In 133 knees, the mean preoperative mechanical and anatomical alignment was 8.8 deg. (range 0.3–25.4 deg.) and 14.5 deg. (range − 1.5 to 30.3 deg.) respectively. Based on the severity of the mechanical deformity 35 knees were placed in group 1, 53 knees in group 2, 25 knees in group 3, and 20 knees in group 4. There was no significant difference in demographic data between the 4 groups of valgus deformity, but females tended to have more severe valgus deformity (Table 2). K/L score in the AP view was 1 or 2 in none, 3 in 80 (60.2%) and 4 in 53 (39.8%) knees. 5 knees had revision surgery (two for instability/dislocation, one for infection and two for aseptic loosening of the tibial and the patella component, respectively). One patient, female, 65 years, BMI of 45 kg/m2, showed a moderate medial instability postoperatively. With a ROM of 120 degrees and no pain whatsoever, we draw no operative consequence. All other patients did not show any postoperative instability.
Comparing knees with posterior stabilized or constrained inlays, the use of the later was more likely with higher valgus (p < 0.001) and female patients (p < 0.001) but no difference in age (p = 0.399) or BMI (p = 0.164) was observed. While the type of insert constraint had no impact on functional outcome (UCLA, p = 0.994, WOMAC p = 0.255, V12 physical, p = 0.315, V12 mental, p = 0.520, or ROM, p = 0.498) it affected postoperative VAS (mean 1.1–1.7, p = 0.036).
Clinical outcome scores were not significantly different between the groups (WOMAC, p = 0.887, ΔWOMAC, p = 0.553, UCLA, p = 0.662, desired-UCLA, p = 0.093, V-12 mental, p = 0.819, V12 physical, p = 0.796, ROM, p = 0.9978, VAS, p = 0.998 and flexion–contracture, p = 0.383) (Fig. 1).
In a second step patients with only mild to moderate OA on AP view (K/L ≤ 3, minJSW of at least 2.0 mm) and mild valgus deformity (< 5 deg.) were compared with cases with “bone on bone” OA on the AP view (K/L = 4, minJSW < 0.5 mm) and advanced valgus deformity (≥ 10 deg.). Both groups had no significant difference in the outcome scores WOMAC (p = 0.935), ΔWOMAC (p = 0.510), V-12 mental (p = 0.102), V-12 physical (p = 0.403), UCLA score (p = 0.403), VAS (p = 0.243) or ROM (p = 0.567) (Fig. 2). Postoperative desired-UCLA score tended to be (p = 0.041) higher in the mild to moderate OA group (desired-UCLA mean: 7.5, range 3–10) compared to the severe OA group (UCLA mean: 5.8, range 2–8). There was no difference in gender (p = 0.301), age at time of surgery (p = 0.203), BMI (p = 0.961) and preoperative ROM (p = 0.918) between the groups. Of note, the first subgroup comprises patients with moderate not minimal osteoarthritis.
Boxplot showing postoperative clinical outcome scores (range of motion (ROM), VF-12 mental and physical, WOMAC) for subgroups with mild or moderate OA and minimal valgus deformity (Kellgren and Lawrence (K/L) ≤ 3, minimal joint space width (minJSW) > 3.0 mm, < 5 deg. of valgus) or “bone on bone” OA and an advanced valgus deformity (K/L = 4, minJSW < 0.5 mm, ≥ 10 deg. of valgus). The clinical outcome was not significantly different between the two groups
Discussion
The current data suggest that neither the degree of valgus deformity nor the severity of osteoarthritis have an impact on the clinical outcome (WOMAC, UCLA, VR-12, VAS or ROM) (Fig. 1) in patients with valgus osteoarthritis who have failed nonoperative treatment. Moderate osteoarthritis with a joint space of at least 2 mm on AP radiographs was not a predictor for poor outcome. This suggests that patients who failed nonoperative treatment and have evidence of at least grade 3 K/L valgus osteoarthritis can undergo successful TKA regardless of the joint space on AP radiographs and that “bone-on-bone” osteoarthritis is not necessary to achieve a significant clinical benefit after TKA.
Patient satisfaction is multifactorial [17]. Today, it is still unclear whether the results of TKA are influenced by the degree of osteoarthritis at the time of surgery [18]. Some authors reported superior results for TKA performed for early OA [4, 5, 7, 19], whereas others reported the opposite [8]. Especially the correlation between the degree of radiographic deformity and postoperative outcome has not been studied. The current data suggest that functional improvements and clinical outcomes are not influenced by the degree of deformity and osteoarthritis at the time of TKA [4, 20]. One of the reasons for this finding might be that AP radiographs underestimate the degree of severity of OA in valgus osteoarthritis and might not be a reliable indicator for cartilage quality in the lateral compartment [21,22,23,24]. The presented data suggest that patients with valgus OA can achieve excellent postoperative results whether they have moderate or severe OA (Fig. 2).
Rationales against early surgery include the greater likelihood of revision surgery in younger patients [25] as well as the potentially higher complication rate [3]. However, these results might not apply to valgus knees. Worsening deformity and increasing instability over the course of valgus osteoarthritis can result in higher short-term complication rates (more complicated surgery, longer surgery duration, increased blood loss, higher percentage of peroneal nerve injuries) [10, 11, 26,27,28] as well as long-term failure rates (higher loosening rates for constrained implants) [29]. The revision rate was reported to be two times higher at 10 years and three times higher after 20 years for constrained or hinged compared to unconstrained implants [29]. The rate of aseptic loosening may increase in knees with more than 11 deg. valgus deformity [28].
In a registry study with 10,361 TKA preoperative valgus deformity was significantly (p < 0.001) associated with peroneal nerve palsy. Of 32 knees with nerve palsy, 10 had 12–25 deg. (mean: 18 deg.) of valgus deformity [30]. The increased risk of peroneal nerve injury could be either the result of direct injury during the lateral release [31, 32] or traction or compromised vascular supply due to stretching of the nerve during the correction of the deformity [33]. Valgus knees with more than 20 deg. valgus and flexion deformity are at increased risk for nerve palsy [33]. Avoiding severe valgus malalignment (> 15 deg.) and more advanced flexion deformities can reduce the risk of peroneal nerve injury according to the literature [9, 34]. The current study suggests that early surgery does not compromise the outcome of TKA in valgus knees.
Delaying surgery in patients with failed nonoperative treatment impacts the patients’ quality of life (WOMAC, VR-12). This reduces their quality-adjusted life-years (QALYs), a measurement tool for clinical effectiveness of a specific procedure [35]. Higher age-at-date-of-surgery and decreased preoperative WOMAC may be related to inferior outcome [4]. Our data seem to support this assumption. Other authors reported that patients’ satisfaction seems to be more related to the postoperative outcome rather than to preoperative symptoms [36].
The extended release of the posterolateral corner in correction of valgus deformity may significantly decrease stability in the medial compartment [37]. Consequently. Consequently, cruciate retaining (CR) TKA was recently reported to be more likely at risk of postoperative instability compared to posterior stabilized (PS) systems [38]. In addition, most modern PS designs accommodate effortless conversion to a constraint if ligamentous stability is not achieved by the described soft tissue release. Following these findings, we only used PS or constrained inserts depending on the soft tissue release necessary. We found no differences on outcome except postoperative VAS. Only one patient showed minor postoperative instability with no pain and good ROM.
The current study has the following limitations: (1) This is a retrospective study and response to nonoperative treatment was judged based on the preoperative office notes alone. (2) All 133 TKAs were performed by one high volume fellowship trained surgeon who does more than 250 TKAs per year at a specialized orthopedic hospital. (3) Manual measurement of the minJSW is influenced by a number of factors, however, this method has proven to provide reproducible results in the literature and in the current inter- and intraobserver analysis [13, 39, 40]. Some subgroup analyzes only compare small populations and might be underpowered. (4) This paper specifically investigated OA in knees with valgus deformity. The conclusions of the study do not apply to patients with neutral or varus mechanical alignment. (5) This study does not display a knee-specific outcome score. However, WOMAC, UCLA, VR-12, VAS and functional outcomes including ROM and degree of flexion contracture provide adequate information about the clinical outcome. (6) The enrolled patients only had a minimum of 2-year follow up and no long-term conclusions can be drawn from the current data.
Conclusion
The current data suggest that neither the degree of valgus deformity nor the severity of osteoarthritis on AP radiographs have an impact on the clinical outcome of TKA in patients with valgus osteoarthritis. Moderate osteoarthritis with a joint space of at least 2 mm on AP radiographs, with evidence of joint space narrowing on PA-flexed-view was not a predictor for poor outcome. Considering that certain complication and the use of more constrained implants are related to the severity of valgus deformity surgeons might proceed with TKA in patients that failed nonoperative treatment but do not display “bone-on-bone” arthritis on AP radiographs.
References
Mancuso CA, Ranawat CS, Esdaile JM, Johanson NA, Charlson ME (1996) Indications for total hip and total knee arthroplasties. Results of orthopaedic surveys. J Arthroplast 11(1):34–46
Liang MH, Cullen KE, Poss R (1982) Primary total hip or knee replacement: evaluation of patients. Ann Intern Med 97(5):735–739
Perry KI, Strasser NL, Harmsen WS, Pagnano MW, Trousdale RT (2015) Minimal preoperative degenerative arthritis may not predict poor tka outcome. Orthopedics 38(8):e681-684. https://doi.org/10.3928/01477447-20150804-54
Chang CB, Yoo JH, Koh IJ, Kang YG, Seong SC, Kim TK (2010) Key factors in determining surgical timing of total knee arthroplasty in osteoarthritic patients: age, radiographic severity, and symptomatic severity. J Orthop Traumatol Off J Italian Soc Orthop Traumatol 11(1):21–27. https://doi.org/10.1007/s10195-010-0086-y
Fortin PR, Penrod JR, Clarke AE, St-Pierre Y, Joseph L, Belisle P, Liang MH, Ferland D, Phillips CB, Mahomed N, Tanzer M, Sledge C, Fossel AH, Katz JN (2002) Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthr Rheum 46(12):3327–3330. https://doi.org/10.1002/art.10631
Gidwani S, Tauro B, Whitehouse S, Newman JH (2003) Do patients need to earn total knee arthroplasty? J Arthroplast 18(2):199–203. https://doi.org/10.1054/arth.2003.50021
Kennedy LG, Newman JH, Ackroyd CE, Dieppe PA (2003) When should we do knee replacements? Knee 10(2):161–166
Peck CN, Childs J, McLauchlan GJ (2014) Inferior outcomes of total knee replacement in early radiological stages of osteoarthritis. Knee 21(6):1229–1232. https://doi.org/10.1016/j.knee.2014.08.018
Boettner F, Renner L, Arana Narbarte D, Egidy C, Faschingbauer M (2016) Total knee arthroplasty for valgus osteoarthritis: the results of a standardized soft-tissue release technique. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24(8):2525–2531. https://doi.org/10.1007/s00167-016-4054-9
Idusuyi OB, Morrey BF (1996) Peroneal nerve palsy after total knee arthroplasty. Assessment of predisposing and prognostic factors. J Bone Jt Surg Am Vol 78(2):177–184
Asp JP, Rand JA (1990) Peroneal nerve palsy after total knee arthroplasty. Clin Orthop Relat Res 261:233–237
Cooke TD, Sled EA, Scudamore RA (2007) Frontal plane knee alignment: a call for standardized measurement. J Rheumatol 34(9):1796–1801
Buckland-Wright JC, Macfarlane DG, Williams SA, Ward RJ (1995) Accuracy and precision of joint space width measurements in standard and macroradiographs of osteoarthritic knees. Ann Rheum Dis 54(11):872–880
Vignon E, Brandt KD, Mercier C, Hochberg M, Hunter D, Mazzuca S, Powell K, Wyman B, Le Graverand MP (2010) Alignment of the medial tibial plateau affects the rate of joint space narrowing in the osteoarthritic knee. Osteoarthr Cartil/OARS Osteoarthr Res Soc 18(11):1436–1440. https://doi.org/10.1016/j.joca.2010.08.012
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(4):1149–1160. https://doi.org/10.3758/brm.41.4.1149
Scott CE, Howie CR, MacDonald D, Biant LC (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Jt Surg Br Vol 92(9):1253–1258. https://doi.org/10.1302/0301-620x.92b9.24394
Lim JT, Luscombe KL, Jones PW, White SH (2006) The effect of preoperative symptom severity on functional outcome of total knee replacement–patients with the lowest preoperative scores achieve the lowest marks. Knee 13(3):216–219. https://doi.org/10.1016/j.knee.2006.01.006
Meftah M, White PB, Ranawat AS, Ranawat CS (2016) Long-term results of total knee arthroplasty in young and active patients with posterior stabilized design. Knee 23(2):318–321. https://doi.org/10.1016/j.knee.2015.10.008
Meding JB, Ritter MA, Faris PM, Keating EM, Harris W (2001) Does the preoperative radiographic degree of osteoarthritis correlate to results in primary total knee arthroplasty? J Arthroplast 16(1):13–16. https://doi.org/10.1054/arth.2001.16501
Guermazi A, Niu J, Hayashi D, Roemer FW, Englund M, Neogi T, Aliabadi P, McLennan CE, Felson DT (2012) Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). BMJ (Clin Res Ed) 345:e5339. https://doi.org/10.1136/bmj.e5339
Kijowski R, Blankenbaker DG, Stanton PT, Fine JP, Smet AAD (2006) Radiographic findings of osteoarthritis versus arthroscopic findings of articular cartilage degeneration in the tibiofemoral joint. Radiology 239(3):818–824. https://doi.org/10.1148/radiol.2393050584
Rueckl K, Boettner F, Maza N, Runer A, Bechler U, Sculco P (2017) The posterior–anterior flexed view is better than the anterior–posterior view for assessing osteoarthritis of the knee. Skelet Radiol. https://doi.org/10.1007/s00256-017-2815-2
Rueckl K, Runer A, Bechler U, Faschingbauer M, Boelch SP, Sculco PK, Boettner F (2019) The posterior–anterior-flexed view is essential for the evaluation of valgus osteoarthritis. A prospective study on 134 valgus knees. BMC Musculoskeletl Disord 20(1):636. https://doi.org/10.1186/s12891-019-3012-3
Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS (2003) Factors affecting the durability of primary total knee prostheses. J Bone Jt Surg Am Vol 85-a(2):259–265
Maempel JF, Riddoch F, Calleja N, Brenkel IJ (2015) Longer hospital stay, more complications, and increased mortality but substantially improved function after knee replacement in older patients. Acta Orthop 86(4):451–456. https://doi.org/10.3109/17453674.2015.1040304
Stern SH, Moeckel BH, Insall JN (1991) Total knee arthroplasty in valgus knees. Clin Orthop Relat Res 273:5–8
Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, Meding JB (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Jt Surg Am Vol 95(2):126–131. https://doi.org/10.2106/jbjs.k.00607
Martin JR, Beahrs TR, Stuhlman CR, Trousdale RT (2016) Complex primary total knee arthroplasty: long-term outcomes. J Bone Jt Surg Am Vol 98(17):1459–1470. https://doi.org/10.2106/jbjs.15.01173
Miyasaka KC, Ranawat CS, Mullaji A (1997) 10- to 20-year followup of total knee arthroplasty for valgus deformities. Clin Orthop Relat Res 345:29–37
Bruzzone M, Ranawat A, Castoldi F, Dettoni F, Rossi P, Rossi R (2010) The risk of direct peroneal nerve injury using the Ranawat “inside-out” lateral release technique in valgus total knee arthroplasty. J Arthroplast 25(1):161–165. https://doi.org/10.1016/j.arth.2008.08.016
Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S (2005) Total knee arthroplasty for severe valgus deformity. J Bone Jt Surg Am Vol 87:271–284. https://doi.org/10.2106/jbjs.e.00308
Rose HA, Hood RW, Otis JC, Ranawat CS, Insall JN (1982) Peroneal-nerve palsy following total knee arthroplasty. A review of The Hospital for Special Surgery experience. J Bone Jt Surg Am Vol 64(3):347–351
Nercessian OA, Ugwonali OF, Park S (2005) Peroneal nerve palsy after total knee arthroplasty. J arthroplast 20(8):1068–1073. https://doi.org/10.1016/j.arth.2005.02.010
Barlow BT, McLawhorn AS, Westrich GH (2017) The cost-effectiveness of dual mobility implants for primary total hip arthroplasty: a computer-based cost-utility model. J Bone Jt Surg Am Vol 99(9):768–777. https://doi.org/10.2106/jbjs.16.00109
Baker PN, Rushton S, Jameson SS, Reed M, Gregg P, Deehan DJ (2013) Patient satisfaction with total knee replacement cannot be predicted from pre-operative variables alone: a cohort study from the national joint registry for England and Wales. Bone Jt J 95-b(10):1359–1365. https://doi.org/10.1302/0301-620x.95b10.32281
Völlner F, Herl F, Greimel F, Benditz A, Renkawitz T, Grifka J, Craiovan B, Weber M (2020) The effects of soft tissue lateral release on the stability of the ligament complex of the knee. Arch Orthop Trauma Surg 140(7):933–940. https://doi.org/10.1007/s00402-020-03422-6
Savov P, Mielke E, Windhagen H, Calliess T, Richter A, Ettinger M (2020) Higher revision rate for posterior cruciate-retaining than posterior-stabilized total knee arthroplasty for the treatment of valgus osteoarthritis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03618-w
Peterfy C, Li J, Zaim S, Duryea J, Lynch J, Miaux Y, Yu W, Genant HK (2003) Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test–retest reproducibility. Skelet Radiol 32(3):128–132. https://doi.org/10.1007/s00256-002-0603-z
Reichmann WM, Maillefert JF, Hunter DJ, Katz JN, Conaghan PG, Losina E (2011) Responsiveness to change and reliability of measurement of radiographic joint space width in osteoarthritis of the knee: a systematic review. Osteoarthr Carti/OARS Osteoarthr Res Soc 19(5):550–556. https://doi.org/10.1016/j.joca.2011.01.023
Author information
Authors and Affiliations
Contributions
Study conception and design: FB, KR, MFK; Material preparation, data collection and analysis: KR, AR, AJ, MF; Draft of the manuscript: KR; Scientific supervision: FB.
Corresponding author
Ethics declarations
Conflict of interest
Author FB has received royalties from Smith and Nephew and OrthoDevelopment and is consultant for Smith and Nephew, OrthoDevelopment, DePuy and Medtronic. He receives research support as a principal investigator for DePuy. All other authors declare they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. The study received IRB approval by the institutional review board at the Hospital for Special Surgery (IRB number: 2017 – 0418).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rueckl, K., Runer, A., Jungwirth-Weinberger, A. et al. Severity of valgus knee osteoarthritis has no effect on clinical outcomes after total knee arthroplasty. Arch Orthop Trauma Surg 141, 1385–1391 (2021). https://doi.org/10.1007/s00402-021-03785-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03785-4