Abstract
Purpose
To evaluate the effects of kinesiophobia on both phases immediately after surgery and the final results after total knee arthroplasty (TKA).
Methods
This study evaluated prospectively 101 patients (mean age 66 ± 8.0 years, 70 women and 31 men), 5 days after surgery, at 1, 6, 12 months, and at a mean final follow-up of 3.2 ± 0.7 years (2.0–4.2 years). Kinesiophobia was assessed with the Tampa Scale for Kinesiophobia (TSK: Activity Avoidance—TSK1 and Harm—TSK2 subscales), and results were evaluated with range of motion, pain and function on 0–10 numeric rating scales, WOMAC and SF-12 (Physical and Mental subscales) scores.
Results
TSK1 was correlated with the acute postoperative pain measured at 5 days (p = 0.031), pain measured at 12 months (p = 0.018), patient perceived function at 12 months (p = 0.025), SF-12P at 6 months (p < 0.001), SF-12P and SF-12M at 12 months (p = 0.001 and p = 0.005, respectively), and WOMAC at both 6 and 12 months of follow-up (p = 0.005 and p = 0.001). The effect of TSK 1 on the final WOMAC score was significant when corrected by age and sex (p = 0.049, η 2 = 0.041): the youngest female patients were affected even by moderate kinesiophobia levels.
Conclusions
Fear of pain and even more avoidance of movement are strongly correlated both with the acute postoperative pain perception and recovery after surgery up to 1 year, thus presenting a relevant clinical impact on the outcome after TKA. Moreover, this study showed that even though at longer follow-up its impact decreases, patients with higher levels of kinesiophobia may present a poorer final outcome, especially women.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is an effective surgical technique which generally improves quality of life [8]. However, although studies focusing on survivorship or surgeon-based measures have generally reported high success rates, problems often persist [24]. In fact, these measures fail to take into consideration post-surgical chronic pain, which may be a heavy burden for up to 30 % of patients after TKA [21]. Since pain reduction is one of the primary reasons for undergoing surgery [8], and considering the exponential increase in TKA and potential revision procedures, this outcome is becoming a major concern not only for patients, but also for researchers and health care providers [14].
A number of studies have focused on the evaluation of factors associated with the persistency of pain after TKA, aimed at recognizing patients at risk and potentially target risk factors [14]. Besides demographic factors such as age, sex, and body weight, psychological factors are increasingly being recognized as a determinant for the final outcome [10, 11], with converging evidence of pain disability resulting not only from pain severity, but rather patients’ interpretation and adjustment to their pain [2]. According to the fear-avoidance model, which explains the role of emotional, cognitive, and behavioural factors in terms of chronic pain and disability, pain can induce a negative appraisal with fear of pain and fear of movement beliefs such as kinesiophobia [13]. Kinesiophobia is a maladaptive strategy that leads to the avoidance of physical activity because of pain-related fear [4], which may lead to illness behaviour and subsequent disability characterized by poor cognitive and physical performance, such as disuse syndrome, thus creating a vicious circle of pain and disability [15]. Although the influence of kinesiophobia on disability in patients affected by knee OA has been already studied, and recent evidence also suggests a correlation with the post-surgery recovery time [4], less explored is its impact on the final outcome after TKA.
Our hypothesis was that both recovery and final results after TKA may be affected by kinesiophobia. Thus, the aim of this study is to prospectively evaluate a large cohort of patients up to a midterm follow-up to document the kinesiophobia effects on patient improvement after TKA.
Materials and methods
All patients who underwent primary TKA at the Rizzoli Orthopaedic Institute (Bologna, Italy) between January 2011 and June 2013 and who were willing to participate were included in this study. Patients who were unable to complete the questionnaires independently because of emotional, cognitive, or language barriers were also excluded from this study.
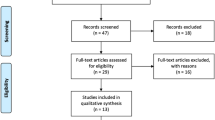
In total, 148 patients were enrolled for the study (232 were screened and asked to participate, and 84 did not accept to fill the requested questionnaires). During the study period, 19 patients were excluded because they underwent: TKA on the opposite knee (n = 13), total hip arthroplasty (n = 2), or because of medical reasons not related to their knee (n = 4). One patient refused to answer to follow-up questionnaires, 24 were not found at follow-up, and 3 died. Consequently, 101 patients were included in the study analysis (Fig. 1). The mean age of this patient cohort was 65.6 ± 8.0 years (median and range 65.0 and 45.0–83.0, respectively). Of these 101 patients, 70 were women and 31 men, BMI 28.5 ± 4.3 (median and range 28.0 and 18.5–39.5, respectively). Patient educational level ranges from elementary school (36 patients), middle school (27), high school (32), and university level (6). The same operation technique with a medial parapatellar approach was used in all the examined patients, who then underwent the same rehabilitation programme during their hospital stay.
Patients were evaluated preoperatively, 5 days after surgery, at 1, 6, 12 months, and at a mean final follow-up of 3.2 ± 0.7 years (median and range 3.3 and 2.0–4.2 years, respectively).
The basal evaluation included the assessment of pain and function on 0–10 numeric rating scales. Moreover, patients completed the following scores: Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) [1], SF-12 [22], and Tampa Scale for Kinesiophobia (TSK) [16].
TSK [20] is one of the most widely used questionnaires for assessing pain beliefs and pain-related fear of movement/reinjury of subjects with musculoskeletal complaints [16]. A 13-item version of the original 17-item self-reported questionnaire was used, with higher scores representing stronger fear-avoidance beliefs in two subscales called Activity Avoidance—TSK1 (a belief that activities causing pain should be avoided) and Harm—TSK2 (a belief that pain is a sign of bodily damage).
Pain was evaluated, together with both active and passive range of motion (ROM) measurements (measurements were taken with a goniometer, with a 2° accuracy), at 5 days of follow-up. Pain and patient perception of function were then evaluated at 1, 6, and 12 months, and at the final follow-up. SF-12 was repeated at 1, 6, and 12 months, and at the final follow-up, and WOMAC was collected also at 6, 12 months, and at the final follow-up.
The first phase of the analysis involved the evaluation of the improvement over time in terms of pain, function, and SF-12. The second phase of the analysis focused on the correlation of kinesiophobia with the previously mentioned scores, as well with WOMAC score over time. Other factors that may have influenced the results after TKA were then explored. Finally, a multivariate analysis was performed to test whether specific patient subgroups were affected differently by kinesiophobia at the final follow-up. This study was approved by the Hospital Ethics Committee and Internal Review Board of the Rizzoli Orthopaedic Institute (Prot. 0032215), and informed consent was obtained from all patients.
Statistical analysis
All continuous data were expressed in terms of the mean and the standard deviation of the mean, and the categorical data were expressed as frequency. The Kolmogorov–Smirnov test was performed to test normality of continuous variables. The repeated-measures general linear model (GLM) with Sidak’s test for multiple comparisons was performed to assess the differences at different follow-up times. The Pearson correlation was used as a univariate analysis to assess the relationship between continuous data. The GLM was used as a multivariate analysis to assess the influence of TSK on the results. For all tests, p < 0.05 was considered significant.
All statistical analysis was performed using SPSS v.19.0 (IBM Corp., Armonk, NY, USA).
Results
Pain significantly improved after treatment at all follow-ups (p < 0.0005), with an increasing improvement for up to 12 months (p < 0.0005) and then stable results up to the final follow-up (Fig. 2). Function improved after treatment at all follow-ups (p < 0.0005), with an increasing improvement up to 6 months (p < 0.0005) and then stable results up to the final follow-up (Fig. 3). SF-12 Physical Health subscale significantly improved after treatment at all follow-ups (p < 0.0005), with an increasing improvement up to 12 months (p < 0.0005) and then stable results up to the final follow-up (Fig. 4). SF-12 Mental Health subscale significantly improved after treatment at 6 and 12 months and at the final evaluation with respect to the basal evaluation (p < 0.0005, p = 0.002, p = 0.007, respectively) (Fig. 4).
SF-12 Physical Health subscale significantly improved after treatment at all follow-ups, with an increasing improvement up to 12 months and then stable results up to the final follow-up. SF-12 Mental Health subscale significantly improved after treatment at 6 and 12 months and at the final evaluation with respect to the basal evaluation
The influence of kinesiophobia on the measured outcomes was analysed separately for the two TSK subscales. TSK1 was correlated with the acute postoperative pain measured at 5 days (p = 0.031, R = 0.225), with pain (p = 0.018, R = 0.234), and patients’ perceived function at 12 months (p = 0.025, R = −0.223), with SF-12 at 6 and 12 months (p < 0.001, R = −0.320 for the Physical Health SF-12 subscale at 6 months, p = 0.001, R = −0.334 for Physical Health SF-12 subscale at 12 months and p = 0.005, R = −0.277 for Mental Health SF-12 subscale at 12 months), and with WOMAC at both 6 and 12 months of follow-up (p = 0.005, R = 0.279 and p = 0.001, R = 0.317, respectively), although no correlation was found at the final mean 3-years follow-up. TSK2 correlated with the basal function (p = 0.006, R = −0.270), but no statistically significant correlations were reached with the post-operative scores. Neither TSK1 nor TSK2 subscales showed any correlation with both active and passive ROM.
Further analysis was performed to analyse parameters that may have influenced the results after TKA. Gender, age, BMI, and educational level did not correlate with the clinical outcome.
Finally, a multivariate analysis was performed to test whether specific patient subgroups were affected differently by kinesiophobia at the final follow-up. The analysis showed that the effect of TSK1 on the final WOMAC score was significant when corrected by age and sex (p = 0.049, η 2 = 0.041): men with a TSK1 score of higher than 20 presented a worse WOMAC score at the final evaluation, regardless of age, whereas in women TSK1 influenced the final results with values higher than 12, with the youngest female patients being affected even by moderate kinesiophobia levels.
Discussion
The most important finding of the present study was that kinesiophobia influences the outcome after TKA, with a different impact on patient’s quality of life and functional improvement according to the time after surgery.
This is in accordance with the fear-avoidance model: if pain is perceived as harmful, pain-related fears (referred to as pain catastrophizing) may develop, which may lead to hypervigilance towards body sensations, such as touch or movement, and to the avoidance of certain behaviours [4].
The amplification of these cognitive and behavioural disorders may impede recovery. In fact, these patients have difficulties in not focusing on the painful or threatening stimulus, which intensifies fear of pain and further increases the attention paid to the stimulus, a vicious circle where the excessively emotional evaluation of pain causes an overall higher perception of the experience of pain [3]. Indeed, in these patients, MRI evaluation showed that chronic pain was associated not only with higher degrees of activity in brain processing areas, but also in areas related to attention, anticipation, and emotional aspects of pain [7]. These psychological processes that lead to adverse pain outcomes may also influence pain modulation through neurophysiological processes, as suggested by studies showing poorer response to opioids for both clinical and experimental pain [19]. Pain catastrophizing may interfere with descending pain-inhibitory systems, facilitate neuroplastic changes in the spinal cord during repeated painful stimulation, and in the end promote pain sensitization [6]. This further sustains the fear-avoidance model, where pain-related fears lead to activity avoidance or escape, which in turn contributes to functional disability. This inactivity has a major impact not only in terms of TKA success, but also on general health, since patients with prolonged periods of inactivity compound disability with deconditioning and higher risks of developing co-morbidities (i.e. obesity and diabetes) [9].
In this light, understanding the influence of psychological factors such a kinesiophobia on the outcome of TKA is of primary importance to identify patients at risk and support interventions to overcome dangerous barriers to full recovery [4]. Currently, only a few studies have evaluated the impact of kinesiophobia on TKA, mainly focusing on its influence on the post-operative recovery phase.
Panchout et al. [4] strictly focused on the hospitalization period for postoperative rehabilitation after TKA and assessed the outcome of 89 consecutive patients. Although no differences were found in terms of duration of hospitalization, maximum passive flexion, or pain intensity, patients without kinesiophobia walked significantly farther, regardless of the presence of obesity. Unver et al. [20] evaluated a small cohort of women undergoing primary bilateral TKA for the treatment of knee OA; although having improved stair ability at 8 weeks and decreased pain at 4 weeks post-surgery, patients still presented fear of falling by 26 weeks and had a strong relationship between fear of falling and stair activities throughout the study time. A more extensive evaluation was more recently performed by Kocic et al. [12], who followed 78 patients treated with primary TKA for up to 6 months. They documented both the high frequency of fear of movement, with a 21.8 % rate, and the impact on the clinical outcome, with poorer results in terms of pain, flexion, and function.
Besides these short-term reports on kinesiophobia, other studies have evaluated TKA results more generally to show a more exaggerated negative orientation towards noxious stimuli. Witvrouw et al. [23] focused on the hospitalization of 43 patients and found catastrophic thinking as a predictor of hospital stay after TKA, whereas other authors evaluated results in the post-acute phase. In particular, a systematic review [2] recently analysed the available evidence of studies focusing on results after at least 3 months after surgery, based on the rationale that pain after 3 months of duration can be considered as chronic, given that it exceeds typical healing time and often constitutes its own disorder that can perpetuate functional disability. Burns et al. identified six prospective longitudinal studies with small-to-medium-sized cohorts and overall short follow-ups. In five out of the six manuscripts, pain catastrophizing was found to be a significant predictor of chronic pain persisting more than 3 months after TKA.
The literature provides moderate-level evidence on the overall influence of pain catastrophizing in the short-term results after TKA, but there is a lack of reports to demonstrate the influence of this psychological component on the final outcome, in particular when considering specifically the impact of kinesiophobia, a key aspect especially for these orthopaedic patients where post-operative movement is both an outcome measure and a necessary component of the rehabilitation process to optimize the overall results.
This study showed, in the largest available cohort of patients undergoing TKA and prospectively followed at the longest final follow-up, that kinesiophobia has a marked influence on the overall results, with a different impact according to the post-operative phase considered. Kinesiophobia influenced the acute post-surgical pain perception and maintained a strong correlation with both pain and function for up to 1 year of follow-up. Moreover, with respect to the current literature, this study showed that afterwards the overall impact of kinesiophobia on the functional result decreased, but the final outcome still remained lower in patients where this psychological component was higher, especially in women. An interesting finding is that the highest correlation between kinesiophobia and results over time was found for the subscale of the score focused on the avoidance of movement in agreement with the findings of Panchout et al. [4]. The activity avoidance may jeopardize both rehabilitation and final recovery, but may also be the focus for targeted treatments. Monticone et al. [15] performed a randomized controlled trial on 110 patients followed up for 6 months and found that a home-based programme based on functional exercises for the management of kinesiophobia was effective in improving disability and quality of life after TKA.
This kind of maladaptive cognition may be effectively managed, and the consequent pain perception and activity avoidance may be positively influenced as well. Wade et al. [21] showed that as pain subsides after surgery for knee OA, catastrophizing does as well, thus challenging its categorization as a stable trait like a personal component. Pain is a multidimensional phenomenon composed of sensitive, cognitive-evaluative, and affective-motivational domains, with a dynamic bidirectional modulation of catastrophizing and perception of pain [16]. Thus, conventional biomedical treatments and cognitive-behavioural treatment may synergically contribute to improving symptoms, having overcome the fear of physical activity, and in the end might improve both patient recovery and final outcome after TKA.
This study presents some limitations. The same prosthesis model has not been used for all patients, which could represent a bias in terms of outcome. However, the high number of patients evaluated represents a strength that should ensure robust findings to be found in terms of psychological influence on the outcome. Even though patients were prospectively enrolled, some patients refused to complete the questionnaires and some were lost to follow-up, due to other diseases or age-related problems. Moreover, many factors may contribute to persisting pain and limited function after TKA [5, 14, 17, 18], and they should be considered to assess each specific contribution to the final results. However, the large cohort of patient evaluated for up to a mean of 3-year follow-up allowed us to observe the influence of kinesiophobia over time, with a more significant impact in the recovery phase up to 12 months and, to a lesser extent, a persisting negative gender-related correlation, with the final outcome affected especially in women with the highest level of kinesiophobia. Thus, these findings are of clinical relevance because they show the impact of kinesiophobia and suggest the possibility of adopting co-interventions to reduce catastrophizing thinking and kinesiophobia and in the end to improve the results of TKA.
Conclusions
Kinesiophobia is a risk factor that may affect TKA results. Fear of pain and even more avoidance of movement are strongly correlated with both the acute postoperative pain perception and recovery after surgery up to 1 year. Even though at longer follow-up times its impact decreases, patients with higher levels of kinesiophobia may present a lower final outcome, especially women. Individuals at risk of pain-related fear of movements should be identified for a proper preoperative assessment of a problematic outcome and be targeted with interventions to prevent the development of pain and disability after TKA.
References
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15(12):1833–1840
Burns LC, Ritvo SE, Ferguson MK, Clarke H, Seltzer Z, Katz J (2015) Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: a systematic review. J Pain Res 5(8):21–32
Doménech J, Sanchis-Alfonso V, Espejo B (2014) Changes in catastrophizing and kinesiophobia are predictive of changes in disability and pain after treatment in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc 22(10):2295–2300
Doury-Panchout F, Metivier JC, Fouquet B (2015) Kinesiophobia negatively influences recovery of joint function following total knee arthroplasty. Eur J Phys Rehabil Med 51(2):155–161
Feldman CH, Dong Y, Katz JN, Donnell-Fink LA, Losina E (2015) Association between socioeconomic status and pain, function and pain catastrophizing at presentation for total knee arthroplasty. BMC Musculoskelet Disord 7(16):18
Goodin BR, McGuire L, Allshouse M, Stapleton L, Haythornthwaite JA, Burns N, Mayes LA, Edwards RR (2009) Associations between catastrophizing and endogenous pain-inhibitory processes: sex differences. J Pain 10(2):180–190
Gracely RH, Geisser ME, Giesecke T, Grant MA, Petzke F, Williams DA, Clauw DJ (2004) Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain 127(Pt 4):835–843
Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D (1998) Health-related quality of life after knee replacement. J Bone Joint Surg Am 80(2):163–173
Heuts PH, Vlaeyen JW, Roelofs J, de Bie RA, Aretz K, van Weel C, van Schayck OC (2004) Pain-related fear and daily functioning in patients with osteoarthritis. Pain 110(1–2):228–235
Hirakawa Y, Hara M, Fujiwara A, Hanada H, Morioka S (2014) The relationship among psychological factors, neglect-like symptoms and postoperative pain after total knee arthroplasty. Pain Res Manag 19(5):251–256
Hirschmann MT, Testa E, Amsler F, Friederich NF (2013) The unhappy total knee arthroplasty (TKA) patient: higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surg Sports Traumatol Arthrosc 21(10):2405–2411
Kocic M, Stankovic A, Lazovic M, Dimitrijevic L, Stankovic I, Spalevic M, Stojiljkovic P, Milenkovic M, Stojanovic Z, Nikolic D (2015) Influence of fear of movement on total knee arthroplasty outcome. Ann Ital Chir 86:148–155
Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW (2007) The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 30(1):77–94
Lewis GN, Rice DA, McNair PJ, Kluger M (2015) Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 114(4):551–561
Monticone M, Ferrante S, Rocca B, Salvaderi S, Fiorentini R, Restelli M, Foti C (2013) Home-based functional exercises aimed at managing kinesiophobia contribute to improving disability and quality of life of patients undergoing total knee arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil 94(2):231–239
Monticone M, Giorgi I, Baiardi P, Barbieri M, Rocca B, Bonezzi C (2010) Development of the Italian version of the Tampa Scale of Kinesiophobia (TSK-I): cross-cultural adaptation, factor analysis, reliability, and validity. Spine (Phila Pa 1976) 20 35(12):1241–1246
Noiseux NO, Callaghan JJ, Clark CR, Zimmerman MB, Sluka KA, Rakel BA (2014) Preoperative predictors of pain following total knee arthroplasty. J Arthroplasty 29(7):1383–1387
Rakel BA, Blodgett NP, Zimmerman MB, Logsden-Sackett N, Clark C, Noiseux N, Callaghan J, Herr K, Geasland K, Yang X, Sluka KA (2012) Predictors of postoperative movement and resting pain following total knee replacement. Pain 153(11):2192–2203
Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, Dunbar M (2009) Psychological determinants of problematic outcomes following total knee arthroplasty. Pain 143(1–2):123–129
Unver B, Ertekin Ö, Karatosun V (2014) Pain, fear of falling and stair climbing ability in patients with knee osteoarthritis before and after knee replacement: 6 month follow-up study. J Back Musculoskelet Rehabil 27(1):77–84
Wade JB, Riddle DL, Thacker LR (2012) Is pain catastrophizing a stable trait or dynamic state in patients scheduled for knee arthroplasty? Clin J Pain 28(2):122–128
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Witvrouw E, Pattyn E, Almqvist KF, Crombez G, Accoe C, Cambier D, Verdonk R (2009) Catastrophic thinking about pain as a predictor of length of hospital stay after total knee arthroplasty: a prospective study. Knee Surg Sports Traumatol Arthrosc 17(10):1189–1194
Wylde V, Dieppe P, Hewlett S, Learmonth ID (2007) Total knee replacement: Is it really an effective procedure for all? Knee 14(6):417–423
Acknowledgments
The authors thank Dr. Elettra Pignotti for statistical assistance and Mr Keith Smith for English editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Filardo, G., Roffi, A., Merli, G. et al. Patient kinesiophobia affects both recovery time and final outcome after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24, 3322–3328 (2016). https://doi.org/10.1007/s00167-015-3898-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3898-8