Research studies focusing on the fear-avoidance model have expanded considerably since the review by Vlaeyen and Linton (Vlaeyen J. W. S. & Linton, S. J. (2000). Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain, 85(3), 317--332). The fear-avoidance model is a cognitive-behavioral account that explains why a minority of acute low back pain sufferers develop a chronic pain problem. This paper reviews the current state of scientific evidence for the individual components of the model: pain severity, pain catastrophizing, attention to pain, escape/avoidance behavior, disability, disuse, and vulnerabilities. Furthermore, support for the contribution of pain-related fear in the inception of low back pain, the development of chronic low back pain from an acute episode, and the maintenance of enduring pain, will be highlighted. Finally, available evidence on recent clinical applications is provided, and unresolved issues that need further exploration are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Despite the fact that almost anyone may experience an acute low back pain (LBP) episode at least once during his/her life, only a small minority develop a chronic low back pain (CLBP) problem (Waddell, 2004b). A traditional biomedical model that focuses upon structural and biomechanical abnormalities cannot sufficiently explain chronic pain and its associated disability. A biopsychosocial model may provide a better account because it also includes psychological and social factors (Waddell, 2004a). One psychological factor that has received much attention in the case of (chronic) pain is fear. Before describing the role of fear in the domain of pain, let us first briefly examine fear and anxiety in general as an introduction.
Fear and Anxiety: A Brief Introduction
Fear is the emotional reaction to a specific, identifiable and immediate threat, such as a dangerous animal or an injury (Rachman, 1998). Fear may protect the individual from impending danger as it instigates defensive behavior that is associated with the fight or flight response (Cannon, 1929). The three main components of fear (interpretation of the stimulus as threatening, increased sympathetic arousal, and defensive behavior) are loosely coupled and can change at different paces (Lang, 1979; Rachman and Hodgson, 1974). Defensive escape behaviors reduce fear levels in the short term, but may strengthen the fear in the long run. Not least they may prevent disconfirmation of the patient's beliefs and sometimes they make the feared outcome more likely to occur. Three recent findings in fear research are notable. First, people with a phobia (intense irrational fear) do not necessarily have a history of being exposed to a traumatic incident (Hermans et al., 2006). Second, during extinction procedures, no unlearning takes place, but rather new learning that leaves the original association between the conditioned and unconditioned stimulus intact, making relapse likely (Bouton, 2002). Third, individual differences in vulnerabilities exist that can affect how likely fear will be experienced, acquired or maintained over time (Mineka and Zinbarg, 2006).
Anxiety, in contrast to fear, is a future-oriented affective state and the source of threat is more elusive without a clear focus. Even though the components of anxiety are similar to those of fear, they are less intense. Furthermore, whereas fear motivates the individual to engage in defensive behaviors, anxiety is associated with preventative behaviors, including avoidance. An important component of anxiety is hypervigilance, which occurs when the individual engages in environmental scanning for potential sources of threat, selectively attends to threat-related rather than neutral stimuli, broadens the attention prior to the detection of these stimuli, and narrows the attention in the presence of such stimuli (Eysenck, 1992). Both avoidance behavior and hypervigilance reduce anxiety in the short term, but may be counterproductive in the long run. Clinically, the distinction between fear and anxiety is less evident, and these terms are frequently used interchangeably.
FEAR AND PAIN
Building upon the knowledge derived from the general fear and anxiety research, the contribution of fear and anxiety in the area of (chronic) pain has been increasingly acknowledged. Pain-related fear and anxiety can best be defined as the fear that emerges when stimuli that are related to pain are perceived as a main threat. The fear and anxiety response comprises psychophysiological (e.g. heightened muscle reactivity), behavioral (e.g. escape and avoidance behavior), as well as cognitive (e.g. catastrophizing thoughts) elements. Depending on the current concerns, different stimuli are attended to and possibly misinterpreted. Fear of pain, fear of work-related activities, fear of movement, and fear of (re)injury have been described as often occurring in patients suffering pain.
The Fear-Avoidance Model of Pain
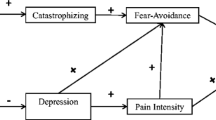
Based upon previous work (Lethem et al., 1983; Philips, 1987; Waddell et al., 1993), Vlaeyen et al. (1995) and Vlaeyen and Linton (2000) proposed a cognitive behavioral model of CLBP that has become known as the fear-avoidance model. This particular model provides an explanation of why CLBP problems and associated disability develop in a minority of those experiencing acute LBP. The basic tenet of the model is that the way in which pain is interpreted may lead to two different pathways (Fig. 1). When acute pain is perceived as non-threatening, patients are likely to maintain engagement in daily activities, through which functional recovery is promoted. In contrast, a vicious circle may be initiated when the pain is catastrophically (mis)interpreted. These dysfunctional interpretations give rise to pain-related fear, and associated safety seeking behaviors such as avoidance/escape and hypervigilance, that can be adaptive in the acute pain stage, but paradoxically worsen the problem in the case of long-lasting pain. The long-term consequences, such as disability and disuse, in turn may lower the threshold at which subsequent pain will be experienced.
The terms fear and anxiety are often used interchangeably with regard to pain. As emphasized above, the distinction between anxiety and fear is theoretically correct, but difficult to make in a clinical context, especially in chronic pain where the threatening stimulus (pain) is constantly present. Asmundson et al. (2004) tried to differentiate between fear and anxiety and presented an updated fear-anxiety-avoidance model. In this updated model, there is no longer a direct link between fear and avoidance behavior, because by definition one cannot avoid a threat that is already present. Instead, they added an anxiety pathway in the anticipation of pain to the fear pathway in the presence of pain. In Fig. 1, both the fear and anxiety pathways are graphically presented. Since it is not yet evident that this updated model added value to the original one, and because of the remaining debate about clinical distinctiveness of fear and anxiety, we will use the term pain-related fear in the remainder of this review.
The Fear-Avoidance Model of Pain: Evidence for its Components
Since the review by Vlaeyen and Linton (2000), numerous research studies have been undertaken in an attempt to further validate the fear-avoidance model, basically focusing on the interrelationships between its constitutive components. Below, the current scientific evidence for the separate elements of the fear-avoidance model will be discussed. The component ‘pain-related fear’ and its contribution in various stages of LBP will be separately addressed in section 3, because of its central position in the fear-avoidance model and the large body of research dedicated to it.
Pain Severity
Until recently, the research literature on the fear-avoidance model did not ascribe a role of importance to pain intensity. In their review, Vlaeyen and Linton (2000) concluded that pain intensity is not a primary factor in avoidance behavior or disability. It has even been provocatively stated that ‘pain-related fear is more disabling than pain itself (Crombez et al., 1999b). It is possible that this may be the case in a subgroup of chronic pain patients, but it has become clear that high pain intensity is in itself a threatening experience that drives escape and avoidance (Eccleston and Crombez, 1999). Indeed, numerous recent studies have shown that pain intensity has a considerable contribution in explaining disability. For example, pain was strongly related to functional disability during the acute stage of LBP (Gheldof et al., 2006; Sieben et al., 2005a), whereas previous LBP history and pain intensity were the best predictors of future disability (Sieben et al., 2005b). Such a relationship may be important for chronic pain as well (Leeuw et al., in press; Mannion et al., 2001; Boersma and Linton, 2005a; Peters et al., 2005; Sorbi et al., 2006; van den Hout et al., 2001a; Woby et al., 2004a). From these current studies, it can be concluded that the association between pain and disability both during the acute and chronic stages of pain may be more important than previously suggested.
Pain Catastrophizing
The term catastrophizing was first coined by Ellis (1962) for the process in which anxious patients dwell on the most extreme negative consequences conceivable. Pain catastrophizing can best be conceived as the cognitive element of the fear network, besides physiological reactivity and behavioral responses, and refers to the process during which pain is interpreted as being extremely threatening (Crombez et al., 1998; Rosenstiel and Keefe, 1983). Pain catastrophizing has consistently been associated with pain disability in pain patients (Peters et al., 2005; Sullivan et al., 2005a; Turner et al., 2004), as well as in the general population (Severeijns et al., 2004). For example, Sullivan et al. (2002) provided prospective support that initial levels of pain catastrophizing were related to subsequent activity intolerance.
In addition to its association with disability, pain catastrophizing may be related to intensified pain in various pain problems (Buer and Linton, 2002; Haythornthwaite et al., 2003; Peters et al., 2005; Severeijns et al., 2001; Sullivan et al., 2005a; Turner et al., 2002, 2004). However, all these studies are correlational, allowing no causal inferences. In this context, a study by Arntz and Claassens (2004) is notable. This study experimentally manipulated the meaning assigned to a painful stimulus and examined its influence on the pain experience. Healthy volunteers, who were led to believe that a cold metal bar to the neck was hot, rated it as more painful and ascribed more damaging properties to it than other healthy volunteers, who were led to believe that the same bar was cold. The damaging interpretation mediated the relationship between the experimental manipulation and the pain experienced. Prospective studies further demonstrated that initial pain catastrophizing is related to higher pain intensity in a variety of situations, e.g. during a subsequent painful procedure (Edwards et al., 2004; Pavlin et al., 2005; Sullivan et al., 1995; Sullivan and Neish, 1999; Sullivan et al., 2004; Vlaeyen et al., 2004b), after an operation (Granot and Ferber, 2005), and in the long-term adjustment to lower-limb amputation and phantom limb pain (Hanley et al., 2004).
There is also some evidence that pain catastrophizing may be considered as a precursor of pain-related fear. For example, Leeuw et al. (in press) demonstrated that in LBP sufferers in the general population, pain catastrophizing was related to pain-related fear six months later, even after accounting for other contributing variables such as initial levels of pain-related fear. Also, Vlaeyen et al. (2004b) found that initial levels of pain catastrophizing were related to subsequent increases in fear during internal atrial cardioversion.
Attention to Pain
Pain that is intense, or that is perceived as threatening, demands attention and may interrupt ongoing activities (Eccleston and Crombez, 1999; Pincus and Morley, 2001). Various studies have demonstrated that excessive attention to pain is dependent upon the presence of pain-related fear (Goubert et al., 2004b; Keogh et al., 2001; Peters et al., 2000; Van Damme et al., 2006). For example, studies that found decreased cognitive task performance in fearful LBP patients interpreted this to be the result of pain-related fear directing attention to pain (Crombez et al., 1999a, 2002a; de Gier et al., 2003; Peters et al., 2002; Eccleston et al., 1997; Rode et al., 2001). Furthermore, diminished attentional bias due to treatment appeared to be mainly explained by reductions in pain-related fear, suggesting that pain vigilance results from pain-related fear (Dehghani et al., 2004). Also pain catastrophizing has been shown to increase the attentional demand of pain in experimental settings (Crombez et al., 2002a; Van Damme et al., 2002, 2004b; Vancleef and Peters, 2006). Although it might be suggested that excessive attention to pain mediates the relationship between pain-related fear and increased pain intensities, there is only little evidence supporting this idea (Crombez et al., 2005). Instead, pain-related fear and pain vigilance seem to contribute independently to the experience of pain (Arntz and Claassens, 2004; Roelofs et al., 2004).
Insight into particular aspects of attentional processes has substantially increased in the past few years (see for a review: Crombez et al., 2005). Evidence converges upon the idea that attentional disruption by pain-related information is not the result of an initial shift of attention to the pain stimuli, but rather stems from difficulties in disengaging attention from these stimuli (Asmundson et al., 2005; Crombez et al., 2005; Roelofs et al., 2005). More evidence comes from studies showing that impeded disengagement seems to be pronounced in high catastrophizers (Van Damme et al., 2004b) For example, it was demonstrated that high pain catastrophizers had more difficulty in disengaging their attention from pain cues than low catastrophizers, because of the erroneous conviction that these pain cues signaled subsequent pain targets (Van Damme et al., 2002). Additionally, it may be that attentional engagement is facilitated by the anticipation of pain (Van Damme et al., 2004a). Interestingly, it was found that an experimentally induced attentional bias was reduced during extinction, but that it easily returned when the feared stimulus was again encountered (Van Damme et al., 2006), which is highly likely in case of chronic pain. In sum, there is evidence that attention may be an important feature in pain perception as predicted by the model.
Escape/Avoidance Behavior
Avoidance refers to behavior aimed at postponing or preventing an aversive situation from occurring (Kanfer and Philips, 1970). Although in case of chronic pain it is not possible to avoid the pain, it is possible to avoid the perceived threat, in this case the activities that are assumed to increase pain or (re)injury. Avoidance behavior might thus be reflected in submaximal performance of activities. Vlaeyen and Linton (2000) presented an impressive overview of studies demonstrating that fearful CLBP patients performed less well on behavioral performance tasks, pointing to possible withdrawal, and thus avoidance, from these tasks. A number of more recent studies also support this assumption. For example, pain-related fear was associated with decreased speed in both preferred and fast walking (Al-Obaidi et al., 2003), with weakened muscle strength (Al-Obaidi et al., 2000; Goubert et al., 2005b), and with diminished performance on physical tasks (Geisser et al., 2000; Vowles and Gross, 2003). For instance, it was shown that in addition to experimentally induced pain anticipation, fear avoidance beliefs were related to diminished physical task performance (Pfingsten et al., 2001).
Disability
Disability refers to problems in executing daily life tasks and activities, in the home as well as the work situation. Disability may be a logical consequence of prolonged avoidance behavior and hypervigilance. It seems clear that avoidance behaviors as defined above have an impact on daily life tasks. Also hypervigilance may contribute to disability. The selective attention to pain-related stimuli, and the associated difficulty with disengaging from these stimuli, might occur at the cost of vigilance to the usual tasks of daily life. Indeed, a large body of research found that CLBP patients with heightened levels of pain-related fear report increased disability (Boersma and Linton, 2005a; Denison et al., 2004; Goubert et al., 2005b; Leeuw et al., in press; Peters et al., 2005; Staerkle et al., 2004; Turner et al., 2000; van den Hout et al., 2001a; Woby et al., 2004a). However, whether the association between pain-related fear and disability is mediated by both avoidance/escape behaviors and hypervigilance has not been examined yet.
Disuse
In addition to the development of functional disability, frequent and enduring avoidance of daily activities may also result in gradual deterioration of a person's muscular system and fitness. The term “disuse syndrome” refers to the physiological and psychological effects of a reduced level of physical activity in daily life (Verbunt et al., 2003a). Thus far, lower or equal daily life activity levels were found when comparing CLBP patients with healthy controls, although the number of studies is rather small (Nielens and Plaghki, 2001; Spenkelink et al., 2002; Verbunt et al., 2001).
Two other aspects of disuse seem relevant: physical deconditioning, which can either be expressed in weakened muscle strength or reduced aerobic fitness, and disordered muscle coordination during physical activity (so-called guarded movements). Although diminished muscle strength was consistently found in CLBP patients as compared to healthy controls (Brox et al., 2005; Kramer et al., 2005; Verbunt et al., 2005), this might be accounted for by submaximal performance owing to pain-related fear (Al-Obaidi et al., 2000; Goubert et al., 2005b; Verbunt et al., 2005). Therefore, aerobic fitness level seems to be a more suitable measure of physical deconditioning. Generally, the physical fitness of CLBP patients is found to be either lower or equal to that of healthy subjects (Verbunt et al., 2003a). Only one current study succeeded in demonstrating that CLBP patients have lower aerobic fitness than matched healthy counterparts, though this could not be explained by pain-related fear or other relevant variables (Smeets et al., 2006a). Other studies also failed to establish significant relationships with regard to physical deconditioning as proposed by the fear-avoidance model (Brox et al., 2005; Verbunt et al., 2003b; Wittink et al., 2000, 2002).
Another aspect related to disuse is disturbed trunk muscle coordination that CLBP patients can present during physical activity. One study demonstrated that experimentally induced fear of pain had only subtle effects on the erector spinae during walking, while leaving the global pattern of trunk kinematics unaffected (Lamoth et al., 2004). More evidence was found by Geisser et al. (2004), who showed that among CLBP patients pain-related fear was not only associated with reduced lumbar flexion and greater EMG in full flexion, but also to abnormalities in the muscle activity during flexion from the standing position. These changes in musculoskeletal functioning and flexion may be important for the understanding of how pain may interfere with daily life functioning.
In sum, neither lower physical activity levels nor the physical consequences of long-term avoidance behavior in CLBP patients were unambiguously confirmed. It may be that these patients avoid certain activities, that is those that are assumed to increase pain or (re)injury, but in general maintain their physical activity levels comparable to healthy people who may be, in general, inactive themselves (Verbunt et al., 2003a). This might explain their serious functional limitations despite unaffected levels of activity. To elucidate the actual contribution of disuse in CLBP, in the future it may be important to study the consequences of LBP within an affected person instead of between groups (Verbunt et al., 2003a).
Vulnerabilities
An intriguing question concerns the etiology of pain catastrophizing and pain-related fear. Are there certain vulnerabilities that predispose individuals to overly attach negative appraisals to pain? If so, does this incline one to misinterpret ambiguous, but harmless, physical sensations as painful or threatening, thereby predisposing an individual to develop pain complaints (Arntz and Claassens, 2004; Pincus and Morley, 2001)? Asmundson et al. (1999) suggested that fear of pain may be secondary to the fundamental fear ‘anxiety sensitivity’, that is the fear of anxiety-related sensations associated with pain. Indeed, there is evidence that pain-related fear is related to anxiety sensitivity (Asmundson et al., 2000; Zvolensky et al., 2001), as well as injury/illness sensitivity (Vancleef et al., 2006), which in turn contributes to the broader construct of trait anxiety (Reiss, 1991). Along the same lines, the more general construct of negative affectivity (or neuroticism) has also been shown to lower the threshold at which pain is perceived as threatening (Gheldof et al., 2006; Goubert et al., 2004b). Because negative affectivity, anxiety sensitivity, and fear of pain seem to share some potential overlap, and at the same time differ in terms of generality, Keogh and Asmundson (2004) proposed to follow the idea put forward by Lilienfeld et al. (1993) in the context of personality research, in approaching these constructs as part of an interrelated hierarchy. In this hierarchy, the more general negative affectivity is placed at the top, and the more specific anxiety sensitivity and fear of pain at lower levels. Although it is not quite clear which specific trait is important for the development and course of LBP, it may be suggested that certain relatively stable vulnerability traits are important and should not be overlooked.
Although speculative, it may be that individuals with an increased vulnerability to catastrophizing and pain-related fear are less changeable in their fear avoidance beliefs than those without these vulnerabilities. For clinical practice, it would therefore be important to identify these stable personality traits, since their presence may require a different, and more thorough approach, than when addressing fear avoidance beliefs in patients without these vulnerabilities.
Above, the support for the separate components of the fear-avoidance models is outlined. To date, only two studies examined the interrelationships of various elements of the fear-avoidance model simultaneously using structural equation modeling. Goubert et al. (2004b) showed that pain catastrophizing and pain-related fear mediated the relationship between neuroticism and pain vigilance, and that pain vigilance was associated with heightened pain severity. Moreover, neuroticism was found to moderate the relationship between pain severity and pain catastrophizing. Cook et al. (2006) demonstrated that pain catastrophizing was related to pain-related fear, depression and disability, that pain-related fear was related to depression and disability, and that both depression and disability were related to pain severity. Although not allowing for causal inferences, which actually constitute the basic premises of the model, these studies do support the associations between various elements of the fear-avoidance model.
PAIN-RELATED FEAR DURING VARIOUS STAGES OF LBP
Although the fear-avoidance model was originally developed to explain the transition from acute to chronic pain, most of the research has been carried out with chronic pain patients, underscoring the evidence for pain-related fear as the mechanism behind the maintenance of chronic pain and pain disability. Nevertheless, more recently, researchers have begun to study the influence of the role of pain-related fear in individuals with acute pain episodes, and a handful of studies have even gone a step further and focused on pain-related fear as a risk factor for the development of pain episodes in pain-free individuals.
Pain-Related Fear as a Maintaining Factor of CLBP
One of the key mechanisms in the maintenance of anxiety disorders is the prolonged use of safety behaviors including escape from, and avoidance of, threatening situations, and the selective attention towards the possible sources of threat. As reviewed above, accumulating evidence seems to underscore the contribution of escape/avoidance behavior and hypervigilance in the area of chronic pain. Fearful pain patients may continuously scan their environment for potential signals of pain, and when the detected stimuli are interpreted as a threat, the attention is more likely to stay attached to those stimuli (Van Damme et al., 2002, 2004a). Not only may these disrupted attentional processes be associated with increased disability because of leaving less attention available for other tasks and activities, but also by leading to intensified pain (Arntz et al., 1994; Arntz and Claassens, 2004). The other possible maintaining factor is avoidance/escape behavior. When CLBP patients have detected a threatening situation, in this case a potential dangerous activity, they will either escape from the activity by not performing it at all, or avoid the activity by submaximal performance or the use of safety behaviors (Al-Obaidi et al., 2000; Goubert et al., 2005b). This behavior fuels the pain-related fear of these patients even further, first because it prevents them from discovering that these activities are harmless, and second because it promotes disability and disuse. Escape/avoidance behavior and disrupted attentional processes may therefore contribute to the maintenance of CLBP.
Pain-Related Fear as a Risk Factor for the Development of Chronic LBP
Due to differences in stringency in evaluating studies for their reviews, Linton (2000) concluded that fear avoidance beliefs were associated with both the inception and continuation of LBP, whereas Pincus et al. (2002) concluded that there was too little support for this conclusion and that instead distress and depressive mood affected the transition to chronicity. More recently, several studies have investigated pain-related fear during the acute pain phase. In acute LBP patients, pain-related fear was found to be associated with diminished participation in activities of daily life (Buer and Linton, 2002), greater perceived disability (Gheldof et al., 2006; Grotle et al., 2004; Swinkels-Meewisse et al., 2003, 2006a,2006b), greater work loss (Grotle et al., 2004), more frequent sick leave (Gheldof et al., 2005), and diminished performance on a lifting task (Swinkels-Meewisse et al., 2006a). Due to its associations with escape/avoidance behavior already during the acute pain phase, pain-related fear might contribute to the development of a chronic pain problem.
Several prospective studies indeed go further in demonstrating that fear avoidance beliefs can influence the transition to CLBP and associated outcomes, such as disability and sick leave. Picavet et al. (2002) showed that both heightened pain-related fear and pain catastrophizing during the acute phase increased the risk of future CLBP and disability. Accordingly, in acute LBP patients it was shown that initial elevated pain-related fear (Swinkels-Meewisse et al., 2006c), fear avoidance beliefs about work (George et al., 2005), or rising levels of pain-related fear in the beginning of a new episode (Sieben et al., 2002) were predictive of subsequent higher disability. Heightened initial levels of pain-related fear were also found to be related to decreased probability of returning to work and greater probability of being on sick leave (Boersma and Linton, 2005b; Fritz et al., 2001; Storheim et al., 2005), and to the recurrence of LBP and care seeking four years later (Burton et al., 2004). Two studies found only minor contributions of pain-related fear during the acute pain phase (Boersma and Linton, 2005a; Sieben et al., 2005a), whereas one study found pain-related fear to be unrelated to future disability (Sieben et al., 2005b). However, in the study of Sieben et al. (2005b) high fearful patients were underrepresented, and this may have resulted in an underestimation.
Pain-Related Fear as a Vulnerability Factor for the Inception of Acute LBP
The fear-avoidance model proposes that fear avoidance beliefs may come into play when an acute pain problem emerges. It therefore seems sensible to assume that fear avoidance beliefs also exist in pain-free people. These beliefs are probably based on previous LBP experiences, personality traits (Goubert et al., 2004b), or observational learning (Mineka and Zinbarg, 2006). Recent studies indeed demonstrated fear avoidance beliefs to be present in pain-free people. For example, pain-free people in the general population reported pain-related fear comparable to, or only slightly lower, than acute and chronic pain patients (Houben et al., 2005a). Furthermore, misconceptions, such as the belief that LBP is caused by tissue damage, were very common in the general population (Goubert et al., 2004a). During pain, these misconceptions may trigger pain-related fear.
These fear avoidance beliefs may act as a vulnerability factor for the inception of a new LBP episode in pain-free people. Fearful people may be more inclined to misinterpret ambiguous physical sensations as threatening or painful, and therefore have an increased likelihood to experience pain (Arntz and Claassens, 2004; Pincus and Morley, 2001). There is indeed some evidence that fear avoidance beliefs may heighten the probability of subsequently developing a new pain episode. In currently pain-free people, pain-related fear substantially increased the risk of the subsequent inception of LBP and diminished physical functioning (Linton et al., 1999). Additionally, in workers who were currently pain free, a higher risk for future LBP onset was found for those who catastrophized about pain (Linton, 2005), and for those with heightened pain-related fear (Van Nieuwenhuyse et al., 2006). Since these studies included participants who were pain-free during the past year, it is important to recognize that the included participants were not pain-free in the sense that they had never experienced LBP before. Due to its high prevalence (Waddell, 2004b), it is very likely that these people had suffered from previous LBP episodes, which also might have influenced the initiation of a new episode.
PAIN-RELATED FEAR AND TREATMENT
The aforementioned findings suggest that pain-related fear may not only be associated with the inception of a LBP episode, but also with the transition from acute to CLBP, and the maintenance of a chronic pain problem. From this knowledge we may deduce that pain-related fear could be an important target for intervention. This, however, raises the question of how pain-related fear might best be tackled within treatment.
Pain-Related Fear: An impeding Factor for Treatment?
A working alliance is of importance for positive treatment progress (Horvath and Symonds, 1991; Mead and Bower, 2000), but pain-related fear could hamper the formation of this alliance. Although rather speculative, fearful CLBP patients may be more inclined to keep searching for biomedical explanations and solutions for their pain problem, may have a history with dissatisfactory health care encounters, may strive for pain relief instead of restoration of activities, and they may more frequently have co-morbid disorders (Hadjistavropoulos and Kowalyk, 2004; Kerns et al., 1999). Because of these features, frustration may be triggered in both the patient and the therapist, thereby negatively affecting the therapeutic relationship (Hadjistavropoulos and Kowalyk, 2004). More research is required to investigate whether pain-related fear actually impedes the patient-therapist relationship.
Patients’ pain-related fear may be fed by the interaction with health care providers. It might be possible that not only the health care providers’ facial expressions, but also the threatening diagnostic labels they use (e.g. back injury, ruptured disc, degenerative changes) may activate the fear network (Boston and Sharpe, 2005). Because of the use of diagnostic terms that may be interpreted by patients as evidence for serious pathology, health care providers may inadvertently increase the threat value of pain. Additionally, health care providers may also hold fear avoidance beliefs themselves, although fortunately the beliefs of health care providers generally appear to be in accordance with current guidelines (Koes et al., 2001), advising the continuation of normal activities including work even when in pain, and discouraging sick leave (Linton et al., 2002b). However, fear avoidance beliefs were found to some degree in health care providers. For example, many would advise patients to avoid painful movements, some believed that sick leave is an adequate treatment, and some worried when their patients were in pain during exercise (Linton et al., 2002b). Most interestingly, these beliefs were related to treatment recommendations. The more strongly therapists held fear avoidance beliefs (Houben et al., 2004; Poiraudeau et al., 2006; Rainville et al., 2000), and the stronger the biomedical orientation of therapists (Houben et al., 2005b), the more it was recommended that CLBP patients should restrict work and physical activities. In addition to the detrimental consequences of inadequate advice, these fear avoidance beliefs of health care providers can induce or strengthen those of their patients, especially in fearful CLBP patients who are likely to be sensitive even to minor hesitations or inconsistencies.
It is not clear whether fearful CLBP patients can benefit optimally from traditional health care. Fearful CLBP patients may sustain their avoidance behaviors regardless of the treatment message, when the disadvantageous consequences of avoidance behavior are neither explicitly addressed, nor managed. In traditional health care, and especially in health care providers with a more biomedical orientation, the message that activity is beneficial is often accompanied by a note of caution especially if the pain increases. It is not surprising then, that fearful CLBP patients may respond with more safety and avoidance behaviors to these treatments than those who are less fearful, thereby gaining less benefit from regular treatments. One study indeed suggested that fear avoidance beliefs counteracted the beneficial effects of an exercise-based therapy (Al-Obaidi et al., 2005), and another indicated that pain catastrophizing hampered the efficacy of usual practitioner care (Jellema et al., 2006). On the contrary, it has been shown that especially for high fear avoiders a regular exercise program was more effective than usual general practitioner care (Klaber Moffett et al., 2004), whereas lower fear avoidance beliefs were associated with less favorable outcomes following a stabilization exercise program (Hicks et al., 2005). One of the questions, of course, is how these treatments have been delivered, and whether pain-related fear and the associated safety behaviors were adequately addressed.
Effectiveness of Cognitive Behavioral Programs
Some recently reported cognitive behavioral treatments have included methods to address pain-related fear. These programs have demonstrated promising results thus far, indicating that it can be beneficial to focus on decreasing pain-related fear. In line with the idea of matching treatments to specific patient characteristics (Vlaeyen and Morley, 2005), it was demonstrated that usual general practitioner care was less suitable in cases of high pain catastrophizing, whereas a minimal intervention focusing on risk factors for chronicity appeared to be more appropriate in the case of elevated fear avoidance beliefs (Jellema et al., 2006). Another study showed a fear avoidance based treatment, consisting of education about fear and avoidance in addition to graded exercise, to be successful in reducing disability as compared to usual care in acute LBP patients high in fear avoidance beliefs, but to be counterproductive for those low in these beliefs (George et al., 2003). It might therefore be that the presence of fear avoidance beliefs may debilitate outcome when usual treatment is applied, whereas fear-avoidance based treatments fail to be effective in the absence of pain-related fear.
Several cognitive behavioral programs, comprising various treatment techniques directed at changing cognitions and improving behavioral participation in activities, have currently been developed (Guzman et al., 2001; Morley et al., 1999; van Tulder et al., 2000). These studies have shown that the effectiveness of these programs in reducing disability was associated with decreases in pain catastrophizing (Burns et al., 2003; Smeets et al., 2006b; Spinhoven et al., 2004; Sullivan and Stanish, 2003; Sullivan et al., 2005b) and pain-related fear (Jensen et al., 2001; Klaber Moffett et al., 2004; Mannion et al., 2001; McCracken et al., 2002; Sullivan and Stanish, 2003; Woby et al., 2004b). For example, it was demonstrated that a short cognitive behavioral intervention was successful in reducing fear avoidance beliefs, together with diminishing the risk of pain continuation, over and above the rather strong natural recovery rate for acute LBP (Linton and Ryberg, 2001). The association between pain-related fear and the effectiveness of treatments is also highlighted by brief educational sessions. As was previously demonstrated (Burton et al., 1999; Moore et al., 2000; Symonds et al., 1995), a straightforward educational campaign comprised of the advice to stay active and discouraging medical interventions, resulted in long-lasting reductions in fear avoidance beliefs in the community as well as in physicians, and in less workers compensation claims for LBP (Buchbinder et al., 2001; Buchbinder and Jolley, 2005). Taken together, these results suggest that cognitive behavioral programs, and even brief educational sessions, can effectively diminish disability, which might be due to reducing fear avoidance beliefs and pain catastrophizing.
Pain-related fear might therefore be an essential target for successful interventions. Yet, the above-mentioned treatments were not developed to specifically and systematically address pain-related fear. It can be suggested that methodically addressing and diminishing fear might be even more powerful. Exposure in vivo, which is a comprehensible example of an idiosyncratic treatment designed only for those with elevated levels of pain-related fear, may therefore be the most suitable treatment to achieve the most significant reduction of pain-related fear and associated disability.
Exposure in vivo
Following the suggestions of Philips (1987), exposure in vivo treatment was developed to gradually confront patients with activities they feared and avoided for a long time due to the belief that these might be damaging for the back. This treatment consists of four components: the choice of functional goals, education about the paradoxical effects of safety behaviors, the establishment of a fear hierarchy, and graded exposure to feared activities in the form of behavioral experiments. Due to gradual and repeated encounters with these feared activities, this treatment may provide patients with the most convincing evidence that expected detrimental consequences of these feared activities are in fact a catastrophic overestimation. Due to this, their fear may diminish and functional abilities might be promoted. A detailed description of exposure in vivo is provided elsewhere (Vlaeyen et al., 2004a).
For the establishment of the fear hierarchy of activities, that constitutes the foundation for the rest of the therapy, The Photograph Series of Daily Activities (PHODA: Kugler et al., 1999) may be the most suitable instrument. It is comprised of photographs of various daily activities, of which patients have to indicate to what extent they think that these can be harmful to the back. The PHODA provides therapists with a tangible tool that specifically assesses the patients’ beliefs about the harmfulness of certain activities for the back. Besides clinical purposes, the PHODA has also been utilized as a measurement tool, and has been shown to have excellent psychometric properties (Leeuw et al., submitted).
Several experimental single case studies, including 2 to 6 patients each, have demonstrated the effectiveness of exposure in vivo as compared to graded activity in fearful CLBP patients, by reporting impressive reductions in pain-related fear and disability, as well as increases in activity levels in the home situation (Boersma et al., 2004; de Jong et al., 2005b; Linton et al., 2002a; Vlaeyen et al., 2001, 2002a,b). Although the size of these improvements was less substantial for the Swedish research group (Boersma et al., 2004; Linton et al., 2002a), it does provide support for extending generalization of exposure in vivo treatment across settings and therapists. Interestingly, the educational part also produced improvements in self-reported pain-related fear and catastrophizing, although these improvements gained strength after subsequent exposure in vivo. Measures of actual behavior, including accelerometer data, and self-reported ability to perform pre-defined goals, improved after the exposure sessions and not after the educational session (de Jong et al., 2005b). Finally, the resumption of daily activities in patients suffering from complex regional pain syndrome was associated with decreases in pain-related fear, but not with a reduction in pain-intensity, which occurred only later in time (de Jong et al., 2005a). A randomized controlled trial comparing usual graded activity with exposure in vivo in fearful patients, currently performed by the first author et al., will provide additional information on the external validity and long-term cost-effectiveness.
Generalization of Exposure in vivo
An important assumption behind exposure in vivo is that the repeated experiences of being able to perform various activities without pain increases or inducing (re)injury to the back during treatment will extend to activities during daily life. However, in line with findings from experimental fear research (e.g Bouton, 2002), several experimental studies suggest that generalization of these corrective encounters is rather limited in chronic pain patients. In patients high in pain catastrophizing, exposure to a particular movement (Goubert et al., 2002; Crombez et al., 2002b), and even to a variety of movements (Goubert et al., 2005b), resulted in subsequent diminished overprediction of pain for those particular movements, but this effect failed to generalize to other dissimilar movements. It might be that these patients learn an exception to the rule ‘activities hurt’ rather than to change their general beliefs regarding the detrimental consequences of activities. Interestingly, these patients on the other hand tended to overgeneralize pain, such that once a certain movement had been painful it was assumed that it would remain painful in the future (Goubert et al., 2005a). For exposure in vivo treatment, it would be interesting to investigate whether the overprediction of injury is as difficult to generalize to dissimilar movements as the overprediction of pain.
Translated into treatment implications, these results emphasize the importance of practicing a wide variety of activities and movements, not only during treatment, but also in the home environment of the patient (Rowe and Craske, 1998a,b). Adding cognitive techniques, such as in behavioral experiments, might also be valuable because of explicitly challenging and correcting erroneous expectations. Although there is no data as yet comparing exposure in vivo to behavioral experiments, it can be suggested that the addition of behavioral experiments may optimize generalization of corrective encounters.
CONCLUSION AND UNEXPLORED ISSUES
Summarizing, it can be stated that there is accumulating support for the fear-avoidance model. As predicted from the vast literature on fear and anxiety, pain-related fear is associated with catastrophic (mis)interpretations of pain, hypervigilance, increased escape and avoidance behaviors, as well as with intensified pain intensity and functional disability. Disrupted attentional processes, and especially impeded attentional disengagement in the case of threatening stimuli, were found in fearful CLBP patients, as well as avoidance behavior as reflected in submaximal physical task performance. There is less evidence for the existence of disuse in CLBP patients. Studies on aerobic fitness level, which seems the most appropriate measure of physical deconditioning, have demonstrated inconsistent findings thus far. Therefore, more research is required to establish whether CLBP patients actually have lower physical activity levels and experience associated physical consequences. Perhaps the disordered motor coordination is a more salient aspect of disuse than reduced fitness. Furthermore, evidence is accumulating that pain severity plays a more important role in disability than previously assumed. Finally, several personal vulnerabilities, such as fundamental fears or neuroticism, may influence whether someone will respond fearfully to a painful experience.
Pain-related fear may augment the vulnerability to develop new LBP episodes in currently pain-free people, may increase the risk for the continuation of LBP complaints, and may maintain complaints when they have become chronic. Some prudence is required though, since it is not straightforward that once patients respond with pain-related fear to pain, they will inevitably become mired in a vicious circle leading to the development and maintenance of enduring pain. This conception disregards the erratic and recurrent course of LBP for most people. For example, the number and duration of episodes, fluctuations in pain intensity, level of disability, occupational consequences, and health care use can vary considerably between people suffering from LBP. These individual differences in the course and consequences of LBP should be kept in mind when interpreting the contribution of pain-related fear during different stages of pain. In fact, the research on contextual factors influencing the occurrence and reinstatement of fear waits to be extended to the area of pain.
It is also important to note that the fear-avoidance model only accounts for the development and maintenance of problems in a subgroup of CLBP patients. Various other factors besides pain-related fear may determine the progress of LBP. Furthermore, supportive evidence for the interrelations between the separate constructs of the fear-avoidance model does not provide evidence for causal interrelationships. Causality can only be established when each construct is experimentally manipulated. It would be highly interesting to investigate the progression of interrelationships between the variables of the fear-avoidance model in a large cohort of acute back pain patients of whom some will develop subsequent chronic pain, for example by using Latent Trajectory Classes Analyses. Additionally, exploring the effects of treatments by manipulating the individual constructs in the fear-avoidance model would shed light on the actual causal contributions. Until now, a large number of cross-sectional and prospective studies at least point to the potential validity of the fear-avoidance model. For the future, a number of interesting issues remain that require further exploration. Some of these will be highlighted below.
Pain-Related fear: When is it Adaptive and when Dysfunctional?
Due to their protective and defensive function in the case of impending or immediate danger, it may be concluded that fear and anxiety are adaptive mechanisms for an individual, and in most cases they are indeed. But when do they become dysfunctional? This is a complex issue as we lack objective measures of what is adaptive. One way to approach this question is to consider contextual issues, e.g. the presence or absence of real harm, and the consequences of fear on function and identity. In acute stages of pain, when the pain is the result of an acute injury, pain-related fear is likely to be adaptive as it will direct attention towards the injury, thereby enhancing the probability of necessary care, e.g. by withdrawal from usual activities so that healing process is facilitated (Wall, 1979). However, in the case of enduring pain, when the pain may no longer be explained by injury, fear can become dysfunctional. The persevering use of avoidance and escape behaviors in this chronic stage may be the result of misdirected problem-solving, in which patients keep seeking to solve their insoluble problem of pain release (Aldrich et al., 2000). However, in the case of chronic pain, these behaviors prevent the individual from disconfirming the level of threat. In addition, hypervigilance and avoidance behavior will interrupt cognitive activity, interfere with daily tasks, and threaten major life goals and personal identity (Morley and Eccleston, 2004). Thus, one could assert that fear, and pain-related fear in particular, is never dysfunctional, but it is the prolonged engagement in these safety behaviors that are dysfunctional.
When to Target Pain-Related Fear?
Most treatments are developed for chronic pain patients, thereby disregarding earlier phases during which the development of CLBP can be tackled. A promising area lies in preventing dysfunctional reactions when a new pain episode is initiated. Since misconceptions about LBP and its management seem very common in the general population in addition to some health care providers, these provide an ultimate opportunity for prevention. Educational campaigns have proved their value in adaptively changing LBP beliefs and associated benefits (Buchbinder and Jolley, 2005; Burton et al., 1999; Moore et al., 2000; Symonds et al., 1995). Although it can be questioned whether changing fear avoidance beliefs will lead to actual behavior change (de Jong et al., 2005b), the potential beneficial effects of educational campaigns should be more extensively explored.
Another challenge lies in the prevention of the development of enduring pain once an acute LBP episode is established. An important example of this is the development (Linton and Hallden, 1998) of the Örebro Musculoskeletal Pain Screening Questionnaire, which identifies several psychological ‘yellow flags’ which signal a heightened risk for chronification of complaints (Boersma and Linton, 2005b; Linton and Boersma, 2003). In addition to identification of those at risk, prevention strategies should be developed that target these risk factors, thereby putting detrimental developmental processes in pain on hold (Linton and Andersson, 2000; Linton and Ryberg, 2001, Linton et al., 2005; Linton and Nordin, 2006).
Pain-Related fear in Patients with Specific Pain Diagnoses
So far, most of the work on pain-related fear has focused on patients with non-specific medical diagnoses such as back pain, chronic headache (Nash et al., 2006; Norton and Asmundson, 2004), fibromyalgia (de Gier et al., 2003; Turk et al., 2004), whiplash disorder (Nederhand et al., 2004; Sterling et al., 2003), and chronic fatigue syndrome (Nijs et al., 2004; Silver et al., 2002). Theoretically, however, there is every reason to believe that fear processes would be applicable to specific pain problems as well. Indeed, the contribution of pain-related fear has been shown to extend to patients with osteoarthritis (Heuts et al., 2004), burn pain (Sgroi et al., 2005), knee injury (Kvist et al., 2005) and neuropathic pain (de Jong et al., 2005a). It will be a challenge for future researchers to integrate fear reduction techniques in medical treatment and care for these patient groups.
The Object of Fear
Fear of pain and associated avoidance behaviors may not be the only kind of fear associated with chronic pain. Given the debilitating consequences of longstanding avoidance behaviors, patients may present with multiple fears and concerns, including the inability to work (functional), having surgery (health), having to sell the house (financial) and being a burden to family members (social; Davies, 2003). For chronic pain patients, another important concern may be social isolation that occurs in response to their diminished participation in daily life. Recently, it was shown that sensitivity to pain and sensitivity for social rejection were mutually reinforcing (Eisenbergera et al., in press). It therefore may be that concerns about social isolation in pain patients inadvertently increase their pain threshold.
Morley and Eccleston (2004) proposed to broaden the fear-avoidance model to those areas that pose a possible threat to an individual's identity, using Carver and Scheier's goal-oriented model of self-regulation (Carver and Scheier, 1998). Following this theory, a distinction is made between approach and avoidance goals. Approach goals are those that the individual is hoping for, whereas avoidance goals consist of situations that have a negative value. Fear is regarded as the emotional reaction to a movement towards an avoidance goal. As chronic pain is associated with moving towards many avoidance goals, e.g. being dependent upon others, it may therefore induce fear. Although this theoretical framework appears a promising avenue for broadening current fear-avoidance models, research efforts have just started. For example, Karoly and Ruehlman (1996) showed that in chronic pain patients, goal conflicts predicted anxiety levels over and above pain-related variables.
Task Persistence Instead of Avoidance
As mentioned before, fear is not always associated with avoidance behavior. Rachman (2004) eloquently describes situations in which fearful individuals are willing to approach a frightening object or situation. In some cases, fear may even be associated with persistence rather than avoidance. For example, both LBP patients who were requested to perform a lifting task (van den Hout et al., 2001b), and healthy controls who were requested to immerse their hand in cold water (Severeijns et al., 2005) with the instruction “as long as possible” demonstrated better performance after an experimentally induced negative mood as compared to those in positive mood. One possible account for these findings is the so-called mood-as-input model, which predicts that task performance is the result of the interaction between mood and certain stop-rules. When individuals adopt an explicit or implicit “As-Many-As-Can” stop rule (they continue until satisfaction is reached about dealing with the task), negative mood will facilitate task performance, whereas positive mood will inhibit task performance. The strength of the mood-as-input model is that it provides specific predictions, including those that are based on the fear-avoidance model, but also those that are based on a novel theoretical basis that may account for findings inconsistent with the fear-avoidance model, such as task perseverance instead of avoidance despite pain-related fear. The validity of this model in the domain of pain, however, awaits further investigation (Vlaeyen and Morley, 2004).
References
Aldrich, S., Eccleston, C., and Crombez, G. (2000). Worrying about chronic pain: vigilance to threat and misdirected problem solving. Behav. Res. Ther. 38: 457–470.
Al-Obaidi, S. M., Al-Zoabi, B., Al-Shuwaie, N., Al-Zaabie, N., and Nelson, R. M. (2003). The influence of pain and pain-related fear and disability beliefs on walking velocity in chronic low back pain. Internat. J. Rehabil. Res. 26: 101–108.
Al-Obaidi, S. M., Beattie, P., Al-Zoabi, B., and Al-Wekeel, S. (2005). The relationship of anticipated pain and fear avoidance beliefs to outcome in patients with chronic low back pain who are not receiving workers' compensation. Spine 30: 1051–1057.
Al-Obaidi, S. M., Nelson, R. M., Al-Awadhi, S., and Al-Shuwaie, N. (2000). The role of anticipation and fear of pain in the persistence of avoidance behavior in patients with chronic low back pain. Spine 25: 1126–1131.
Arntz, A., and Claassens, L. (2004). The meaning of pain influences its experienced intensity. Pain 109: 20–25.
Arntz, A., Dreessen, L., and De Jong P. (1994). The influence of anxiety on pain: Attentional and attributional mediators. Pain 56: 307–314.
Asmundson, G. J., Norton, P. J., and Vlaeyen, J. W. S. (2004). Fear-avoidance models of chronic pain: An overview. In: G. J. Asmundson, J. W. S. Vlaeyen, and G. Crombez (Eds.), Understanding and treating fear of pain, Oxford University Press, Oxford, pp. 3–24.
Asmundson, G. J., Wright, K. D., and Hadjistavropoulos, H. D. (2000). Anxiety sensitivity and disabling chronic health conditions: state of the art and future directions. Scand. J. Behav. Ther. 29: 100–117.
Asmundson, G. J. G. Norton, P. J., and Norton, G. R. (1999). Beyond pain: The role of fear and avoidance in chronicity. 19: 97–119.
Asmundson, G. J. G., Wright, K. D., and Hadjistavropoulos, H. D. (2005). Hypervigilance and attentional fixedness in chronic musculoskeletal pain: consistency of findings across modified stroop and dot-probe tasks. J. Pain 6: 497–506.
Boersma, K., and Linton, S. J. (2005a). How does persistent pain develop? An analysis of the relationship between psychological variables, pain and function across stages of chronicity. Behav. Res. Ther. 43: 1495–1507.
Boersma, K., and Linton, S. J. (2005b). Screening to identify patients at risk: profiles of psychological risk factors for early intervention. Clin. J. Pain 21: 38–43.
Boersma, K., Linton, S. J., Overmeer, T., Jansson, M., Vlaeyen, J. W. S., and de Jong, J. (2004). Lowering fear-avoidance and enhancing function through exposure in vivo; A multiple baseline study across six patients with back pain. Pain 108: 8–16.
Boston, A., and Sharpe, L. (2005). The role of threat-expectancy in acute pain: effects on attentional bias, coping strategy effectiveness and response to pain. Pain 119: 168–175.
Bouton, M. E. (2002). Context, ambiguity, and unlearning: sources of relapse after behavioral extinction. Biol. Psychiat. 52: 976–986.
Brox, J. I., Storheim, K., Holm, I., Friis, A., and Reikeras, O. (2005). Disability, pain, psychological factors and physical performance in healthy controls, patients with sub-acute and chronic low back pain: a case-control study. J. Rehabil. Med. 37: 95–99.
Buchbinder, R., and Jolley, D. (2005). Effects of a media campaign on back beliefs is sustained 3 years after its cessation. Spine 30: 1323–1330.
Buchbinder, R., Jolley, D., and Wyatt, M. (2001). Volvo award winner in clinical studies: effects of a media campaign on back pain beliefs and its potential influence on management of low back pain in general practice. Spine 26: 2535–2542.
Buer, N., and Linton, S. J. (2002). Fear-avoidance beliefs and catastrophizing: occurrence and risk factor in back pain and ADL in the general population. Pain 99: 485–491.
Burns, J. W., Kubilus, A., Bruehl, S., Harden, R. N., and Lofland, K. (2003). Do changes in cognitive factors influence outcome following multidisciplinary treatment for chronic pain? A cross-lagged panel analysis. J. Consult. Clin. Psychol. 71: 81–91.
Burton, A. K., McClune, T. D., Clarke, R. D., and Main, C. J. (2004). Long-term follow-up of patients with low back pain attending for manipulative care: outcomes and predictors. Manual Therapy 9: 30–35.
Burton, A. K., Waddell, G., Tillotson, K. M., and Summerton, N. (1999). Information and advice to patients with back pain can have a positive affect. Spine 24: 2484–2491.
Cannon, W. B. (1929). Bodily changes in pain, hunger, fear and rage: an account of recent researches into the functions of emotional excitement. Appleton-Century-Crofts, New York.
Carver, C. S., and Scheier, M. F. (1998). On the self-regulation of behavior, Cambridge University Press, Cambridge.
Cook, A. J., Brawer, P. A., and Vowles, K. E. (2006). The fear-avoidance model of chronic pain: Validation and age analysis using structural equation modeling. Pain 121: 195–206.
Crombez, G., Eccleston, C., Baeyens, F., and Eelen, P. (1998). When somatic information threatens, catastrophic thinking enhances attentional interference. Pain 75: 187–198.
Crombez, G., Eccleston, C., Baeyens, F., Van Houdenhove, B., and Van Den Broeck, A. (1999a). Attention to chronic pain is dependent upon pain-related fear. J. Psychosom. Res. 47: 403–410.
Crombez, G., Eccleston, C., Van Den Broeck, A., Van Houdenhove, B., and Goubert, L. (2002a). The effects of catastrophic thinking about pain on attentional interference by pain: no mediation of negative affectivity in healthy volunteers and in patients with low back pain. Pain Res. Manag. 7: 31–39.
Crombez, G., Van Damme, S., and Eccleston, C. (2005). Hypervigilance to pain: an experimental and clinical analysis. Pain 116: 4–7.
Crombez, G., Vlaeyen, J. W., Heuts, P. H., and Lysens, R. (1999b). Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain 80: 329–339.
Crombez, G., Vlaeyen, J. W. S., Eccleston, C., Vansteenwegen, D., Lysens, R., and Eelen, P. (2002b). Exposure to physical movements in low back pain patients: restricted effects of generalization. Health Psychol. 21: 573–578.
Davies, C. (2003). Self-discrepancy Theory and Chronic Pain. University of Leeds, Leeds.
de Gier, M., Peters, M. L., and Vlaeyen, J. W. S. (2003). Fear of pain, physical performance, and attentional processes in patients with fibromyalgia. Pain 104: 121–130.
de Jong, J. R., Vlaeyen, J. W. S., Onghena, P., Cuypers, C., den Hollander, M., and Ruijgrok, J. (2005a). Reduction of pain-related fear in complex regional pain syndrome type I: the application of graded exposure in vivo. Pain 116: 264–275.
de Jong, J. R., Vlaeyen, J. W. S., Onghena, P., Goossens, M. J. E. B., Geilen, M., and Mulder, H. (2005b). Fear of movement/(re)injury in chronic low back pain: education of exposure in vivo as mediator to fear reduction? Clin J Pain 21: 9–17.
Dehghani, M., Sharpe, L., and Nicholas, M. K. (2004). Modification of attentional biases in chronic pain patients: a preliminary study. European J. Pain 8: 585–594.
Denison, E., Asenlof, P., and Lindberg, P. (2004). Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain 111: 245–252.
Eccleston, C., and Crombez, G. (1999). Pain demands attention: A cognitive-affective model of the interruptive function of pain. 125: 356–366.
Eccleston, C., Crombez, G., Aldrich, S., and Stannard, C. (1997). Attention and somatic awareness in chronic pain. Pain 72: 209–215.
Edwards, R. R., Fillingim, R. B., Maixner, W., Sigurdsson, A, and Haythornthwaite, J. (2004). Catastrophizing predicts changes in thermal pain responses after resolution of acute dental pain. J. Pain. 5: 164–170.
Eisenbergera, N. I., Jarchob, J. M., Lieberman, M. D., and Naliboff, B. D. (in press). An experimental study of shared sensitivity to physical pain and social rejection. Pain xx: xx–xx.
Ellis, A. (1962). Reason and emotion in psychotherapy. Lyle-Stuart, New York.
Eysenck, M. W. (1992). Anxiety: the cognitive perspective. Erlbaum, Hove.
Fritz, J. M., George, S. Z., and Delitto, A. (2001). The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain 94: 7–15.
Geisser, M. E., Haig, A. J., and Theisen, M. E. (2000). Activity avoidance and function in persons with chronic back pain. J. Occup. Rehabil. 10: 215–227.
Geisser, M. E., Haig, A. J., Wallbom, A. S., and Wiggert, E. A. (2004). Pain-related fear, lumbar flexion, and dynamic EMG among persons with chronic musculoskeletal low back pain. Clin. J. Pain 20: 61–69.
George, S. Z., Bialosky, J. E., and Donald, D. A. (2005). The centralization phenomenon and fear-avoidance beliefs as prognostic factors for acute low back pain: a preliminary investigation involving patients classified for specific exercise. J. Orthop. Sports. Phys. Ther. 35: 580–588.
George, S. Z., Fritz, J. M., Bialosky, J. E., and Donald, D. A. (2003). The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine 28: 2551–2560.
Gheldof, E. L., Vinck, J., Vlaeyen, J. W. S., Hidding, A., and Crombez, G. (2005). The differential role of pain, work characteristics and pain-related fear in explaining back pain and sick leave in occupational settings. Pain 113: 71–81.
Gheldof, E. L. M., Vinck, J., Van Den Bussche, E., Vlaeyen, J. W. S., Hidding, A., and Crombez, G. (2006). Pain and pain-related fear are associated with functional and social disability in an occupational setting: Evidence of mediation by pain-related fear. European J. Pain 10: 513–525.
Goubert, L., Crombez, G., and Danneels, L. (2005a). The reluctance to generalize corrective experiences in chronic low back pain patients: a questionnaire study of dysfunctional cognitions. Behav. Res. Ther. 43: 1055–1067.
Goubert, L., Crombez, G., and De bourdeaudhuij, I. (2004a). Low back pain, disability and back pain myths in a community sample: prevalence and interrelationships. European J. Pain 8: 385–394.
Goubert, L., Crombez, G., and Lysens, R. (2005b). Effects of varied-stimulus exposure on overpredictions of pain and behavioural performance in low back pain patients. Behav. Res. Ther. 43: 1347–1361.
Goubert, L., Crombez, G., and Van Damme, S. (2004b). The role of neuroticism, pain catastrophizing and pain-related fear in vigilance to pain: a structural equations approach. Pain 107: 234–241.
Goubert, L., Francken, G., Crombez, G., Vansteenwegen, D., and Lysens, R. (2002). Exposure to physical movement in chronic back pain patients: No evidence for generalization across different movements. Behav. Res. Ther. 40: 415–429.
Granot, M., and Ferber, S. G. (2005). The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin. J. Pain. 21: 439–445.
Grotle, M., Vollestad, N. K., Veierod, M. B., and Brox, J. I. (2004). Fear-avoidance beliefs and distress in relation to disability in acute and chronic low back pain. Pain 112: 343–352.
Guzman, J., Esmail, R., Karjalainen, K., Malmivaara, A., Irvin, E., and Bombardier, C. (2001). Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ 322: 1511–1516.
Hadjistavropoulos, H. D., and Kowalyk, K. M. (2004). Patient-therapist relationships among patients with pain-related fear. In: G. J. G. Asmundson, J. W. S. Vlaeyen and G. Combez (Eds.), Understanding and treating fear of pain. Oxford University Press, New York.
Hanley, M. A., Jensen, M. P., Ehde, D. M., Hoffman, A. J., Patterson, D. R., and Robinson, L. R. (2004). Psychosocial predictors of long-term adjustment to lower-limb amputation and phantom limb pain. Disabil. Rehabil. 26: 882–893.
Haythornthwaite, J. A., Clark, M. R., Pappagallo, M., and Raja, S. N. (2003). Pain coping strategies play a role in the persistence of pain in post-herpetic neuralgia. Pain 106: 453–460.
Hermans, D., Craske, M. G., Mineka, S., and Lovibond, P. F. (2006). Extinction in human fear conditioning. Biol. Psychiatry. 30: 361–368.
Heuts, P. H. T. G., Vlaeyen, J. W. S., Roelofs, J., de Bie, R. A., Aretz, K., van Weel, C., and van Schayck, O. C. (2004). Pain-related fear and daily functioning in patients with osteoarthritis. Pain 110: 228–235.
Hicks, G. E., Fritz, J. M., Delitto, A., and McGill, S. M. (2005). Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch. Phy. Med.Rehabil. 86: 1753–1762.
Horvath, A. O., and Symonds, B. D. (1991). Relation between working alliance and outcome in psychotherapy: A meta-analysis. J. Counsel. Psychol. 38: 139–149.
Houben, R. M. A., Leeuw, M., Vlaeyen, J. W. S., Goubert, L., and Picavet, H. S. J. (2005a). Fear of movement/injury in the general population: Factor structure and psychometric properties of an adapted version of the Tampa Scale for Kinesiophobia. J. B. Med. 28: 415–424.
Houben, R. M. A., Ostelo, R. W. J. G., Vlaeyen, J. W. S., Wolters, P. M. J. C., Peters, M., and Stomp-van den Berg, S. G. M. (2005b). Health care providers' orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. European J. Pain 9: 173–183.
Houben, R. M. A., Vlaeyen, J. W. S., Peters, M., Ostelo, R. W. J. G., Wolters, P. M. J. C., and Stomp-van den Berg, S. G. M. (2004). Health care providers' attitudes and beliefs towards common low back pain: factor structure and psychometric properties of the HC-PAIRS. Clin. J. Pain 20: 37–44.
Jellema, P., Van Der Horst, H. E., Vlaeyen, J. W. S., Stalman, W. A. B., Bouter, L. M., and Van Der Windt D. A. W. M. (2006). Predictors of outcome in patients with (sub)acute low back pain differ across treatment groups. Spine 31: 1699–1705.
Jensen, M. P., Turner, J. A., and Romano, J. M. (2001). Changes in beliefs, catastrophizing, and coping are associated with improvement in multidisciplinary pain treatment. J. Consult. Clin. Psychol. 69: 655–662.
Kanfer, F. H., and Philips, J. S. (1970). Learning foundations of behaviour therapy. Wiley, New York.
Karoly, P., and Ruehlman, L. S. (1996). Motivational implications of pain: chronicity, psychological distress, and work goal construal in a national sample of adults. Health Psychol. 15: 383–390.
Keogh, E., and Asmundson, G. J. G. (2004). Negative affectivity, catastrophizing, and anxiety sensitivity. In: G. J. G. Asmundson, J. W. S. Vlaeyen and G. Crombez (Eds.), Understanding and treating fear of pain. Oxford University Press, Oxford, pp. 91–116.
Keogh, E., Ellery, D., Hunt, C., and Hannent, I. (2001). Selective attentional bias for pain-related stimuli amongst pain fearful individuals. Pain 91: 91–100.
Kerns, R. D., Bayer, L. A., and Findley, J. C. (1999). Motivation and adherence in the management of chronic pain. In: A. R. Block, E. Fernandez and E. F. Kremer (Eds.), Handbook of Pain Syndromes: Biopsychosocial Perspectives. Lawrence Erlbaum Associates, Mahwah, NJ, pp. 99–121.
Klaber Moffett, J. A., Carr, J., and Howarth, E. H. (2004). High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine 29: 1167–1179.
Koes, B. W., van Tulder, M. W., Ostelo, R., Kim Burton, A., and Waddell, G. (2001). Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine 26: 2504–2513.
Kramer, M., Ebert, V., Kinzl, L., Dehner, C., Elbel, M., and Hartwig, E. (2005). Surface electromyography of the paravertebral muscles in patients with chronic low back pain. Arch. Phys. Med. Rehabil. 86: 31–36.
Kugler, K., Wijn, J., Geilen, M., de Jong, J., and Vlaeyen, J. W. S. (1999). The Photograph series of Daily Activities (PHODA). CD-rom version 1.0., Institute for Rehabilitation Research and School for Physiotherapy Heerlen, The Netherlands.
Kvist, J., Ek, A., Sporrstedt, K., and Good, L. (2005). Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol. Arthrosc. 13: 393–397.
Lamoth, C. J., Daffertshofer, A., Meijer, O. G., Lorimer Moseley, G., Wuisman, P. I., and Beek, P. J. (2004). Effects of experimentally induced pain and fear of pain on trunk coordination and back muscle activity during walking. Clin. Biomech. (Bristol, Avon) 19: 551–563.
Lang, P. J. (1979). A bio-informational theory of emotional imagery. Psychophysiology 16: 495–512.
Leeuw, M., Goossens, M. E. J. B., van Breukelen, G. J. P., Boersma, K., and Vlaeyen, J. W. S. (submitted). Measuring perceived harmfulness of physical activities in chronic low back pain patients: the Photograph Series of Daily Activities – Short electronic Version. The Journal of Pain.
Leeuw, M., Houben, R. M. A., Severeijns, R., Picavet, H. S. J., Schouten, E. G. W., & Vlaeyen, J. W. S. (in press). Pain-related fear in low back pain: a prospective study in the general population. European J. Pain.
Lethem, J., Slade, P. D., Troup, J. D., and Bentley, G. (1983). Outline of a fear-avoidance model of exaggerated pain perception: I. Behav. Res. Ther. 21: 401–408.
Lilienfeld, S. O., Jacob, R. G., and Turner, S. M. (1993). Anxiety sensitivity: An examination of theoretical and methodological issues. Adv. Behav. Res. Ther. 15: 147–183.
Linton, S. J. (2000). A review of psychological risk factors in back and neck pain. Spine 25: 1148–1156.
Linton, S. J. (2005). Do psychological factors increase the risk for back pain in the general population in both a cross-sectional and prospective analysis? Pain 9: 355–361.
Linton, S. J., and Andersson, T. (2000). Can chronic disability be prevented? A randomized trial of a cognitive-behavior intervention and two forms of information for patients with spinal pain. Spine 25: 2825–2831.
Linton, S. J., and Boersma, K. (2003). Early identification of patients at risk of developing a persistent back problem: the predictive validity of the Orebro Musculoskeletal Pain Questionnaire. Clin. J. Pain 19: 80–86.
Linton, S. J., Boersma, K., Jansson, M., Svard, L., and Botvalde, M. (2005). The effects of cognitive-behavioral and physical therapy preventive interventions on pain-related sick leave: a randomized controlled trial. Clin. J. Pain 21: 109–119.
Linton, S. J., Buer, N., Vlaeyen, J. W. S., and Hellsing, A.-L. (1999). Are fear-avoidance beliefs related to the inception of an episode of back pain? A prospective study. Psychol. Health 14: 1051–1059.
Linton, S. J., and Hallden, K. (1998). Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin. J. Pain 14: 209–215.
Linton, S. J., and Nordin, E. (2006). A 5-year follow-up evaluation of the health and economic consequences of an early cognitive behavioral intervention for back pain: a randomized, controlled trial. Spine 31: 853–858.
Linton, S. J., Overmeer, T., Janson, M., Vlaeyen, J. W. S., and de Jong, J. R. (2002a). Graded in-vivo exposure treatment for fear-avoidant pain patients with functional disability: A case study. Cogn. Behav. Ther. 31: 49–58.
Linton, S. J., and Ryberg, M. (2001). A cognitive-behavioral group intervention as prevention for persistent neck and back pain in a non-patient population: a randomized controlled trial. Pain 90: xx–xx.
Linton, S. J., Vlaeyen, J. W. S., and Ostelo, R. W. J. G. (2002b). The back pain beliefs of health care providers: are we fear-avoidant? J. Occup. Rehabil. 12: 223–232.
Mannion, A. F., Junge, A., Taimela, S., Muntener, M., Lorenzo, K., and Dvorak, J. (2001). Active therapy for chronic low back pain: part 3. Factors influencing self-rated disability and its change following therapy. Spine 26: 920–929.
McCracken, L. M., Gross, R. T., and Eccleston, C. (2002). Multimethod assessment of treatment process in chronic low back pain: comparison of reported pain-related anxiety with directly measured physical capacity. Behav. Res. Ther. 40: 585–594.
Mead, N., and Bower, P. (2000). Patient-centredness: A conceptual framework and review of the empirical literature. Soc. Sci. Med. 51: 1087–1110.
Mineka, S., and Zinbarg, R. (2006). A contemporary learning theory perspective on the etiology of anxiety disorders: it's not what you thought it was. Am. Psychol. 61: 10–26.
Moore, J. E., BVon Korff, M., Cherkin, D., Saunders, K., and Lorig, K. (2000). A randomized trial of a cognitive-behavioral program for enhancing back pain self care in a primary care setting. Pain 88: 145–153.
Morley, S., and Eccleston, C. (2004). The object of fear in pain. In: G. J. Asmundson, J. W. S. Vlaeyen and G. Crombez (Eds.), Understanding and treating fear of pain. Oxford University Press, Oxford, pp. 163–188.
Morley, S., Eccleston, C., and Williams, A. (1999). Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain 80: 1–13.
Nash, J. M., D. M. W., Nicholson, R., and Trask, P. C. (2006). The contribution of pain-related anxiety to disability from headache. J. Behav. Med. 29: 61–67.
Nederhand, M. J., Ijzerman, M. J., Hermens, H. J., Turk, D. C., and Zilvold, G. (2004). Predictive value of fear avoidance in developing chronic neck pain disability: consequences for clinical decision making. Arch. Phys. Med. Rehabil. 85: 496–501.
Nielens, H., and Plaghki, L. (2001). Cardiorespiratory fitness, physical activity level, and chronic pain: are men more affected than women? Clin. J. Pain 17: 129–137.
Nijs, J., Vanherberghen, K., Duquet, W., and De Meirleir, K. (2004). Chronic fatigue syndrome: lack of association between pain-related fear of movement and exercise capacity and disability. Phys. Ther. 84: 696–705.
Norton, P. J., and Asmundson, G. J. G. (2004). Anxiety sensitivity, fear, and avoidance behavior in headache pain. Pain 111: 218–223.
Pavlin, D. J., Sullivan, M. J., Freund, P. R., and Roesen, K. (2005). Catastrophizing: a risk factor for postsurgical pain. Clin. J. Pain 21: 83–90.
Peters, M. L., Vlaeyen, J. W. S., and Kunnen, A. M. W. (2002). Is pain-related fear a predictor of somatosensory hypervigilance in chronic low back pain patients? 40: 85–103.
Peters, M. L., Vlaeyen, J. W. S., and van Drunen, C. (2000). Do fibromyalgia patients display hypervigilance for innocuous somatosensory stimuli? Application of a body scanning reaction time paradigm. Pain 86: 283–292.
Peters, M. L., Vlaeyen, J. W. S., and Weber, W. E. J. (2005). The joint contribution of physical pathology, pain-related fear and catastrophizing to chronic back pain disability. Pain 113: 45–50.
Pfingsten, M., Leibing, E., Harter, W., Kröner-Herwig, B., Hempel, D., Kronshage, U., and Hildebrandt, J. (2001). Fear-avoidance behavior and anticipation of pain in patients with chronic low back pain: A randomized controlled study. Pain Med. 2: 259–266.
Philips, H. C. (1987). Avoidance behaviour and its role in sustaining chronic pain. Behav. Res. Ther. 25: 273–279.
Picavet, H. S., Vlaeyen, J. W. S., and Schouten, J. S. (2002). Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am. J. Epidemiol. 156: 1028–1034.
Pincus, T., Burton, A. K., Vogel, S., and Field, A. P. (2002). A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back. Spine 27: E109–E120.
Pincus, T., and Morley, S. (2001). Cognitive-processing bias in chronic pain: a review and integration. Psychol. Bull. 127: 599–617.
Poiraudeau, S., Rannou, F., Le Henanff, A., Coudeyre, E., Rozenberg, S., Huas, D., Martineau, C., Jolivet-Landreau, I., Revel, M., and Ravaud, P. (2006). Outcome of subacute low back pain: influence of patients' and rheumatologists' characteristics. Rheumatol.-(Oxford) 45: 718–723.
Rachman, S. (1998). Anxiety. Psychological Press, Hove.
Rachman, S. (2004). Fear and Courage: A Psychological Perspective. Soc. Res. 71: 149–176.
Rachman, S., and Hodgson, R. (1974). Synchrony and desynchrony in fear and avoidance. Behav. Res. Ther. 12: 311–318.
Rainville, J., Carlson, N., Polatin, P., Gatchel, R. J., and Indahl, A. (2000). Exploration of physicians' recommendations for activities in chronic low back pain. Spine 25: 2210–2220.
Reiss, S. (1991). Expectancy theory of fear, anxiety, and panic. Clin. Psychol. Rev. 11: 141–153.
Rode, S, Salkovskis, P. M., and Jack, T. (2001). An experimental study of attention, labelling and memory in people suffering from chronic pain. Pain 94: 193–203.
Roelofs, J., Peters, M. L., Fassaert, T., and Vlaeyen, J. W. S. (2005). The role of fear of movement and injury in selective attentional processing in patients with chronic low back pain: a dot-probe evaluation. J. Pain 6: 294–300.
Roelofs, J., Peters, M. L., Patijn, J., Schouten, E. G. W., and Vlaeyen, J. W. S. (2004). Electronic diary assessment of pain-related fear, attention to pain, and pain intensity in chronic low back pain patients. Pain 112: 335–342.
Rosenstiel, A. K., and Keefe, F. J. (1983). The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain 17: 33–44.
Rowe, M. K., and Craske, M. G. (1998a). Effects of an expanding-spaced vs massed exposure schedule on fear reduction and return of fear. Behav. Res. Ther. 36: 701–717.
Rowe, M. K., and Craske, M. G. (1998b). Effects of varied-stimulus exposure training on fear reduction and return of fear. Behav. Res. Ther. 36: 719–734.
Severeijns, R., Van Den Hout, M. A., and Vlaeyen, J. W. S. (2005). The causal status of pain catastrophizing: an experimental test with healthy participants. European J. Pain 9: 257–265.
Severeijns, R., Vlaeyen, J. W. S., Van Den Hout, M. A., and Picavet, H. S. J. (2004). Pain catastrophizing is associated with health indices in musculoskeletal pain: a cross-sectional study in the dutch community. Health Psychol. 23: 49–57.
Severeijns, R., Vlaeyen, J. W. S., Van Den Hout, M. A., and Weber, W. E. (2001). Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin. J. Pain 17: 165–172.
Sgroi, M. I., Willebrand, M., Ekselius, L., Gerdin, B., and Andersson, G. (2005). Fear-avoidance in recovered burn patients: association with psychological and somatic symptoms. J. Health Psychol. 10: 491–502.
Sieben, J. M., Portegijs, P. J. M., Vlaeyen, J. W. S., and Knottnerus, J. A. (2005a). Pain-related fear at the start of a new low back pain episode. European J. Pain 9: 635–641.
Sieben, J. M., Vlaeyen, J. W. S., Portegeijs, P. J. M., Verbunt, J. A., van Riet-Rutgers, S., Kester, A. D. M., Von Korff, M., Arntz, A., and Knottnerus, J. A. (2005b). A longitudinal study on the predictive validity of the fear-avoidance model in low back pain. Pain 117: 162–170.
Sieben, J. M., Vlaeyen, J. W. S., Tuerlinckx, S., and Portegijs, P. J. (2002). Pain-related fear in acute low back pain: the first two weeks of a new episode. European J. Pain 6: 229–237.
Silver, A., Haeny, M., Vijayadurai, P., Wilks, D., Pattrick, M., and Main, C. J. (2002). The role of fear of physical movement and activity in chronic fatigue syndrome. J. Psychosom. Res. 52: 485–493.
Smeets, R. J., Wittink, H., Hidding, A., and Knottnerus, J. A. (2006a). Do patients with chronic low back pain have a lower level of aerobic fitness than healthy controls?: Are pain, disability, fear of injury, working status, or level of leisure time activity associated with the difference in aerobic fitness level? Spine 31: 90–98.
Smeets, R. J. E. M., Vlaeyen, J. W. S., Kester, A. D. M., and Knottnerus, J. A. (2006b). Reduction of Pain Catastrophizing Mediates the Outcome of Both Physical and Cognitive-Behavioral Treatment in Chronic Low Back Pain. J. Pain 7: 261–271.
Sorbi, M. J., Peters, M. L., Kruise, D. A., Maas, C. J., Kerssens, J. J., Verhaak, P. F., and Bensing, J. M. (2006). Electronic momentary assessment in chronic pain II: psychological pain responses as predictors of pain disability. Clin. J. Pain 22: 67–81.
Spenkelink, C. D., Hutten, M. M., Hermens, H. J., and Greitemann, B. O. (2002). Assessment of activities of daily living with an ambulatory monitoring system: a comparative study in patients with chronic low back pain and nonsymptomatic controls. Clin. Rehabil. 16: 16–26.
Spinhoven, P., ter Kuile, M., Kole-Snijders, A. M. J., Hutten Mansfeld, M., and den Ouden, D. J., J. W. S. V. (2004). Catastrophizing and internal pain control as mediators of outcome in the multidisciplinary treatment of chronic low back pain. European J. Pain 8: 211–219.
Staerkle, R., Mannion, A. F., Elfering, A., Junge, A., Semmer, N. K., Jacobshagen, N., Grob, D., Dvorak, J., and Boos, N. (2004). Longitudinal validation of the fear-avoidance beliefs questionnaire (FABQ) in a Swiss-German sample of low back pain patients. European Spine J. 13: 332–340.
Sterling, M., Kenardy, J., Jull, G., and Vicenzino, B. (2003). The development of psychological changes following whiplash injury. Pain 106: 481–489.
Storheim, K., Brox, J. I., Holm, I., and Bo, K. (2005). Predictors of return to work in patients sick listed for sub-acute low back pain: a 12-month follow-up study. J. Rehabil. Med. 37: xx–xx.
Sullivan, M. J., and Neish, N. (1999). The effects of disclosure on pain during dental hygiene treatment: the moderating role of catastrophizing. Pain 79: 155–163.
Sullivan, M. J., Rodgers, W. M., Wilson, P. M., Bell, G. J., Murray, T. C., and Fraser, S. N. (2002). An experimental investigation of the relation between catastrophizing and activity intolerance. Pain 100: 47–53.
Sullivan, M. J., and Stanish, W. D. (2003). Psychologically based occupational rehabilitation: the Pain-Disability Prevention Program. Clin. J. Pain 19: 97–104.
Sullivan, M. J. L., Bishop, S. R., and Pivik, J. (1995). The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 7: 524–532.
Sullivan, M. J. L., Lynch, M. E., and Clark, A. J. (2005a). Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain 113: 310–315.
Sullivan, M. J. L., Thorn, B., Rodgers, W., and Ward, L. C. (2004). Path model of psychological antecedents to pain experience: experimental and clinical findings. Clin. J. Pain 20: 164–173.
Sullivan, M. J. L., Ward, L. C., Tripp, D., French, D. J., Adams, H., and Stanish, W. D. (2005b). Secondary prevention of work disability: community-based psychosocial intervention for musculoskeletal disorders. J. Occup. Rehabil. 15: 377–392.
Swinkels-Meewisse, I. E., Roelofs, J., Oostendorp, R. A., Verbeek, A. L., and Vlaeyen, J. W. S. (2006a). Acute low back pain: pain-related fear and pain catastrophizing influence physical performance and perceived disability. Pain 120: 36–43.
Swinkels-Meewisse, I. E., Roelofs, J., Verbeek, A. L., Oostendorp, R. A., and Vlaeyen, J. W. S. (2003). Fear of movement/(re)injury, disability and participation in acute low back pain. Pain 105: 371–379.
Swinkels-Meewisse, I. E., Roelofs, J., Verbeek, A. L., Oostendorp, R. A., and Vlaeyen, J. W. S. (2006b). Fear-avoidance beliefs, disability, and participation in workers and non-workers with acute low back pain. Clin. J. Pain 22: 45–54.
Swinkels-Meewisse, I. E. J., Roelofs, J., Schouten, E. G. W., Verbeek, A. L. M., Oostendorp, R. A. B., and Vlaeyen, J. W. S. (2006c). Fear of movement/(re)Injury predicting chronic disabling low back pain: a prospective inception cohort study. Spine 31: 658–664.
Symonds, T. L., Burton, A. K., Tilotson, K. M., and Main, C. J. (1995). Absence resulting from low back trouble can be reduced by psyochosocial intervention at the work place. Spine 20: 2738–2745.
Turk, D. C., Robinson, J. P., and Burwinkle, T. (2004). Prevalence of fear of pain and activity in patients with fibromyalgia syndrome. J. Pain 5: 483–490.
Turner, J. A., Jensen, M. P., and Romano, J. M. (2000). Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? xxxxxxxx 85: 115–125.
Turner, J. A., Jensen, M. P., Warms, C. A., and Cardenas, D. D. (2002). Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain 98: 127–134.
Turner, J. A., Mancl, L., and Aaron, L. A. (2004). Pain-related catastrophizing: a daily process study. Pain 103–111.
Van Damme, S., Crombez, G., and Eccleston, C. (2002). Retarded disengagement from pain cues: the effects of pain catastrophizing and pain expectancy. Pain 100: 111–118.
Van Damme, S., Crombez, G., and Eccleston, C. (2004a). The anticipation of pain modulates spatial attention: evidence for pain-specificity in high-pain catastrophizers. Pain 111: 392–399.
Van Damme, S., Crombez, G., and Eccleston, C. (2004b). Disengagement from pain: the role of catastrophic thinking about pain. Pain 107: 70–76.
Van Damme, S., Crombez, G., Hermans, D., Koster, E. H., and Eccleston, C. (2006). The role of extinction and reinstatement in attentional bias to threat: A conditioning approach. Behav. Res. Ther. 44: 1555–1563.
Van Den Hout, J. H. C., Vlaeyen, J. W. S., Heuts, P. H. T. G., Sillen, W. J. H., and Willen, A. J. E. H. L. (2001a). Functional disability in non-specific low back pain: the role of pain-related fear and problem-solving skills. Int. J. Behav. Med. 8: 149–162.
Van Den Hout, J. H. C., Vlaeyen, J. W. S., Houben, R. M. A., Soeters, A. P. M., and Peters, M. L. (2001b). The effects of failure feedback and pain-related fear on pain report, pain tolerance and pain avoidance in chronic low back pain patients. 92: 247–257.
Van Nieuwenhuyse, A., Somville, P. R., Crombez, G., Burdorf, A., Verbeke, G., Johannik, K., Van den Bergh, O., Masschelein, R., Mairiaux, P., and Moens, G. F. (2006). The role of physical workload and pain related fear in the development of low back pain in young workers: evidence from the BelCoBack Study; results after one year of follow up. Occup. Environ. Med. 63: 45–52.
van Tulder, M. W., Ostelo, R., Vlaeyen, J. W. S., Linton, S. J., Morley, S. J., and Assendelft, W. J. (2000). Behavioral treatment for chronic low back pain: a sustematic review within the framework of the Cochrane Back Review Group. Spine 25: xx–xx.
Vancleef, L. M. G., and Peters, M. L. (2006). Pain catastrophizing, but not injury/illness sensitivity or anxiety sensitivity, anhances attentional interference by pain. J. Pain 7: 23–30.
Vancleef, L. M. G., Peters, M. L., Roelofs, J., and Asmundson, G. J. G. (2006). Do fundamental fears differentially contribute to pain-related fear and pain catastrophizing? An evaluation of the sensitivity index. European J. Pain 10: 527–536.
Verbunt, J. A., Seelen, H. A. M., Vlaeyen, J. W. S., Bousema, E. J., Van Der Heijden, G. J., Heuts, P. H. T. G., and Knottnerus, J. A. (2005). Pain-related factors contributing to muscle inhibition in patients with chronic low back pain: an experimental investigation based on superimposed electrical stimulation. Clin. J. Pain 21: 232–240.
Verbunt, J. A., Seelen, H. A. M., Vlaeyen, J. W. S., van de Heijden, G. J., Heuts, P. H. T. G., Pons, K., and Knottnerus, J. A. (2003a). Disuse and deconditioning in chronic low back pain: concepts and hypotheses on contributing mechanisms. European J. Pain 7: 9–21.
Verbunt, J. A., Seelen, H. A. M., Vlaeyen, J. W. S., Van Der Heijden, G. J., and Knottnerus, J. A. (2003b). Fear of injury and physical deconditioning in patients with chronic low back pain. Arch. Phys. Med. Rehabil. 84: 1227–1232.
Verbunt, J. A., Westerterp, K. R., Van Der Heijden, G. J., Seelen, H. A., Vlaeyen, J. W. S., and Knottnerus, J. A. (2001). Physical activity in daily life in patients with chronic low back pain. Arch. Phys. Med. Rehabil. 82: 726–730.
Vlaeyen, J. W., De Jong, J. R., Onghena, P., Kerckhoffs-Hanssen, M., and Kole-Snijders, A. M. (2002a). Can pain-related fear be reduced? The application of cognitive- behavioural exposure in vivo. Pain Res. Manag. 7: 144–153.
Vlaeyen, J. W. S., de Jong, J., Geilen, M., Heuts, P. H. T. G., and van Breukelen, G. (2001). Graded exposure in vivo in the treatment of pain-related fear: a replicated single-case experimental design in four patients with chronic low back pain. Behaviour Research and Therapy 39: 151–166.
Vlaeyen, J. W. S., de Jong, J., Geilen, M., Heuts, P. H. T. G., and van Breukelen, G. (2002b). The treatment of fear of movement/(re)injury in chronic low back pain: Further evidence on the effectiveness of exposure in vivo. Clinical journal of pain 18: 251–261.
Vlaeyen, J. W. S., de Jong, J., Leeuw, M., and Crombez, G. (2004a). Fear reduction in chronic pain: graded exposure in vivo with behavioral experiments. In: G. J. Asmundson, J. W. S. Vlaeyen and G. Crombez (Eds.), Understanding and Treating Fear of Pain, Oxford University Press, Oxford.
Vlaeyen, J. W. S., Kole Snijders, A. M. J., Boeren, R. G. B., and van Eek, H. (1995). Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. 62: 363–372.
Vlaeyen, J. W. S., and Linton, S. J. (2000). Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 85: 317–332.
Vlaeyen, J. W. S., and Morley, S. (2004). Active despite pain: the putative role of stop-rules and current mood. Pain 110: 512–516.
Vlaeyen, J. W. S., and Morley, S. (2005). Cognitive-behavioral treatments for chronic pain: what works for whom? Clinical Journal of Pain 21: 1–8.
Vlaeyen, J. W. S., Timmermans, C., Rodriguez, L. M., Crombez, G., van Horne, W., Ayers, G. M., Albert, A., and Wellens, H. J. (2004b). Catastrophic thinking about pain increases discomfort during internal atrial cardioversion. Journal of Psychosomatic Research 56: 139–144.
Vowles, K. E., and Gross, R. T. (2003). Work-related beliefs about injury and physical capability for work in individuals with chronic pain. Pain 101: 291–298.
Waddell, G. (2004a). The biopsychosocial model. In: G. Waddel (Ed.), The Back Pain Revolution. Churchill Livingston, Edinburgh, pp. 265–282.
Waddell, G. (2004b). The epidemiology of back pain. In: G. Waddell (Ed.), The Back Pain Revolution. Churchill Livingston, Edinburgh, pp. 71–89.
Waddell, G., Newton, M., Henderson, I., Somerville, D., and Main, C. J. (1993). A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 52: 157–168.
Wall, P. D. (1979). On the relation of injury to pain. The John J. Bonica lecture. Pain 6: 253–264.
Wittink, H., Hoskins Michel, T., Wagner, A., Sukiennik, A., and Rogers, W. (2000). Deconditioning in patients with chronic low back pain: fact or fiction? Spine 25: 2221–2228.
Wittink, H., Michel, T. H., Sukiennik, A., Gascon, C., and Rogers, W. (2002). The association of pain with aerobic fitness in patients with chronic low back pain. Arch. Phys. Med. Rehabil. 83: 1467–1471.
Woby, S. R., Watson, P. J., Roach, N. K., and Urmston, M. (2004a). Adjustment to chronic low back pain—the relative influence of fear-avoidance beliefs, catastrophizing, and appraisals of control. Behav. Res. Ther. 42: 761–774.
Woby, S. R., Watson, P. J., Roach, N. K., and Urmston, M. (2004b). Are changes in fear-avoidance beliefs, catastrophizing, and appraisals of control, predictive of changes in chronic low back pain and disability? European J. Pain 8: 201–210.
Zvolensky, M. J., Goodie, J. L., McNeil, D. W., Sperry, J. A., and Sorrell, J. T. (2001). Anxiety sensitivity in the prediction of pain-related fear and anxiety in a heterogeneous chronic pain population. 39: 683–696.
ACKNOWLEDGEMENTS
This study was supported by Grant nr. 1436.0002 of the Netherlands Organisation for Health Research and Development (ZonMw).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leeuw, M., Goossens, M.E.J.B., Linton, S.J. et al. The Fear-Avoidance Model of Musculoskeletal Pain: Current State of Scientific Evidence. J Behav Med 30, 77–94 (2007). https://doi.org/10.1007/s10865-006-9085-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-006-9085-0