Abstract
Purpose
To evaluate the effectiveness of arthroscopic debridement (DB), partial (PR), and complete repair (CR) for massive rotator cuff tears (mRCT) in terms of functional and subjective parameters, and repair integrity.
Methods
For this single-centre study, 68 consecutive shoulders with mRCT involving at least three tendons and treated with arthroscopic DB (n = 23), PR (n = 22), and CR (n = 23) were included. All patients (52–81 years) were prospectively assessed before and at a mean of 45 months after surgery using functional and subjective parameters. Preoperative tendon rupture pattern and post-operative repair integrity were assessed by MRI. A coding system describing accurately rotator cuff rupture, treatment, and integrity was established.
Results
All treatment groups improved significantly from pre- to post-operative (P < 0.01), while preoperative parameters, except fatty degeneration, were not significantly different. However, post-operative comparisons revealed similar scores with DB (constant score, CS 65.8 ± 14.7, qDASH 24.1 ± 20.6) and PR (CS 67.5 ± 9.9, P = n.s.; qDASH 20.5 ± 14.4, P = n.s.), while CR were significantly better (CS 80.3 ± 8.9; qDASH 7.0 ± 8.7; P ≤ 0.001). Force couple restoration of PR did not significantly influence outcome. Re-tear rates with CR (29 %) were lower compared to PR (53 %). Intact CR compared to intact PR showed better CS (83.4 ± 7.3 vs. 68.5 ± 10.6, P = 0.009) and qDASH (5.4 ± 8.3 vs. 21.2 ± 9.5, P = 0.006). The vast majority of patients were satisfied with their arthroscopic procedure (DB 87 %; PR 86 %; CR 91 %).
Conclusion
Arthroscopic DB, PR, and CR were effective in treating mRCT involving at least three tendons. Reparability of mRCT was influenced by fatty degeneration of the muscles. However, CR showed the most favourable short-term improvements.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Massive rotator cuff tears (mRCT), clinically defined as tears involving more than two tendons [16] and with a diameter width of at least 5 cm [10], are a challenging pathology to treat. Reparability of mRCT is mainly dependent on muscle atrophy, fatty infiltration, and tendon retraction [18, 27, 34], as well as on surgeon’s experience and skill set; thus, a complete repair cannot always be achieved. Debridement, as an alternative treatment option to repair, was reported to yield fair results [32]. Although the repair of mRCT was formerly mainly performed as an open procedure [16], with the evolution of arthroscopy and its releasing techniques, satisfactory outcomes have also been reported with arthroscopic mRCT repair [5, 8, 21]. However, for non-repairable tears, Burkhart [4] introduced the partial or ‘functional’ repair, where the less retracted tendon edges restore the rotator cuff’s force couple [6] resulting in ‘a more balanced shoulder’. Nevertheless, as re-tear rates after suture repairs were reported as high as 94 % [15] and debridement only procedures showed good results, especially regarding shorter operating and rehabilitation time [3], the best treatment option for tears involving two or more rotator cuff tendons remains a matter of discussion.
The majority of studies investigating arthroscopic treatment options for mRCT have been reporting on either one [8, 25, 35] or compared two procedures [3, 19]. To our knowledge, the only single-centre study comparing debridement with partial and complete repair presented functional outcome results, but they did not investigate repair integrity [29]. Healing rates of large and massive tears after arthroscopic rotator cuff repair between 6 % [15] and 91 % [30] have been reported, but only few studies used magnetic resonance imaging (MRI) [2, 21]. We are unaware of any arthroscopic study investigating these three different treatment options in three-tendon tears including analysis of functional outcomes and repair integrity on MRI.
The purpose of this cohort study was to evaluate the effectiveness of arthroscopic debridement (DB), partial (PR), and complete repair (CR) for massive rotator cuff tears (mRCT) involving at least three tendons. We hypothesized that functional outcome would be improved regardless arthroscopic management for mRCT; however, repair integrity would be better with CR than PR.
Materials and methods
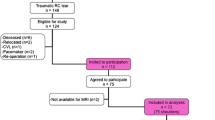
Between January 2008 and December 2009, 144 patients with mRCT underwent shoulder arthroscopy at our hospital. Included were patients with failed non-operative treatment for at least 6 months having a mRCT involving at least three tendons suspected by preoperative MRI or ultrasound, and verified during arthroscopy. Patients with pseudoparalysis defined as complete inhibition of motion and radiological signs of cuff tear arthropathy; older than 85 years; or with previous shoulder surgeries were excluded. Sixty-five patients did not meet study’s inclusion criteria, and 12 patients refused to participate. A group of 67 patients (28 women and 39 men, one bilateral) with a mean age of 66.5 ± 7.2 years were included in this study. Written informed consent was obtained for all patients.
Clinical and subjective assessment
All patients were clinically evaluated by an independent orthopaedic specialist before and after surgery using the constant score (CS) and its subgroups [9] as well as active range of motion in forward flexion, abduction, and external rotation. Additionally, the post-operative total CS was adjusted [36] for age and gender to reflect a percentage of what is considered normal and was finally graded into excellent (>91 %), good (81–90 %), satisfactory (71–80 %), fair (61–70 %), and poor (<60 %). A subjective questionnaire including the ten-point visual analogue scale (VAS) for pain (scale 0–10; 0 = no pain, 10 = severe pain), subjective shoulder value (SSV; percentage of a 100 % normal shoulder) [17], and the quick disabilities of the arm, shoulder, and hand score (qDASH; best: 0, worst: 100) were prospectively collected before surgery and at the latest follow-up. Furthermore, at follow-up, patients were asked to rate their satisfaction with the procedure. Complications were monitored throughout the study.
Radiological and intraoperative assessment
Baseline examination included MRI (n = 60) or ultrasound for patients with pacemakers and claustrophobia (n = 8) to examine the affected shoulder. Pre- and post-operative MRIs (3.0 tesla magnetic resonance scanner, Magnetom Verio, Siemens Medical Solution, Erlangen, Germany) were evaluated by two independent orthopaedic surgeons, who were not directly involved in the surgeries. Tendon retraction and fatty infiltration of the muscle bellies of the supraspinatus (SSP), the infraspinatus (ISP), the subscapularis (SSC), and teres minor (TM) were assessed according to Patte [31] and the modified Goutallier [14] classification. The global fatty degeneration index (GFDI) [18], which is the mean value of fatty infiltration of the three muscles, was calculated. Tendon integrity after arthroscopic rotator cuff repair, but not after arthroscopic DB, was also assessed by MRI. Those eight patients, who had no post-operative MRI due to various reasons including pacemaker, claustrophobia, and refusal, were examined using ultrasound. Due to given artefacts, caused by metal anchors used for tendon repairs, an adapted version of the Sugaya’s [33] classification was utilized. Hence, each tendon was classified according to the following types: tendons showing homogeneous low-intensity or partial high-intensity areas with sufficient thickness were regarded as intact; thinning of the tendon without or minor discontinuity on one image was regarded as partly re-ruptured; and obvious discontinuity in more than one slice was regarded as re-tear.
Massive rotator cuff tear classification system
To summarize mRCT pathology and unify various different existing classification systems, a coding system to describe tear (Fig. 1), treatment, and re-rupture patterns was created.
Drawings and codes to describe a rotator cuff tendon tear. a, b Examples for rupture patterns of rotator cuff tears according to the rupture code (RuC): a intact rotator cuff (RuC: 0n000); b intact subscapularis tendon, normal long head of biceps tendon, full-tendon full-thickness supraspinatus tendon tear, partial-tendon partial-thickness infraspinatus tendon tear, intact teres minor tendon (RuC: 0n140); c intact subscapularis tendon, normal long head of biceps tendon, full-tendon full-thickness supraspinatus tendon tear, partial-tendon full-thickness infraspinatus tendon tear, intact teres minor tendon (RuC: 0n130); and d partial-tendon full-thickness subscapularis tendon tear, dislocated long head of biceps tendon, full-tendon full-thickness supraspinatus tendon tear, full-tendon full-thickness infraspinatus tendon tear, intact teres minor tendon (RuC: 3d110)
The mRCT rupture code (RuC) is based on arthroscopic findings and classifies torn tendons according to width and thickness (full or partial) including five groups: (0) no rupture, (1) full-tendon full-thickness tear (typical for a complete SSP tear), (2) full-tendon partial-thickness tear (such as bursal or articular sided partial tears), (3) partial-tendon full-thickness tears (typical for upper SSC tendon tears or partial ISP tendon tears), and (4) partial-tendon partial-thickness tears (i.e. type I tears of the SSC tendon according to Lafosse et al. [24] or partial SSP rupture Ellman I° [12]). The long head of biceps (LHB) tendon was classified as ‘n’ for normal, ‘a’ for absent, ‘p’ for partially torn, or ‘d’ for dislocated. Given these options, each tendon was classified according to the RuC beginning from anterior to posterior (SSC-LHB-SSP-ISP-TM). Examples for rupture patterns of rotator cuff tears according to the RuC are presented in Fig. 1a–d.
Furthermore, a treatment code (TxC) for each tendon, in the same order (SSC-LHB-SSP-ISP-TM) as for the pathology, including (0) left untreated or debridement (for LHB: absent or untreated), (1) partially repaired (for LHB: tenotomy), and (2) completely repaired (for LHB: tenodesis), was established (e.g. a CR with biceps tenotomy would then be the TxC 21220).
Additionally, a re-tear code (RrC) describes all tendons, except the LHB tendon, in the same order as the other codes (SSC-SSP-ISP-TM) using (0) for left untreated or debridement, (1) for intact suture, and (2) for re-ruptured sutures. For example, a completely re-ruptured CR would then be RrC 2220.
Surgical procedure and rehabilitation protocol
Arthroscopic procedures were performed by three experienced shoulder surgeons (WA, BK, SS). Patients were placed in lateral decubitus position. In general anaesthesia with interscalene nerve block), a standard posterior viewing portal was established, and other portals were placed as needed. After treatment of concomitant lesions (subacromial decompression, distal clavicle resection, LHB tenotomy/tenodesis), the rotator cuff was debrided and tissue quality, tendon mobility, retraction, and rupture shape was assessed. Whenever decision of an attempt for partial or complete rotator cuff reconstruction was made, extensive tendon releases (double, anterior, or interval slide in continuity [26]) with resection of the coracohumeral ligament of the coracoid base, juxtaglenoidal as well as extraarticluar tendon and muscle mobilization were performed. Where the subscapularis tendon was torn (≥Lafosse II°), a refixation in a single row fashion was carried out. Thereafter, the posterosuperior rotator cuff was addressed aiming to bring the tendons back to the footprint of the greater tuberosity for complete coverage (suture bridge repair). Otherwise, a medializing single row repair using margin convergence techniques was performed. In cases where despite margin convergence techniques a complete repair was not possible, a partial repair was attempted with refixation of all possible tendons and the goal of force couple restoration. Most of the three arthroscopic procedures were performed with concomitant treatments (DB 91 %; PR 86 %; CR 96 %).
According to the rehabilitation protocol for tendon repairs, shoulders were immobilized for 6 weeks using a sling (UltraSling, Breg MDSS GmbH, Hannover, Germany). Physiotherapy mobilization regimen included immediate passive motion and passive-assisted motion with closed chain exercises to work scapulothoracal muscles. Active full range of motion exercises was allowed to be started 6 weeks post-operatively or immediately after surgery in case of debridement.
Institutional review board (Ethikkommission des Krankenhauses der Barmherzigen Schwestern Wien) approval was obtained for this prospective non-randomized single-centre cohort study.
Statistical analysis
The sample size, which was calculated a priori according to preliminary data of patients with rotator cuff tears, required to detect a relevant difference of 12 points and a standard deviation of 15 points between pre- and post-operative CS (paired-sample t test) with a power of 90 % and a type I error of 5 % is at least 18 patients in each group. Descriptive statistics were used to present patients’ characteristics. Continuous variables were tested by visual inspection and the Kolmogorov–Smirnov test. Normal distributed continuous variables were expressed as: mean ± standard deviation; non-normal distributed continuous variables as median and range; and categorical data with absolute frequencies and percentages. The Chi-square or Fisher exact test was used for discrete variables. Demographic data were evaluated using one-way analysis of variance (ANOVA), Chi-square, and Kruskal–Wallis tests. Paired t tests and Wilcoxon matched-pair tests (depending on variable distribution) were performed to analyse differences between pre- and post-operative measurements. Independent t tests and Mann–Whitney U tests were used to compare outcome scores between treatment groups. For Table 3, due to small numbers of partly re-ruptured tendons, we combined partly and totally re-ruptured tendons into one group (re-rupture). The level of statistical significance was set at the conventional P < 0.05 for all tests. All data were analysed using SPSS 21® (IBM® Corporation, Armonk, NY, USA).
Results
Rupture patterns and reparability of all 68 mRCT are shown in Table 1. All baseline characteristics, except of GFDI, were similar between the three arthroscopic treatments for mRCT (Table 2). Detailed group analyses regarding GFDI revealed significant differences between DB versus PR (P = 0.046); PR versus CR (P = 0.003); and CR versus DB (P < 0.001). Furthermore, there were more SSC, SSP, and ISP muscles with high-grade fatty infiltration (grade 3 or 4: as much or more fat than muscle [14]) in the DB group (6, 59, 29 %, respectively) than in PR (5, 27, 9 %, respectively) and CR (0, 10, 5 %, respectively). The only three patients with a grade 4 fatty degeneration of the ISP underwent debridement alone. None of the patients with CR had a fatty infiltration higher than grade 3 [14].
Revision surgery was required for six patients (8.8 %): three patients required open lavage and debridement for post-operative infection (PR n = 2; CR n = 1); one patient had an arthroscopic anchor removal for implant loosening after intact PR; and two patients were revised with a reverse total shoulder arthroplasty for progressive pain and loss of function (DB, retorn CR). The median follow-up for the remaining 62 shoulders (47 right, 15 left) was 42 months (range 23–70 months).
Clinical and subjective outcome
All clinical and subjective scores significantly improved from pre- to post-operative (P < 0.01; Supplement Table A). Results of the total CS and its subgroups, SSV, and qDASH for each arthroscopic treatment group are summarized in Fig. 2. PR reached similar post-operative outcome when compared to DB; however, all scores (CS, VAS, SSV, and qDASH) were significantly better in the CR group (P ≤ 0.02; Supplement Table A).
No significant differences regarding post-operative outcome between PR with (n = 11) and without (n = 8) force couple restoration were detected (total CS 65.9 ± 9.7 vs. 69.6 ± 10.4; SSV 70.0 ± 14.8 vs. 79.4 ± 10.8; qDASH 24.8 ± 11.0 vs. 14.5 ± 17.0). Even when post-operative total CS, SSV, and qDASH of DB were compared to PR with force couple restoration as well as to PR without force couple restoration, no significant differences were detected.
The vast majority of patients were satisfied with their arthroscopic procedure (DB 87 %; PR 86 %; CR 91 %).
Repair integrity
More partially than completely repaired tendons were totally re-ruptured (53 and 29 %, respectively), whereas more intact tendons were detected with CR (47 %) compared to PR (40 %). The overall re-tear rate including totally and partially re-ruptured tendons was 56 %.
Intact CR showed significantly better outcome compared to intact PR (total CS 83.4 ± 7.3 vs. 68.5 ± 10.6, P = 0.009; SSV 95.0 ± 6.0 vs. 75.8 ± 12.0, P = 0.002; qDASH 5.4 ± 8.3 vs. 21.2 ± 9.5, P = 0.020). No differences were detected regarding total CS, SSV, qDASH between intact PR and DB. Interestingly, no significant differences were found between intact versus re-ruptured PR and CR when compared within integrity groups.
Significantly more patients without concomitant treatment required revision surgery (33 %) than patients undergoing additional procedures (7 %); all other investigated factors did not influence post-operative outcome (Table 3).
Discussion
The most important findings were (1) that all three arthroscopic surgical techniques lead to significant improvements from baseline to the latest follow-up regarding clinical and subjective outcomes; (2) that more intact tendons were detected with complete than with partial repairs; and (3) that complete repairs were significantly superior to partial repairs and debridements, whereas debridement and partial repair did not show significant differences.
An inherent weakness of common rotator cuff tear classification systems is that they still rely on a former anatomical model and that they do hardly correlate with reported tear size (i.e. supraspinatus tear of 2.5 cm) according to a recent anatomical study by Mochizuki et al. [28]. Additionally, Kuhn et al. [23] showed low interobserver agreement in classifying rotator cuff tears; the only agreement was found in distinguishing partial from full-thickness tears. To overcome difficulties in classifying rotator cuff tears, we established a simplified rotator cuff rupture code allowing specification according to involved tendon thickness (full or partial) as well as width (full or partial).
Potential factors influencing arthroscopic reparability of mRCT and treatment strategies may be related to surgeon’s experience and skills [1], as well as the rehabilitation protocol (immobilization versus immediate active motion). Similar to other studies [11, 37], in the present work, tendon reparability was affected by fatty infiltration, although functional improvement was not hindered as reported by Burkhart et al. [5].
Force couple restoration in partial repairs is generally believed to be important for a more balanced shoulder and a better functional outcome [4]. Yet, we are unaware of any study confirming this theory. According to our findings, there is no difference in any parameter whether the force couple reconstruction in PR could be achieved or not, even when compared to DB. Our findings are similar to a recently published study [35] reporting no increase in abduction strength after arthroscopic partial repair, but an improvement in active forward flexion and abduction. In the same study [35], the partial repair was described as a force couple restoration leaving a small residual tendon defect or only part of the footprint uncovered, while in our PR regardless of force couple restoration, not all tendons could be forwarded to the footprint, and therefore, a notable defect remained in the rotator cuff. Obviously, discrepancies in defining partial repair and force couple restoration are evident. Important to notice is that three studies investigating partial repair in mRCT excluded those cases with SSC involvement [3, 13, 22]. Thus, it can be assumed that this partial repair would result in a functional repair. Interestingly, comparing such a force couple restoration to debridement one study [13] showed significant differences, but the other one did not [3]. Satisfactory outcome with arthroscopic debridement or partial repair regardless of force couple restoration was reported in all studies [3, 13, 22].
According to such findings, it might be assumed that arthroscopic surgery to treat mRCT regardless of the technique leads to better short-term outcome; however, in our post-operative findings, CR was superior to PR and DB in the majority of the parameters. As opposed to our results, a retrospective study by Iagulli et al. [19], which compared only between partial and complete repair, did not detect significant post-operative differences in outcome. As their only outcome parameter was the UCLA score, pain, strength, or range of motion were not outlined separately, and thus, it is of limited comparative value.
The only study [29] reporting functional outcome of all three treatment methods for mRCT was able to observe a trend towards better overall motion and strength in complete and partial repair compared to debridement, which is only partly consistent with the present work. While the group reported significant improvements in external rotation, but only a trend towards better subjective score for those patients who underwent complete compared to partial repair, we found CR to be superior regarding strength, but not with range of motion. Such differences are likely attributed to the uneven distribution of patients with fewer patients in their debridement (n = 6) and partial repair (n = 11) group compared to our study. Furthermore, results may be not comparable since different surgical techniques (open vs. arthroscopic) were used. Unfortunately, this retrospective comparison study by Moser et al. [29] did not report fatty infiltration and re-tear rates.
The overall re-tear rate (56 %) in the present study was slightly higher than reported by the few other MRI-based studies (42 % [21]; 53 % [7]) and by the US-based report of Berth et al. (52 % [3]), which may be due to differences in fatty infiltration and tear size. Interestingly, although all values were better in the intact tendon groups, significant differences between intact and re-rupture within the repair groups were not detectable, which might be explained by the small number of cases in the groups. Post-operative strength in abduction was significantly better in CR than in PR and DB, while preoperative strength was the lowest in CR, indicating that the highest improvements regarding strength can be reached with CR. Thus, this study’s results suggest that the primary aim to treat mRCT should be a CR. However, if a CR is not achievable, it is still questionable if PR instead of DB, since outcome results are similar, is to be the preferred arthroscopic procedure. Notwithstanding, a pioneer work by Zvijac et al. [38] showed a deterioration of shoulder function after debridement at a long-term follow-up. Comparative long-term studies, especially regarding partial rotator cuff repairs, are still necessary to assess differences between treatment options.
A limitation of the present study is the relative small number of subjects per treatment group and that patients were treated by three different surgeons. However, our results are similar to single treatment studies regarding arthroscopic debridement [20], partial [35], and complete repairs [8]. We are also aware that our study is not randomized. Although numbers of subjects in the treatment groups were nearly equal, randomization in such a challenging pathology, where tendon repair depends very much on tissue quality, three-dimensional tendon retraction, and tendon substance defects, is not feasible. Yet, the clinical relevance of the present study comparing arthroscopic debridement, partial, and complete repair for mRCT is that all three techniques significantly improve post-operative outcome. However, CR—if possible—should be aimed for, whereas force couple restoration in PR does not influence clinical outcome as opposed to its theory.
Conclusion
Arthroscopic DB, PR, and CR were effective in treating mRCT involving at least three tendons. Reparability of mRCT was influenced by fatty degeneration of the muscles. However, CR showed the most favourable improvements in this short-term follow-up.
References
Anakwenze OA, Baldwin K, Milby AH, Warrender W, Shulman B, Abboud JA (2013) Arthroscopic repair of large rotator cuff tears using the double-row technique: an analysis of surgeon experience on efficiency and outcomes. J Shoulder Elbow Surg 22(1):26–31
Berdusco R, Trantalis JN, Nelson AA, Sohmer S, More KD, Wong B, Boorman RS, Lo IK (2013) Arthroscopic repair of massive, contracted, immobile tears using interval slides: clinical and MRI structural follow-up. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2683-9
Berth A, Neumann W, Awiszus F, Pap G (2010) Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol 11(1):13–20
Burkhart SS (1994) Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy 10(1):4–19
Burkhart SS, Barth JR, Richards DP, Zlatkin MB, Larsen M (2007) Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy 23(4):347–354
Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A (1994) Partial repair of irreparable rotator cuff tears. Arthroscopy 10(4):363–370
Choi S, Kim MK, Kim GM, Roh YH, Hwang IK, Kang H (2014) Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg. doi:10.1016/j.jse.2014.02.021
Chung SW, Kim JY, Kim MH, Kim SH, Oh JH (2013) Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med 41(7):1674–1683
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
DeOrio JK, Cofield RH (1984) Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am 66(4):563–567
Dwyer T, Razmjou H, Henry P, Gosselin-Fournier S, Holtby R (2013) Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2745-z
Ellman H (1990) Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res 254:64–74
Franceschi F, Papalia R, Vasta S, Leonardi F, Maffulli N, Denaro V (2015) Surgical management of irreparable rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 23(2):494–501
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 8(6):599–605
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86-A(2):219–224
Gerber C, Fuchs B, Hodler J (2000) The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 82(4):505–515
Gilbart MK, Gerber C (2007) Comparison of the subjective shoulder value and the constant score. J Shoulder Elbow Surg 16(6):717–721
Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S (2003) Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg 12(6):550–554
Iagulli ND, Field LD, Hobgood ER, Ramsey JR, Savoie FH 3rd (2012) Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med 40(5):1022–1026
Kempf JF, Gleyze P, Bonnomet F, Walch G, Mole D, Frank A, Beaufils P, Levigne C, Rio B, Jaffe A (1999) A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy 15(1):56–66
Kim JR, Cho YS, Ryu KJ, Kim JH (2012) Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: assessment of repair integrity on magnetic resonance imaging. Am J Sports Med 40(4):786–793
Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM (2012) Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy 28(6):761–768
Kuhn JE, Dunn WR, Ma B, Wright RW, Jones G, Spencer EE, Wolf B, Safran M, Spindler KP, McCarty E, Kelly B, Holloway B (2007) Interobserver agreement in the classification of rotator cuff tears. Am J Sports Med 35(3):437–441
Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R (2007) Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am 89(6):1184–1193
Liem D, Lengers N, Dedy N, Poetzl W, Steinbeck J, Marquardt B (2008) Arthroscopic debridement of massive irreparable rotator cuff tears. Arthroscopy 24(7):743–748
Lo IK, Burkhart SS (2004) The interval slide in continuity: a method of mobilizing the anterosuperior rotator cuff without disrupting the tear margins. Arthroscopy 20(4):435–441
Meyer DC, Wieser K, Farshad M, Gerber C (2012) Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med 40(10):2242–2247
Mochizuki T, Sugaya H, Uomizu M, Maeda K, Matsuki K, Sekiya I, Muneta T, Akita K (2008) Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am 90(5):962–969
Moser M, Jablonski MV, Horodyski M, Wright TW (2007) Functional outcome of surgically treated massive rotator cuff tears: a comparison of complete repair, partial repair, and debridement. Orthopedics 30(6):479–482
Park JY, Siti HT, Keum JS, Moon SG, Oh KS (2010) Does an arthroscopic suture bridge technique maintain repair integrity?: a serial evaluation by ultrasonography. Clin Orthop Relat Res 468(6):1578–1587
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res 254:81–86
Rockwood CA Jr, Williams GR Jr, Burkhead WZ Jr (1995) Debridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am 77(6):857–866
Sugaya H, Maeda K, Matsuki K, Moriishi J (2007) Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 89(5):953–960
Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F (1996) Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand 67(3):264–268
Wellmann M, Lichtenberg S, da Silva G, Magosch P, Habermeyer P (2013) Results of arthroscopic partial repair of large retracted rotator cuff tears. Arthroscopy 29(8):1275–1282
Yian EH, Ramappa AJ, Arneberg O, Gerber C (2005) The Constant score in normal shoulders. J Shoulder Elbow Surg 14(2):128–133
Yoo JH, Cho NS, Rhee YG (2013) Effect of postoperative repair integrity on health-related quality of life after rotator cuff repair: healed versus retear group. Am J Sports Med 41(11):2637–2644
Zvijac JE, Levy HJ, Lemak LJ (1994) Arthroscopic subacromial decompression in the treatment of full thickness rotator cuff tears: a 3- to 6-year follow-up. Arthroscopy 10(5):518–523
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Heuberer, P.R., Kölblinger, R., Buchleitner, S. et al. Arthroscopic management of massive rotator cuff tears: an evaluation of debridement, complete, and partial repair with and without force couple restoration. Knee Surg Sports Traumatol Arthrosc 24, 3828–3837 (2016). https://doi.org/10.1007/s00167-015-3739-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3739-9