Abstract
Purpose
While a significant research has gone into identifying patients at highest risk of recurrence following primary patellar dislocation, there has been little work exploring the outcomes of patients who do not have a recurrent patellar dislocation. We hypothesize that patients without recurrent dislocation episodes will exhibit significantly higher KOOSs than those who suffer recurrent dislocations, but lower scores than published age-matched normative data.
Methods
A retrospective review of patients with nonoperatively treated primary lateral patellar dislocations was carried out, and patients were contacted at a mean of 3.4 years (range 1.3–5.5 years) post-injury. Information regarding subsequent treatment and recurrent dislocations along with patient-reported outcome scores and activity level was collected.
Results
One hundred and eleven patients (29.8 %) of 373 eligible patients agreed to study participation, seven of whom were excluded because they underwent subsequent patellar stabilization surgery on the index knee. Seventy-six patients (73.1 %) reported no further dislocation events, and the mean KOOS subscales at follow-up were: symptoms—80.2 ± 18.8, pain—81.8 ± 16.2, ADL—88.7 ± 15.9, sport/recreation—72.1 ± 24.4, and QOL—63.9 ± 23.8 at a mean follow-up of 3.3 years (range 1.3–5.5 years). No significant differences in any of the KOOS subscales were noted between these patients and the group that reported recurrent patellar dislocations. Only 26.4 % of the patients without further dislocations reported they were able to return to desired sport activities without limitations following their dislocation.
Conclusion
Patients who do not report recurrent patellar dislocations following nonoperative treatment of primary patellar dislocations are in many cases limited by this injury 3 years following the initial dislocation event.
Level of evidence
Retrospective cohort study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral patellar dislocations are debilitating injuries that frequently affect young, active patients. In spite of the relatively high incidence of this condition, there remains a significant controversy regarding the ideal treatment protocol [23]. Management of acute primary patellar dislocation has historically been conservative, with early operative treatment reserved for patients with associated osteochondral injuries or fractures [17]. This recommendation is based on natural history studies that have demonstrated that 50–70 % of patients will suffer no recurrent dislocations with conservative management of this injury [5, 7, 9, 10]. The conclusion that 30–50 % of patients do well with nonoperative management because they do not redislocate is flawed as patients may continue to have pain, subjective feelings of instability, or other symptoms that limit their activity level and harm their quality of life without experiencing an additional dislocation event.
While a significant research has gone into identifying patients at highest risk of recurrent dislocation [1, 8, 24], there has been little work exploring the outcomes of patients who do not have a recurrent patellar dislocation following nonoperative management of a primary lateral patellar dislocation. These patients’ activity level, symptoms of subjective instability, and quality of life have been poorly defined in prior studies. Given the controversy surrounding the ideal management of acute primary patellar dislocations, a more detailed assessment of patients who have not suffered recurrent dislocations is critical.
The goal of this study is to assess the outcomes of patients treated nonoperatively for primary lateral patellar dislocations with a focus on those patients in whom no subsequent patellar dislocations occur. We hypothesize that these patients will exhibit significantly higher KOOSs than those who suffer recurrent dislocations, but fail to return to pre-injury activity levels and continue to report lower patient-reported outcome scores than published age-matched normative data.
Materials and methods
Patients who presented to two high-volume sports medicine centres between 2008 and 2012 with a primary patellar dislocation were identified through billing records. Following institutional review board approval, chart review was undertaken to confirm the diagnosis and collect demographic information. Patients were eligible for inclusion if they suffered a primary lateral patellar dislocation during the study period and were treated without a surgical procedure to improve patellar stability. The nonoperative treatment protocol varied by physician preference, but typically included bracing with a focus on early mobilization and restoration of range of motion and function.
The patients identified as meeting inclusion criteria were contacted by mail and/or telephone at a minimum 2 years follow the index dislocation event and were asked to complete a questionnaire that included Minnesota Activity Scale and Knee Injury and Osteoarthritis Outcome Score (KOOS) [19, 20], as well as provide information regarding subsequent treatment and whether a recurrent patellar dislocation occurred. Patients who underwent a patellar stabilization procedure during the follow-up period were excluded, leaving the study group of patients who were treated without surgical stabilization.
Institutional review board approval
This study was approved by the Institutional Review Board of The Ohio State University, study 2013H0221.
Statistical analysis
Data were compiled, and descriptive statistics were calculated. Patients were subsequently divided into two groups based on whether they suffered a recurrent patellar dislocation in the follow-up period. Mean KOOSs of patients in each of the two groups were compared using unpaired t tests. A power analysis demonstrated that 102 patients would be needed to detect a clinically relevant 10-point difference in KOOS subscales with a power of 0.80 and α = 0.5 based on normative KOOS data [18]. A comparison of demographic variables was made to determine whether the patients who were available for follow-up were a representative sample of the initial population.
Results
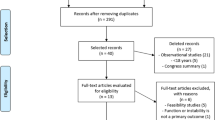
Chart review yielded a total of 405 patients who presented with a primary patellar dislocation during the study period. Thirty-two patients that were treated initially with a patellar stabilization procedure were excluded, yielding 373 patients eligible for inclusion in the study. Of the eligible patients, 111 patients (29.8 %) were contacted, agreed to study participation, and completed the outcome questionnaire. Seven patients were excluded from analysis because they had undergone subsequent patellar stabilization surgery on the index knee (Fig. 1).
The remaining 104 patients form the study population and consisted of 50 patients from (centre removed for blinding) and 54 patient from (centre removed for blinding). There were 26 patients that were treated with initial arthroscopic debridement without stabilization and 78 patients who were treated nonoperatively. There were 63 females (60.6 %) and 41 males (39.4 %), with a mean age of 23.8 ± 8.9 years (range 11–48 years) at the time of primary dislocation. The patients who did not complete survey were not significantly different in age (mean age of 23.6 ± 8.9 years, p = NS) and sex (49 % male, p = NS) compared to the included patients. At a mean follow-up of 3.4 years (range 1.3–5.5 years), the mean KOOS subscales were: symptoms—78.9 ± 18.8, pain—80.6 ± 17.2, ADL—87.9 ± 17.3, sport/recreation function—69.9 ± 24.9, and QOL—62.5 ± 24.7.
During the follow-up period, 76 patients (73.1 %) reported no further dislocation events, while the remaining 28 patients (26.9 %) reported at least one recurrent dislocation. In the group that reported no subsequent patellar dislocations, the mean KOOS subscales were: symptoms—80.2 ± 18.8, pain—81.8 ± 16.2, ADL—88.7 ± 15.9, sport/recreation—72.1 ± 24.4, and QOL—63.9 ± 23.8 at a mean follow-up of 3.3 years (range 1.3–5.5 years). No significant differences in any of the KOOS subscales were noted between these patients and the group that reported recurrent patellar dislocations in the follow-up period (Table 1).
Among the 72 patients without recurrent dislocations who completed the Minnesota Activity Scale, 62 patients (86.1 %) reported that they were able to return to their most important physical activity following their patellar dislocation. However, only 19 patients (26.4 %) reported they were able to return to activities without limitations following their dislocation. Of the 53 patients reporting limitations to their activity level, 46 (86.8 %) identified their patellar dislocation as the source of their limited activity level.
Discussion
The key finding of this study is that patients who do not report recurrent patellar dislocations following nonoperative treatment of primary patellar dislocations are in many cases still quite limited by this injury at an average of 3.3 years following the initial dislocation event. In contrast to our hypothesis, a large proportion of these patients report persistent limitations in their activity level that they attribute to the patellar dislocation and the patient-reported outcomes of this group are not significantly different from those who do report recurrent patellar dislocations but have not undergone surgical stabilization.
The KOOSs reported by patients in the study who did not report subsequent patellar dislocations are worse than KOOSs reported by control patients of similar age by Paradowski et al. [18] (Fig. 2). The most striking differences are noted in the sport/recreation function and knee-related quality of life subscales. These data are consistent with the reports by patients in the study group that they remain limited in the return to desired activity and, importantly, attribute this limitation to persistent problems with their knee.
Graph of KOOS subscales of patients who reported no recurrent patellar dislocations after their initial dislocation event and age-matched controls [18]
The findings of this study indicate that in many patients, current conservative treatment for this injury does not restore patients to pre-injury function. Numerous nonoperative treatment protocols have been described, but the overall progression is fairly consistent. Following an early period in which swelling and pain are controlled (usually with some period of immobilization) and motion is restored, therapy progresses along functional guidelines by addressing poor core strength, gluteal weakness, and dynamic knee valgus, which contribute to the knee positions and movement patterns that can lead to recurrent dislocation [12–14, 22]. It is important to note that this study does not compare patients treated operatively with those treated nonoperatively and therefore should not be misconstrued as evidence that initial operative treatment in these patients is superior. Rather, these data demonstrate that the presence or absence of recurrent dislocations alone is not sufficient to assess patients following this injury and point out the need for further comparative studies evaluating treatment of these injuries to improve the results reported here.
Some prior studies have touched on the topic of activity limitation and pain following nonoperative treatment of patellar instability. A short-term follow-up study by Atkin et al. [1] demonstrated that at 6 months following dislocation, over 30 % of patients were still unable to return to sport and the vast majority demonstrated decreased activity relative to their pre-injury level, although none had suffered a recurrent dislocation. Several recent prospective studies comparing operative and nonoperative management of acute first-time patellar dislocations provide further insight into the results of nonoperative treatment in these patients [6, 11]. These studies demonstrate a significant variability in Kujala (pain) scores following nonoperative treatment, with three studies reporting a mean value between 69 and 78 [2–4], while three studies reported relatively good scores in the mid-1980s–1990s [15, 16, 21]. Importantly, these studies did not specifically report Kujala scores based on whether a recurrent dislocation occurred, limiting the available information about these patients.
In a longer-term study of 100 nonoperatively treated patellar dislocations, Maenpaa and Lehto reported on 56 patients that did not exhibit recurrent dislocations [10]. They reported 19 of these patients (33.9 %) were dissatisfied enough with their knee function to undergo late reconstructive surgery, but again, the results beyond an absence of recurrent dislocations were not specifically reported for the remaining 37 patients [10].
Several limitations of the current study are noted. Primarily, the follow-up rate is quite low, making response bias possible. The patients who participated in the study may not be representative of the treatment group as a whole. Analysis of demographic data between the participants and the remaining patients did demonstrate the groups to be similar age and sex. There may, however, be other differences between the two groups that are not known. This limitation does not preclude the study from providing useful information, as it is the first to specifically report on the function of those patients who did not report recurrent dislocations following nonoperative treatment of primary patellar dislocations. Even if these patients represent only a nonrepresentative subset of the treatment group, it remains clear that at least some patients who do not have recurrent dislocations following treatment are significantly limited in their knee function and would likely benefit from further treatment.
An additional limitation is the lack of radiographic studies that would allow for a detailed analysis of potential imaging predictors of poor outcome in the absence of recurrent dislocation. Certain imaging factors associated with increased risk of recurrent dislocation such as trochlear dysplasia, patella alta, or skeletal immaturity may also be associated with poorer outcome even in those without recurrent instability. Further studies are needed to investigate these questions.
The most clinically relevant finding of this study is the clear evidence that the presence or absence of recurrent dislocations alone is not sufficient to describe the outcome of patients following a primary patellar dislocation. Patient-reported outcome scores provide a more complete picture of the patient’s outcome, and their use should be considered in assessment of these patients.
Conclusion
Many patients who do not report recurrent patellar dislocations following nonoperative treatment of primary patellar dislocations are still limited by this injury at an average of 3 years following the initial dislocation event. Complete assessment of the success of nonoperative management of primary patellar dislocations requires investigation beyond the incidence of recurrent dislocations.
References
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C (2000) Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28:472–479
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 40:114–122
Camanho GL, Viegas Ade C, Bitar AC, Demange MK, Hernandez AJ (2009) Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 25:620–625
Christiansen SE, Jakobsen BW, Lund B, Lind M (2008) Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 24:881–887
Cofield RH, Bryan RS (1977) Acute dislocation of the patella: results of conservative treatment. J Trauma 17:526–531
Erickson BJ, Mascarenhas R, Sayegh ET, Saltzman B, Verma NN, Bush-Joseph CA, Cole BJ, Bach BR Jr (2015) Does operative treatment of first-time patellar dislocations lead to increased patellofemoral stability? A systematic review of overlapping meta-analyses. Arthroscopy 31:1207–1215
Hawkins RJ, Bell RH, Anisette G (1986) Acute patellar dislocations. The natural history. Am J Sports Med 14:117–120
Lewallen LW, McIntosh AL, Dahm DL (2013) Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 41:575–581
Maenpaa H, Huhtala H, Lehto MU (1997) Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand 68:424–426
Maenpaa H, Lehto MU (1997) Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med 25:213–217
Magnussen RA, Duffee AR, Kalu D, Flanigan DC (2015) Does early operative treatment improve outcomes of primary patellar dislocation? A systematic review. Curr Orthop Pract 26:281–286
McConnell J (2007) Rehabilitation and nonoperative treatment of patellar instability. Sports Med Arthrosc 15:95–104
Menetrey J, Putman S, Gard S (2014) Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc 22:2320–2326
Monson J, Arendt EA (2012) Rehabilitative protocols for select patellofemoral procedures and nonoperative management schemes. Sports Med Arthrosc 20:136–144
Nikku R, Nietosvaara Y, Aalto K, Kallio PE (2005) Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop 76:699–704
Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y (2008) Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am 90:463–470
Panni AS, Vasso M, Cerciello S (2013) Acute patellar dislocation. What to do? Knee Surg Sports Traumatol Arthrosc 21:275–278
Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM (2006) Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS). BMC Musculoskelet Disord 7:38
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee injury and osteoarthritis outcome score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Roos EM, Toksvig-Larsen S (2003) Knee injury and osteoarthritis outcome score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Sillanpaa PJ, Mattila VM, Maenpaa H, Kiuru M, Visuri T, Pihlajamaki H (2009) Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. J Bone Joint Surg Am 91:263–273
Smith TO, Chester R, Cross J, Hunt N, Clark A, Donell ST (2015) Rehabilitation following first-time patellar dislocation: a randomised controlled trial of purported vastus medialis obliquus muscle versus general quadriceps strengthening exercises. Knee 22:313–320
Smith TO, Donell S, Song F, Hing CB (2015) Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev 2:CD008106
Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE (2015) The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: a magnetic resonance imaging study. Am J Sports Med 43:921–927
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Magnussen, R.A., Verlage, M., Stock, E. et al. Primary patellar dislocations without surgical stabilization or recurrence: how well are these patients really doing?. Knee Surg Sports Traumatol Arthrosc 25, 2352–2356 (2017). https://doi.org/10.1007/s00167-015-3716-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3716-3