Abstract
Purpose
The purpose was to describe physical activity with respect to leisure and working activity in patients operated on by high tibial osteotomy using the hemicallotasis technique for knee osteoarthritis (OA), preoperatively and 10 years postoperatively.
Methods
Seventy-nine patients, median age 55 (range 35–66), operated on by high tibial osteotomy using the hemicallotasis technique for knee OA 2001–2003 were included. Questionnaires for evaluation of physical and working activity, satisfaction as well as the Knee injury and Osteoarthritis Outcome Score (KOOS) were filled in preoperatively and 2 and 10 years postoperatively. Conversion to knee arthroplasty was obtained through the Swedish Knee Arthroplasty Register. Changes between two postoperative measurements were assessed by Wilcoxon’s rank test.
Results
Twenty-five patients were converted to a total knee arthroplasty, and nine patients were lost to follow-up during the 10 years, resulted in 45 patients available for follow-up. Preoperatively, 33/45 patients were physically active mainly in heavy yard/household work, and 43/45 patients were working active. Ten years after the HCO, 23/45 patients were still active with golf, dancing, hiking, etc., and 23/45 were retired. At 10 years postoperatively compared to 2 years postoperatively, the patients experienced more problems with pain (89 compared to 69, p = <0.0001). Of 45 patients, 36 were satisfied with the high tibial osteotomy surgery in general 10 years postoperatively, while 13/45 were satisfied with their sport and recreational function.
Conclusions
The 10-year results indicate that high tibial osteotomy using the hemicallotasis technique for knee OA is an option for selected patients that improves the level of physical activity, with mild deterioration over time, and gives the majority of the patients the possibility to be working active until retirement.
Level of evidence
Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sport and recreational activities are important for many individuals to gain and maintain physical and mental health. In patients with knee osteoarthritis (OA), physical limitations and pain cause successively increasing disabilities that affects daily living.
High tibial osteotomy (HTO) is a joint-preserving alternative, mostly used in younger and/or physically active patients with uni-compartmental knee OA. HTO alters the load from the damaged to the unaffected compartment of the knee in purpose to reduce pain, increase function and postpone or in the best cases eliminate the need of knee replacement.
Several methods and techniques are possible for HTO. HTO with the hemicallotasis technique (HCO) is an open-wedge osteotomy that allows free mobilization and weight bearing immediately postoperatively, an advantage over the traditional method of closed-wedge osteotomy and the open-wedge osteotomy with internal fixation that usually requires partial loading and/or braces/plaster [14]. The internal fixation is secured with several different types of plates of which some have reported mid-term results concluding that the technique is suitable for medial uni-compartmental OA [2, 7, 11, 13, 26, 27]. However, the number of patients in these studies is relatively few. Further, the open-wedge osteotomies are bone sparing in contrast to closed-wedge osteotomy that may be a favour if conversion to knee arthroplasty will be necessary. The HCO allows correction of larger deformities, the precision of the correction can be more accurate, and the patients have no implant left after the fixator is removed. Disadvantages of the HCO technique are the relatively long time with external fixation as well as the need of more frequent follow-ups.
Few studies have evaluated the effect of knee OA on sport and recreational activities before and after high tibial osteotomy in the long term. In a retrospective study, Saltzmann et al. found that younger patients were able to participate in sport and recreational activities 36 months postoperatively similar to the preoperative level after HTO using the open-wedge technique with internal fixation [20]. In a prospective study, only half of the patients operated on by HTO with the hemicallotasis technique (HCO) were sport and recreation active the year before surgery and reported extreme severity with sport and recreation function. The sport and recreation function was significantly improved at the 2-year follow-up, however, indicated still considerable problems [21]. In a retrospective follow-up, 9/27 patients operated on with HTO using the close-wedge technique were able to manage high-activity sports and heavy work 11 years after surgery [11].
Differences in patient selection, indication for surgery and method of HTO used may be reasons for varying result. However, there is probably a wide variation in sport and recreation activity experience among patients, from high-demanding sport active patients to patients that never have participated in any kind of sports and recreational activities.
The hypothesis was that the majority of the patients operated on by the HCO for knee OA have advantages of the surgery 10 years postoperatively with respect to leisure and working activity. As the longer perspective of knee reconstruction surgery is important in younger and/or physically active patients, the aim of this study was to describe physical activity with respect to leisure and working activity preoperatively until 10 years postoperatively.
Materials and methods
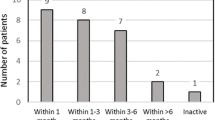
Ninety-six high tibial osteotomies operated on by the hemicallotasis technique (HCO) for knee OA were scheduled in 87 consecutive patients, 65 % men with a mean age of 54 years (range 35–66), between August 2001 and April 2003 at the department of Orthopaedics, Lund University Hospital, Sweden. The left HCO in patients with simultaneously surgery and the first HCO in patients with bilateral surgery within one year were excluded. As eight patients disagreed to participate in the study, 79 patients were included (Fig. 1). Patient’s demographics are given in Table 1.
High tibial osteotomy by the hemicallotasis technique (HCO)
HCO is an open-wedge osteotomy based on successive correction of the malalignment using an external fixation [8, 9].
The indication of surgery by the HCO is a consideration based on several aspects, such as the presence of radiographic knee OA, knee alignment, pain, disability and level of activity in both working life and leisure time. When the orthopaedic surgeon found an indication for HCO, the patient was given written and verbal information in a special outpatient clinic for patients treated by external fixation and the final decision on surgery was taken. In the present study, one surgeon (STL) assessed all subjects.
Postoperative treatment
Full weight bearing and free mobilization were allowed postoperatively. Physiotherapy was prescribed individually and related to the needs for each patient. The patient and physiotherapist decided the length of the rehabilitation period.
The patients visited the outpatient clinic for pin site care, initiation and follow-up of the correction once a week during the treatment period. The correction started 7–10 days postoperatively. The patient made the correction by adjusting one quarter of a turn four times per day on a distractor placed at the external fixator. The correction was determined by radiographic hip–knee–ankle angle (HKA-angle) of the knee. In patients with medial knee OA, the goal was to archive 4° of valgus and 0–3° of varus in those with lateral knee OA. About 10 weeks postoperatively, the first healing control by radiography and ultrasound examination was performed. If the osteotomy healing was satisfying, the patient did a weight-bearing test, i.e. walking (with or without crutches) for an extended period of time varying from some hours to some days without the fixation but still with the pins in situ. If no symptoms arouse, the pins were removed at the out patient clinic. If the patient developed symptoms, the fixation was applied again for another 2–4 weeks and the healing control was repeated.
Study design
The patients were informed about the study during the preoperative visit and gave their written consent to participate. Patient characteristics were obtained prior to surgery. The postoperative HKA-angle was documented when the correction was finalized. Questionnaires for evaluation of physical activity and working activity as well as the disease-specific questionnaire were filled in and returned in a prepaid envelope before surgery preoperatively and at the 2- and 10-year follow-ups. At the 10-year follow-up, questions on satisfaction were added. The dates of conversion to knee arthroplasty during the 10-year follow-up were obtained through the Swedish Knee Arthroplasty Register (SKAR).
Outcome measures
Level of physical activity
Level of physical activity was assessed with regard to working activity and leisure activities [16]. Working activity was assessed as working, retired, unemployed or on sick leave. Leisure activities were reported on a scale from 0 to 6: (0) no household work: TV and reading only; (1) minimal household work, card games, sewing; (2) light yard work, light household work, shopping; (3) heavy yard work, heavy household work; (4) golf, dancing, hiking, water aerobics; (5) recreational sports; and (6) competitive sports. Preoperatively, the patients were asked to recall their level of physical activity during childhood to young adults as well as the year before surgery.
The Knee injury and Osteoarthritis Outcome Score (KOOS)
The KOOS [16, 17] was used as clinical outcome. KOOS was developed to be used for short- and long-term follow-up studies of knee injury and knee OA and comprises five subscales: pain, symptoms, activities in daily living (ADL), sport and recreational function (Sport/rec) and knee-related quality of life (QoL). The KOOS subscale sport and recreational function includes questions that assess more demanding functions such as kneeling, squatting, jumping and running. Standardized answer options are given (five Likert boxes), and each question gets a score from 0 to 4. A score from 0 to 100 is calculated for each subscale; 100 represent no problems. A difference of 8–10 points is considered a clinically significant difference [18].
Satisfaction
At the 10-year follow-ups, the patients were asked about their satisfaction with the surgery in general and in sport and recreational function especially. The responses were graded on a five-point Likert scale from “totally satisfied” to “very dissatisfied”.
The study was approved by the Ethics Committee of the Medical Faculty, Lund University (LU565-01) and was performed in accordance with the Declaration of Helsinki.
Statistics analysis
During the 10-year follow-up, patients were excluded due to reasons such as death, conversion to knee arthroplasty and lost to follow-up. The 2- and 10-year data in those patients included at 10 years were evaluated. Only preoperative data are presented for those patients converted to a knee arthroplasty within the 10 years and those lost to follow-up at 10 years, respectively.
The results of the level of physical activity and working activity are given as numbers of patients for each of the follow-ups and presented in diagrams. The patients were defined as satisfied with the surgery in general and in sport and recreational function, respectively, if the answered “totally satisfied” or “fairly satisfied” being presented as numbers of patients. KOOS data are given in mean and standard deviation (SD). Changes between two postoperative measurements were assessed by Wilcoxon’s rank test for each of the five KOOS subscales. The level of significance was set to p < 0.05. To be considered as a difference between two measurements in KOOS subscales, the results should be statistically significant (p < 0.5) as well as clinically significant (≥8 points).
Results
The majority of the patients scheduled for the HCO suffered from medial knee OA, Ahlbäck [1] grades 2–3, with mean malalignment of 10°. All patients achieved an acceptable degree of correction (Table 1), and the median time in external fixation was 94 days (range 75–156).
During the childhood and as young adults, the majority of the patients recalled that they were physically active in competitive and recreational sports (level 6 and 5) and reported activities such as heavy yard work, heavy household work (level 3) preoperatively (Fig. 2), while 73/79 patients were working active (Fig. 3).
Leisure activities in 45 patients followed preoperatively until 10 years postoperatively. Comp sport: competitive sport; rec sports: recreational sports, golf, dance: golf, dancing, hiking, water aerobics; heavy: heavy yard work, heavy household work; light: light yard work, light household work, shopping; minimal: minimal household work, card games and sewing; no: no household work, only TV and reading
During the 10-year follow-up, 25 of the 79 patients (32 %) were converted to a total knee arthroplasty (TKA), with similar proportion of patients in varus (20/70) and valgus knees (3/9), with the majority (18 patients) being converted between 5 and 10 years. The median time between the HCO and the TKA was 84 months (range 10–120). As nine patients did not answer the questionnaires at the 10-year follow-up, 45 patients were available for follow-up over the 10-year period (Fig. 1).
Similar to the initial cohort of 79 patients, the remaining 45 patients were physically active mainly in heavy yard work and heavy household work (level 3) the year before the HCO and were working active.
Two years postoperatively, the patients had increased their physical activity level, showing that more than half of the patients were active in activities such as golf, dancing, hiking and/or water aerobics (level 4) (Fig. 2); however, a few more patients were retired (Fig. 3).
Ten years after the HCO, almost half of the patients were still active with golf, dancing, hiking and/or water aerobics (level 4) (Fig. 2), and more than half of the patients were retired (Fig. 3).
The 45 patients available for follow-up over the 10-year period reported statistically and clinically significantly improved knee-related pain, function and quality of life 2 years after the HCO compared to preoperatively that persisted at 10 years (Fig. 4). However, at the 10-year follow-up compared to the 2-year follow-up, the patients experienced more problems with pain, ADL function and quality of life (Fig. 4).
KOOS profile of the 45 patients followed preoperatively until 10 years postoperatively. KOOS = Knee injury and Osteoarthritis Outcome Score, ADL = activity in daily life, Sport/rec = sport and recreational function, QoL = quality of life. *Statistically and clinically significant differences preoperatively and 2 years postoperatively. **Statistically and clinically significant differences 2 years and 10 years postoperatively
Most of the patients were satisfied (“totally satisfied”, “fairly satisfied” or “slightly satisfied”) with the HCO surgery in general 10 years postoperatively, while almost half of the patients were satisfied with their sport and recreational function (Fig. 5).
Compared to the patients followed up over 10 years, those patients converted to TKA during the 10-year follow-up reported preoperatively statistically and clinically significantly worse knee-related pain, symptoms and ADL function. Nine patients were lost to follow-up at 10 years and were similar to those followed over 10 years with respect to patient’s characteristics (Fig. 6).
KOOS profile of preoperative mean scores and SD for patients included and followed up over 10 years, patients whom were converted to a TKA within 10 years and patients lost to follow-up, respectively. TKA = total knee arthroplasty, KOOS = Knee injury and Osteoarthritis Outcome Score, ADL = activity in daily life, Sport/rec = sport and recreational function, QoL = quality of life. *Statistically and clinically significant difference between the groups “included at 10 years” and “TKA within 10 years”
Discussion
The most important finding of the present study was that in the majority of the patients operated on by HCO for knee OA, the level of physical activity gained 2 years postoperatively compared to the year before surgery was to a certain extent maintained also at 10 years.
Considering the almost three times higher risk of revision of knee arthroplasty in patients <55 years (24 % for UKA and 9 % for TKA) than those 55 years and older [24], the younger patients have a longer expected lifetime and higher activity levels, and the demands on the operated knee are considerably greater in the younger than in the older patients. The revision option after a TKA is another TKA that usually will be not as good as the primary one. We respectfully suggest that HTO delays the need of a knee arthroplasty in 70 % of the younger patients for at least 10 years which could be considered beneficial, a success and an excellent alternative to knee arthroplasty.
Our study has some limitations in common with longer-term follow-up studies, evaluating less common interventions and thereby relatively small study populations.
HTO is the least commonly used alternative in the knee reconstruction surgery for OA in Sweden. The present study is a single-centre study resulting in relatively few patients left to evaluate after 10 years. One-third of the patients included in our study had been converted to knee arthroplasty within 10 years and that is in line with the findings in earlier published population-based studies from Sweden [25] and Finland [10], showing that the 10-year risk of revision was approximately 30 %. However, there are some publications including at least 100 patients, showing rates of revision at 10 years between 5 and 20 % [4–6, 12, 22]. The reasons for these discrepancies may be differences in study size, loss to follow-up, patient selection or other factors. The above-mentioned population-based study also showed that the risk of revision increased by increasing age which as well is in line with our findings in the present study was that the patients converted to a knee arthroplasty were somewhat older than those followed for 10 years. The nine patients lost to follow-up seemed to be similar preoperatively to those evaluated at 10 years. In a recently published 10-year follow-up, study from Australia including 100 patients operated on with the closed-wedge osteotomy showed that BMI > 30 was unfavourable [6]. However, the BMI may have changed over time, and the BMI 10 years later or at the time for conversion to an arthroplasty may be as interesting as the preoperative BMI.
Patients not converted to a knee replacement and follow-up during a 10-year period after HCO for OA improved their physical activity level 2 years postoperatively compared to the year before surgery and were still working active. A good half of the patients maintained their activity level after 10 years, and another good half were retired. Although about two-thirds of the patients were not satisfied with their sport and recreational function at 10 years postoperatively, the majority of the patients were satisfied with the HCO surgery in general. Bonnin et al. [3] asked active and motivated patients whether the HTO could match their expectations after 4 years and a good half of the 136 patients reported that they were as active as they expected to be before the intervention and almost all of them were satisfied.
The HCO results in reduced pain and improved function in patients with knee OA 2 years after surgery have been shown earlier [23]. The present study shows that these improvements can persist 10 years postoperatively. However, the patients reported more problems with pain, ADL function and quality of life over time compared to the 2-year follow-up which may not be remarkable as the patients still have their OA disease and getting older.
According to a report from the Swedish Sport Association, about 40 % of the Swedes in corresponding age groups are active in some kind of moderate recreational or sport activity three times a week. Reference data from KOOS in the same age groups [15] show that our study population reaches comparable results 2 years postoperatively with respect to pain, other symptoms and ADL, but worse results in sport and recreation function as well as knee-related quality of life. However, despite the good clinical results after HCO, it could be questioned whether the patient’s expectations of surgical treatment of severe knee OA on sport and recreations activities should be based on or compared with knee healthy individuals.
Odenbring et al. [11] studied whether younger or more active middle-aged patients (mean age 42 years) with Ahlbäck grade I knee OA were able to return to an active lifestyle and even sports 11 years after HTO and found that 1/3 of the patients were able to manage high-activity sports or heavy work. On the other hand, Salzmann et al. [20] studied whether active patients (mean age 41 years) with painful and mild knee OA were able to resume sporting activities approximately 3 years after surgery and concluded that HTO allowed patients to return to sport and recreational activities similar to the preoperative level. In more age-comparable studies, Bonnin and his colleagues [3] showed that motivated patients were able to resume strenuous activities following HTO after in mean 4 years in a population with a mean age of 59 years (range 24–80) at the time for evaluation. Saragaglia et al. [21] evaluated the resumption of physical activity and sports after in mean 6 years in patients mean age of 50 years (range 32–67) and concluded that knee osteotomies for OA allow the resumption of sustained physical activity such as jogging or skiing downhill in a majority of patients.
The study population differed in terms of age and severity of OA to the studies by Odenbring [11] and Salzmann [19] as we have studied patients in average 10 years older and with a more severe grade of knee OA. Also the indications for surgery may be different in the studies by Salzmann et al. [20] and Saragaglia et al. [21] when the purpose was to study whether the patients were able to resume sporting activities after HTO. Considering that non-operated knee OA causes successively increasing disabilities that affect the ability to participate in high-demanding activities, the expectations of HTO may not be primarily to participate in such activities. Such high-demanding activities are, however, a short-term benefit which could increase the progression with less good longer-term outcome.
The OA patients are healthy but disabled. Bonnin et al. [3] pointed out that HTO patients must be informed that they will typically not recover their pre-pathology level and that residual pain during strenuous sports is not exceptional. Surgeries with HTO or knee arthroplasty are alternatives when non-surgical treatment no longer works and pain and functional disabilities affects their working, leisure and ADL ability. Even if sport and recreational activities are important for many individuals, increasing disabilities probably change their lifestyle to less demanding activities long before surgery is an alternative. Even if tennis, downhill skiing, hiking, etc., can be demanding activities that can be performed in different levels depending on skill and physical capacity which makes activities scales difficult to use in a comparative way. Therefore, activity scales may also include time and effort needed.
There is no evidence-based knowledge considering sport and recreation activities in patients who had knee replacement surgery. There are only case presentations on patients that can perform high-demanding activities and great performances such as long cross-country skiing competitions, competitive sports and running marathons. Therefore, we have no scientific comparative knowledge at all regarding the most common surgical procedure for knee OA. Clearly these few patients do not represent the average middle-aged knee OA patient. Patients performing these activities have a physical capacity, knowledge and experience of exercise and training and not at least, probably a motivation over the average.
Conclusion
The results indicate that HCO for knee OA is an option for selected patients that improve the level of physical activity in the early postoperative course and gives the possibility to be working active until retirement. One-third of the patients were converted to TKA mainly after 5–10 years. For the remaining patients, there was a mild deterioration of the results over time. The results of the study can be used to give the patients’ realistic expectations of the treatment.
References
Ahlback S (1968) Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn 277(Suppl):7–72
Bode G, von Heyden J, Pestka J, Schmal H, Salzmann G, Südkamp N, Niemeyer P (2013) Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2762-y
Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E (2013) Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc 21(1):64–73
Flecher X, Parratte S, Aubaniac JM, Argenson JN (2006) A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 452:91–96
Gstottner M, Pedross F, Liebensteiner M, Bach C (2008) Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg 128(1):111–115
Howells NR, Salmon L, Waller A, Scanelli J, Pinczewski LA (2014) The outcome at ten years of lateral closing-wedge high tibial osteotomy: determinants of survival and functional outcome. Bone Jt J 96-B(11):1491–1497
Lind M, McClelland J, Wittwer JE, Whitehead TS, Feller JA, Webster KE (2013) Gait analysis of walking before and after medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):74–81
Magyar G, Toksvig-Larsen S, Lindstrand A (1998) Open wedge tibial osteotomy by callus distraction in gonarthrosis: operative technique and early results in 36 patients. Acta Orthop Scand 69(2):147–151
Magyar G, Ahl TL, Vibe P, Toksvig-Larsen S, Lindstrand A (1999) Open-wedge osteotomy by hemicallotasis or the closed-wedge technique for osteoarthritis of the knee: a randomised study of 50 operations. J Bone Jt Surg Br 81(3):444–448
Niinimäki TT, Eskelinen A, Mann BS, Junnila M, Ohtonen P, Leppilahti J (2012) Survivorship of high tibial osteotomy in the treatment of osteoarthritis of the knee: finnish registry-based study of 3195 knees. J Bone Jt Surg Br 94(11):1517–1521
Odenbring S, Tjornstrand B, Egund N, Hagstedt B, Hovelius L, Lindstrand A, Luxhoj T, Svanstrom A (1989) Function after tibial osteotomy for medial gonarthrosis below aged 50 years. Acta Orthop Scand 60(5):527–531
Odenbring S, Egund N, Knutson K, Lindstrand A, Larsen ST (1990) Revision after osteotomy for gonarthrosis: a 10–19-year follow-up of 314 cases. Acta Orthop Scand 61(2):128–130
Osti M, Gohm A, Schlick B, Benedetto KP (2013) Complication rate following high tibial open-wedge osteotomy with spacer plates for incipient osteoarthritis of the knee with varus malalignment. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2757-8
Pape D, Kohn D, van Giffen N, Hoffmann A, Seil R, Lorbach O (2013) Differences in fixation stability between spacer plate and plate fixator following high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):82–90
Paradowski PT, Englund M, Roos EM, Lohmander LS (2004) Similar group mean scores, but large individual variations, in patient-relevant outcomes over 2 years in meniscectomized subjects with and without radiographic knee osteoarthritis. Health Qual Life Outcomes 2:38
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and osteoarthritis outcome score (KOOS)–validation of a Swedish version. Scand J Med Sci Sports 8(6):439–448
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and osteoarthritis outcome score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):88–96
Roos EM, Roos HP, Lohmander LS (1999) WOMAC Osteoarthritis index–additional dimensions for use in subjects with post-traumatic osteoarthritis of the knee: Western Ontario and MacMaster Universities. Osteoarthritis Cartilage 7(2):216–221
Roos EM, Lohmander LS (2003) The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Salzmann GM, Ahrens P, Naal FD, El-Azab H, Spang JT, Imhoff AB, Lorenz S (2009) Sporting activity after high tibial osteotomy for the treatment of medial compartment knee osteoarthritis. Am J Sports Med 37(2):312–318
Saragaglia D, Rouchy RC, Krayan A, Refaie R (2014) Return to sports after valgus osteotomy of the knee joint in patients with medial unicompartmental osteoarthritis. Int Orthop 38(10):2109–2114
Spahn G, Hofmann GO, von Engelhardt LV, Li M, Neubauer H, Klinger HM (2013) The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 21(1):96–112
W-Dahl A, Toksvig-Larsen S, Roos EM (2005) A 2-year prospective study of patient-relevant outcomes in patients operated on for knee osteoarthritis with tibial osteotomy. BMC Musculoskelet Disord 6:18
W-Dahl A, Robertsson O, Lidgren V (2010) Surgery for knee osteoarthritis in younger patients. Acta Orthop 81(2):161–164
W-Dahl A, Robertsson O, Lohmander LS (2012) High tibial osteotomy in Sweden, 1998–2007: a population-based study of the use and rate of revision to knee arthroplasty. Acta Orthop 83(3):244–248
van Egmond N, van Grinsven S, van Loon CJ, Gaasbeek RD, van Kampen A (2014) Better clinical results after closed- compared to open-wedge high tibial osteotomy in patients with medial knee osteoarthritis and varus leg alignment. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3303-z
Zaki SH, Rae PJ (2009) High tibial valgus osteotomy using the Tomofix plate–medium-term results in young patients. Acta Orthop Belg 75(3):360–367
Acknowledgments
This study was partly founded by the Swedish National Centre for Research in Sports.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
W-Dahl, A., Toksvig-Larsen, S. & Lindstrand, A. Ten-year results of physical activity after high tibial osteotomy in patients with knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 25, 902–909 (2017). https://doi.org/10.1007/s00167-015-3693-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3693-6