Abstract
Purpose
There has been increasing interest in accelerated programs for knee arthroplasty. We examined the efficacy and safety of an outpatient surgery (OS) pathway in patients undergoing unicompartmental knee arthroplasty (UKA).
Methods
This case–controlled study evaluates patients operated for UKA in an OS pathway (n = 20) compared to rapid recovery (RR), the current standard (n = 20). We investigated whether patients could be discharged on the day of surgery, resulting in comparable or better outcome by means of adverse events (AEs) in terms of pain (numerical rating scale, NRS), incidences of postoperative nausea and vomiting (PONV) and opiate use (<48 h postoperatively), complication and readmission rates (<3 months postoperatively). Patient-reported outcome measures (PROMS) were obtained preoperatively and 3 months postoperatively.
Results
Postoperative pain (NRS > 5) was the most common reason for prolonged hospital stay in the OS pathway. Eighty-five per cent of the patients were discharged on the day of surgery, whereas 95 % of the patients were discharged on postoperative day 3 in the RR pathway. Overall, median pain scores in both pathways did not exceed a NRS score of 5, without significant differences (RR vs. OS) in the number of patients with PONV (4 vs. 2) and opiate use (11 vs. 9) <48 h postoperatively. At 3 months postoperatively, no significant differences were found for AEs and PROMS between both pathways.
Conclusion
The results of this study illustrates that an OS pathway for UKA is effective and safe with acceptable clinical outcome. Well-established and adequate standardized protocols, inclusion and exclusion criteria and a change in mindset for both the patient and the multidisciplinary team are the key factors for the implementation of an OS pathway.
Level of evidence
Case–control study, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Care pathways in orthopaedic surgery are designed to prepare and optimize patients before, during and after surgery. These pathways improve the quality of the patient’s care ensuring reduction of surgical stress, PONV and pain [16–19, 21], with increased patient satisfaction whilst reducing the length of stay [17]. Slowly but surely, orthopaedic surgeons are convinced of revolutionary changes on evidence-based interventions within the elective knee arthroplasty [16–19, 21]. Success requires the implementation of a clear pathway applying a selected number of scientifically supported procedures, used together and implemented in a multimodal care pathway [15, 19, 20, 33]. Outpatient surgery (OS) pathways are designed for patients initiated for elective surgery on the day of admission into the hospital with a planned discharge, without an overnight stay in a hospital bed [32]. OS is commonly used for small elective surgical procedures, but may be used for more complex and challenging cases. For example, knee arthroplasty, which is more common in the USA than in Europe [31].
Due to the ageing of the population and the implantation of prosthesis in younger patients, the number of knee joint replacement surgeries in Western countries is increasing strongly [26]. The number of joint arthroplasties in the USA in 2006 was estimated at 600,000 operations [9]. This number of operations will even increase with 134 % in 9 years [23]. Due to the advancement of multidisciplinary pathways, outpatient UKA is allowing more surgical procedures to be performed; a cost reduction should be possible [3, 30]. On the other hand, health care organizations create strategies to decline the use of resources, with the preservation of the quality of care [27].
In 2011, optimization of the conventional pathway [28] resulted into an enhanced recovery pathway for knee arthroplasty. After years of experience, this optimization resulted in an OS pathway for UKA. OS is accomplished by a patient-specific approach, an optimized process in which the individual proactive patient is essential. Recent literature supports early discharge on the day of operation [4, 8, 10, 13, 22]. Published results on outpatient knee arthroplasty are rare and only consist of papers from the USA. Europe is more conservative to change care pathways and/or health care systems. At the moment, optimized enhanced recovery programs still need to be implemented in most of the orthopaedic departments around Europe, since the literature on enhanced recovery for knee arthroplasty mostly included the literature from the Scandinavian countries.
Further research needs to be done to emphasize the effectiveness and safety of outpatient pathways in patients undergoing UKA with the use of generally applicable protocols.
A case-controlled pilot study was performed over the first 20 consecutive cases operated in an OS pathway; these results were compared with a control group operated in a conventional enhanced recovery pathway (RR). We investigated whether patients could be discharged on the day of surgery as scheduled, resulting in comparable or better outcome by means of adverse events (AEs) and patient-reported outcome measurements (PROMS).
Materials and methods
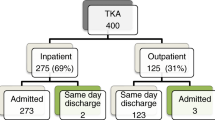
All patients were informed and consented to providing data for anonymous use. Between December 2013 and June 2014, 34 patients with indication for primary UKA [29] were potential candidates to participate in the OS pathway. Patients with severe cardiologic, pulmonary and/or internal diseases were excluded. These patients required an overnight stay for additional treatment pre-, peri- and postoperative for adjustment of medication (e.g. diabetes mellitus (DM), bridging anticoagulation). Patients who were not able to understand and complete the procedure due to cognitive dysfunction, fear to follow the outpatient procedure, or those who could not be discharged to their home environment were also excluded (Fig. 1). Twenty patients were eligible candidates to participate in the OS pathway. If patients were excluded from the OS pathway, they were treated in the RR pathway as the standard pathway in our department for hip and knee arthroplasty.
Pathways
Within OS, a personal coach (a relative) indirectly reduces the workload on the ward, by involvement as much as possible, to inspire, correct and support the patient during inpatient and outpatient for the first 48 h postoperatively.
Patients received preoperative education and exercise training, to become familiar with walking (stairs) with crutches and transfers from bed to a chair and vice versa, information about the inpatient and outpatient process and home-based rehabilitation.
All surgeries were performed with the use of patient-specific pin guides (Signature, Biomet, Warsaw INC) and tourniquets by a single experienced knee arthroplasty surgeon (NK). Patients received the (un-)cemented Oxford phase III UKA (Biomet, Bridgend, UK). Prophylactic antibiotics (2 g Cefazolin) were administered 30 min before incision. A second dose (1 g Cefazolin) was administered before discharge. The third dose (300 mg Cedax) was taken orally the first postoperative morning at home. Patients were operated under general or spinal anaesthesia. Local infiltration analgesia (LIA) was used intraoperative according to Kerr and Kohan [21]. In order to prevent PONV, dexamethasone was used intraoperative (8 mg iv). Tranexamic acid (dose 1 g if weight <100 kg, 1.5 g if weight >100 kg) was provided intravenously at wound closure. No drains or urinary catheters were used. Urinary retention was tested with the use of a bladder scan (Verathon®, BVI 9400). A compression bandage was used to reduce knee swelling [7] and to increase the effect of the LIA [1] during the first 8 h postoperative and was removed before discharge. Cooling by ice packs, to cope with knee swelling, was advised within the first 24 h postoperatively. An optimized and opioid sparing-pain protocol was provided (Table 1). As rescue pain medication, tramadol 50 mg was administered (max. 2 times daily). If the patient still suffered from high pain intensity while still in hospital after tramadol, 15 mg of dipidolor was injected intramuscularly (max. 6 times daily).
The first mobilization was attempted within 4–6 h postoperatively, including transfer from the bed to a chair, standing and walking with a walker if possible. If necessary in their home environment, walking stairs with crutches were practiced before discharge. Patients received instructions for self-administering subcutaneous syringes for thrombosis prophylaxis (Fondaprinux 2.5 mg, Arixtra®, GlaxoSmithKline) administered once each evening for 35 days, starting at 22:00 p.m. directly postoperative. After discharge, physiotherapy in their home environment was started 14 days postoperatively. All patients were seen at the outpatient clinic on days 4 and 14, and at the 6 weeks and 3 months postoperatively.
Patients were briefed on the overall discharge criteria (dry wound, general well-being, independent mobilization with crutches and if necessary walking stairs with crutches). The ward physician examined the discharge criteria. If there was any deterioration or a lack of progress in the function, the operating surgeon was consulted. All patients were contacted by telephone the first day after discharge by the ward physician.
Twenty patients without severe cardiologic, pulmonary, internal diseases, and/or cognitive dysfunction, who had been operated on by the same surgeon between December 2011 and November 2012 for UKA following the RR pathway, were randomly selected from this cohort (n = 79). Beside the differences between both pathways as summarized in Table 2, pre-, peri- and postoperative procedures and pain protocol were identical in both groups as well as the completed operative and clinical reports.
Outcome
AEs were classified as patient related (e.g. pain, PONV), thrombo-embolic events (e.g. deep venous thrombosis; DVT) and wound disorders, surgical related (e.g. infection) and/or prosthesis related (e.g. loosening). Experienced pain, measured by a Numerical Rating Scale (NRS, 0–10, 10 being ‘worst pain’), and incidences of PONV were evaluated during the first 48 h postoperatively. If pain or PONV was reason for delayed first mobilization and/or prolonged hospital stay, it was recorded in the patient’s clinical report. All patients filled in a diary on if they were affected with (extreme) pain and/or PONV. All AEs and readmissions to the hospital were recorded throughout the entire study period of 3 months postoperatively. Length of hospital stay was evaluated as time between hospital admission and discharge in days. Early mobilization (hours) was recorded as time between the start of anaesthesia until the first mobilization. PROMS were obtained preoperatively and 3 months postoperatively including the Dutch validated Oxford knee score (OKS; 12–60, 12 being the best outcome) [14] and EuroQol-5D (EQ-5D; 0–1, 1 indicates the best health state) [6].
This case-controlled study was performed in compliance with the Helsinki Declaration of 1975, as revised in 2000, and was studied and approved by the local Institutional Review Board (IRB: Atrium-Orbis Zuyd, Heerlen, The Netherlands, IRB Nr. 14-N-52) and registered online at the Dutch Trial Register (www.trialregister.nl, Nr. NTR4579).
Statistical analysis
The primary outcome of this case–control pilot study was to investigate whether UKA patients can go home as scheduled on the day of surgery. Sample size calculations were performed based on the results with two different pathways we used before implementation of the OS pathway: Joint Care [28] and RR (see materials and methods). Ten randomly selected patients (Joint Care) undergoing elective UKA had a mean (SD) hospitalization of 3.7 (1.17) days. The mean (SD) hospitalization of 10 other random selected patients, who followed the RR pathway, was 2.6 (0.97) days. With an alpha of 0.05 and 1-beta error of 0.8, an expected reduction of 1.6 days in the OS group, we would need 18 patients, 20 taking into account if assumed that both groups have the largest SD (1.17). This study included 40 patients, 20 in each arm. Statistically significant differences between both groups were analysed with nonparametric Mann–Whitney U test, since data were not normally distributed as tested with the Shapiro–Wilk test. Chi-square tests were used for categorical variables. p values were considered to be statistically significant at p ≤ 0.05 for all analysis. All statistical analyses were done with use of SPSS version 17.0 for windows (Inc., Chicago, IL). Results are presented as either with frequencies (%), mean (SD) or median (range).
Results
Forty patients were recruited for this study, 20 patients in each group. No patients were lost to follow-up. Baseline demographics and operative data are summarized in Table 3. All patients were discharged to their home environment, accompanied by a personal coach or relative.
Seventeen patients (85 %) in the OS pathway were discharged on the day of surgery as scheduled, whereas in the RR pathway 95 % of the patients were discharged <3 days postoperatively. Prolonged hospital stay was not significantly different. Three patients in the OS pathway had a prolonged hospital stay; 2 patients suffered from high pain intensity (NRS > 5), and both were discharged on postoperative day 2, as 1 other patient had a fear to go home and was discharged on postoperative day 1. In the RR pathway, 1 patient was suspicious for a DVT, and therefore, discharge was delayed (discharged on postoperative day 3). However, DVT was not diagnosed with echo duplex.
Early mobilization was comparable between the RR and OS pathways (n.s.). In both pathways, 1 patient was not able to mobilize due to high pain intensity <6 and <4 h, respectively. Delayed first mobilization occurred in 1 patient (RR) because of PONV, as another patient in the RR pathway had to cope with vasovagal syncope. Time between hospital admission and discharge was significantly different (p < 0.00) between both pathways: 2.6 days (1.2–4.1) in the RR pathway compared to 0.5 day (0.4–2.2) in the OS pathway. NRS pain scores were not significantly different preoperatively and <48 h postoperatively, measured on fixed time points throughout the day. Overall, median postoperative pain scores did not exceed a NRS score of 5 during the first 48 h (Fig. 2).
Distribution of median, first and third percentiles and range for NRS pain scores (Y axis) for both pathways (RR rapid recovery, OS outpatient surgery) measured preoperative (Pre OR), before (BFM)- and after (AFM) the first mobilization, at 16:00 and 22:00 h and on days 1 and 2 at 8:00, 16:00 and 22:00 h (X axis). Minimum and maximum are displayed with the whiskers
There were no significant differences (RR vs. OS) in the number of patients with PONV (4 vs. 2) and opiate use (11 vs. 9) <48 h postoperatively. AEs occurred only in one patient in the OS pathway. This patient was readmitted <3 months postoperatively. The patient did not follow instructions for home-based physiotherapy during the first 6 weeks postoperatively and suffered from knee stiffness resulting in a limited knee flexion of 30°. This required manipulation under anaesthesia after which the patient recovered completely. At 3-month follow-up, the mean (SD) OKS and EQ-5D significantly (p < 0.05) improved within each pathway, from 35.2 (8.1) to 22.7 (6.5) and 0.77 (0.1) to 0.85 (0.1) for the RR pathway and 32.0 (7.5) to 24.4 (7.6) and 0.75 (0.1) to 0.85 (0.1) in the OS pathway. There were no significant differences between both pathways.
Discussion
The most important findings of the present study was that outpatient unicompartimental knee arthroplasty is effective and safe with good short-term clinical results in selected patients, with comparable outcomes as patients operated in a conventional pathway.
Only six papers studied the feasibility of an outpatient pathway for knee arthroplasty of which the methodological evidence was poor (Table 4). These papers have considerable limitations including poorly presented details of their cohorts [4, 10, 13, 22]. For example, only four studies provided data on inclusion and exclusion criteria and only the study of Kolisek et al. [22] included a control group. However, they all reported comparable outcome without significant worsened results, in terms of AEs, readmission rates and prolonged hospital stay. This paper presents the preliminary results on elective UKA in an OS setting in the Netherlands.
There are some contradictions about the definition of OS. Kolisek et al. [22] aimed to discharge patients <23 h after surgery. As presented by the WHO [32], OS is defined as admission and discharge on the day of surgery, without an overnight stay in the hospital. Berger et al. [4, 5] operated patients in an outpatient pathway as the first surgeries of the day [5] or before noon [4]. Their pain protocol allows sufficient time for postoperative pain control. Therefore, these organizational aspects should be taken into account in order to prevent a prolonged hospital stay.
Our results show that it is effective and safe to operate selected patients in an outpatient UKA pathway, as 85 % of all the UKA patients were discharged on the day of surgery as scheduled, without increased AEs and readmission rate as compared to our conventional pathway. This was in line with our expectations and with previously published results by others, who also studied the feasibility and safety of outpatient knee arthroplasty (Table 4). Cross et al. [8] reported that 100 % of the patients operated for UKA (n = 105) were directly discharged home on the day of surgery. Slightly less (93 %) were discharged on the day of surgery with total knee arthroplasty (TKA) compared to 96 % of the patients operated for UKA [4]. Recently, Gondusky et al. [13] published their prospective study comparing UKA patients in a pathway with a planned overnight stay (n = 47) and one with a planned discharge on the day of surgery (n = 160). They found that 100 % of the patients were able to return home the evening of the day of surgery.
In our series, high pain intensity was the main factor for an overnight stay in our hospital. Berger et al. [4] found that 3.6 % of the TKA patients could not be discharged on the day of surgery due to inadequate pain control. Pain management is one of the key factors for acceptable outcomes of multidisciplinary outpatient pathways [4]. This includes a well-established multimodal protocol, consisting perioperative LIA [3, 12] and an optimized pain protocol for pre-, peri- and postoperative analgesia.
The optimized pain protocol also intended to prevent side effects of medication, which enables patients to mobilize <4 h postoperatively. Only one patient (RR) could not mobilize due to PONV. As we know, these preventions are crucial for early mobilization [11] and length of hospital stay [25]. Our discharge results could be influenced by the use of tranexamic acid and dexamethasone in the OS pathway, since there is extensive literature on the advantages of using these medications during arthroplasty procedures in the prevention of blood loss [34] and PONV [2]. This could be seen as a confounder in our series, although none of the patients in the OS and RR pathways needed blood transfusion or had a prolonged hospital stay due to wound leakage. Even though the amount of patients with PONV was lower in the OS pathway without a significant difference, another possible reason for prolonged hospital stay is fear to go home, as found by Berger et al. [4]. Therefore, fear to go home must be included as exclusion criteria for the OS pathway, which was seen in one patient in the OS pathway, resulting in prolonged hospital stay with discharge the first day postoperatively. Other causes that can delay discharge are administrative failures [3, 30] but were not seen in our series.
AEs and readmission rates were not significantly different between both groups. This was in line with the results published by others (Table 4). More complications <1 week postoperatively were seen after TKA rather than UKA during the outpatient procedure [4]. Previous series published by Berger et al. [5] showed fewer complications for outpatient TKA, in which they used more stringent inclusion criteria. Recently, Lovald et al. [24] concluded that pre-existing comorbidities and particularly heart failure are major risk factors for AEs after outpatient and short-stay TKA. Furthermore, evidence to include or exclude patients in an outpatient setting is limited. Besides the preselected patients in our series, based on general criteria, we suggest that there is a need for proper inclusion and exclusion criteria for outpatient knee arthroplasty.
This single surgeon, case-controlled pilot study, with a limited number of patients, could raise questions about the general applicability. We agree with Berger et al. [4], based on the experience with the use of clinical pathways, a stepwise implementation of an enhanced pathway, with the aim to discharge patients on the day of surgery, will be more effective and safe. Once these changes have been put in place, it will often be necessary to re-evaluate the new structures, to explore and extend the roles of the multidisciplinary team, to ensure optimal pre-, peri- and postoperative care. On the other hand, expansion of a day care surgery pathway involves an extensive change in mindset, both for patients and dedicated multidisciplinary team. Health care organizations and hospital management need to be convinced of the possibilities of optimized clinical pathways. With the use of simplified protocols and standards, which are applicable in every hospital, each hospital is able to reduce waiting periods and length of hospital stay [28]. This could result in lower costs, with comparable or improved patient satisfaction.
Obviously, there are some methodological limitations in order to say something about the AEs because of the small number of patients included in this study. These results might be inappropriate to use to conclude that the amount of AEs is comparable between both pathways. Further studies on AEs as an outcome with sufficient power and sample size are needed to assess whether these outcome measures differ between both pathways.
Finally, we recommend that further well-designed randomized controlled trials with larger patient series will be needed to confirm our preliminary results. After this, health care organizations and hospital management will probably be convinced of the need of optimized clinical pathways.
Conclusion
Well-established and adequate protocols, standardized general applicable inclusion and exclusion criteria and a change in mindset for both the patient and the multidisciplinary team are the key factors for the successful implementation of an outpatient surgical pathway for unicompartimental knee arthroplasty.
References
Andersen LØ, Husted H, Otte KS et al (2008) A compression bandage improves local infiltration analgesia in total knee arthroplasty. Acta Orthop 79(6):806–811
Backes JR, Bentley JC, Politi JR et al (2013) Dexamethasone reduces length of hospitalization and improves postoperative pain and nausea after total joint arthroplasty: a prospective, randomized controlled trial. J Arthroplasty 28(8 Suppl):11–17
Beard DJ, Murray DW, Rees JL et al (2002) Accelerated recovery for unicompartmental knee replacement—a feasibility study. Knee 9(3):221–224
Berger RA, Kusuma SK, Sanders SA et al (2009) The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res 467(6):1443–1449
Berger RA, Sanders S, Gerlinger T et al (2005) Outpatient total knee arthroplasty with a minimally invasive technique. J Arthroplasty 20:33–38
Brooks R (1996) EuroQol: the current state of play. Health Policy 37(1):53–72
Cheung A, Lykostratis H, Holloway I (2014) Compression bandaging improves mobility following total knee replacement in an enhanced recovery setting. J Perioper Pract 24(4):84–86
Cross MB, Berger R (2014) Feasibility and safety of performing outpatient unicompartmental knee arthroplasty. Int Orthop 38(2):443–447
Del Pozo JL, Patel R (2009) Clinical Practice. Infection Associated with Prosthetic Joints. New Engl J Med 361:787–794
Dervin F, Madden SM, Crawford-Newton BA et al (2012) Outpatient unicompartment knee arthroplasty with indwelling femoral nerve catheter. J Arthroplasty 27(6):1159–1165
Essving P, Axelsson K, Åberg E et al (2011) Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. Anesth Analg 113(4):926–933
Essving P, Axelsson K, Kjellberg J et al (2009) Reduced hospital stay, morphine consumption, and pain intensity with local infiltration analgesia after unicompartmental knee arthroplasty. Acta Orthopaedica 80(2):213–219
Gondusky JS, Choi L, Khalaf N et al (2014) Day of Surgery Discharge after Unicompartmental Knee Arthroplasty: an Effective Perioperative Pathway. J Arthroplasty 29(3):516–519
Haverkamp D, Breugem SJ, Sierevelt IN et al (2005) Translation and validation of the Dutch version of the Oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop 76(3):347–352
Husted H, Holm G (2006) Fast-track in total hip and knee arthroplasty–experiences from Hvidovre University Hospital, Denmark. Injury 37(5):31–35
Husted H, Lunn HT, Troelsen A et al (2011) Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthopaedica 82:679–684
Kehlet H, Andersen LØ (2011) Local infiltration analgesia in joint replacement: the evidence and recommendations for clinical practice. Acta Anaesthesiol Scand 55:778–784
Kehlet H, Dahl JB (2003) Anaesthesia, surgery, and challenges in postoperative recovery. Lancet 362:1921–1928
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248:189–198
Kerr DR, Kohan L (2008) Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery. A case study of 325 patients. Acta Orthopaedica 79:174–183
Kolisek FR, McGrath MS, Jessup NM et al (2009) Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res 467(6):1438–1442
Losina E, Thornhill TS, Rome BN et al (2012) The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 94(3):201–207
Lovald S, Ong K, Lau E et al (2014) Patient selection in outpatient and short-stay total knee arthroplasty. J Surg Orthop Adv 23(1):2–8
Munk S, Dalsgaard J, Bjerggaard K et al (2012) Early recovery after fast-track Oxford unicompartmental knee arthroplasty. 35 patients with minimal invasive surgery. Acta Orthopaedica 83(1):41–45
Ostendorf M, Johnell O, Malchau H et al (2002) The epidemiology of total hip replacement in The Netherlands and Sweden: present status and future needs. Acta Orthopaedica 73(3):282–286
Pearson SD, Goulart-Fisher D, Lee TH (1995) Critical pathways as a strategy for improving care: problems and potential. Ann Intern Med 123(12):941–948
Pilot P, Bogie R, Draijer WF et al (2006) Experience in the first four years of rapid recovery; is it safe? Injury 37(5):37–40
Price AJ, Webb J, Topf H et al (2001) Oxford Hip and Knee Group. Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16(8):970–976
Reilly KA, Beard DJ, Barker KL et al (2005) Efficacy of an accelerated recovery protocol for Oxford unicompartmental knee arthroplasty—a randomised controlled trial. Knee 12(5):351–357
Verma R, Alladi R, Jackson I et al (2011) Day case and short stay surgery: 2. Anesthesia 66:417–434
World Health Organization (2007) European observatory on health systems and policies; Day surgery: Make it happen
Wilmore DW, Kehlet H (2001) Management of patients in Fast-track surgery. BMJ 24(322):473–476
Zhang H, Chen J, Chen F et al (2012) The effect of tranexamic acid on blood loss and use of blood products in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 20(9):1742–1752
Conflict of interest
One author (NK) is a payed consultant for Biomet on the Signature surgical procedure. The other authors declare that they have no conflict of interest. No financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kort, N.P., Bemelmans, Y.F.L. & Schotanus, M.G.M. Outpatient surgery for unicompartmental knee arthroplasty is effective and safe. Knee Surg Sports Traumatol Arthrosc 25, 2659–2667 (2017). https://doi.org/10.1007/s00167-015-3680-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3680-y