Abstract
Purpose
The aim of the study was to make an anthropometric analysis at the resected surfaces of the proximal tibia in the Turkish population and to compare the data with the dimensions of tibial components in current use. We hypothesized that tibial components currently available on the market do not fulfil the requirements of this population and a new tibial component design may be required, especially for female patients with small stature.
Methods
Anthropometric data from the proximal tibia of 226 knees in 226 Turkish subjects were measured using magnetic resonance imaging. We measured the mediolateral, middle anteroposterior, medial and lateral anteroposterior dimensions and the aspect ratio of the resected proximal tibial surface. All morphological data were compared with the dimensions of five contemporary tibial implants, including asymmetric and symmetric design types.
Results
The dimensions of the tibial plateau of Turkish knees demonstrated significant differences according to gender (P < 0.05). Among the different tibial implants reviewed, neither asymmetric nor symmetric designs exhibited a perfect conformity to proximal tibial morphology in size and shape. The vast majority of tibial implants involved in this study tend to overhang anteroposteriorly, and a statistically significant number of women (21 %, P < 0.05) had tibial anteroposterior diameters smaller than the smallest available tibial component.
Conclusion
Tibial components designed according to anthropometric measurements of Western populations do not perfectly meet the requirements of Turkish population. These data could provide the basis for designing the optimal and smaller tibial component for this population, especially for women, is required for best fit.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, total knee arthroplasty (TKA) is considered the treatment of choice in the advanced stages of knee osteoarthritis, particularly for its ability to provide function and pain relief. To achieve a successful outcome in TKA, aside from accurate bone cutting and adequate balancing of the soft tissues, maximizing tibial coverage with the correct component size is mandatory for minimizing the stress applied to the bone–implant interface and ensuring an appropriate load transmission [2, 16–18]. Thus, an anthropometrically well-designed knee prosthesis that matches properly to the resected surface of the bone is key for long-term survivorship in TKA [6].
Compared to the femoral side, the tibial component is more prone to complications in TKA [4]. If a tibial component does not match properly to the resected proximal part of the tibia, the surgeon may have to choose either a larger, overhanging component or a smaller, underhanging one [31, 32]. An underhanging tibial component in the mediolateral (ML) or anteroposterior (AP) planes may subside on the weaker cancellous bone eventually, especially if the postero-medial cortical area of the tibia is uncovered [2]. Subsidence of the tibial component leads to malalignment, increased wear instability and dissociation of prostheses in the long term [25, 32]. Conversely, a large tibial component that is overhanging, especially at the medial side, may cause soft tissue irritation and persistent knee pain after TKA [3, 5, 11, 22]. Although it remains unclear how much of a mismatch between the implant and the morphology of the knee might be tolerable [26], an optimal size component is essential to achieve both long-term survivorship and patient satisfaction [16, 32]. However, previous studies demonstrated that the current designs of contemporary components do not fit adequately with the anthropometric variety of different ethnic groups [7, 14, 15, 19, 27–29, 34, 35].
The problem is not only the size but also the shape of the component. The existing literature regarding tibial component shape is conflicting; it has yet to be decided which geometry of the tibial component provides superior long-term outcomes [9, 16, 20, 33]. In the current era, there is growing shift from the symmetric non-anatomical tibial component to the more anatomical component [26]. To maximize tibial coverage and achieve more cortical support, some authors advocate the use of asymmetric tibial components to mimic the asymmetry of the resected proximal tibia [9, 25, 33]. Additionally, in a recent study authors found the increased bony coverage when anatomical designs were used [10].
As with across the world, there is likely an increasing prevalence of TKA consumption in Turkish population. However, no data have been reported regarding the anthropometry of the proximal tibia for Turkish people, and to date, no study has evaluated whether commercially available tibial components completely fulfil the requirements of this population. Therefore, the aim of the present study was to evaluate the anthropometric data of the proximal tibial plateau of the Turkish population using magnetic resonance imaging (MRI), as well as to compare these measurements with the dimensions of commonly available tibial components.
Materials and methods
Morphologic data from the proximal tibia of 226 knees in 226 subjects were analysed, wherein one knee of each subject was studied (left or right, as chosen randomly). There were 138 women and 88 men, and the median age was 57.4 ± 7.4 years. They were recruited consecutively following approval by the institute review board and the collection of the informed consent from each subject. The study was approved by the institutional review board of BezmialemVakif University Hospital.
Subjects were first clinically observed and included in the study if they had a normal lower limb appearance and normal alignment, with no prior trauma or congenital deformities. Full-length standing radiographs of each subject were obtained, and mechanical axis was measured with a digital radiological system. The hip-knee angle coronal plane alignment of the subjects was 3.7° (5.1) varus. There were 41 healthy knees from normal volunteers, and 185 knees had radiographic evidence of grade I–II osteoarthritis according to Kellgreen and Lawrence classification, who were not TKA candidates. The exclusion criteria were patients with any deformity in the coronal and sagittal plane, lower extremity malalignment (metaphyseal varus/valgus >10°), knee flexion deformities >10°, substantial bone loss, history of previous surgery, proximal tibial fracture, or knees with any implants. Patients under the age of 50 years were also excluded. Because a CT scan packs a mega dose of radiation, MRI was preferred for the proximal tibial measurements in this study.
MRI measurements
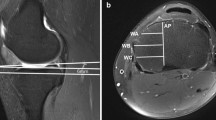
MRI images of each knee were obtained using a 1.5-Tesla MRI system (Siemens Magnetom Avanto 1.5 T, Siemens AG, Munich, Germany). During the scan, the subject was placed in the supine position on the table with the involved knee relaxed and stabilized in extended position in a leg holder. This position was maintained throughout the scanning procedure to minimize errors in measurements because of limb rotations. Axial, coronal and sagittal sections through the resection level of the proximal tibia and the epicondylar axis of the femur were obtained. Simulated proximal tibial resections and radiological measurements were virtually performed on each subject using a digital radiological system (NovaPACs Diagnostic Viewer, Utah, USA) with advanced capabilities for orthopaedic morphological analysis. With the guidance of multislice images on the digital radiological system, simulated resection levels and cutting thickness were determined (Fig. 1) and the simulated axial slices were taken perpendicular to the mechanical axis of the tibia with a 7° posterior slope from 8 mm below the highest point of lateral tibial plateau (Fig. 2).
As described previously [20, 27], a standardized protocol was followed to measure the proximal tibial dimensions. For the chosen slice, the ML and AP dimensions were calculated to evaluate the gross size of the proximal tibial surface. The ML dimension is a line drawn in the axial plane to the tibial cut surface, which is parallel to the epicondylar axis of the femur and is the longest mediolateral distance of the proximal tibia (Fig. 3). It is formed by a line between the lateral epicondylar prominence and the medial sulcus of the medial epicondyle, as described by Uehara et al. [27]. The AP line was drawn perpendicular to the ML line and passed through the mid-point of it. The AP dimensions of the medial and lateral tibial condyles were measured separately. The medial AP (MAP) size was considered the length of the line drawn parallel to the middle AP line, which passes through the posterior-most point of the medial tibial condyle. Similarly, the lateral AP (LAP) size was formed by the length of the line drawn parallel to the AP line, which passes through the posterior-most point of the lateral tibial condyle. The lengths of the MAP and LAP from the AP line were measured and named CM and CL, respectively. Subsequently, the tibial aspect ratios (ARs) were calculated. AR defines the ratio of the AP to the ML dimensions of the proximal part of the tibia, and it is expressed as a percentage (AP/ML × 100) [14].
All data were evaluated by one orthopaedic surgeon and one radiologist. Each parameter was measured two times in a randomly selected knee. The standard deviation of these two measurements was used to assess the repeatability of the measurements. Then, all collected data were compared with previous studies [ 14, 23, 27, 32]. To determine the optimal tibial component design for this population, all parameters were compared with currently available 4 symmetric and 1 asymmetric tibial base plates. Finally, the AR and its comparison with the ML dimension of the proximal tibia were calculated to estimate whether the tibial component shape is appropriate for the Turkish population.
Tibial component designs
The symmetric tibial components of Vanguard (Biomet, Warsaw, IN, USA), Sigma (DePuy Synthes Inc., Warsaw, IN, USA), Optetrak (Exactech Inc., Gainesville, FL, USA) and Nexgen (Zimmer Inc.,Warsaw, IN, USA), as well as the asymmetric tibial component of Genesis II (Smith & Nephew Inc., Memphis, TN, USA), were used for comparison. The AP and ML dimensions of these components were obtained from the manufacturers, and all the available sizes of each component design were used in the analysis. According to the manufacturers’ manuals, the medial or lateral AP diameters were taken into account for the symmetric implants, while the larger medial AP diameter was considered for Genesis II.
Statistical analysis
A sample size of 226 subjects was determined for this study. This sample size was larger than the table value of 200 (anticipated population proportion—30 %; confidence level = 95 %; absolute precision of 10 % points) [21, 30] and in keeping with previous studies that have investigated morphometry [15, 20, 24, 29, 36].
The SPSS software 16.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The dimensions were summarized as the mean and standard deviation. The independent sample t test and Pearson’s correlation coefficient were used to determine the significance of the differences between males and females. Descriptive statistics, an analysis of variance (ANOVA) and a Chi-square analysis were used for comparing implants and patients. P values of less than 0.05 were considered statistically significant.
Results
Measurements of proximal tibial dimensions are summarized in Table 1. Females had significantly smaller AP, ML, MAP and LAP dimensions than males (P < 0.001). Measurements indicated that the medial tibial plateau was larger than the lateral tibial plateau anteroposteriorly by an average of 8.0 mm for men and 7.6 mm for women (n.s.). In addition, the distance of the MAP (CM) and LAP (CL) lines from the AP line were measured, and MAP was found to be closer to the AP than LAP by an average of 4.4 mm in males and 2.8 mm in females (P < 0.01). These results confirm the asymmetric shape of the proximal tibial surface at the resection level in the Turkish population.
The majority of female knees were found to be matched with the smaller-size tibial components, while the males matched with the larger sizes. Additionally, for both genders, the AP sizes of all tibial implants tended to overhang for the given AP dimensions. In other words, the tibial components that matched properly with the AP dimension underhanged mediolaterally or the components that matched properly with the ML dimension were overhanged anteroposteriorly. The comparisons of the dimensions of the tibial components and of the average tibial dimensions of males and females are shown in Figs. 4 and 5. A statistically significant number of women (n = 29, 21 %, P < 0.001) had tibial AP dimensions smaller than the smallest available (38 mm) tibial component. Despite this inappropriate matching with the components involved in this study, the data set of the study population was found to be relatively more consistent with the dimensions of Vanguard and Optetrak prostheses compared to those of Sigma, Nexgen and Genesis II. However, this difference was not statistically significant (n.s.).
Proximal tibial ML and AP dimensions of females compared with the dimensions in five conventional tibial prostheses. The black line represents the median values for the female population. This graphic demonstrates that vast majority of the tibial components tended to be too large for Turkish women for a given AP dimension. Among these prostheses, Biomet design followed the population data most consistently compared to the others
A statistically significant difference was noted between the median ARs of females and males (P < 0.05). Additionally, the measurements demonstrated a progressive decline in the AR with an increase in the ML dimensions for both males and females, indicating that small knees were longer in the ML direction (P < 0.05). Through the comparison of the tibial components, we found that all prostheses followed a similar horizontal pattern with a minimal decrease in the AR, irrespective of gender. The shapes of five tibial components illustrating a progressive decrease in AR with an increasing AP dimension are shown in Figs. 6 and 7.
Proximal tibial aspect ratio and the ML dimension of male subjects compared with the dimensions of five conventional tibial prostheses. The line represents the median values for the male population. The Biomet and Exactech designs follow the declining aspect ratio more consistently as compared to the male population
Proximal tibial aspect ratio and the AP dimension of females compared with the dimensions of five conventional tibial prostheses. The line represents the median values for the female population. The population data show a progressive decrease in the aspect ratio with the increasing ML size of the knee, whereas most of the prostheses show a relatively constant aspect ratio
Discussion
The most important finding of the present study was that the MRI measurements of the proximal tibial plateau of the study population showed significant gender difference and mismatching with the dimensions of commonly available tibial components. Data from the current study indicate that males showed higher AP and ML dimensions than females with higher AR for the given ML dimension. In addition, most of tibial implants involved in this study tend to overhang anteroposteriorly and a significant number of females had tibial anteroposterior diameters smaller than the smallest available tibial component.
Although Turkish people have a similar build and stature compared with Western people [12], this population has its own anthropometric differences. Several studies have investigated the morphology of Asian knees and compared them with Western counterparts [7, 15, 28, 36]. To date, however, no data have been reported regarding the anthropometry of the proximal tibia among the Turkish population, and this is the first report, to our knowledge, on this topic.
This study resulted in several findings. First, measurements revealed that most females have significantly smaller dimensions at the simulated resection level of the proximal tibia than males do. This difference was expected and is similar to what has been reported previously [20, 23, 27, 34]. In the present study, most men (77 of 89) had an AP diameter range between 40 and 55 mm, whereas most women (107 of 138) ranged between 35 and 45 mm. The ML dimensions of the tibial component should focus on a length of 65–75 mm for women and 75–85 mm for men, considering that 90 % of knees fell into this range. Consequently, a tibial component with a size variation in the ML length of 65–85 mm and in the AP length of 35–55 mm is suitable for the majority of the Turkish population. When our measurement data were compared with the previously published data, the AP and ML lengths were found to be smaller than those in the Western population [23], but similar to those in the Asian-Pacific population [20, 27] (Table 2).
Second, the study measurements demonstrated that the medial tibial plateau was larger than the lateral tibial plateau in the Turkish population, irrespective of gender. This result indicates the asymmetric shape of the proximal tibial surface at the simulated resection level, which is consistent with previous reports [20, 27]. However, the existing literature regarding the use of the symmetric or asymmetric tibial components is conflicting. Some studies recommend using an asymmetric tibial component [9, 25, 33], whereas others prefer symmetric designs [16, 20]. Most of the currently available tibial components have a symmetric design. Nevertheless, if a symmetric component is placed on an asymmetric surface, it would inevitably cause either medial undersizing or a lateral overhang [20, 31]. An undersized symmetric component may cause an increase in contact stress and poor load transfer across its surface, and it would eventually result in subsidence if the implant is not resting on the harder cortical bone rim. On the contrary, a large symmetric component that is overhanging may cause soft tissue irritation and pain at the lateral compartment of the knee [5]. On the other hand, there has been no clear evidence of the functional advantage of using asymmetric components, even though an asymmetric tibial component appears to be theoretically beneficial in maximizing tibial surface coverage [1, 13]. Most recently, it is found that symmetric and asymmetric base plate designs provided similar levels of tibial bone coverage [8]. Furthermore, asymmetric tibial designs necessitate doubling the inventory and stock for the operating room due to the bilaterality of the required components, which means additional costs for the healthcare system. To solve the implant mismatch problem, anatomical tibial components, gender-specific prostheses, patient-specific prostheses or custom-made implants may offer promising solutions. This finding has been confirmed recently. An anatomical design tibial implant demonstrated a meaningful increase in tibial coverage with a minimal component overhang compared to symmetric and asymmetric designs [10]. Increasing the number of tibial component sizes may also improve tibial coverage independent of tibial morphology.
When the existing data were compared with the five conventional prostheses, it was found that the tibial components that matched properly with the AP dimension were undersized mediolaterally or the components that matched properly with the ML dimension were oversized anteroposteriorly. Overall, the vast majority of tibial components for women tended to be too large for a given AP dimension and a statistically significant number of women had a tibial anteroposterior diameter smaller than the smallest available tibial component. Thus, a smaller-sized tibial component design with a shorter AP dimension (<38 mm) is required, especially for female patients with small statures in the Turkish population. Although the aforementioned five prostheses currently available on the market do not fulfil the requirements of this population, according to our existing data, Vanguard and Optetrak were more closely matched to the proximal tibia than others, especially for males. Surprisingly, an asymmetric component (Genesis II) was less closely matched when compared to these two symmetric components. Although this finding demonstrates a difference, it was not statistically significant.
The AR is used to describe the shape of the anticipated tibial component [20]. According to this study, a lower AR was found for a larger ML dimension of the proximal tibia and a higher AR was found for a smaller ML dimension of the proximal tibia. This means that with every decrease in the ML dimension of the proximal tibia, the shape of the anticipated tibial component becomes more oval and with every increase in the ML dimension, it becomes less oval for use in the Turkish population. However, the majority of these components showed a relatively constant AR with an increase in the ML dimension, which leads to oversizing problems with the increasing ML dimensions of the proximal tibia in this population. Thus, a tibial component that is suitable for the Turkish population would be one whose AR decreased with an increase in the ML dimension.
There are limitations of this study that should be noted. In this study, the dimensions were measured at only one MRI level on the proximal tibia. Although measurements are based on the commonly accepted cut level and inclination degree, there is always a possibility of obtaining different lengths or clinical variability between different cut levels and inclination degrees. Anthropometric data of the simulated resection level may not be representative for the decisions intraoperatively such as increasing the resection depth or posterior slope to improve ligament balance. The lack of comparison with the data obtained during surgery in a similarly aged group of patients is another limitation. Although study subjects were recruited with a minimum age of 50 years, all the results in this study were based on healthy subjects or low-grade arthritis, not TKA candidates. However, the proximal tibial dimensions of knees in end-stage arthritic patients may be deformed and shaped quite differently when compared to non-arthritic or low-grade arthritic knees, and this may affect the size and the coverage of tibial components. It has been shown previously that arthritic knees are different from healthy ones, suggesting that prosthetic designs should be based on data from diseased knees [6, 24]. The impact of these limitations on the results may require further investigation.
As the number of TKA performed increases every year, understanding the morphological variety between different populations would guide surgeons when choosing the optimum component. This study revealed the anthropometric data of tibial plateau in the Turkish population and evaluated the conformity of contemporary tibial component designs. The clinical implications of the observations in the present study demonstrated that currently available tibial components do not perfectly meet the implant shape requirements of this population.
Conclusion
The results of this study provide anthropometric data of the proximal tibia in the Turkish population. These data can be used as a guideline to design a tibial component suitable for Turkish patients. In this population, especially in women, there is a need for a tibial component having an AP diameter of <38 mm, which is smaller than the currently available small tibial prosthetic sizes. We conclude that, as with many new advancements in arthroplasty technology, patient-specific prosthetic components may eradicate component mismatch in the near future.
References
Bindelglass DF, Dorr LD (1998) Symmetry versus asymmetry in the design of total knee femoral components-an unsolved controversy. J Arthroplasty 13:939–944
Bloebaum RD, Bachus KN, Mitchell W, Hofmann G, Hofmann AA (1994) Analysis of the bone surface area in resected tibia. Implications in tibial component subsidence and fixation. Clin Orthop Relat Res 309:2–10
Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E (2013) Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc 21(10):2314–2324
Canale ST (2003) Campbell’s operative orthopaedics, 10th edn, vol 1.Mosby, Philadelphia, p 292
Chau R, Gulati A, Pandit H, Beard DJ, Price AJ, Dodd CA, Gill HS, Murray DW (2009) Tibial component overhang following unicompartmental knee replacement-does it matter? Knee 16:310–313
Cheng CK, Lung CY, Lee YM, Huang CH (1999) A new approach of designing the tibial base plate of total knee prostheses. Clin Biomech 14:112–117
Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF, Fu YW, Li YQ (2009) Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee 16(5):341–347
Clary C, Aram L, Deffenbaugh D, Heldreth M (2014) Tibial base design and patient morphology affecting tibial coverage and rotational alignment after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(12):3012–3018
Crockarell JR Jr, Hicks JM, Schroeder RJ, Guyton JL, Harkess JW, Lavelle DG (2010) Total knee arthroplasty with asymmetric femoral condyles and tibial tray. J Arthroplasty 25(1):108–113
Dai Y, Scuderi GR, Bischoff JE, Bertin K, Tarabichi S, Rajgopal A (2014) Anatomic tibial component design can increase tibial coverage and rotational alignment accuracy: a comparison of six contemporary designs. Knee Surg Sports Traumatol Arthrosc 22:2911–2923
Dennis DA (2004) Evaluation of painful total knee arthroplasty. J Arthroplasty 19(4 Suppl 1):35–40
Güleç E, Akın G, Sagir M, Koca Özer B, Gültekin T, Bektaş Y (2009) Anthropometric dimensions of Anatolian people: results of 2005 Turkish Anthropometric Survey.[Article in Turkish]. Ankara Üniversitesi Dil ve Tarih-Coğrafya Fakültesi Dergisi 49:187–201
Harwin SF (1998) Patellofemoral complications in symmetrical total knee arthroplasty. J Arthroplasty 13:753–762
Hitt K, Shurman JR 2nd, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA (2003) Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am 85-A(Suppl 4):115–122
Ho WP, Cheng CK, Liau JJ (2006) Morphometrical measurements of resected surface of femurs in Chinese knees: correlation to the sizing of current femoral implants. Knee 13:12–14
Incavo SJ, Ronchetti PJ, Howe JG, Tranowski JP (1994) Tibial plateau coverage in total knee arthroplasty. Clin Orthop Relat Res 299:81–85
Insall JN (1993) Surgical techniques and instrumentation in total knee arthroplasty. In: Insall JN, Windsor RE, Scott WN et al (eds) Surgery of the knee, 2nd edn. Churchill Livingstone, New York, p 739
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Küçükdurmaz F, Tuncay I, Elmadağ M, Tunçer N (2014) Morphometry of the medial tibial plateau in Turkish knees: correlation to the current tibial components of unicompartmental knee arthroplasty. Acta Orthop Traumatol Turc 48:147–151
Kwak DS, Surendran S, Pengatteeri YH, Park SE, Choi KN, Gopinathan P, Han SH, Han CW (2007) Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee 14(4):295–300
Lwanga SK, Lemeshaw S (1991) Sample size determination in health studies: a practical manual. World Health Organization, Geneva
Mahoney OM, Kinsey T (2010) Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am 95:1115–1121
Mensch JS, Amstutz HC (1975) Knee morphology as a guide to knee replacement. Clin Orthop Relat Res 112:231–241
Puthumanapully PK, Harris SJ, Leong A, Cobb JP, Amis AA, Jeffers J (2014) A morphometric study of normal and varus knees. Knee Surg Sports Traumatol Arthrosc 22:2891–2899
Stulberg BN, Dombrowski RM, Froimson M, Easley K (1995) Computed tomography analysis of proximal tibial coverage. Clin Orthop Relat Res 311:148–156
Thienpont E, Becker R (2014) Anthropometric measurements of the knee: time to make it fit. Knee Surg Sports Traumatol Arthrosc 22:2889–2890
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. J Arthroplasty 17:1028–1032
Urabe K, Miura H, Kuwano T, Matsuda S, Nagamine R, Sakai S, Masuda K, Iwamoto Y (2003) Comparison between the shape of resected femoral sections and femoral prostheses used in total knee arthroplasty in Japanese patients: simulation using three-dimensional computed tomography. J Knee Surg 16:27–33
Vaidya SV, Ranawat CS, Aroojis A, Laud NS (2000) Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty 15:79–85
Wang D, Bakhai A, Del Buono A, Maffulli N (2013) Sample size determination for clinical research. Muscles Ligaments Tendons J 3:116–117
Westrich GH, Agulnick MA, Laskin RS, Haas SB, Sculco TP (1997) Current analysis of tibial coverage in total knee arthroplasty. Knee 4:87–91
Westrich GH, Haas SB, Insall JN, Frachie A (1995) Resection specimen analysis of proximal tibial anatomy based on 100 total knee arthroplasty specimens. J Arthroplasty 10:47–51
Wevers HW, Simurda M, Griffin M, Tarrel J (1994) Improved fit by asymmetric tibial prosthesis for total knee arthroplasty. Med Eng Phys 16:297–300
Yang B, Song CH, Yu JK, Yang YQ, Gong X, Chen LX, Wang YJ, Wang J (2014) Intraoperative anthropometric measurements of tibial morphology: comparisons with the dimensions of current tibial implants. Knee Surg Sports Traumatol Arthrosc 22:2924–2930
Yip DK, Zhu YH, Chiu KY, Ng TP (2004) Distal rotational alignment of the Chinese femur and its relevance in total knee arthroplasty. J Arthroplasty 19:613–619
Yue B, Varadarajan KM, Ai S, Tang Rubash HE, Li G (2011) Differences of anthropometry between Chinese and white men and women. J Arthroplasty 26(1):124–130
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erkocak, O.F., Kucukdurmaz, F., Sayar, S. et al. Anthropometric measurements of tibial plateau and correlation with the current tibial implants. Knee Surg Sports Traumatol Arthrosc 24, 2990–2997 (2016). https://doi.org/10.1007/s00167-015-3609-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3609-5