Abstract
Purpose
Hamstring tendons are commonly used as a graft source for ACL reconstruction. This study seeks to determine whether either the diameter of the tendon graft or the age of the patient influences the outcome of the ACL reconstruction when measured using a standard, previously validated laxity measurement device.
Methods
This is a retrospective study of 88 patients who underwent ACL reconstruction with a short, quadrupled tendon technique, using the semitendinosus ± gracilis tendons. Patients included in this study were sequential, unilateral, complete ACL ruptures. The patients were followed for a minimum of 1 year postoperatively, with a mean follow-up of 26 months. Patients were divided into three groups according to the diameter (Ø) of the graft: group 1 (32 patients): 8 mm ≤ Ø ≤ 9 mm; group 2 (28 patients): 9 mm < Ø ≤ 10 mm; and group 3 (28 patients): Ø > 10 mm. Three groups with differential laxity at 134 N (Δ134 = healthy side vs. operated side) measured with the laximeter GNRB® were compared. The risk of residual laxity (OR) between the three groups taking age, gender, BMI and meniscus status into account was calculated. A side-to-side laxity >3 mm was considered as a residual laxity.
Results
The mean patient age at the time of reconstruction was 29.4 years. The three groups were comparable. Postoperative Δ134 was 1.50 ± 1.3, 1.59 ± 1.5 and 2 ± 1.7 mm for groups 1 through 3, respectively. Δ134 > 3 mm was observed in three patients in group 1, four patients in group 2 and nine patients in group 3. As compared to group 1, OR was 1.46 (95 % CI 0.35–6.05) and 3.31 (95 % CI 0.89–12.34) in groups 2 and 3, respectively. Adjustment for age, gender, BMI and meniscus did not change the estimates [OR 1.44 (95 % CI 0.34–6.16) and 3.92 (95 % CI 1–15.37)] in groups 2 and 3, respectively. Patients younger than 20 had a significantly higher average postoperative laximetry (2.4 ± 1.5 mm) compared to those aged 20 years and over (1.5 ± 1.5 mm) (p = 0.03), regardless of the diameter of the graft.
Conclusion
The diameter of the graft between 8 and 10 mm does not affect the laximetric results of an ACL reconstruction. Therefore, there does not appear to be a benefit to harvesting and adding further tissue to increase the diameter of the graft above 10 mm. Patients younger than 20 represent a population at risk of graft elongation. In these patients at risk, postoperative management needs to be modified (delayed weight bearing, articulated splinting, slower rehabilitation) in the first months.
Level of evidence
Retrospective case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reconstruction of the anterior cruciate ligament (ACL) is a common surgery, with increasingly successful results. A popular graft choice for the reconstruction is autograft hamstring tendons (HT) [24]. Techniques have included the use of both the semitendinosus (ST) and gracilis (G), and more recently a single tendon that is implanted in a quadrupled preparation [8]. Hamstring tendon techniques have been shown to have lower morbidity than that of the patellar tendon [2, 5, 16, 35], and successful results have been reported in many published articles [16, 20, 23, 24, 30, 32]. Biomechanical studies have shown that in 4-strand graft, the HT was equivalent or superior in terms of strength to graft bone-patellar tendon-bone [15, 38]. Despite much progress, revision rates of ACL reconstructions are between 1.8 and 10.4 % [39, 40]. ACL reconstruction with HT tendons can involve using an isolated ST, but the G can be added as necessary (ST–G) [8]. It has been shown that gender, age, height and body mass index (BMI) were predictive of the diameter and length of the tendons [33, 36, 37]. While we can predict the size of the tendons, we do not know precisely for each patient the dimensions of the native ACL we seek to rebuild. Recent publications have focused on the risk factors for failure of ACL reconstruction. A graft having a diameter of <8 mm has been associated with a high rate revision according to Magnussen et al. [23]. The procedure on a patient younger than 25 years according to Kamien et al. [18, 23] or younger than 20 for Magnussen et al. [18, 23] is also a risk factor for failure. The new element in this work is that the laximetric measurements were performed with a precise and reproducible laximeter at the preoperative and the latest follow-up. The aim of this study was to evaluate whether the diameter of the HT graft or patient age influences postoperative laximetry results after ACL reconstruction and whether this might have some influence on the post-op care management. The hypotheses were as follows:
-
1.
The larger the diameter of the graft, the lower the laxity measured.
-
2.
The younger the subject, the higher the risk of failure.
Materials and methods
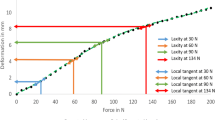
This was a retrospective, single-centre study on 88 consecutive ACL reconstructions using a short, quadrupled strand, single-bundle autograft. The reconstruction was performed by one single senior operator (HR) between January 2010 and January 2011. Included criteria were unilateral complete ACL tears, with or without partial meniscal lesions, with a minimum follow-up of 1 year. Exclusion criteria were as follows: partial ACL lesion, bilateral ACL lesions, combined ligament injuries, revisions and adolescents (<15 years), total or subtotal meniscectomy. The operative age, sex, height and weight of patients and the type of graft (semitendinosus mostly isolated) were recorded. The graft length must be less than sum of the length of the intra-articular path of the ACL and the length of tibial and femoral sockets; it was a short graft around 57 ± 3 mm in this series [8]. The diameter of the middle of the graft prepared in a close loop was measured using a calibrator, after preparation and pretension (Fig. 1). Patients were divided into three groups according to the diameter of the middle of the graft: group 1: 8 mm ≤ Ø ≤ 9 mm (n = 32), group 2: 9 mm < Ø ≤ 10 mm (n = 28) and group 3: Ø > 10 mm (n = 28). No graft had a diameter of <8 mm. All patients were reviewed clinically by an independent examiner, at a minimum of 1 year and a comparative laximetric measurement taken with GNRB® (GeNouRoB, Laval, France) at the time of the latest follow-up [28]. The measurement accuracy of the GNRB® is 0.1 mm [28]. A “residual laxity” of the ACL reconstruction with HT was defined by a differential laximetry of greater than 3 mm at 134 N (Δ134 > 3 mm). This threshold of 3 mm corresponds to the grade B (“nearly normal”) in the objective International Knee Documentation Committee score (IKDC). The average age of all patients at the time of surgery was 29.4 ± 10.2 years (15–54). There were 70 men (79 %) and 18 women (21 %). The distribution of meniscus status (intact, sutured or meniscectomy) is in Table 1.
The procedure was performed under general anaesthesia, most often associated with a femoral block and without a tourniquet. The arthroscopic assessment allowed the treatment of associated injuries (meniscal, chondral). Meniscal lesions were either sutured using an “all inside” technique or resected. The harvesting of the HT (ST ± G) was performed using an oblique 3-cm incision centred on their tibial insertion. We recommend sparing the gracilis, because the ST length can be generally quadrupled. If the ST was insufficient in length or thickness, experienced most frequently in short patients, the G was secondarily harvested. Tendons were cleaned of muscle insertion. The length of the prepared graft was chosen proportionally to patient height and averaged approximately 55–60 mm [8]. The tendon was wrapped around polypropylene tapes and then tensioned up to 200N for 30 s on a dedicated traction table [8, 12]. After traction was applied, the diameter of the graft was measured at each end and at its centre with a calibrator (Fig. 1). The measurement accuracy of the calibrator is 0.5 mm. Targeting of the femoral footprint was accomplished using an out-in guide at 120°, aimed at the centre of the femoral anatomical footprint and controlled by a fluoroscopic image [29]. The tibial targeting was performed using a standard tibial guide set to 60°, aimed at the centre of the tibial footprint. Retrograde reaming created sockets in the femur, and tibia sized according to the diameter of each end of the graft. The graft was then passed into the knee through the medial portal, and suspensory tapes were fixed in the tibia and femur using an absorbable interference screw (PLLA-βTCP). Knee stability was assessed with Lachman and pivot shift tests. Absence of roof impingement was then confirmed. Postoperatively, full weight bearing was allowed when quadriceps control was adequate. A careful rehabilitation was continued for 1–2 months. The resumption of pivot sports was allowed after the 7 month and after validation by clinical results and iso-kinetic testing. The Regional Ethics Committee (University of Angers, France) gave its approval for this clinical study (Number: 2010/07).
Statistical analysis
Patients were divided into three groups according to the diameter of the middle of the graft. An ANOVA test was used to compare the diameter of the graft between the three groups, (group 1: 8 mm ≤ Ø ≤ 9 mm, group 2: 9 mm < Ø ≤ 10 mm and group 3: Ø > 10 mm), BMI or age of patients with differential laximetry at 134N. Logistic regression was used to compare the risk (odds ratio) of excessive laxity between the three groups, group 1 being considered as the reference. Multivariate analyses were also computed taking age, gender and meniscus status into account. Fisher’s exact test was used to investigate the relationship between gender and the residual laxity. The Pearson correlation test was used to investigate the relationship between BMI and the diameter of the graft. The Student’s t test was used for mean comparisons. All statistical tests were computed considering a threshold of 0.05 as statistically significant. Analyses were conducted using STATA 12.
Results
The average follow-up was 26 months (12–44). The mean and SD diameter of the graft was 9.9 ± 1 mm (8–12). Fifty-two patients (59.1 %) had isolated ST graft and 36 patients a ST–G graft (40.9 %). The mean and SD diameter of the isolated ST grafts was 10.4 ± 1 and 9.5 ± 0.9 mm for ST–G grafts (ns). Using the laximetric results and definition of side-to-side laxity >3 mm, there was an overall 15.4 % residual laxity rate for the ST group and 22.2 % for the ST–G group (ns) (Table 2). There was no difference in patient size between the isolated ST group (176.1 ± 8.6 cm) and the ST–G group (174.1 ± 7.1 cm; ns) or in gender difference (10 women and 42 men for the ST group and 8 women and 28 men for the ST–G group; ns). There was a statistically significant correlation for the isolated ST group (p < 0.001) between the diameter of the graft and the size of the patient groups but not for the ST–G group (ns). The diameter of the graft was significantly higher among men (10 ± 1 mm) than in women (9.1 ± 1 mm; p = 0.002). The residual laxity rate among men was 16.7 and 25 % for women, with no statistically significant difference (ns) (Table 3). The residual laxity among the three groups was not statistically different according to the meniscus status (present or meniscectomy; ns).
There was no significant difference in the preoperative differential laxity between the three groups (Table 1). The mean postoperative Δ134 was, respectively, 1.5 ± 1.3 mm, 1.6 ± 1.5 mm and 2 ± 1.8 mm for groups 1, 2 and 3 (Table 1). There was no significant difference in the number of residual laxities between the three groups (ns). There were 16 patients with “residual laxity” (Δ134 > 3 mm) in total (18.2 %); three in group 1, four in group 2 and nine in group 3. However, as compared to group 1, OR was 1.46 (95 % CI 0.3–6) and 3.31 (95 % CI 0.9–12.3) in groups 2 and 3, respectively. The power analysis for the comparison between groups 1 and 2 was 10 %. Adjustment for age, gender and meniscus status did not change the estimates [OR 1.44 (95 % CI 0.3–6.2) and 3.92 (95 % CI 1–15.4)] in groups 2 and 3, respectively. No patient to our knowledge has had a revision. The average diameter of the graft in the “residual laxity” group (16 patients) was 10.4 ± 1 and 9.8 ± 1 mm in the group (72 patients) without residual laxity (ns).
Patients younger than 20 (18 cases) had a significantly higher average postoperative laximetry (2.4 ± 1.5 mm) compared to those aged 20 and over (1.5 ± 1.5 mm) (p = 0.03), regardless of the diameter of the graft (Table 4). The number of “residual laxity” cases (Δ134 > 3 mm) was also higher in the group of younger patients (27.8 %) than in patients aged 20 or over (15.7 %), but the difference was not significant (ns).
There were 31 overweight patients (BMI ≥ 25 kg/m2) (35.2 %), and among this population there were eight obese patients (BMI ≥ 30 kg/m2) (9 %). There were seven cases of “residual laxity” in patients with a BMI ≥ 25 kg/m2 (22.6 %) and none in obese patients (Table 5). There was statistically no more failure among overweight patients (ns) and obese patients (ns) than in the rest of the population.
Discussion
The most important finding of the present study was the increased risk of residual laxity (OR 3.31) in group 3 (Ø > 10 mm), as compared to group 1 (8 mm ≤ Ø ≤ 9 mm) in ACL reconstruction. There was no difference between group 1 as compared to group 2 (9 mm < Ø ≤ 10 mm), but the power analysis for the comparison was 10 %. Our results were not explained by age, gender difference nor meniscus status between groups according to our adjusted analyses.
Therefore, there does not appear to be a benefit to harvesting and adding further tissue to increase the diameter of the graft. With this quadrupled-ST technique, the exception would be if the ST is not sufficiently long or thick. This study also showed that patients below 20 had a higher postoperative laximetry than patients 20 or over.
We now know preoperatively how to predict the length and diameter of the HT tendons with size, sex and weight of the patient and more recently using MRI and ultrasound [6, 10, 14, 22, 33, 36, 37]. The length of the ST is strongly correlated with the height of the patient, while its diameter is correlated with the BMI; the correlations are weaker for the G [36]. Recent work by Magnussen et al. [23, 25] and Mariscalco et al. [23, 25] has shown that the diameter of an HT graft should be a minimum of 8 mm to obtain sufficient stability The development of short grafts allows surgeons to use the ST alone. Typically, this is a four- or five-strand reconstruction of a diameter greater than or equal to 8 mm and an average length of 56 ± 4.5 mm. It is also possible using short graft techniques to add the G to the ST to achieve a graft with a greater diameter, when the ST is short (small patient) or of inadequate diameter. Among the patients, there is significant variability in the diameter and length of the ST and G [22, 33]. Short graft techniques allow a better adjustment of the diameter of the graft in accordance with the length and diameter of the HT tendons. The reconstructed ACL size is determined by the harvested graft size, not by the size of the native ACL; if the graft is small, the resulting reconstructed ACL is also small. The removal of the ST alone or associated with the G (ST–G) does not lead to long-term deficit of knee flexion or loss of muscle strength [19, 21]. Biomechanical and animal studies have proven the importance of the diameter of the graft for the stability of the reconstruction at time 0 [9, 11, 15]. After implantation, the graft undergoes a process of ligamentization, the effectiveness of which is more important than the initial diameter for the quality of the final result [13]. It seemed logical to assume that the larger the diameter of the graft, the more it would be resistant to traction, but this assumption is contradicted by the clinical results. In our study, there was a significant laximetric difference related to the diameter of the graft, above 10 mm, compared to below or equal to 10 mm (p = 0.04). This result is consistent with recently published literature [3, 4, 16, 23, 25]. We defined our measured “residual laxity” threshold by a side-to-side laximetry >3 mm (grade B in IKDC objective score), measured with the GNRB® [28]. We had an overall “residual laxity” rate of 18.2 %. Kamien et al. [18] have found with different criteria (differential laximetry with the KT1000 > 5 mm or reoperation) a rate of 15.3 %, similar to that of our study. There was no greater rate of “residual laxity” in group 1 (8 ≤ Ø ≤ 9 mm) than in group 2 (9 < Ø ≤ 10 mm) (ns). We cannot exclude the hypothesis of a lack of power to explain this absence of association. Indeed, for an OR of 1.44 the power was only 10 %. This lack of relationship if the diameter of the graft is between 8 and 10 mm and the measured laxity make us aware of the importance of other factors such as the anatomical positioning of tunnels, the postoperative rehabilitation and compliance and the use of postoperative brace or splint.
Most grafts in groups 1 and 2 were ST only. Iriushischima et al. showed that the ST was sufficient to reproduce the size of the native ACL mid-substance cross-sectional area [17]. In group 3, there was mostly an association of the ST and the gracilis, which was significantly larger than the native ACL [17].
Two hypotheses are possible to explain the residual laxity in large graft (Ø > 10 mm). First, a graft that is too large may create a condition of roof impingement leading to abrasion and injury to collagen fibres and delayed revascularization [13]. Matsubara et al. [26] demonstrated that intercondylar roof impingement increases in anatomical single-bundle reconstruction with the diameter of the graft and hyperextension of the knee. Second, if the graft is too large, the centre of the graft will remain hypocellular and will not be revascularised much, if at all, in the weeks following post-implantation [1]. The revascularization starts at the graft’s periphery, and the origin is thought to be the Hoffa fat pad and the synovium [1].
There was greater “residual laxity” measured (Δ134 > 3 mm) in patients younger than 20 years (27.8 %) than among older patients (15.7 %), and the difference was significant (p = 0.03). A revision or differential laxity rate greater than 5 mm was found in patients <20 (14.3 %) for Magnussen et al. [23]. It is partly explained by a higher level of sports practiced (Tegner scale) by these young patients, regardless of the type of transplant (hamstring tendon, patellar tendon or allograft) and the diameter of the graft to the hamstring [7, 24, 31, 34]. In these patients at risk, postoperative follow-ups probably need to be modified (delayed weight bearing, articulated splinting as well as later and slower rehabilitation) to protect the ligamentization of the graft in the first few months. We did not find a difference in the group <25 years or ≥25 as has been demonstrated by Kamien et al. [18].
The diameter of the graft in women was significantly lower than in men in our study (9.1 vs. 10 mm, p = 0.04) as has been found in other studies [14, 16], and the rate of “residual laxity” (Δ134 > 3 mm) was higher among women (22.2 %) than men (17.1 %), but the difference was not significant (ns). Two studies have found a higher rate of residual laxity among women [27, 39, 40], and two found no difference according to gender [18, 20].
Weight did not influence postoperative laximetry. Overweight patients (BMI ≥ 25 kg/m2) or obese patients (BMI ≥ 30 kg/m2) did not have a higher risk of residual laxity of their ACL reconstruction.
The study has several limitations. The mean follow-up time of 26 months with that of 12 months for some patients may be insufficient. The laximetric measurement after a minimum of 1 year is taken as final in the absence of further trauma. Anatomical positioning of the graft in the femur and tibia, an important failure factor by progressive lengthening, was not studied. The activity level evaluated by the Tegner scale and the IKDC subjective score were not studied. The type of postoperative rehabilitation was not evaluated individually, although all patients theoretically proceeded under the same protocol.
The strengths of the article are that all patients were operated on using the same technique and by the same senior surgeon. The laximetric revision was performed with a precise and reproducible laximeter at the latest follow-up [28].
In the patient group <20, postoperative follow-up needs to be modified (delayed weight bearing, articulated splinting as well as later and slower rehabilitation) to protect the graft in the first months.
Conclusion
The diameter of the graft between 8 and 10 mm does not affect the laximetric results of an ACL reconstruction. Provided that its diameter is greater than 8 mm, there is no need for a large diameter transplant (>10 mm) to improve laximetric results. Patients under 20 represent a population at risk of ACL reconstruction lengthening. In this young population, postoperative recovery needs to be slowed.
References
Amiel D, Kleiner JB, Roux RD, Harwood FL, Akeson WH (1986) The phenomenon of “ligamentization”: anterior cruciate ligament reconstruction with autogenous patellar tendon. J Orthop Res 4(2):162–172
Andersson D, Samuelsson K, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. Arthroscopy 25(6):653–685
Barrett GR, Noojin FK, Hartzog CW, Nash CR (2002) Reconstruction of the anterior cruciate ligament in females: a comparison of hamstring versus patellar tendon autograft. Arthroscopy 18(1):46–54
Bedi A, Maak T, Musahl V, O’Loughlin P, Choi D, Citak M, Pearle AD (2011) Effect of tunnel position and graft size in single-bundle anterior cruciate ligament reconstruction: an evaluation of time-zero knee stability. Arthroscopy 27(11):1543–1551
Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS (2006) Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ 332(7548):995–1001
Bickel BA, Fowler TT, Mowbray JG, Adler B, Klingele K, Phillips G (2008) Preoperative magnetic resonance imaging cross-sectional area for the measurement of hamstring autograft diameter for reconstruction of the adolescent anterior cruciate ligament. Arthroscopy 24(12):1336–1341
Borchers JR, Pedroza A, Kaeding C (2009) Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case–control study. Am J Sports Med 37(12):2362–2367
Collette M, Cassard X (2011) The tape locking screw technique (TLS): a new ACL reconstruction method using a short hamstring graft. Orthop Traumatol Surg Res 97(5):555–559
Cummings JF, Grood ES, Levy MS, Korvick DL, Wyatt R, Noyes FR (2002) The effects of graft width and graft laxity on the outcome of caprine anterior cruciate ligament reconstruction. J Orthop Res 20(2):338–345
Erquicia JI, Gelber PE, Doreste JL, Pelfort X, Abat F, Monllau JC (2013) How to improve the prediction of quadrupled semitendinosus and gracilis autograft sizes with magnetic resonance imaging and ultrasonography. Am J Sports Med 41(8):1857–1863
Grood ES, Walz-Hasselfeld KA, Holden JP, Noyes FR, Levy MS, Butler DL, Jackson DW, Drez DJ (1992) The correlation between anterior-posterior translation and cross-sectional area of anterior cruciate ligament reconstructions. J Orthop Res 10(6):878–885
Guillard C, Lintz F, Odri GA, Vogeli D, Colin F, Collon S, Chappard D, Gouin F, Robert H (2012) Effects of graft pretensioning in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20(11):2208–2213
Hamada M, Shino K, Horibe S, Mitsuoka T, Toritsuka Y, Nakamura N (2005) Changes in cross-sectional area of hamstring anterior cruciate ligament grafts as a function of time following transplantation. Arthroscopy 21(8):917–922
Hamada M, Shino K, Mitsuoka T, Abe N, Horibe S (1998) Cross-sectional area measurement of the semitendinosus tendon for anterior cruciate ligament reconstruction. Arthroscopy 14(7):696–701
Hamner DL, Brown CH Jr, Steiner ME, Hecker AT, Hayes WC (1999) Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 81(4):549–557
Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA (2005) Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy 21(4):412–417
Iriuchishima T, Yorifuji H, Aizawa S, Tajika Y, Murakami T, Fu FH (2014) Evaluation of ACL mid-substance cross-sectional area for reconstructed autograft selection. Knee Surg Sports Traumatol Arthrosc 22(1):207–213
Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR (2013) Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med 41(8):1808–1812
Karimi-Mobarakeh M, Mardani-Kivi M, Mortazavi A, Saheb-Ekhtiari K, Hashemi-Motlagh K (2014) Role of gracilis harvesting in four-strand hamstring tendon anterior cruciate ligament reconstruction: a double-blinded prospective randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-2890-z
Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI (2007) A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and gracilis tendon graft. Am J Sports Med 35(5):729–739
Ko MS, Yang SJ, Ha JK, Choi JY, Kim JG (2012) Correlation between hamstring flexor power restoration and functional performance test: 2-year follow-up after ACL reconstruction using hamstring autograft. Knee Surg Relat Res 24(2):113–119
Ma CB, Keifa E, Dunn W, Fu FH, Harner CD (2010) Can pre-operative measures predict quadruple hamstring graft diameter? Knee 17(1):81–83
Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE (2012) Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 28(4):526–531
Maletis GB, Cameron SL, Tengan JJ, Burchette RJ (2007) A prospective randomized study of anterior cruciate ligament reconstruction: a comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med 35(3):384–394
Mariscalco MW, Flanigan DC, Mitchell J, Pedroza AD, Jones MH, Andrish JT, Parker RD, Kaeding CC, Magnussen RA (2013) The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a multicenter orthopaedic outcomes network (MOON) cohort study. Arthroscopy 29(12):1948–1953
Matsubara H, Okazaki K, Tashiro Y, Toyoda K, Uemura M, Hashizume M, Iwamoto Y (2013) Intercondylar roof impingement after anatomic double-bundle anterior cruciate ligament reconstruction in patients with knee hyperextension. Am J Sports Med 41(12):2819–2827
Noojin FK, Barrett GR, Hartzog CW, Nash CR (2000) Clinical comparison of intraarticular anterior cruciate ligament reconstruction using autogenous semitendinosus and gracilis tendons in men versus women. Am J Sports Med 28(6):783–789
Robert H, Nouveau S, Gageot S, Gagniere B (2009) A new knee arthrometer, the GNRB: experience in ACL complete and partial tears. Orthop Traumatol Surg Res 95(3):171–176
Robert HE, Bouguennec N, Vogeli D, Berton E, Bowen M (2013) Coverage of the anterior cruciate ligament femoral footprint using 3 different approaches in single-bundle reconstruction: a cadaveric study analyzed by 3-dimensional computed tomography. Am J Sports Med 41(10):2375–2383
Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K (2006) A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med 34(12):1933–1940
Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005) Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 21(8):948–957
Samuelsson K, Andersson D, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 25(10):1139–1174
Schwartzberg R, Burkhart B, Lariviere C (2008) Prediction of hamstring tendon autograft diameter and length for anterior cruciate ligament reconstruction. Am J Orthop 37(3):157–159
Shelbourne KD, Gray T, Haro M (2009) Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 37(2):246–251
Tibor LM, Long JL, Schilling PL, Lilly RJ, Carpenter JE, Miller BS (2010) Clinical outcomes after anterior cruciate ligament reconstruction: a meta-analysis of autograft versus allograft tissue. Sports Health 2(1):56–72
Treme G, Diduch DR, Billante MJ, Miller MD, Hart JM (2008) Hamstring graft size prediction: a prospective clinical evaluation. Am J Sports Med 36(11):2204–2209
Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM (2007) Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med 35(11):1945–1949
Wilson TW, Zafuta MP, Zobitz M (1999) A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med 27(2):202–207
Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, Wolf BR, Spindler KP (2007) Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective moon cohort study. Am J Sports Med 35(7):1131–1134
Wright RW, Magnussen RA, Dunn WR, Spindler KP (2011) Ipsilateral graft and contralateral ACL rupture at 5 years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am 93(12):1159–1165
Acknowledgments
The authors kindly appreciate the technical assistance for statistical analyses of Bertrand Gagnière, MD (Institut de Veille Sanitaire. Rennes. France).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marchand, J.B., Ruiz, N., Coupry, A. et al. Do graft diameter or patient age influence the results of ACL reconstruction?. Knee Surg Sports Traumatol Arthrosc 24, 2998–3004 (2016). https://doi.org/10.1007/s00167-015-3608-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3608-6