Abstract
Purpose
Evaluating joint laxity and graft compliance after ACL surgery may be used to quantify biomechanical graft properties during the ligamentization process. This study aimed to analyse the evolvement of joint laxity and graft compliance of short hamstring tendon grafts after ACL reconstruction (ACLR).
Methods
Forty-seven patients that underwent ACLR were retrospectively enrolled. Joint laxity was quantified with a GNRB® arthrometer before surgery, then at 15 days, at 1/3/6/9 months (M1–M9), at 1 year postoperatively and then again at the last mean follow-up (FU) of 14.7 ± 3.0 months. The side-to-side laxity difference (ΔL in mm) was measured at 30 and 60 N at every FU, additionally at 90 N from M3 on and at 134 N from M6 on. The side-to-side compliance difference (ΔC in µm/N) was calculated for each graft.
Results
Mean ΔL and ΔC decreased significantly between preoperative and M1 for all applied forces (at 30 N, ΔL: 0.8 mm, p < 0.0001; ΔC: 25.9 µm/N, p < 0.001). Between M1 and M9, ΔL increased significantly at 30 N (p = 0.02) and 60 N (p < 0.001), while ΔC increased by 15.2 µm/N at 30 N (p = 0.003) and 14.9 µm/N at 60 N (p = 0.001). Between M9 and the last FU, there were no significant differences for ΔL and ΔC.
Conclusion
Joint laxity and graft compliance evolve during the first postoperative year with a phase between the first and ninth postoperative month of relative weakness. According to the established evolvement profile, return to pivoting or contact sports should be considered only after stabilization of joint laxity and graft compliance.
Level of evidence
Retrospective cohort study, Level III
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction is a common procedure with almost 47.000 ruptures operated in France alone in 2016. The aim of ACL reconstruction (ACLR) is to restore the sagittal and rotatory stability of the knee and to prevent from secondary knee injuries, such as meniscal tears [36]. Common means of evaluating success of treatment are by assessment and comparison of pre- and postoperative knee joint laxity. The Lachman manoeuvre and pivot-shift test are often used, but they are found to be imprecise and subjective [5]. For more objective knee joint laxity assessment, several devices are used to measure anterior tibial translation, such as the KT-1000™ manual arthrometer (MEDmetric®, San Diego, USA) [14], the Rolimeter™ (Aircast, Summit, USA) [2], the radiological Telos™ stress device (Gmbh Hungen/Obbornhafen, Germany) [30] and the GNRB® (Genourob, Laval, France) arthrometer [25]. The GNRB® offers 0.1 mm accuracy for automated measurement of anterior tibial translation and has a higher sensitivity and specificity than both the KT-1000™ and the Telos™, with better intra- and interoperator reproducibility [3, 8, 12].
Many studies that have objectively evaluated knee joint laxity (“laximetry”) suggest that a greater measurement is associated with greater intra-articular pathology (meniscal and/or ligamentous lesions) [3, 21, 35]. Some have used laximetry to compare different types of grafts [4], or as a means of postoperative outcome evaluation [29, 42]. There are, however, few studies that have focused on the evolvement of knee joint laxity during the first postoperative year [15, 38]. Given that the graft undergoes histological and micro-architectural changes during this “ligamentization” period [1, 10, 32], the biomechanical properties of the graft may change too. Some studies showed a correlation between the signal intensity of the graft on MRI and its mechanical properties [9, 23]. To date, MRI is the only validated in vivo non-invasive analysis of the ligamentization process [31]. If there appears to be a correlation between the evolvement of knee joint laxity and the ligamentization process, laximetry may be an additional tool for in vivo non-invasive analysis of graft maturation or ligamentization.
This study aimed to analyse the evolvement of joint laxity and graft compliance (reverse of stiffness) after primary ACL reconstruction using hamstring tendon (HT) short grafts during the first postoperative year. It was hypothesized that knee joint laxity and graft compliance gradually evolve during the first year. A secondary aim was to determine if factors, such as age, gender, body mass index (BMI), meniscal lesions or associated anterolateral ligament (ALL) reconstruction would affect this evolvement.
Materials and methods
All patients agreed to participate in this study and provided written informed consent. This study received ethical approval before commencement by the Medical Ethical Committee at the University of Angers (#2013/07). The study was done in agreement with the ethical standards of the French National research committee and with the 1964 Declaration of Helsinki and its later amendments. This is a single centre (North Mayenne Hospital) and single-surgeon (HR) study. All patients that were operated between 2013 and 2017 for a primary unilateral ACL rupture were included. Pre- and postoperative laximetry data were collected for all patients and registered in the medical record. Exclusion criteria for analysis were multiple ligament injured knee, open physes, ACL reconstruction failure, and lost to follow-up. Relevant patient characteristics such as age, gender and BMI were extracted from the electronic medical record. Details regarding the surgery were extracted from the surgical report. All data were retrospectively collected and analysed.
Surgical technique
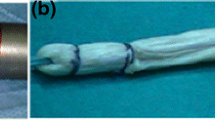
All patients underwent ACLR according to the Tape Locking Screw (TLS) technique (Laboratoire FH, Mulhouse, France) [12] using a quadruple-bundle semi-tendinosus short graft (ST4). If the diameter of the semi-tendinosus was considered too small, the gracilis tendon was used to create a 4-strand graft (ST-G). The graft was pretensioned at a maximum preload of 200 N for 30 s on a traction table. The fixation in the tunnels was ensured by bioabsorbable screws (PLLA-βTCP). A notchplasty was systematically performed in the event of graft-impingement in extension. For patients practising pivoting or pivoting-contact sports, or patients with a gross pivot-shift (grade 3) during examination under anaesthesia (by HR), an additional anterolateral ligament (ALL) reconstruction was performed with the gracilis tendon (TLS ST4 + G2 technique) or by a lateral tenodesis according to the Lemaire technique using fascia lata graft [27] if the gracilis tendon was used for ACLR. Meniscal tears were managed surgically by a suture-repair whenever possible or by abstention for stable lesions. If preserving the torn meniscus was not possible, a partial meniscectomy was performed.
Rehabilitation
Full weight-bearing with crutches was allowed immediately postoperative. Physiotherapy started on the 15th postoperative day with isometric exercises of the quadriceps and hamstrings. Return to straight-line running was allowed for each patient after the third month. After 9 months, the return to sports (RTS) capacity was evaluated for each individual patient by subjective parameters (subjective IKDC score) and objective criteria (functional tests, muscular strength).
Measurement protocol
The GNRB® arthrometer was used to measure anterior tibial translation at 20° of knee flexion, as such reproducing the Lachman manoeuvre. The GNRB® arthrometer measures anterior tibial translation (displacement in millimetres, with a 0.1 mm accuracy) for every 5 N of applied force. All patients underwent preoperative laximetry of both the healthy and injured knee. During postoperative follow-up (FU), joint laxity was measured for both knees at 15 days, 1, 3, 6, 9 months (M1, M3, M6, M9), 1 year and at the last FU. All knees were measured at 30 and 60 N at each FU. Measuring at 90 N and 134 N started only at M3 and M6, respectively, to protect the healing graft in the earliest phases.
For each FU, a force–displacement curve was created on Excel (e.g. Fig. 1) using a 4th degree polynomial regression equation (f(x) = ax4 + bx3 + cx2 + dx + e) that reflects the characteristic viscoelastic behaviour of the native ACL [6, 22]. For each measurement, the R2 coefficient of determination [26] was calculated to be as close as possible to 1. The joint laxity difference (ΔL, in mm) between the operated knee and healthy knee was calculated at each force level (30, 60, 90, and 134 N) for each subject with a 0.1 mm accuracy. Graft compliance was defined as the director coefficient of the tangent-line to the force–displacement curve at any given point (using the polynomial equation: f(x) = ax3 + bx2 + cx + d). The graft compliance difference (ΔC, in µm/N) between the operated knee and healthy knee was calculated at each force level (30, 60, 90, and 134 N) for each subject.
Statistical analysis
Statistical analyses were performed using SPSS Statistics® version 23 software (IBM®, Armonk, USA). Continuous variables were described using means and standard deviations. Categorical variables were tabulated with absolute and relative frequencies. The means of ΔL and ΔC were compared by paired Student t tests. Subgroup analyses were performed for age at surgery, gender, BMI, initial laxity at 134 N, presence of meniscal lesions, graft diameter and associated ALL reconstruction. Dichotomous categories were analysed by Mann–Whitney tests and nominal categories with non-parametric Kruskal–Wallis tests. The statistical significance threshold was set as p < 0.05.
Results
Forty-seven patients with complete laximetry data were enrolled in the study. At the last FU, 5 patients (10.6%) had a laximetry result that was considered a stabilisation failure (ΔL greater than 3 mm at 134 N) [20, 34] and were thus excluded from analysis. The mean age at surgery was 28.1 ± 9.6 years (13–46). The mean BMI was 24.5 ± 4.0 kg/m2 (18.7–37.7). There were 35 complete ACL ruptures and 12 partial lesions. Ten patients had an additional extraarticular ALL reconstruction with fascia lata (5) or gracilis (5) graft. Meniscal lesions were present in 31 patients: 17 medial meniscus lesions, 9 lateral meniscus lesions, and 5 bi-meniscal lesions. A ST4 graft was used in 37 cases and a 4-strand ST-G graft in 10 cases. The mean diameter of the femoral tunnel was 8.5 mm (7–10.5 mm) and 9.0 mm for the tibial tunnel (7.5–10.5 mm). A notchplasty was performed in 3 patients. The mean follow-up was 14.7 ± 3.0 months (12–22 months). Group characteristics are summarized in Table 1.
Preoperatively, ΔL was 1.0 ± 0.7 mm at 30 N, 2.1 ± 1.1 mm at 60 N, 2.8 ± 1.3 mm at 90 N and 3.4 ± 1.2 mm at 134 N, respectively. At the last FU, ΔL measured 0.5 ± 0.6 mm at 30 N, 0.9 ± 0.9 mm at 60 N, 1.1 ± 1.0 mm at 90 N and 1.2 ± 1.1 mm at 134 N (Fig. 2). For low ranges of force (30 and 60 N), there was a significant decrease of ΔL between preoperative and M1 (Table 2). Between M1 and M9, there was a significant increase of ΔL: 0.4 mm at 30 N (p = 0.002) and 0.9 mm at 60 N (p = 0.0004). For higher ranges of force (90 and 134 N), there was a general tendency for an increase of ΔL between M1 and M9, which then stabilized between M9 and the last FU, with non-significant difference.
Between preoperative and the last FU, there was a significant decrease of ΔC for all levels of force; 17.9 µm/N at 30 N (p = 0.001), 13.6 µm/n at 60 N (p = 0.001), 15.7 µm/N at 90 N (p = 0.005) and 15.9 µm/n at 134 N (p = 0.002) respectively (Fig. 3). At low ranges of force, there was a significant decrease of ΔC between preoperative and M1 (p < 0.0001 at 30 and 60 N) and then a significant increase between M1 and M9 (0.5 µm/N at 30 N, p = 0.002; 1.0 µm/N at 60 N, p = 0.0004) (Table 3). Between M9 and the last FU, ΔC significantly decreased at 30 N (8.2 µm/N, p = 0.01) and 60 N (6.9 µm/N, p = 0.016). For higher ranges of force, the decrease was significant between preoperative and M3 at 90 N and between preoperative and M6 at 134 N, after which there was no difference.
Five patients (10.6%) were excluded from main analysis because of a ΔL greater than 3 mm at any FU and were thus regarded a reconstruction failure. Patient characteristics for this subgroup are summarized in Table 4. For patients #10 (Fig. 4a, b), #23, and #38, joint laxity and graft compliance continued to increase after M9 stabilisation. Patient #25 had gross initial laxity and correction did not appear sufficient at M1. Patient #3 demonstrated great laxity and compliance (26.7 µm/N at 30 N and 41.8 µm/N at 60 N) since M6.
For subgroup analysis, all patients (including the five reconstruction failures) were included. Seven variables were considered: age, gender, BMI, meniscus lesions, preoperative laxity at 134 N, graft diameter and additional ALL reconstruction. Subgroups were created for each variable. ΔL and ΔC was not statistically significantly different in any of the subgroups (Fig. 4).
a Evolvement of ΔL at 30, 60, 90 and 134 N for Patient #10. ΔL Side-to-side laxity difference in mm, D15 15th postoperative day, FU follow-up, M1 1st postoperative month, M3 3rd postoperative month, M6 6th postoperative month, M9 9th postoperative month. b Evolvement of ΔC at 30, 60, 90 and 134 N for Patient #10. ΔC Side-to-side compliance difference in mm
Discussion
The most important finding of this study was a 3-phase joint laxity and graft compliance evolvement profile during the first postoperative year after ACL reconstruction. During the first phase (between preoperative and M1) ΔL and ΔC decrease significantly, then during the second phase (between M1 and M9) ΔL and ΔC gradually increase, and during the third phase (between M9 and last FU) ΔL and ΔC stabilise. At the last FU, mean ΔL was close to 1 mm (range 0–2.8 mm) at all force-levels, which is consistent with other series [12, 29, 34, 41].
Theoretically, an increase of joint laxity after ACL reconstruction is the sum of elongation of the graft and slippage (or failure) of the fixation. Few authors have studied the biomechanical evolvement of grafts regularly during the first year after ACL reconstruction [15, 38]. Graft fixation by the TLS screw system was studied in an animal model comparing four different ways of fixation [33]. The TLS screw fixation appeared to be very rigid (yield load and pull-out strength) during cyclic loading and load to failure tests [33]. During the first phase (up to M1), joint laxity and graft compliance remained low and its measurements were very close to the contralateral, healthy knee. While the initial decrease in ΔL and ΔC is to be expected directly after ACL reconstruction because of the reconstruction itself, graft pretensioning and initial tensioning of the graft during fixation may also contribute. The purpose of graft conditioning is to produce a structural realignment of the graft fibers, resulting in a more uniform graft loading. The gradual increase of joint laxity (ΔL) during the second phase may well be associated with progressive elongation of the graft, which then stabilises after the ninth month. The degradation of biomechanical properties during this phase could be explained by the necrosis and remodelling phase of the ligamentization process [10]. During this second phase, graft compliance (ΔC) was high at low force-levels, but appeared relatively low and comparable to the healthy contralateral knee for higher levels of force. With the recovery of mobility from 1 month, the graft lengthens slightly at low stress to allow complete recovery of the flexion of the knee. This corresponds to the restoration of the physiological laxity of the operated knee. The counterintuitive relationship between ΔL and ΔC during this phase may be due to the increasing recruitment of collagen fibers of the graft with the increase of force.
These results show that the viscoelastic properties of a normal ACL were not fully restored after ACL reconstruction [6]. Joint laxity and graft compliance were consistently higher than the contralateral, healthy knee for all levels of force. Siupsinskas et al. showed a stabilisation of ΔL with 4 strand HT grafts between 6 and 12 months after surgery (59 knees measured with GNRB® up to 1 year) [39]. In addition, a study by Semay et al. showed a stabilisation of ΔL after 1 year (20 ACL reconstructions measured with GNRB® [38]. Delahaye et al. found a stabilisation of ΔL after 6 months and a gradual stabilisation of ΔC over time (148 ACL reconstructions, KT-2000 arthrometer) [15]. However, in their study ΔC was calculated by taking the compliance difference at 89 and 134 N, implying that the mechanical behaviour of the graft is linear between these values, which is not consistent with other findings in the literature [22]. Bercovy et al. measured ΔL in 113 ACL reconstructed knees up to 3 years postoperative [6]. Stiffness decreased postoperatively up to 1 year, after which it stabilized, however, consistently lower than the healthy contralateral ACL. Unlike these studies, we found that the restoration of knee laxity and compliance was not a linear phenomenon during the first operative year.
Several animal studies examined the tensile strength and stiffness of autografts after ACL reconstruction. Weiler et al. found that Achilles tendon graft stiffness decreased during the first postoperative weeks and remained 50% lower than the native ACL 1 year after [40]. Blickenstaff et al. found that mechanical graft characteristics improve from the 12th week up to the 1st year, using an ST autograft in rabbits [7]. In both studies, graft stiffness at 1 year remained lower than that of the normal ACL, despite mature ligamentization. In these studies, no explanation was provided on the improvement of mechanical properties after the third month. Another animal study, on patellar tendon autografts in rhesus macaque monkeys, showed a decrease of mechanical properties (laxity and stiffness) up to 12 weeks and a stabilisation thereafter [11]. These results are chronologically concordant with our findings.
The graft ligamentization process is classically described in three successive phases: an early phase of cell and collagenous fibre depletion and partial necrosis, followed by a remodelling phase with neovascularization and invasion of fibroblastic cells and finally a maturation phase. The increase of laxity and compliance during the second phase (M1–M9) found in this study may well be in accordance with these necrosis and remodelling phenomena. Most studies with graft biopsies agreed on a ligamentization duration of 1–3 years [16, 37]. The duration of each phase is different according to different authors. Duration of each phase appears to be mainly dependent on the ligament environment, the positioning of the graft and the micro-trauma that are induced by physiotherapy. Our results show a stabilisation of ΔL and ΔC at the end of the first year, which may indicate the ending of the remodelling phase of ligamentization.
Multiple authors reported on graft appearance on MRI during the ligamentization process. Murakami et al. found that grafts were hyperintense (high signal/noise quotient) up to 1 year, and 31% remained high after 19 months [23]. Ntoulia et al. found a homogeneous and weak hyperintense signal of the grafts at 2 years postoperative [28]. Similar results were found by Muramatsu et al. up to 60 months postoperative [24]. Pauvert et al. reported that maturation of the graft was slow, gradual, and spread over a minimum of 2 years [31]. Finally, Weiler et al. found a correlation between the graft appearance on MRI and the mechanical graft properties in an animal study [40]. It appears that the maturation phase of ligamentization of ACL grafts on MRI takes longer than for the knee to biomechanically stabilise, as our results indicate.
With subgroup analyses, no statistically significant differences were found in ΔL and ΔC with regard to age, gender, BMI or initial joint laxity. For patients with bi-meniscal lesions significantly higher preoperative ΔL and ΔC were found, which can be explained by the fact that greater intra-articular damage leads to greater joint laxity. There was no difference in ΔL and ΔC for isolated medial or lateral meniscus lesions. There did not appear to be any effect of an additional ALL reconstruction on the sagittal stability of the knee.
Strengths of this study are a relative high number of patients, complete datasets for all follow-up moments, the use of a validated automated laximeter (GNRB®) [8, 13, 19] and a follow-up that extended well over 1 year postoperative. Measurements were done by the same observer, trained to use the GNRB® device.
However, this study has several limitations that need to be acknowledged too. First, it is still unknown how surgical technique affected the outcome results. For example, a lateral tenodesis or an ALL reconstruction could improve sagittal laxity, but it is still unproved. The condition of the graft was not postoperatively evaluated either arthroscopically or by MRI. By excluding patients with the suggestion of a failed reconstruction, we tried to compensate for this problem. The possibility of a generalized joint hypermobility has not been studied, although it is known to be a risk factor for ACL injuries [25]. A longer follow-up may further our understanding of the 3-phase evolvement profile; between M9 and the last FU ΔC still significantly decreased at low force-levels, while the corresponding ΔL had already stabilized. Perhaps is this finding associated with the maturation phase of ligamentization. This study did not consider any other grafts than short hamstring tendon grafts. Subgroup analyses were carried out with relatively small groups, with a substantial lack of statistical power.
Evaluating joint laxity and graft compliance during the first postoperative year may influence the rehabilitation process and serve as an additional decision tool for important milestones such as RTS [17, 41]. Possibly does a relative increase of graft compliance during this period indicate graft weakness, even before functional symptoms occur, and thus prevent from progressing the physical therapy protocol or even taking a step back. Inversely, the gradual decrease and stabilisation of ΔL and ΔC may herald the third phase and also weigh into the RTS decision. This study showed that ΔL and ΔC decrease and gradually stabilise after the ninth month, which is very much in accordance with a general RTS consensus among surgeons and with clinical findings in the literature [17, 18, 43].
Conclusion
Joint laxity and graft compliance evolve during the first postoperative year with a phase between the first and ninth postoperative months of relative weakness. According to the established evolvement profile, return to pivoting or contact sports should be considered only after stabilization of joint laxity and graft compliance.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ALL:
-
Anterolateral ligament
- BMI:
-
Body mass index
- ΔC:
-
Differential compliance
- ΔL:
-
Differential laxity
- M1:
-
First postoperative month
- M3:
-
Third postoperative month
- M6:
-
Sixth postoperative month
- M9:
-
Ninth postoperative month
- RTS:
-
Return to sports
- ST:
-
Semi-tendinosus
- ST-G:
-
Semi-tendinosus + gracilis
References
Amiel D, Kleiner JB, Roux RD, Harwood FL, Akeson WH (1986) The phenomenon of “Ligamentization”: anterior cruciate ligament reconstruction with autogenous patellar tendon. J Orthop Res 4:162–172
Balasch H, Schiller M, Friebel H, Hoffmann F (1999) Evaluation of anterior knee joint instability with the Rolimeter. A test in comparison with manual assessment and measuring with the KT-1000 arthrometer. Knee Surg Sports Traumatol Arthrosc 7:204–208
Beldame J, Mouchel S, Bertiaux S, Adam JM, Mouilhade F, Roussignol X, Dujardin F (2012) Anterior knee laxity measurement: comparison of passive stress radiographs Telos® and “Lerat”, and GNRB® arthrometer. Orthop Traumatol Surg Res 98:744–750
Belk JW, Kraeutler MJ, Marshall HA, Goodrich JA, McCarty EC (2018) Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction: a systematic review of comparative studies with minimum 2-year follow-up. Arthroscopy 34:1699–1707
Benvenuti JF, Vallotton JA, Meystre JL, Leyvraz PF (1998) Objective assessment of the anterior tibial translation in Lachman test position: comparison between three types of measurement. Knee Surg Sports Traumatol Arthrosc 6:215–219
Bercovy M, Weber E (1995) Evaluation of laxity, rigidity and compliance of the normal and pathological knee. Application to survival curves of ligamentoplasties. Rev Chir Orthop Reparatrice Appar Mot 81:114–127
Blickenstaff KR, Grana WA, Egle D (1997) Analysis of a semitendinosus autograft in a rabbit model. Am J Sports Med 25:554–559
Bouguennec N, Odri GA, Graveleau N, Colombet P (2015) Comparative reproducibility of TELOS and GNRB for instrumental measurement of anterior tibial translation in normal knees. Orthop Traumatol Surg Res 101:301–305
Cavaignac E, Marot V, Faruch M, Reina N, Murgier J, Accadbled F, Berard E, Chiron P (2018) Hamstring graft incorporation according to the length of the graft inside tunnels. Am J Sports Med 46:348–356
Claes S, Verdonk P, Forsyth R, Bellemans J (2011) The “ligamentization” process in anterior cruciate ligament reconstruction: What happens to the human graft? A systematic review of the literature. Am J Sports Med 39:2476–2483
Clancy W, Narechania RG, Rosenberg TD, Gmeiner JG, Wisnefske DD, Lange TA (1981) Anterior and posterior cruciate ligament reconstruction in Rhesus Monkeys. J Bone J Surg Am 63:1270–1284
Collette M, Cassard X (2011) The Tape Locking Screw technique (TLS): a new ACL reconstruction method using a short hamstring graft. Orthop Traumatol Surg Res 97:555–559
Collette M, Courville J, Forton M, Gagnière B (2012) Objective evaluation of anterior knee laxity; comparison of the KT-1000 and GNRB® arthrometers. Knee Surg Sports Traumatol Arthrosc 20:2233–2238
Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R (1985) Instrumented measurement of anterior laxity of the knee. J Bone Jt Surg Am 67:720–726
Delahaye H, Wiart F, Bibré P, Mortreux P, Vanvelcenaher J, Istas D, Letombe A (2008) Laxometric evaluation of the knee after anterior cruciate ligament plasty. J Traumatol Sport 25:199–203
Djian P, Rousseau R, Bellier G, Christel P (2014) Biological aspects of anterior cruciate ligament reconstruction using an autologous tendon graft. J Traumatol Sport 31:153–160
Fulton J, Wright K, Kelly M, Zebrosky B, Zanis M, Drvol C, Butler R (2014) Injury risk is altered by previous injury: a systematic review of the literature and presentation of causative neuromuscular factors. Int J Sports Phys Ther 9:583–595
Geffroy L, Lefevre N, Thevenin-Lemoine C, Peyronnet A, Lakhal W, Fayard JM, Chotel F (2018) Return to sport and re-tears after anterior cruciate ligament reconstruction in children and adolescents. Orthop Traumatol Surg Res 104:S183–S188
Lefevre N, Bohu Y, Naouri JF, Klouche S, Herman S (2014) Validity of GNRB® arthrometer compared to TelosTM in the assessment of partial anterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc 22:285–290
Lewis PB, Dushi Parameswaran A, Rue JPH, Bach BR (2008) Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med 36:2028–2036
Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP, Andrish JT, Jones MH, Parker RD, McCarty EC, Marx RG, Amendola A, Wolf BR, Flanigan DC, Kaeding CC, Brophy RH, Matava MJ, Wright RW, Dunn WR (2016) Effect of high-grade preoperative knee laxity on anterior cruciate ligament reconstruction outcomes. Am J Sports Med 44:3077–3082
Maitland ME, Bell GD, Mohtadi NGH, Herzog W (1995) Quantitative analysis of anterior cruciate ligament instability. Clin Biomech (Bristol, Avon) 10:93–97
Murakami Y, Sumen Y, Ochi M, Fujimoto E, Adachi N, Ikuta Y (1998) MR evaluation of human anterior cruciate ligament autograft on oblique axial imaging. J Comput Assist Tomogr 22:270–275
Muramatsu K, Hachiya Y, Izawa H (2008) Serial evaluation of human anterior cruciate ligament grafts by contrast-enhanced magnetic resonance imaging: comparison of allografts and autografts. Arthroscopy 24:1038–1044
Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE (2008) The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med 36:1073–1080
Nagelkerke NJD (2008) A note on a general definition of the coefficient of determination miscellanea a note on a general definition of the coefficient of determination. Biometrika 78:691–692
Ntagiopoulos P, Dejour D (2018) Extra-articular plasty for revision anterior cruciate ligament reconstruction. Clin Sports Med 37:115–125
Ntoulia A, Papadopoulou F, Zampeli F, Ristanis S, Argyropoulou M, Georgoulis A (2013) Evaluation with contrast-enhanced magnetic resonance imaging of the anterior cruciate ligament graft during its healing process: a two-year prospective study. Skelet Radiol 42:541–552
Orfeuvre B, Pailhé R, Sigwalt L, Rubens Duval B, Lateur G, Plaweski S, Saragaglia D (2018) Anterior cruciate ligament reconstruction with the Tape Locking Screw (TLS) and a short hamstring graft: clinical evaluation of 61 cases with a minimum 12 months’ follow-up. Orthop Traumatol Surg Res 104:701–705
Passler H, Mansat C (1986) Le test de Lachman radiologique. Une méthode simple et sûre pour le diagnostic des lésions des ligaments croisés. Sport Med 10:22–27
Pauvert A, Robert H, Gicquel P, Graveleau N, Pujol N, Chotel F, Lefevre N (2018) MRI study of the ligamentization of ACL grafts in children with open growth plates. Orthop Traumatol Surg Res 104:S161–S167
Pauzenberger L, Syré S, Schurz M (2013) “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy 29:1712–1721
Robert H, Bowen M, Odry G, Collette M, Cassard X, Lanternier H, De Polignac T (2014) A comparison of four tibial-fixation systems in hamstring-graft anterior ligament reconstruction. Eur J Orthop Surg Traumatol 25:339–347
Robert H, Limozin R, De Polignac T (2011) Single-bundle reconstruction in quadruple Semi tendinosus graft of the ACL according to the TLS technique. Clinical results of a series of 74 knees with minimum 18 months follow-up. Rev Chir Orthop Traumatol 97:S40–S45
Robert H, Nouveau S, Gageot S, Gagnière B (2009) A new knee arthrometer, the GNRB®: experience in ACL complete and partial tears. Surg Res 95:171–176
Sanders TL, Kremers HM, Bryan AJ, Fruth KM, Larson DR, Pareek A, Levy BA, Stuart MJ, Dahm DL, Krych AJ (2016) Is anterior cruciate ligament reconstruction effective in preventing secondary meniscal tears and osteoarthritis? Am J Sports Med 44:1699–1707
Scranton PE, Lanzer WL, Ferguson MS, Kirkman TR, Pflaster DS (1998) Mechanisms of anterior cruciate ligament neovascularization and ligamentization. Arthroscopy 14:702–716
Semay B, Rambaud A, Philippot R, Édouard P (2016) Évolution de la laxité antéro-postérieure par GnRB à 6,9 et 12 mois d’une reconstruction du ligament croisé antérieur. Rev Chir Orthopédique Traumatol 102:S138–S139
Siupsinskas L, Gudas R, Salatkaite S (2018) Changes in laxity of the reconstructed ACL in professional and recreational athletes. Knee Surg Sports Traumatol Arthrosc 26:415
Weiler A, Peters G, Mäurer J, Unterhauser FN, Südkamp NP (2001) Biomechanical properties and vascularity of an anterior cruciate ligament graft can be predicted by contrast-enhanced magnetic resonance imaging: a two-year study in sheep. Am J Sports Med 29:751–761
Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A (2018) Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sport Traumatol Arthrosc 26:3636–3644
Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler HH (2011) Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy 27:653–665
Zaffagnini S, Macchiarola L, Cucurnia I, Grassi A, Signorelli C (2018) Laxity-based return to play. In: Musahl V, Karlsson J, Krutsch W, Mandelbaum B, Espregueira-Mendes J (eds) Return to play football. Springer, New York, pp 193–203
Acknowledgements
The authors wish to thank Yannis Clair, a biomechanical engineer, for his assistance in methodology of data collection and statistical analysis.
Funding
There is no funding source for this study.
Author information
Authors and Affiliations
Contributions
TP and HR participated in the design of the study and data-collection. TP carried out statistical analysis and writing of the manuscript. HR and BM have contributed to writing of the manuscript and its correction. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethical approval
The ethical approvement statement was obtained from the Ethical Comitee of Angers University Hospital (Study # 2013/07).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pouderoux, T., Muller, B. & Robert, H. Joint laxity and graft compliance increase during the first year following ACL reconstruction with short hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc 28, 1979–1988 (2020). https://doi.org/10.1007/s00167-019-05711-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05711-z