Abstract
Purpose
Intraoperative fracture of the lateral cortex fractures of the tibia is a potential complication of high tibial osteotomy (HTO), which may result in inadequate rotational alignment of the distal tibia. Our aim was to determine how rotational malalignment of the distal tibial segment distal would affect intraarticular contact pressure distribution in the knee and ankle joints.
Methods
A medial, L-shaped opening-wedge HTO was performed on seven human lower body specimens. A stainless steel device with integrated load cell was used to axially load the leg. Pressure-sensitive sensors were used to measure intraarticular contact pressures. Intraoperative changes in alignment were monitored in real time using computer navigation. Measurements were performed in the native knee alignment, after 10° and 15° of alignment correction and with the distal tibia fixed at 15° of external rotation.
Results
Moderate-to-large alignment changes after medial opening-wedge HTO resulted in a shift in intraarticular contact pressures from the medial compartment of the knee towards the lateral compartment. However, fixation of the distal tibial segment at 15° of external rotation neutralized this intended beneficial effect. In the ankle, external rotation of the distal tibia also caused a reduction in contact pressures and tibiotalar contact area.
Conclusion
Malrotation of the distal tibial fragment negates the intended effect of offloading the diseased compartment of the knee, with the contact pressures remaining similar to those of the native knee. Furthermore, malrotation leads to abnormal ankle contact pressures. Care should be taken to ensure appropriate rotational alignment of the distal tibial segment during intraoperative fixation of HTO procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Opening-wedge high tibial osteotomy (HTO) is commonly used for the surgical treatment of moderate osteoarthritis (OA) of the medial compartment of the knee. Numerous studies have documented the effects of HTO on the biomechanics of the knee [1, 2, 4, 5, 7, 8, 10, 19, 21–23, 27]. It has been shown that medial compartment pressures decrease with progressive increase in the valgus alignment of the leg, leading to improved pain and function [1, 16, 18].
Published techniques for medial opening-wedge HTO recommend leaving the lateral cortex intact, so as to provide rotational stability for the construct [13, 14]. However, intraoperative lateral cortex fractures may still occur in about 25 % of cases, and the stability of the construct may be compromised [3, 9, 15, 17, 24, 26]. Previous research has shown that tibial malrotation affects the distribution of loads within the knee [28]. However, the effect that distal tibial malrotation during HTO might have on knee and ankle pressures has not been previously studied.
The aim of this experiment was to evaluate how rotational malalignment of the tibial segment distal to the osteotomy site would affect intraarticular contact pressure distribution in the knee and ankle joints. We hypothesized that distal tibial malrotation would result in changes in the magnitude of the contact forces and of the contact area in both the knee and the ankle.
Materials and methods
Eight whole-body human cadaveric specimens were procured. Specimens were included if their ages were between 40 and 65 years. Our exclusion criteria were as follows: traumatic lower limb malalignment; absence of the anterior cruciate ligament (ACL); articular cartilage defects; signs of osteoarthritic changes; and meniscal injury. One specimen was discarded due to having an absent ACL and grade III osteoarthritis, leaving seven specimens available for testing. Specimens were fully thawed at room temperature prior to surgery.
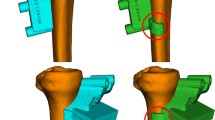
Specimens were placed supine on an operating table. A medial parapatellar arthrotomy was first performed on all specimens to explore the intraarticular knee space and assesses for ligamental or cartilaginous damage. Through a medial approach, the superficial fibres of the medial collateral ligament were released and a medial, L-shaped opening-wedge HTO was performed using the technique described by Lobenhoffer and Agneskirchner [6, 13, 14]. With the aid of fluoroscopy, two 2.5-mm Kirschner wires were inserted 5 cm distal to the joint line, starting proximal to the pes anserinus and extending to the level of the tip of the fibula at the lateral cortex. An oblique osteotomy was performed in the posterior two-thirds of the medial aspect of the tibia distal to the Kirschner wires and parallel to the tibial slope, carefully leaving intact a 10-mm lateral bone bridge. A second osteotomy was started in the anterior one-third of the tibia at an angle of 135°, leaving the tibial tuberosity intact. Osteotomes were carefully inserted and used to open the osteotomy up to the desired angle. An external fixator was used to secure the open-wedge osteotomy during testing at each step of alignment correction (10° and 15°) and of distal tibial rotation (0° and 15°).
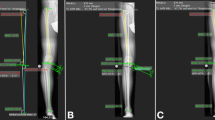
Leg alignment changes were tracked and recorded in real time using a computer navigation system (Vector Vision, BrainLAB, Munich, Germany). Minimally invasive reference arrays were attached to the femoral and tibial shafts. An isocentric mobile C-arm with 3D imaging capability (Siremobil ISO-C 3D, Siemens, Germany) was used to scan the knee joint. The imaging dataset was transferred to the navigation system, and registration was performed. The combination of the acquired 3D imaging and computer navigation data allows for real-time monitoring of the mechanical axis. Hence, we were able to follow intraoperative changes in alignment live through a computer interface.
To further monitor and confirm mechanical alignment changes after increasing the medial tibial opening, we placed a lead-impregnated axis board underneath the leg [12]. The long axis was situated through both the centre of the femoral head and the centre of the talus. Correct positioning was confirmed using fluoroscopy. Once the board was in place, subsequent fluoroscopic images were used to identify the location of the mechanical axis in relation to the centre of the knee joint and to quantify alignment changes by measuring the angle between the mechanical axis line and the tibial plafond outline.
A previously developed stainless steel device was used to axially load the leg [11]. The loading device was attached to the pelvis using Schanz screws, and the foot was secured to a distal plate. The set-up allows for axial loading with the knee in full extension. An integrated load cell was used to track in real time the applied load and torque.
Pressure-sensitive sensors (K-Scan 4000, Tekscan, South Boston, MA, USA) were used to collect intraarticular contact pressures. These sensors are 0.1 mm thin, and its pressure-sensitive area contains 62 sensels/cm2. They are placed inside the joint, covering the articular surface. The opposite end is inserted into a handle designed to read the data being collected during testing.
Baseline measurements were taken for each leg in its native alignment. An axial loading force was applied to the leg in the caudal–cranial direction and gradually ramped up from 0 to 550 N [25]. Intraarticular contact pressure (kg) and contact area (mm2) data were measured and collected in real time.
The study was approved by the Ethics Commission of the Hannover Medical School with the number 1199-2011.
Statistical analysis
Stata/SE 12.1 (StataCorp LP, College Station, TX, USA) was used for all analyses. An a priori sample size calculation showed that testing at least six specimens would be necessary to ensure 0.80 power. Multiple linear regression models were constructed to estimate changes in contact pressure and contact surface area in the medial and lateral compartments of the knee and in the ankle, in response to 10° and 15° changes in mechanical alignment and to 15° of distal tibial rotation. The following variables were also measured in real time during testing and were included as covariates in our models: side; force (axial, horizontal and vertical); torque (axial, horizontal and vertical); and changes in knee alignment (varus and valgus; ante- and retrocurvature; and axial angle). For all tests, α was set to 0.05. Results are presented as mean and 95 % confidence interval (95 % CI), or as percentage change, wherever appropriate.
Results
Tables 1 and 2 summarize the results for the knee and the ankle, respectively.
Moderate-to-large alignment changes after medial opening-wedge HTO resulted in a significant shift in intraarticular contact pressures from the medial compartment of the knee towards the lateral compartment (pressure ratio: 1.9; P < 0.05). However, fixation of the distal tibial segment at 15° of external rotation neutralized this intended beneficial effect (pressure ratio: 1.1; P < 0.05) (Figs. 1a, b, 2). A significant increase in tibiofemoral contact area was also observed in the medial compartment (P < 0.05) (Fig. 3a, b).
Visualization of the changes in intraarticular knee pressures in a single specimen as a function of alignment correction and distal tibial rotation. Alignment correction successfully shifted the load towards the lateral compartment. On the other hand, malrotation of the distal tibial segment led to increased pressures in the medial compartment
In the ankle, external rotation of the distal tibia caused a significant reduction in contact pressures (Fig. 4) and tibiotalar contact area (Fig. 5) (P < 0.05).
Discussion
The most important finding of this study was that fixation of the distal tibial fragment in rotational malalignment negated the intended beneficial effect of offloading the medial compartment in opening-wedge medial HTO. Additionally, we found that malrotation of the distal tibial led to abnormal load distribution in the ankle joint.
Valgus realignment of the leg through a medial opening-wedge HTO is advocated for the treatment of isolated medial compartment OA of the knee. While highly successful, certain complications have been reported, including intra- and post-operative lateral cortex fractures [15, 17, 24, 26]. Published techniques for medial opening-wedge HTO recommend leaving at least 1 cm of intact lateral cortex to maintain rotational control of the construct [13, 14]. Han et al. [9] determined that aiming the plane of the osteotomy towards a safe zone located between the tip of the fibular head and the circumference line of the fibular head reduced the risk of lateral cortex fractures. Akamatsu et al. [3] showed that navigation could help reduce undercorrection in cases of lateral cortex fractures. The type of implant used can also affect the post-operative stability of the construct, with plate fixation leading to better stability compared to spacer plates [20].
However, despite improvements in HTO technique, intraoperative fractures of the lateral cortex still occur. After analysing a series of 104 HTOs, Takeuchi et al. [24] reported a 25 % incidence of lateral cortex fractures. More recently, Martin et al. [15] reported 20 % of undisplaced lateral cortical breaches and 6 % lateral hinge fractures in a series of 323 cases. When the lateral cortical hinge becomes compromised, intraoperative control over the construct may become difficult, oftentimes leading to post-operative varus malalignment [26].
This study has several potential limitations. Since the current set-up does not allow for testing in knee flexion or to simulate dynamic in vivo joint movements, we only tested the specimens in biostatic axial loading conditions. Due to the lack of in vivo muscular forces simulation, we cannot determine the exact role of some musculotendinous structures in the load distribution of the ankle joint. It is possible that the action of the Achilles tendon in particular could affect the distribution of forces within the ankle. Additionally, the 10°–15° correction applied in this study may not represent routine clinical practice and that it has the potential drawback of over- or undercorrecting individual specimens. However, we believe that this standardized approach is valuable and that the aim of the study of comparing non-rotated to malrotated states was successfully achieved, especially considering that each specimen essentially served as their own control. The estimation models used in this study take into account the alignment of each specimen, therefore reducing their potentially confounding effect.
Conclusion
Malrotation of the distal tibial fragment negates the intended effect of offloading the diseased compartment of the knee, with the contact pressures remaining similar to those of the native knee. Furthermore, malrotation leads to abnormal ankle contact pressures. Care should be taken to ensure appropriate rotational alignment of the distal tibial segment during intraoperative fixation of HTO procedures.
References
Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P (2004) Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg 124(9):575–584
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23(8):852–861
Akamatsu Y, Mitsugi N, Mochida Y, Taki N, Kobayashi H, Takeuchi R, Saito T (2012) Navigated opening wedge high tibial osteotomy improves intraoperative correction angle compared with conventional method. Knee Surg Sports Traumatol Arthrosc 20(3):586–593
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):197–205
Fening SD, Kovacic J, Kambic H, McLean S, Scott J, Miniaci A (2008) The effects of modified posterior tibial slope on anterior cruciate ligament strain and knee kinematics: a human cadaveric study. J Knee Surg 21(3):205–211
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2013) Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 21(1):170–180
Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD (2007) Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med 35(9):1443–1449
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2):376–382
Han SB, Lee DH, Shetty GM, Chae DJ, Song JG, Nha KW (2013) A “safe zone” in medial open-wedge high tibia osteotomy to prevent lateral cortex fracture. Knee Surg Sports Traumatol Arthrosc 21(1):90–95
Javidan P, Adamson GJ, Miller JR, Durand P Jr, Dawson PA, Pink MM, Lee TQ (2013) The effect of medial opening wedge proximal tibial osteotomy on patellofemoral contact. Am J Sports Med 41(1):80–86
Kendoff D, Board TN, Citak M, Gardner MJ, Hankemeier S, Ostermeier S, Krettek C, Hufner T (2008) Navigated lower limb axis measurements: influence of mechanical weight-bearing simulation. J Orthop Res 26(4):553–561
Liodakis E, Kenawey M, Liodaki E, Mommsen P, Krettek C, Hankemeier S (2010) The axis-board: an alternative to the cable technique for intraoperative assessment of lower limb alignment. Technol Health Care 18(3):165–171
Lobenhoffer P, Agneskirchner J, Zoch W (2004) Open valgus alignment osteotomy of the proximal tibia with fixation by medial plate fixator. Der Orthopade 33(2):153–160
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11(3):132–138
Martin R, Birmingham TB, Willits K, Litchfield R, Lebel ME, Giffin JR (2014) Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med 42(5):1118–1126
McKellop HA, Sigholm G, Redfern FC, Doyle B, Sarmiento A, Luck JV Sr (1991) The effect of simulated fracture-angulations of the tibia on cartilage pressures in the knee joint. J Bone Joint Surg Am 73(9):1382–1391
Miller BS, Downie B, McDonough EB, Wojtys EM (2009) Complications after medial opening wedge high tibial osteotomy. Arthroscopy 25(6):639–646
Mina C, Garrett WE Jr, Pietrobon R, Glisson R, Higgins L (2008) High tibial osteotomy for unloading osteochondral defects in the medial compartment of the knee. Am J Sports Med 36(5):949–955
Pape D, Duchow J, Rupp S, Seil R, Kohn D (2006) Partial release of the superficial medial collateral ligament for open-wedge high tibial osteotomy. A human cadaver study evaluating medial joint opening by stress radiography. Knee Surg Sports Traumatol Arthrosc 14(2):141–148
Pape D, Kohn D, van Giffen N, Hoffmann A, Seil R, Lorbach O (2013) Differences in fixation stability between spacer plate and plate fixator following high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):82–89
Rodner CM, Adams DJ, Diaz-Doran V, Tate JP, Santangelo SA, Mazzocca AD, Arciero RA (2006) Medial opening wedge tibial osteotomy and the sagittal plane: the effect of increasing tibial slope on tibiofemoral contact pressure. Am J Sports Med 34(9):1431–1441
Stoffel K, Willers C, Korshid O, Kuster M (2007) Patellofemoral contact pressure following high tibial osteotomy: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 15(9):1094–1100
Suero EM, Sabbagh Y, Westphal R, Hawi N, Citak M, Wahl FM, Krettek C, Liodakis E (2014) Effect of medial opening wedge high tibial osteotomy on intraarticular knee and ankle contact pressures. J Orthop Res. doi:10.1002/jor.22793
Takeuchi R, Ishikawa H, Kumagai K, Yamaguchi Y, Chiba N, Akamatsu Y, Saito T (2012) Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: a new classification of lateral hinge fracture. Arthroscopy 28(1):85–94
Tarr RR, Resnick CT, Wagner KS, Sarmiento A (1985) Changes in tibiotalar joint contact areas following experimentally induced tibial angular deformities. Clin Orthop Relat Res 199:72–80
van Raaij TM, Brouwer RW, de Vlieger R, Reijman M, Verhaar JA (2008) Opposite cortical fracture in high tibial osteotomy: lateral closing compared to the medial opening-wedge technique. Acta Orthop 79(4):508–514
Voos JE, Suero EM, Citak M, Petrigliano FP, Bosscher MR, Wickiewicz TL, Pearle AD (2012) Effect of tibial slope on the stability of the anterior cruciate ligament-deficient knee. Knee Surg Sports Traumatol Arthrosc 20(8):1626–1631
Yazdi H, Mallakzadeh M, Sadat Farshidfar S, Givehchian B, Daneshparvar H, Behensky H (2014) The effect of tibial rotation on knee medial and lateral compartment contact pressure. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3321-x
Acknowledgments
None of the authors have any professional or financial affiliations that could have biased this study. Funding awarded by the German Research Foundation (DFG) was used to construct the device used for axially loading the limb and the computer interface used to monitor changes in the knee joint during the experiments. Funding awarded by the Robert Mathys Foundation (RMS) was used for all materials required for performing the surgeries and for performing ankle measurements.
Author information
Authors and Affiliations
Corresponding author
Additional information
Eduardo M. Suero and Nael Hawi have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Suero, E.M., Hawi, N., Westphal, R. et al. The effect of distal tibial rotation during high tibial osteotomy on the contact pressures in the knee and ankle joints. Knee Surg Sports Traumatol Arthrosc 25, 299–305 (2017). https://doi.org/10.1007/s00167-015-3553-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3553-4