Abstract
Patella infera is a known complication of high tibial osteotomy (HTO) that can cause anterior knee pain due to excessive stresses associated with abnormal patellofemoral (PF) joint biomechanics. However, the translation of these abnormal biomechanics to native cartilage pressure has not been explored. The present study was designed to compare the PF contact pressures of three different HTOs in a human cadaveric model of valgus tibiofemoral correction. Nine fresh cadaveric knees underwent (1) medial opening wedge (OWHTO) with a proximal tuberosity osteotomy (PTO), (2) OWHTO with a distal tuberosity osteotomy (DTO), and (3) a lateral closing wedge (CWHTO). The specimens were mounted in a custom knee simulation rig, with muscle forces being simulated using a pulley system and weights. The PF contact pressure was recorded using an electronic pressure sensor at 15°, 30°, 60°, 90°, and 120° of knee flexion, with results of the intact knees obtained as relative control. Compared to the intact knee, the DTO OWHTO and CWHTO did not significantly (P > 0.05) influence PF pressure at any flexion angle. On the other hand, PTO OWHTO lead to a significant elevation in PF cartilage pressure at 30° (P < 0.05), 60° (P < 0.005), and 90° (P < 0.0005) knee flexion. We conclude from these results that DTO OWHTO maintains normal joint biomechanics and has no significant effect on PF cartilage pressure. In patients who complain of pre-existing anterior knee pain, DTO OWHTO or CWHTO should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of varus tibiofemoral malignment and associated medial compartment osteoarthritis of the knee by a high tibial osteotomy (HTO) is a well accepted treatment option [2, 12, 13, 18, 20, 53, 55, 56, 64]. Lateralization of the loading axis decompresses the overloaded medial compartment of the knee, thereby minimizing pain and inhibiting osteoarthritic degeneration. But although valgus correction is clinically successful, patella infera is a common postoperative complication linked to this technique, with incidence reported as high as 89% [12, 18, 23, 36, 53, 56, 64]. The alteration of patella height in the lateral closing HTO (LCHTO) is caused by interstitial scarring of the patella ligament and bone formation behind the patellar ligament [7, 53], whereas in the medial opening wedge HTO (OWHTO) it is caused by a distalisation of the tibial tuberosity [18, 53, 56]. The clinical sequelae of patella infera generally present as anterior knee pain, patellar locking, crepitus, and reduced range of motion, but may also complicate total knee replacement [36, 49, 64]. Patients presenting with patella infera after HTO or TKA experience greater postoperative anterior knee pain [49, 63]; a complication often attributed to patella malalignment and maltracking [29, 30, 64] and elevated cartilage pressure [8, 10, 17, 32, 47, 58, 61]. Although many surgeons still adopt the LCHTO technique, and it has been suggested that this technique exhibits less patella infera that conventional OWHTO [7], the closing wedge technique is consistently compromised by medial collateral ligament instability and other complications postoperatively [26, 40].
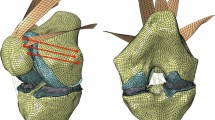
A new technique for preserving the insertion of the patellar ligament and the anatomical location of the tibial tuberosity has recently been described [18]. Unlike traditional OWHTO where a single plane osteotomy is performed proximal to the tuberosity (PTO), the distal tuberosity osteotomy (DTO) OWHTO procedure allows the tuberosity to remain attached to the proximal region of the tibia (Fig. 1). Opening of the wedge does not alter the position of patella attachment at the tuberosity, therefore preventing patella infera complication. Whilst patella height does not seem to be affected, an alteration of pressure in the patellofemoral joint through medio-lateral changes of tuberosity position is an untested phenomenon. Indeed, it has been shown that lateralization of the tibial tuberosity increases the Q angle and lateral patellofemoral contact pressure [22, 28]. Hence, whilst DTO OWHTO may be clinically useful in preventing patella infera, attention must be paid to maintain normal joint kinematics.
Patellofemoral cartilage pressure should be unchanged after knee surgery in order to halt joint surface deterioration. To this end, the changes in patellofemoral pressure following HTO have not been well investigated. Hence, we report on the effect of three different types of HTO on contact pressure within the patellofemoral joint.
Materials and methods
Cadaveric knees
Nine fresh-frozen human male cadaveric knees of (median age 72 ± 8.1; six female and three male) were used. Approximately 20 cm of proximal femur and distal tibia were preserved. All knees had not been operated on previously and had relatively normal tibiofemoral alignment. Biplanar radiographs were taken to exclude any osseous pathology, pre-existing disease, or trauma. The specimens were wrapped in saline soaked cloth, and stored at −30°C in tightly sealed plastic bags. Joints were thawed over 24 h before testing. All testing was conducted under regulations outlined by the University of Western Australia Research Ethics Committee.
Osteotomies
The knees were dissected of all skin and subcutaneous tissue. Proximal medial opening (PTO OWHTO), distal medial OWHTO (DTO OWHTO), and lateral closing HTO (CWHTO) were performed on the cadaveric knees sequentially in the aforementioned order (Fig. 1). (1) DTO OWHTO: The osteotomy was performed as detailed by Gaasbeck et al. [18], so that the tuberosity remained proximally attached to the tibia; thereby maintaining patellar height after opening the osteotomy. Primarily, the transverse tibial osteotomy leaves at least 1 cm of the tuberosity thickness intact, before the osteotomy is continued posteriorly through the tibia. Then, from the tibial osteotomy, the tuberosity was cut distally in the frontal plane towards the anterior tibial cortex. Following medial plate fixation with a 3.5 mm LCP, the distal part of the tuberosity is fixed with a bicortical screw to the tibia to increase the fixation strength. (2) PTO OWHTO: While the medial plate fixation remained in place, the transverse osteotomy of the tibia was completed towards the anterior cortex creating a mobile tuberosity. After removing the screw, the tuberosity was distalised and lateralized to its original position and fixed to the tibia with two screws. For both the medial proximal and medial distal OWHTO, the base of the osteotomy was opened and a hard plastic wedge with a base of 14 mm was inserted (Fig. 2). (3) CWHTO: The medial locking plate was removed while the tuberosity remained fixed with screws to the tibia. A lateral bony wedge with a base of 14 mm was resected. The cortex of the medial tibia was aligned and the lateral gap was closed. The medial side was stabilized with a stapler while the lateral osteotomy was fixed with a 3.5 mm LCP.
Knee simulator (Fig. 3)
This rig was designed to permit free rotation of the tibia during flexion. Each knee was therefore mounted in a customized passive motion rig with the femur potted in a cubic metal cylinder using dental cement (Glastone 3000, Die Stone, Type V, Densply, Perth, AU). The cylinder was lined up with the transepicondylar knee axis. An aluminium ring attached to the tibia articulated with a low-friction roller, thus avoiding the constraints associated with gripping the tibia by hand. A clamp was secured to the quadriceps tendon 2 cm proximal to the superior patella. The clamp was connected to a weight. An 87 N extensor muscle loading force was applied. This load is similar to Elias’ et al. [15]. An additional force of 8.5 N was added to the ITB, and 21 N to the biceps and the semimembranosus/semitendinosus tendon, respectively. This distribution of the forces is similar to the force ratios used by other authors [3, 19, 51]. Each knee was flexed with the quadriceps aligned with the femur (Fig. 3.)
Contact pressure measurement
The Pedar™ pressure measurement system was used to assess patellofemoral pressure. The pressure sensor was inserted into the knee joint through a small suprapatellar arthrotomy and placed between the patella and the femoral condyles in the patella groove. The sensor system contains over 80 sensors with a size of 1 cm2each. The sensors have a pressure range of 30–1,200 kPa, with a resolution of 5 kPa. The peak value was taken for each flexion angle. To ensure measurement reliability, each test was conducted four times by taking out the sensor and replacing it in the patellofemoral joint. Hence, each knee value represented the mean of four repeated measurements. The patellofemoral pressure was tested in a total of nine cadaveric knees. The outcome pressures for each treatment group are presented as a mean pressure of all nine knees relative to the mean pressure of the intact knees at 15° flexion.
Statistical analysis
The pressure outcomes of each treatment were presented as relative mean pressure ± standard error of mean (SEM) of the nine knees compared to the mean pressure of the intact knees at 15° flexion, which were designated a value of 1. The student’s t test was used to compare the three osteotomies against the intact knees at each flexion angle, with significance determined by P values less than 0.05.
Results
Patellofemoral contact pressure
Contact pressure in the patellofemoral joint space was analysed at 15°, 30°, 60°, 90°, and 120° knee flexion angles following sequential distal medial opening, proximal medial opening, and lateral closing wedge high tibial osteotomy in cadaveric knees (Fig. 4). The relative cartilage pressure of the intact knees started at 1.0 ± 0.09 at 15° flexion, before peaking at 3.25 ± 0.15 at 90° to exhibit a maximal 325% pressure increase, then dropping to 2.85 ± 0.14 at 120°. Pressure following lateral closing wedge osteotomy started at 1.14 ± 0.10 at 15° flexion, before peaking at 3.01 ± 0.13 at 90° to exhibit a maximal 301% pressure increase, then dropping to 3.00 ± 0.08 at 120°. Proximal opening wedge osteotomy cartilage pressure started at 1.54 ± 0.17 at 15° flexion, before peaking at 4.11 ± 0.16 at 60° to exhibit a maximal 411% pressure increase, then dropping to 3.16 ± 0.08 at 120°. The distal opening wedge osteotomy technique produced a cartilage pressure of 1.26 ± 0.13 at 15° flexion, before peaking at 3.35 ± 0.07 at 90° to exhibit a maximal 335% pressure increase, then dropping to 3.12 ± 0.12 at 120° (Fig. 4).
Relative patellofemoral pressures at 15°, 30°, 60° and 90° flexion following lateral closing HTO, proximal tuberosity medial opening HTO, and distal tuberosity medial opening HTO. Both distal tuberosity medial opening HTO and lateral closing HTO did not show a significant difference (P > 0.05) to the intact knee at all flexion angles. In contrast, the proximal tuberosity medial opening HTO technique showed a significant increase in patellofemoral pressure at 30° (P < 0.05), 60° (P < 0.005), and 90° (P < 0.0005) knee flexion. All pressures presented as mean pressure relative to the intact knee at 15°, designated a value of 1. All values presented as mean ± SEM. *P < 0.05, **P < 0.005, ***P < 0.0005
The cartilage pressure following PTO opening wedge technique was significantly increased at 15° (P < 0.05), 30° (P < 0.005), and 60° (P < 0.0005) flexion when compared to the intact knee. The difference was not significant at 90° and 120°. In contrast to the proximal opening wedge technique, cartilage pressure following distal opening wedge osteotomy and closing wedge was not significantly (P > 0.05) different to the intact knee at all flexion angles.
Discussion
OWHTO is commonly accepted as a clinically effective procedure, but is plagued by postoperative complication. Specifically, patella infera following medial OWHTO with proximal tibial osteotomy (PTO) can predispose to anterior knee pain, crepitus, and reduced range of motion [12, 18, 23, 36, 53, 56, 64]. Although technical refinements [21, 24, 50, 56, 62, 64] have been trialed to decrease patella infera incidence, they are subject to considerations such as the size of correction and their effect on union [50]. Furthermore, PTO OWHTO produces a significant alteration in cartilage pressure, a factor linked to the degeneration of joint cartilage [2, 5, 10, 59]. This paper has elucidated that whilst PTO OWHTO produces a significant elevation in cartilage pressure, distal tibial osteotomy (DTO OWHTO) and closing wedge osteotomy produce no significant patellofemoral pressure change compared to the intact knee.
Many surgeons favor a lateral closing wedge HTO for treating varus tibiofemoral malignment, with up to 71% good results reported at 8 years follow-up [11, 31, 42]. But it should be noted that the procedure is limited by complications such as medial collateral ligament instability, patella infera, loss of correction, delayed union and nonunion, fracture, and arthrofibrosis [7, 16, 26, 33, 44, 48, 54, 62, 63]. Whilst complications following medial opening wedge HTO have also been illustrated, the frequency appears reduced and clinical outcomes are generally comparable to the closing wedge technique [1, 25, 26, 40, 41, 43, 60]. However, opening wedge osteotomy is clearly set apart by its reduced comparative invasiveness; with the closing wedge procedure relying on extensor muscle separation for the fibular osteotomy, and the risk of peroneal nerve palsy following fibula osteotomy. Asides from bypassing these issues, opening wedge osteotomy has the additional benefit of allowing coronal and sagittal corrections intraoperatively to optimize loading axis transmission through the knee. In order to clarify the more effective technique, the authors believe more research into comparative outcomes and complications such as patella infera are warranted.
Patella infera might not only accelerate cartilage degeneration through an increase in patellofemoral load, but also through a change in normal knee kinematics. As suggested by Andriacchi et al. [5, 10], this loss of load-bearing homeostasis in PTO OWHTO may translate to an inferior shift of patellofemoral pressure from an area of high loading and acclimatized coefficient of shear friction, to an area of low loading, causing mechanical injury to the newly loaded cartilage and inferring an exacerbated coefficient of shear friction that heightens the susceptibility to degeneration [5]. Given the fact that joint areas with low contact pressure and infrequent load-bearing are more sensitive to mechanical injury and cartilage loss [5, 8, 10], this inferior alteration in joint kinematics may have a two-fold effect on degeneration of the joint surface. It is likely that not only would the newly loaded area be susceptible to degeneration, but adhering to Wolff’s Law and the well known compression-induced maintenance of articular cartilage matrix metabolism, the previously loaded area may experience cartilage degeneration by aberrant subchondral bone remodeling and/or an imbalance between the anabolic and catabolic regulators of cartilage matrix. Indeed, various studies have documented the link between abnormal pressure and osteoarthritis [8, 10, 17, 32, 47, 58, 61].
Additionally, patella infera has been documented by several groups as a common complication of OWHTO for valgus correction of medial compartment osteoarthritis in the knee [18, 49, 53, 56, 63, 64]. Patella infera and early tendofemoral moment are thought to commonly result in anterior knee pain after conventional OWHTO. It should be noted however that whilst anterior knee pain is reported as an OWHTO complication within the literature, Mont et al. [46] found that patella infera did not affect clinical outcome, although the criteria used to determine patella infera (Insall-Salvati ratio less than 1.0) was less stringent than used by Windsor et al. [63] who reported 80% patella infera in their osteotomized cohort. Whilst the clinical significance of patella infera may not be well established [25, 53, 64], the exaggerated technical difficulty of total knee arthroplasty (TKA) subsequent to HTO certainly is. To this end, numerous authors have commented on the difficulty of revision to TKA after HTO, with concern mainly surrounding deformities of the proximal part of the tibia, patellar eversion, and soft tissue imbalances [4, 9, 27, 34, 37, 46, 57, 63]. Whilst further research is needed to confirm any conclusions drawn from this study, we believe distal opening wedge osteotomy or closing wedge osteotomy may reduce or prevent many of these complications, particularly deformation of the proximal tibia.
Whilst the findings of this study are clinically important to the safety and efficacy of correcting valgus tibiofemoral deformities, there are two limitations in this experiment worthy of discussion. Firstly, previous studies have predominantly used Tekscan pressure-sensitive films as a measurement device [2, 15], while this study used a Pedar™ system. The main difference in these two systems is that Tekscan films are 0.1 mm thick, whereas the Pedar™ sensor system is closer to 1 mm. The exact consequence of this increased sensor thickness is unclear, but we believe the raw pressure data in the present study has been altered to a small degree through the thickness of the sensor system. But in acknowledging this fact, our raw pressure data was similar to previously published data with Tekscan film [15, 28, 38, 39]. Secondly, the angle of correction made in this study was relatively large compared to that commonly observed [12, 13, 20, 53]. Gaasbeck [18] recently reported that the larger the correction angle made in OWHTO, the lower the resulting patella height. Therefore, we would expect a quantitatively smaller effect on patellofemoral cartilage pressure in smaller correction procedures, a hypothesis consistent with that of Mont et al. [45].
A successful HTO outcome relies on proper patient selection, stage of arthrosis, and the precision and maintenance of adequate operative correction [6, 25, 44, 48, 52]. Regarding the precision of the correction, we see an indication for lateral closing wedge osteotomy in patients with severe osteoarthritis of the medial compartment combined with an increased posterior tibial slope. A medial opening wedge osteotomy above the tuberosity should be considered only in cases with patella alta. In all other cases, we favor the medial opening wedge technique with a biplanar osteotomy below the tibial tuberosity (DTO). Additionally, larger correction angles are not contraindicated for the opening osteotomy, since an increase in medial compartment pressure can be avoided by releasing the superficial portion of the medial collateral ligament. Importantly, the deep portion of the medial collateral ligament (the stabilizing portion) remains intact. In the case of a concurrent anterior cruciate ligament reconstruction, the opening wedge osteotomy has the advantage of being quicker than the lateral closing wedge osteotomy, although one should take care not to increase posterior slope in this case since this would increases stress on the reconstructed ligament [14].
Given the relative advantages of DTO OWHTO compared to the traditional lateral closing wedge osteotomy (less invasiveness, shorter operation time, higher precision for correction, no risk of peroneal nerve palsy) [35, 40] and to the PTO OWHTO (maintenance of patellofemoral cartilage pressure with the possible prophylactic effect of this on cartilage degeneration), we recommend this technique for valgus correction of medial compartment osteoarthritis, specially in those with pre-existing anterior knee pain, either due to patella infera or patello femoral arthritic changes.
References
Adili A, Bhandari M, Giffin R, Whately C, Kwok DC (2002) Valgus high tibial osteotomy comparison between an Ilizarov and a Coventry wedge technique for the treatment of medial compartment osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 10:169–176
Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P (2004) Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees Winner of the AGA-DonJoy award 2004. Arch Orthop Trauma Surg 124:575–84
Ahmed (1988) The effect of quadriceps tension characteristics on the patellar tracking pattern. In: Presented at 34th annual meeting ORS, Atlanta
Amendola A, Rorabeck CH, Bourne RB, Apyan PM (1989) Total knee arthroplasty following high tibial osteotomy for osteoarthritis. J Arthroplasty 4(Suppl):S11–S17
Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S (2004) A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng 32:447–457
Berman AT, Bosacco SJ, Kirshner S, Avolio A Jr (1991) Factors influencing long-term results in high tibial osteotomy. Clin Orthop Relat Res 192–208
Brouwer RW, Bierma-Zeinstra SM, van Koeveringe AJ, Verhaar JA (2005) Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br 87:1227–1232
Bullough PG (1992) The pathology of osteoarthritis. WB Saunders, Philadelphia, pp 39–69
Cameron HU, Park YS (1996) Total knee replacement following high tibial osteotomy and unicompartmental knee. Orthopedics 19:807–808
Carter DR, Beaupre GS, Wong M, Smith RL, Andriacchi TP, Schurman DJ (2004) The mechanobiology of articular cartilage development and degeneration. Clin Orthop Relat Res S69–S77
Coventry MB (1979) Upper tibial osteotomy for gonarthrosis. The evolution of the operation in the last 18 years and long term results. Orthop Clin North Am 10:191–210
Coventry MB, Bowman PW (1982) Long-term results of upper tibial osteotomy for degenerative arthritis of the knee. Acta Orthop Belg 48:139–156
Coventry MB, Ilstrup DM, Wallrichs SL (1993) Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am 75:196–201
Dejour H, Neyret P, Boileau P, Donell ST (1994) Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthop Relat Res 220–228
Elias JJ, Wilson DR, Adamson R, Cosgarea AJ (2004) Evaluation of a computational model used to predict the patellofemoral contact pressure distribution. J Biomech 37:295–302
Engel GM, Lippert FG 3rd (1981) Valgus tibial osteotomy: avoiding the pitfalls. Clin Orthop Relat Res 137–143
Flahiff CM, Kraus VB, Huebner JL, Setton LA (2004) Cartilage mechanics in the guinea pig model of osteoarthritis studied with an osmotic loading method. Osteoarthritis Cartilage 12:383–388
Gaasbeek RD, Sonneveld H, van Heerwaarden RJ, Jacobs WC, Wymenga AB (2004) Distal tuberosity osteotomy in open wedge high tibial osteotomy can prevent patella infera: a new technique. Knee 11:457–461
Gill TJ, DeFrate LE, Wang C, Carey CT, Zayontz S et al (2003) The biomechanical effect of posterior cruciate ligament reconstruction on knee joint function. Kinematic response to simulated muscle loads. Am J Sports Med 31:530–536
Goutallier D, Hernigou P, Medevielle D, Debeyre J (1986) Outcome at more than 10 years of 93 tibial osteotomies for internal arthritis in genu varum (or the predominant influence of the frontal angular correction). Rev Chir Orthop Reparatrice Appar Mot 72:101–113
Goutallier D, Julieron A, Hernigou P (1992) Cement wedge replacing iliac graft in tibial wedge osteotomy. Rev Chir Orthop Reparatrice Appar Mot 78:138–144
Hasler EM, Herzog W (1998) Quantification of in vivo patellofemoral contact forces before and after ACL transection. J Biomech 31:37–44
Hernigou P, Goutallier D (1987) Outcome of the femoropatellar joint in osteoarthritic genu varum after tibial wedge osteotomy for angulation 10 to 13 year regression. Rev Chir Orthop Reparatrice Appar Mot 73:43–48
Hernigou P, Ma W (2001) Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee 8:103–110
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 69:332–354
Hoell S, Suttmoeller J, Stoll V, Fuchs S, Gosheger G (2005) The high tibial osteotomy, open versus closed wedge, a comparison of methods in 108 patients. Arch Orthop Trauma Surg 125:638–643
Hofmann AA, Kane KR (1994) Total knee arthroplasty after high tibial osteotomy. Orthopedics 17:887–890
Huberti HH, Hayes WC (1984) Patellofemoral contact pressures The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am 66:715–724
Hughston JC, Deese M (1988) Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med 16:383–388
Insall JN (1981) Patella pain syndromes and chondromalacia patellae. Instr Course Lect 30:342–356
Insall JN, Joseph DM, Msika C (1984) High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am 66:1040–1048
Islam N, Haqqi TM, Jepsen KJ, Kraay M, Welter JF et al (2002) Hydrostatic pressure induces apoptosis in human chondrocytes from osteoarthritic cartilage through up-regulation of tumor necrosis factor-alpha, inducible nitric oxide synthase, p53, c-myc, and bax-alpha, and suppression of bcl-2. J Cell Biochem 87:266–278
Jackson JP, Waugh W (1974) The technique and complications of upper tibial osteotomy. A review of 226 operations. J Bone Joint Surg Br 56:236–245
Jackson M, Sarangi PP, Newman JH (1994) Revision total knee arthroplasty. Comparison of outcome following primary proximal tibial osteotomy or unicompartmental arthroplasty. J Arthroplasty 9:539–542
Jakob RP, Jacobi M (2004) Closing wedge osteotomy of the tibial head in treatment of single compartment arthrosis. Orthopade 33:143–152
Kaper BP, Bourne RB, Rorabeck CH, Macdonald SJ (2001) Patellar infera after high tibial osteotomy. J Arthroplasty 16:168–173
Katz MM, Hungerford DS, Krackow KA, Lennox DW (1987) Results of total knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Joint Surg Am 69:225–233
Li G, DeFrate LE, Zayontz S, Park SE, Gill TJ (2004) The effect of tibiofemoral joint kinematics on patellofemoral contact pressures under simulated muscle loads. J Orthop Res 22:801–806
Li G, Park SE, DeFrate LE, Schutzer ME, Ji L et al (2005) The cartilage thickness distribution in the tibiofemoral joint and its correlation with cartilage-to-cartilage contact. Clin Biomech (Bristol, Avon) 20:736–744
Lobenhoffer P, Agneskirchner J, Zoch W (2004) Open valgus alignment osteotomy of the proximal tibia with fixation by medial plate fixator. Orthopade 33:153–160
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11:132–138
Lootvoet L, Massinon A, Rossillon R, Himmer O, Lambert K, Ghosez JP (1993) Upper tibial osteotomy for gonarthrosis in genu varum. Apropos of a series of 193 cases reviewed 6 to 10 years later. Rev Chir Orthop Reparatrice Appar Mot 79:375–384
Marti RK, Verhagen RA, Kerkhoffs GM, Moojen TM (2001) Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am 83-A:164–170
Matthews LS, Goldstein SA, Malvitz TA, Katz BP, Kaufer H (1988) Proximal tibial osteotomy. Factors that influence the duration of satisfactory function. Clin Orthop Relat Res 193–200
Mont MA, Alexander N, Krackow KA, Hungerford DS (1994) Total knee arthroplasty after failed high tibial osteotomy. Orthop Clin North Am 25:515–525
Mont MA, Antonaides S, Krackow KA, Hungerford DS (1994) Total knee arthroplasty after failed high tibial osteotomy. A comparison with a matched group. Clin Orthop Relat Res 125–30
Morrell KC, Hodge WA, Krebs DE, Mann RW (2005) Corroboration of in vivo cartilage pressures with implications for synovial joint tribology and osteoarthritis causation. Proc Natl Acad Sci USA 102:14819–14824
Naudie D, Bourne RB, Rorabeck CH, Bourne TJ (1999) The Install Award. Survivorship of the high tibial valgus osteotomy A 10- to -22-year followup study. Clin Orthop Relat Res 18–27
Noda T, Yasuda S, Nagano K, Takahara Y, Namba Y, Inoue H (2000) Clinico-radiological study of total knee arthroplasty after high tibial osteotomy. J Orthop Sci 5:5–36
Noyes FR, Mayfield W, Barber-Westin SD, Albright JC, Heckmann TP (2006) Opening wedge high tibial osteotomy: an operative technique and rehabilitation program to decrease complications and promote early union and function. Am J Sports Med 34(8):1262–1273
Powers CM, Lilley JC, Lee TQ (1998) The effects of axial and multi-plane loading of the extensor mechanism on the patellofemoral joint. Clin Biomech (Bristol, Avon) 13:616–624
Rudan JF, Simurda MA (1990) High tibial osteotomy. A prospective clinical and roentgenographic review. Clin Orthop Relat Res 251–256
Scuderi GR, Windsor RE, Insall JN (1989) Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am 71:245–248
Shea JD (1973) Osteoarthrosis of the knee: diagnosis and complications of treatment by high tibial osteotomy. South Med J 66:1030–1034
Stoffel K, Stachowiak G, Kuster M (2004) Open wedge high tibial osteotomy: biomechanical investigation of the modified Arthrex Osteotomy Plate (Puddu Plate) and the TomoFix Plate. Clin Biomech (Bristol, Avon) 19:944–950
Tigani D, Ferrari D, Trentani P, Barbanti-Brodano G, Trentani F (2001) Patellar height after high tibial osteotomy. Int Orthop 24:331–334
Toksvig-Larsen S, Magyar G, Onsten I, Ryd L, Lindstrand A (1998) Fixation of the tibial component of total knee arthroplasty after high tibial osteotomy: a matched radiostereometric study. J Bone Joint Surg Br 80:295–297
Trindade MC, Shida J, Ikenoue T, Lee MS, Lin EY et al (2004) Intermittent hydrostatic pressure inhibits matrix metalloproteinase and pro-inflammatory mediator release from human osteoarthritic chondrocytes in vitro. Osteoarthr Cartil 12:729–735
Vanwanseele B, Eckstein F, Knecht H, Stussi E, Spaepen A (2002) Knee cartilage of spinal cord-injured patients displays progressive thinning in the absence of normal joint loading and movement. Arthr Rheum 46:2073–2078
Warden SJ, Morris HG, Crossley KM, Brukner PD, Bennell KL (2005) Delayed- and non-union following opening wedge high tibial osteotomy: surgeons’ results from 182 completed cases. Knee Surg Sports Traumatol Arthrosc 13:34–37
Westacott CI, Urban JP, Goldring MB, Elson CJ (2002) The effects of pressure on chondrocyte tumour necrosis factor receptor expression. Biorheology 39:125–132
Westrich GH, Peters LE, Haas SB, Buly RL, Windsor RE (1998) Patella height after high tibial osteotomy with internal fixation and early motion. Clin Orthop Relat Res 169–174
Windsor RE, Insall JN, Vince KG (1988) Technical considerations of total knee arthroplasty after proximal tibial osteotomy. J Bone Joint Surg Am 70:547–555
Wright JM, Heavrin B, Begg M, Sakyrd G, Sterett W (2001) Observations on patellar height following opening wedge proximal tibial osteotomy. Am J Knee Surg 14:163–173
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stoffel, K., Willers, C., Korshid, O. et al. Patellofemoral contact pressure following high tibial osteotomy: a cadaveric study. Knee Surg Sports Traumatol Arthr 15, 1094–1100 (2007). https://doi.org/10.1007/s00167-007-0297-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-007-0297-9