Abstract
Purpose
It remains unclear what the contribution of the PCL is in total knee arthroplasty (TKA). The goal of this study was to investigate the influence of the PCL in TKA in relationship to clinical outcome, strength and proprioception.
Methods
Two arthroplasty designs were compared: a posterior cruciate-substituting (PS) and a posterior cruciate-retaining (CR) TKA. A retrospective analysis was performed of 27 CR and 18 PS implants with a minimum of 1 year in vivo. Both groups were compared in terms of clinical outcome (range of motion, visual analogue scale for pain, Hospital for Special Surgery Knee Scoring system, Lysholm score and Knee Injury and Osteoarthritis Outcome Score), strength (Biodex System 3 Dynamometer®) and proprioception (balance and postural control using the Balance Master system®). Each design was also compared to the non-operated contralateral side in terms of strength and proprioception.
Results
There were no significant differences between both designs in terms of clinical outcome and strength. In terms of proprioception, only the rhythmic weight test at slow and moderate speed shifting from left to right was significant in favour of the CR design. None of the unilateral stance tests showed any significant difference between both designs. There was no difference in terms of strength and proprioception between the operated side and the non-operated side.
Conclusion
Retaining the PCL in TKA does not result in an improved performance in terms of clinical outcome and proprioception and does not show any difference in muscle strength.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The PCL plays a role in stability and proprioception of the knee joint. These proprioceptive capacities have been attributed to the presence of mechanoreceptors, which finally result in dynamic stability of the joint [12, 19, 21, 30–32, 34–36].
In total knee arthroplasty, currently two main designs of primary total knee arthroplasty are used: a PCL-retaining (CR) and a PCL-substituting (PS) design. Proponents of PCL retention refer to a theoretical increase in femoral rollback, improved knee kinematics and more proprioception. This would potentially contribute to an increase in patient satisfaction and patient perceived function [1, 9, 13, 16, 29, 33, 37, 41].
Despite the fact that partial restoration of joint sensation after TKA has been demonstrated using CR knees the isolated contribution and functional role of the PCL remains uncertain, as many structures contribute to proprioception: the collateral ligaments, the joint capsule, the periost, the cruciate ligaments, the interosseous membranes, the muscles and the skin [3, 4, 8, 10, 16, 17, 25, 39, 43–45]. Proprioception is defined as the sense of position, movement and balance [39]. In previous studies, proprioception between CR and PS designs has been measured for active or passive movement sense [3, 8, 17, 25, 39, 43, 45]. However, these tests do not challenge a person’s capacity to control skilled activities, and this can be analysed by testing balance and postural control, which are two other characteristics of proprioception. When evaluating balance and postural control, unilateral and bilateral stance with eyes open and closed on different supporting surfaces can be tested. However, in those tests the vestibular organ also plays a role in the proprioceptive pathways [42].
So far, clinical data does not seem to support retention of the PCL [5, 18, 22, 23, 26–29, 32], and in order to have a complete functional analysis of the knee, strength should be analysed using isokinetic muscle testing [6, 7]. Since mechanoreceptors react to loads by a reflex-efferent response with muscle activation, a reduction in muscle activation could cause a loss of muscle strength, which might lead to instability of the knee [11]. In that way, substituting the PCL could lead to a loss of muscle strength. However, so far, no correlation has been shown between proprioception and muscle strength.
The aim of this study was to perform a functional comparison between CR and PS TKA within a single patient population. Clinical outcome, proprioception (balance and postural control) and strength of a cruciate-retaining and a cruciate-substituting TKA design were both compared to each other and to the non-operated side. An attempt was made to find a correlation between muscle strength and proprioception as well.
Materials and methods
All patients who underwent TKA between 2006 and 2009 at the Department of Orthopaedic Surgery in Roeselare were screened retrospectively for inclusion and exclusion criteria. Indications for TKA were end-stage osteoarthritis without inflammatory OA. A single system of knee prosthesis (Scorpio®, Stryker, Kalamazoo, Michigan, USA) was used for all cases. All patients underwent surgery by the senior author (L.VDD), using a measured resection technique. In the CR group, the PCL was protected with the use of an osteotome anteriorly from the PCL insertion. The decision whether to resect the PCL was made preoperatively. The PCL was substituted when balancing the gaps was insufficient: a tight flexion gap and in severe varus and valgus patients. The femoral and tibial component was cemented, the patella was resurfaced, and the polyethylene was fixed bearing. All patients underwent the same post-operative rehabilitation programme.
Exclusion criteria for the study were as follows: vestibular deficiencies, neurological deficiencies or prior history of neurological impairment (such as a cerebrovascular accident), metabolic disease (such as diabetes mellitus) and any other type of orthopaedic surgery of the lower extremities or spine apart from the TKA. In order to compare the operated side to the contralateral side, locomotoric symptoms at the contralateral and ipsilateral (above and below the TKA) limb should at least be minimal and not interfering with activity daily living (ADL). In order to exclude any post-operative interference, all knees were evaluated at a minimum of 1 year after TKA.
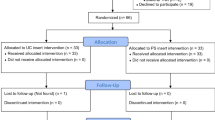
Forty-five patients were identified, of which 27 patients had a cruciate-retaining (CR) and 18 patients a cruciate-substituting (PS) design, matched the criteria and all consented for the study.
Patients were evaluated clinically, for proprioception and for strength.
Clinical assessment
The clinical outcome was scored by assessing range of motion and several clinical scores: the Knee Injury and Osteoarthritis Outcome Score (KOOS), the Hospital for Special Surgery score (HSS), the Lysholm score and the visual analogue scale for pain (VAS). Patients were also asked whether they felt a click in their TKA and whether that was painful.
Assessment of proprioception and balance
Proprioception was evaluated in terms of balance and postural control using the Balance Master system® (Neurocom, Clackamas, OR, USA) [30, 42]. This is a computerized dual-force plate system that allows measurement of the vertical forces exerted by the patient’s lower limb. It provides real-time information on movement and the centre of gravity (COG), scaled according to their height, with visual biofeedback to the patient. Analyses of postural control and balance consisted of five different subtests:
-
1.
Weight-bearing squat (WBS) measures the percentage of body weight undergone by each leg consecutively while standing erect, and then, squatting in three positions of knee flexion (30°, 60° and 90°). All subjects were instructed to try to maintain equal weight on the two legs at all time. We compared the CR and PS TKA for both the operated side (OS) and the non-operated side (N-OS)
-
2.
In the modified Clinical Test of Sensory Interaction on Balance (mCTSIB), subjects need to keep their balance in a bilateral standing position in four different conditions: standing on firm surface (FS) and unstable surface (US) (foam), consecutively with their eyes open (EO) and eyes closed (EC). The postural sway velocity is measured (degrees per second).
-
3.
The unilateral stance test (UST) quantifies postural sway velocity (degrees per second) with subjects standing on either the operated or non-operated side, with eyes open (EO) and with eyes closed (EC). For this test, we compared the CR versus the PS group. Each design was analysed to the non-operated side as well. Finally, we analysed the normalized values of the PS and the CR group to each other. This normalized value is considered as the ratio of the operated side to the non-operated side, i.e. using the non-operated side as a control group.
-
4.
The limits of stability test (LOS) quantifies the maximum distance participants can lean their bodies in a given direction without losing balance. Eight targets distributed from a central point are displayed on a screen in front of the participants. These targets represent the maximum theoretical distance, according to their height, which the participants should be able to reach without losing their balance. The direction of the test was forward, backward left and right. Instead of measuring out left and right, we measured out the movement towards the operated side. Targets were highlighted in random order on the screen, and participants were asked to shift their body as far as possible in the direction of the consecutive targets without losing their balance. Four parameters were calculated:
-
(a)
Reaction time (RT) is the time in seconds between the command to move and the patient’s first movement.
-
(b)
Movement velocity (MVL) is the average speed of movement in degrees per second.
-
(c)
Endpoint excursion (EPE) is the percentage of distance reached in relation to the total distance from the centre to the target.
-
(d)
Directional control (DC) is a comparison of the amount of movement in the intended direction (towards the target) to the amount of extraneous movement (away from the target).
-
(a)
-
5.
The rhythmic weight shift test (RWS) quantifies the subject’s ability to rhythmically move their COG from the left to the right and forward to backward at three different speeds: slow, moderate and fast. This is a bilateral stance test in which velocity (degrees per second) and directional controls are measured for both directions.
All tests were conducted by a single, experienced examiner; blinded to the type of arthroplasty.
Assessment of strength
Concentric knee extensor and flexor strength were evaluated using a Biodex System 3 Dynamometer® (Biodex Medical, Shirley, NY, USA). An isokinetic strength test of both extensors (quadriceps) and flexors (hamstrings) was conducted at angular velocities of 60° and 180° per second. All subjects warmed up for testing by 10 min on an exercise bike with low resistance at 60 rpm. Subjects were then seated on the Biodex system with their back supported in a comfortable position and pelvis and thigh stabilized by straps. The range of motion tested was set at 0°–90° of knee flexion.
Subjects were provided instructions using a standardized script, and the importance of maximum effort was emphasized. All participants were given three submaximal practice trials and a subsequent rest period of 30 s before actual testing began.
Each test at 60 and 180°/s velocity consisted of three efforts at maximal contraction with a rest period of 30 s between each effort. The maximal value (peak torque) of knee extensor and flexor strength at both angle velocities were recorded and used to calculate the hamstrings/quadriceps ratio (H/Q). In all subjects, the tests were performed on both knees. The non-operated side was tested first. All the tests were conducted by a single, experienced examiner; blinded to the type of arthroplasty.
Several data were compared. PS design versus CR design was analysed for peak torque of the quadriceps and hamstrings and for the H/Q ratio. The H/Q ratio was also investigated between TKA versus non-operated side within PS and CR group and between the PS design and CR design, relative to the non-operated side (normalized values).
Approval for the study was obtained at Stedelijk Ziekenhuis (Roeselare, Belgium) by the ethical board. All patients signed an informed consent.
Statistical analysis
All statistical analyses were computed with use of SPSS 19.0 (SPSS Inc., Chicago, Illinois). Analysis of variance and independent samples t-tests were used to compare mean values of continuous variables. Independent non-parametric Mann–Whitney U and Wilcoxon signed-rank tests were used to evaluate the difference between patient groups (CR vs PS) in terms of the different continuous variables. The level of significance was set on 0.05.
Results
Both groups of TKA design were similar. The mean age was 70.5 years (SD 6.4, range 55.9–82.5) for the CR group and 68.0 years (SD 8.4, range 49.0–78.9) for the PS group. The mean time between surgery and analysis was 2.9 years (SD 0.8, range 1.5–4.4) for the CR group 3.1 years (SD 0.8, range 2.0–4.5) for the PS group. The male/female ratio was 0.33 in the CR group and 0.55 in the PS group.
Clinical outcome (Table 1)
There was no statistical significance in any of the clinical scores, nor was there a significant difference in range of motion. No significant difference was noted in clicking sensation between CR and PS group, and none of the clicks were considered painful.
Proprioception and balance
All outcomes were statistically analysed comparing CR and PS designs (Tables 2, 3). Two tests showed a significant difference in favour of CR knees: the velocity when moving to the left and right on slow (p = 0.01) and moderate (p = 0.03) speeds in the RWS test showed statistically higher speeds for the CR design. As for the USTs, no significant difference was seen in results within the CR or the PS design.
When comparing the normalized values of both designs in the UST, no statistical significance was shown with the eyes open test and the eyes closed test. Comparison of both TKA designs to the non-operated contralateral leg in that same UST revealed no significant differences as well.
Strength
Isokinetic strength revealed no statistical difference between the PS and CR design. There was no difference with the contralateral side for the CR or the PS design (Table 4).
Comparing the normalized values (operated side relative to the non-operated side) of the H/Q ratios of the CR group versus the PS group did not show any significant difference in outcome as well.
Finally, no difference was seen when comparing the ratio of H/Q for the CR and PS TKA to the non-operated side.
Discussion
In this study, in which an extensive comparison between CR and PS design in terms of proprioception (postural control and balance), strength and clinical outcome was performed, the most important finding is that no difference was seen between CR and PS implants in primary TKA.
The clinical outcome results in this study are comparable to recent studies and meta-analysis [5, 18, 22, 23, 26–28, 32]. While a large, prospective randomized study by Kim et al. did not reveal any difference in range of motion, three meta-analyses did found a significant difference in favour of the posterior-stabilized implants. In our study, we could not reveal any superiority of range of motion of one design over another. Several authors have suggested that retaining the PCL in TKA contributes to proprioception leading to an increase in patient satisfaction and a more ‘normal’ feeling after TKA [1, 9, 13, 16, 29, 37, 41]. However, based on our results and other studies performed, there is insufficient evidence supporting this hypothesis [7, 8, 15, 25, 39, 43, 44]. Equivalence was found in all statistical tests, except for two showing significance in favour of the CR design. This test was a bilateral stance test in which the speed of movement towards an object was defined.
Since the non-operated side can be eliminated in the UST, this test was probably the most important one comparing the two TKA designs. In that test, it was possible to compare both designs to each other and compare each design with the control side as well. No statistical difference between both designs was revealed. As mentioned, the contralateral native knee was used as a control. It has been shown that proprioception is diminished in osteoarthritic joints and taking into account the average age of our population, there will likely be some kind of degeneration at the spine or the contralateral lower limb [3, 4, 24]. However, standing plain radiographs of the spine or the contralateral limb in order to objectify any osteoarthritic deficiencies were not performed. This might influence our results. An effort was made to reduce this selection bias by only including these patients with no or minimal complaints at the contralateral side, with no interference in ADL [20, 40]. Comparing both the operated and non-operated side made it possible to normalize the values for proprioception and strength of the PS and the CR group, using the non-operated side as a control group. However, none of the results of these normalized values showed any significant difference in proprioception and strength.
Although mechanoreceptors have been demonstrated in the PCL of arthritic knees and in specimens after CR-TKA, no clinical trials have been able to prove the functional and proprioceptive role of the PCL in TKA [46]. The results from our USTs demonstrate that proprioceptive capacities in TKA do recover to at least the state of the non-operated side. But despite this recovery in proprioception, our other analyses comparing PS and CR designs clarify that the PCL does not seem contribute to it. These findings are in line with the results from previous studies [7, 8, 25, 39, 43, 44]. In arthritic knees, several factors have shown to influence proprioception: inflammation, pain, joint laxity, diminished joint space and a loss of mechanoreceptors [19, 20, 38, 40]. Proprioception after TKA seems to depend on structures around the knee other than the PCL, such as the collateral ligaments, the peri-articular muscle tendons and the joint capsule [43]. Based on the obtained results in this study, restoration of the joint space and adequately retensioning of the joint capsule and ligaments by appropriate balancing the TKA will restore the proprioceptive capacities and knee joint function, rather than the preservation of the PCL [2, 44].
As for strength, our results do not support a possible decrease in strength when substituting the PCL in TKA. There was no difference in outcome of strength between both designs as compared to the control group, which is in line with previous studies [7, 15].
In the past, several studies have been performed to compare proprioception between PS and CR designs [8, 17, 25, 39, 43–45]. Although these results are variable, they suggest that the PCL does not contribute to proprioception [8, 17, 25, 39, 43]. Yet, these studies have shown to have some weaknesses of which our study tried to anticipate on. Two studies evaluated two different total knee systems while taking only a good clinical result into account. Moreover, they also tested proprioception in a passive way, which has been shown to be less reliable and has large interval tolerance compared to active tests [14, 42]. Iisshii in 1997 and Lattanzio in 1998 published retrospective studies with a limited patient population, but they did test proprioception actively, using an electrogoniometer [17, 25]. Swanik et al. published on 20 knees, comparing both designs 1.5 months before and 6 months after TKA [43]. Although the study was prospective, the short-term follow-up might interfere with post-operative rehabilitation and influence results [31].
Despite the fact that the biggest weakness of the present study is the retrospective and the non-randomized character, it is believed that this study has several advantages.
Compared with previous studies, reporting on proprioception and strength, this study was able to investigate a large population, in which proprioception was analysed in an active way. Instead of movement sense and joint position, this study tested another characteristic of proprioception between CR and PS designs: balance and postural control. In order to avoid bias on proprioception, very strict inclusion and exclusion criteria were used. These criteria were necessary and made it possible to investigate bilateral and USTs, to compare the operated and non-operated side and to lower the possible interference of other structures in process of proprioception (such as the spine, hips, ankles and vestibular organ).
This study compared strength, proprioception and clinical outcome between CR and PS knees versus a control group. Despite our inclusion and exclusion criteria, this study did not only address TKA’s with a good clinical result, which made it possible not to rely on the outcome of patients to perform tests for strength and proprioception. A minor result after CR or PS TKA might indeed influence results negatively, but this needs to be taken into account when evaluating both groups. The present study was able to compare outcome, proprioception and strength between both the PS and CR group and compare proprioception and strength between the operated side and the non-operated side within both designs. Although we did not have any clinical outliers in our control group, we did use normalized values (the ratio of the TKA to the contralateral side) to compare the PS and the CR groups in order to diminish any possible bias. As mentioned before, even these results did not show any significant difference between both groups.
This study does have its limitations. Despite the extensive comparison and large sample size between CR and PS implants compared with previously performed studies, it is retrospective study without randomization. Therefore, further research should focus on prospective randomized studies in order to confirm the findings of our study.
Preserving the PCL in primary TKA does not contribute to a superior result in terms of clinical outcome, strength and proprioception. Proprioception around the knee is complex and many structures contribute it. The PCL alone does not seem to be an important contributor in restoring balance, postural control and strength after primary TKA. Other anatomical structures in the knee and proper gap balancing in extension and flexion seem to have a more important role to it. While proponents of PCL preservation believe that the PCL is crucial for proprioception and patient perceived function, the results of this study could not support this.
Conclusion
Based on our results, retaining the PCL in TKA does not result in an improved performance in terms of clinical outcome, proprioception or muscle strength in CR knees compared with PS knees using the native, contralateral knee as control. The PCL does not seem to play an important role in balance/postural control and strength in TKA. Proprioception after TKA is complex and multivariable and depends most likely on other soft tissue structures of the knee, such as the collateral ligaments, the capsule and the peri-articular muscle tendons.
References
Andriacchi TP, Galante JO (1988) Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty 3(Suppl):S13–S19
Attfield SF, Wilton TJ, Pratt DJ, Sambatakakis A (1996) Soft-tissue balance and recovery of proprioception after total knee replacement. J Bone Joint Surg Br 78:540–545
Barrack RL, Skinner HB, Cook SD, Haddad RJ (1983) Effect of articular disease and total knee arthroplasty on knee joint-position sense. J Neurophysiol 50:684–687
Barrett DS, Cobb AG, Bentley G (1991) Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br 73:53–56
Bercik MJ, Joshi A, Parvizi J (2013) Posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty. J Arthroplasty 28:439–444
Berman AT, Zarro VJ, Bosacco SJ, Israelite C (1987) Quantitative gait analysis after unilateral or bilateral total knee replacement. J Bone Joint Surg Am 69:1340–1345
Bolanos AA, Colizza WA, McCann PD, Gotlin RS, Wootten ME, Kahn BA, Insall JN (1998) A comparison of isokinetic strength testing and gait analysis in patients with posterior cruciate-retaining and substituting knee arthroplasties. J Arthroplasty 13:906–915
Cash RM, Gonzalez MH, Garst J, Barmada R, Stern SH (1996) Proprioception after arthroplasty: role of the posterior cruciate ligament. Clin Orthop Relat Res 331:172–178
Chalidis BE, Sachinis NP, Papadopoulos P, Petsatodis E, Christodoulou AG, Petsatodis G (2011) Long-term results of posterior-cruciate-retaining Genesis I total knee arthroplasty. J Orthop Sci 16:726–731
Del Valle ME, Harwin SF, Maestro A, Murcia A, Vega JA (1998) Immunohistochemical analysis of mechanoreceptors in the human posterior cruciate ligament: a demonstration of its proprioceptive role and clinical relevance. J Arthroplasty 13:916–922
Fisher NM, White SC, Yack HJ, Smolinski RJ, Pendergast DR (1997) Muscle function and gait in patients with knee osteoarthritis before and after muscle rehabilitation. Disabil Rehabil 19:47–55
Franchi A, Zaccherotti G, Aglietti P (1995) Neural system of the human posterior cruciate ligament in osteoarthritis. J Arthroplasty 10:679–682
Fuchs S, Thorwesten L, Niewerth S (1999) Proprioceptive function in knees with and without total knee arthroplasty. Am J Phys Med Rehabil 78:39–45
Good L, Roos H, Gottlieb D, Beynnon B (1999) Joint position sense is not changed after acute disruption of the anterior cruciate ligament. Acta Orthopaedica 70(2):194–198
Huang CH, Lee YM, Liau JJ, Cheng CK (1998) Comparison of muscle strength of posterior cruciate-retained versus cruciate-sacrificed total knee arthroplasty. J Arthroplasty 13:779–783
Insall JN (1988) Presidential address to The Knee Society. Choices and compromises in total knee arthroplasty. Clin Orthop Relat Res 226:43–48
Ishii Y, Terajima K, Terashima S, Koga Y (1997) Three-dimensional kinematics of the human knee with intracortical pin fixation. Clin Orthop Relat Res 343:144–150
Jacobs WCH, Clement DJ, Wymenga AB (2005) Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev. The Cochrane Library, 2005, Issue 4
Johansson H (1991) Role of knee ligaments in proprioception and regulation of muscle stiffness. J Electromyogr Kinesiol 1:158–179
Kaplan FS, Nixon JE, Reitz M, Rindfleish L, Tucker J (1985) Age-related changes in proprioception and sensation of joint position. Acta Orthop Scand 56:72–74
Katonis PG, Assimakopoulos AP, Agapitos MV, Exarchou EI (1991) Mechanoreceptors in the posterior cruciate ligament. Histologic study on cadaver knees. Acta Orthop Scand 62:276–278
Kim Y-H, Choi Y, Kwon O-R, Kim J-S (2009) Functional outcome and range of motion of high-flexion posterior cruciate-retaining and high-flexion posterior cruciate-substituting total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am 91:753–760
Kolisek FR, McGrath MS, Marker DR, Jessup N, Seyler TM, Mont MA, Lowry Barnes C (2009) Posterior-stabilized versus posterior cruciate ligament-retaining total knee arthroplasty. Iowa Orthop J 29:23–27
Koralewicz LM, Engh GA (2000) Comparison of proprioception in arthritic and age-matched normal knees. J Bone Joint Surg Am 82-A:1582–1588
Lattanzio PJ, Chess DG, MacDermid JC (1998) Effect of the posterior cruciate ligament in knee-joint proprioception in total knee arthroplasty. J Arthroplasty 13:580–585
Li N, Tan Y, Deng Y, Chen L (2014) Posterior cruciate-retaining versus posterior stabilized total knee arthroplasty: a meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc 22:556–564
Luo S, Zhao JM, Su W, Li X, Dong G (2012) Posterior cruciate substituting versus posterior cruciate retaining total knee arthroplasty prostheses: a meta-analysis. Knee 19:246–252
Lützner J, Firmbach F-P, Lützner C, Dexel J, Kirschner S (2014) Similar stability and range of motion between cruciate-retaining and cruciate-substituting ultracongruent insert total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-2892-x
Matsumoto T, Kubo S, Muratsu H, Matsushita T, Ishida K, Kawakami Y, Oka S, Matsuzaki T, Kuroda Y, Nishida K, Akisue T, Kuroda R, Kurosaka M (2013) Different pattern in gap balancing between the cruciate-retaining and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2338–2345
Naylor M, Romani W (2006) Test–retest reliability of three dynamic tests obtained from active females using the neurocom balance master. J Sport Rehabil 15(4):326
Nerhus TK, Heir S, Thornes E, Madsen JE, Ekeland A (2010) Time-dependent improvement in functional outcome following LCS rotating platform knee replacement. Acta Orthop 81:727–732
Peters CL, Mulkey P, Erickson J, Anderson MB, Pelt CE (2014) Comparison of total knee arthroplasty with highly congruent anterior-stabilized bearings versus a cruciate-retaining design. Clin Orthop Relat Res 472:175–180
Pierzchała A, Kusz D, Widuchowski J (2005) The role of the posterior cruciate ligament in total knee replacement. Ortop Traumatol Rehabil 7:666–672
Pitman MI, Nainzadeh N, Menche D, Gasalberti R, Song EK (1992) The intraoperative evaluation of the neurosensory function of the anterior cruciate ligament in humans using somatosensory evoked potentials. Arthroscopy 8:442–447
Safran MR, Allen AA, Lephart SM, Borsa PA, Fu FH, Harner CD (1999) Proprioception in the posterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc 7:310–317
Schultz RA, Miller DC, Kerr CS, Micheli L (1984) Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am 66:1072–1076
Scott RD, Volatile TB (1986) Twelve years’ experience with posterior cruciate-retaining total knee arthroplasty. Clin Orthop Relat Res 205:100–107
Sharma L, Pai YC (1997) Impaired proprioception and osteoarthritis. Curr Opin Rheumatol 9:253–258
Simmons S, Lephart S, Rubash H, Borsa P, Barrack RL (1996) Proprioception following total knee arthroplasty with and without the posterior cruciate ligament. J Arthroplasty 11:763–768
Skinner HB, Barrack RL, Cook SD (1984) Age-related decline in proprioception. Clin Orthop Relat Res 184:208–211
Sorger JI, Federle D, Kirk PG, Grood E, Cochran J, Levy M (1997) The posterior cruciate ligament in total knee arthroplasty. J Arthroplasty 12:869–879
Stillman BC (2002) Making sense of proprioception. Physiotherapy 88:667–676
Swanik CB, Lephart SM, Rubash HE (2004) Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am 86:328–334
Wada M, Kawahara H, Shimada S, Miyazaki T, Baba H (2002) Joint proprioception before and after total knee arthroplasty. Clin Orthop Relat Res 403:161–167
Warren PJ, Olanlokun TK, Cobb AG, Bentley G (1993) Proprioception after knee arthroplasty. The influence of prosthetic design. Clin Orthop Relat Res 297:82–187
Zhang K, Mihalko WM (2012) Posterior cruciate mechanoreceptors in osteoarthritic and cruciate-retaining TKA retrievals: a pilot study. Clin Orthop Relat Res 470:1855–1859
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vandekerckhove, PJ.T.K., Parys, R., Tampere, T. et al. Does cruciate retention primary total knee arthroplasty affect proprioception, strength and clinical outcome?. Knee Surg Sports Traumatol Arthrosc 23, 1644–1652 (2015). https://doi.org/10.1007/s00167-014-3384-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3384-8