Abstract
Purpose
To compare different types of knee arthroplasty, in selected patients with a knee score above 80 points, for their post-operative changes in anteroposterior (AP) laxity and proprioception.
Methods
Four groups of each ten patients were tested for AP translation after different types of arthroplasty with a KT-1000 device at 30°, 60° and 90° of flexion. Proprioception of the joint was evaluated by joint position sense with three different tests. Clinical outcome of stability and proprioceptive testing was analysed by comparing the results of three (KSS, KOOS and FJS-12) patient-reported outcome measurement scores (PROMS) for each of the different implant types.
Results
Anteroposterior laxity was observed at 30° and 90° of flexion for the two PS TKA designs included in this study, but not for the UKA or the medial pivot design. All knee designs, except UKA, had an increased laxity at 60° of flexion. Proprioceptive testing was inconclusive. PROMS were not able to identify differences in clinical outcome among different knee designs in these selected patients, despite observed differences in AP laxity.
Conclusion
Increased AP laxity is a result of the surgical procedure in knee arthroplasty. UKA is the only design mimicking native laxity of the knee. A medial pivot design can obtain the same result as UKA at 30° and 90° of flexion, but not at the importantly cited 60° of flexion as tested under non-load-bearing conditions. The clinical relevance of this study is that despite of an important range of AP translations among the different knee designs, good-to-excellent patient-reported outcome was observed within the findings of this study.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arthroplasty surgery comes with the resection of degenerative tissues like damaged cartilage, bone and ligaments and the substitution of these former with metal, polyethylene and constraint devices within the implant. Depending on the type of arthritis and the degree of lower limb deviation, the amount of constraint to restore stability within the joint might be different [25]. The constraint necessary for the treatment of isolated anteromedial arthritis with unicompartmental arthroplasty (UKA) is limited, because the disease process will be less generalized and all the natural ligaments of the knee can be retained. However, when a 30° type II Krackow valgus knee is treated in a rheumatoid arthritis patient, the stretch out of the medial collateral ligament and the necessary soft tissue releases on the concave side might ask for much more constraint [21, 23].
Recent literature has shown that 20–30 % of knee arthroplasty patients are dissatisfied after their surgery [11, 26, 31]. Anteroposterior (AP) instability or lack of proprioception might be some of the factors leading to an “unhappy patient”. In most total knee arthroplasty (TKA) designs, mostly ACL and often PCL are resected and substituted by some design feature increasing the AP constraint [39]. The sagittal plane is overall less studied after knee arthroplasty than the coronal and axial plane. Both with studies about the radiological aspects [24, 30], as with studies about clinical outcome after arthroplasty with alignment corrections in the sagittal plane [42]. This despite of the fact that during gait and weight-bearing activities, the sagittal plane might be as important, if not more important than the former two planes [2].
The clinical importance of AP stability for normal knee kinematics is obvious in the athlete’s knee where since many decades reconstructions of the central pivot are performed [12]. The importance of sagittal stability is less clear in TKA patients. The observation that not so many patients obtain a “Forgotten Joint” opens the door for new research about possible causes of dissatisfaction, like AP laxity or instability and lack of proprioception [5, 40].
The purpose of this study was to test the hypothesis that AP translation and proprioception would vary according to the design of knee arthroplasty used when compared to the contralateral unoperated side. Comparing these findings with patient-reported outcome scores to differentiate results for each level of constraint was to the best of our knowledge not studied before.
Materials and methods
From all consecutive patients undergoing knee arthroplasty between 2010 and 2014 by a single surgeon (ET), patients were selected for this retrospective cohort study according to the following criteria. Inclusion criteria were both sexes with an age between 55 and 85 years, operated for primary varus bone on bone osteoarthritis (OA). Patients were either treated with a unicompartmental knee arthroplasty (UKA)-type Zimmer unicompartmental knee (ZUK, Zimmer, Warsaw, USA) or with a total knee arthroplasty. Within the TKA group three levels of constraint were selected. The Vanguard posterostabilized (PS) (Biomet, Warsaw, USA) was used as a flat-on-flat, minimal-constraint PS knee, the Persona PS (Zimmer, Warsaw, USA) as a PS TKA with slightly more medial constraint and finally the Sphere (Medacta, Castel San Pietro, Switzerland) as a medial pivot design with medial AP constraint and on the lateral side a flat tibial tray allowing roll back and external rotation around the medial pivot point. The selection between UKA and TKA was done according to criteria from literature.
The included patients all presented pre-operatively a Kellgren–Lawrence IV bone on bone medial arthritis confirmed on radiographs. CT Arthrography was used to determine whether the disease was isolated to the medial compartment or if it was tricompartmental [41]. Patients selected for TKA were randomized to receive a Vanguard, Persona or Sphere implant according to the surgical programme planning system. An implant was pre-selected for certain time slots of the day, and the selected patient for that time slot underwent this procedure (centralized assignment quasi-randomization). The surgeon had at least 1 year of experience with each of the utilized knee systems.
All implants in this study were cemented and the patella was resurfaced in all TKA groups. Intra-medullary alignment was used on the femoral side and extra-medullary alignment on the tibial side. Sizing of the components was done intra-operatively according to the surgeon’s experience, but measured resection of the bone was utilized to confirm that resections corresponded to implant thicknesses. UKA was implanted with a tibia first technique followed by a spacer gap femoral resection. The mean (SD) tourniquet time for all surgeries was 50 (10) minutes with a mean (SD) surgical time of 70 (20) minutes. Patients received antibiotic prophylaxis, and antibiotic-loaded cement was used. VTE prevention with heparin was 10 days. Full weight bearing without crutches was allowed immediately after surgery and physiotherapy prescribed for 3 months.
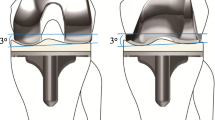
The surgery had to be unilateral, and the contralateral side could not present more than KL grade II OA or signs of previous knee surgery, malalignment or instability to serve as the control group. Furthermore, all the included patients had to have a knee score (KSS) of at least 80 on file and satisfy the following radiological measurements, both on the pre-operative and on post-operative radiographs. The pre-operative HKA angle should be maximally 170° to avoid soft tissue stretching because of the deformity, and the post-operative HKA angle needed to be corrected to 180° ± 3° for the TKA groups. For the UKA group residual varus was accepted as long as a correction from pre-operative alignment could be observed. The posterior condylar offset needed to remain within 3 mm of its pre-operative value (corresponding to the cartilage thickness of the posterior condyles). It was measured both on pre-operative and post-operative lateral radiographs as described by Bellemans et al. [6]. The posterior condylar offset ratio needed to be 0.44 on the pre-operative radiographs and 0.47 on the post-operative radiographs as described by Johal et al. [18]. Finally, the tibial slope needed to be within 5° of posterior slope [28]. The post-operative distal femoral joint line needed to remain within 2 mm of the original joint line, and no CR TKA designs were included to avoid the potential bias of posterior cruciate ligament integrity [15].
A minimal follow-up of 1 year without complications was necessary to be eligible for this study.
Exclusion criteria were previous knee surgery like cruciate ligament surgery, knee osteotomy, valgus deformity, varus deformity of more than 170° HKA, residual post-operative deficits in knee flexion or extension, diseases of the soft tissues (Ehler–Danlos), inflammatory arthritis, history of infection and finally neurological disorders. Patients who used morphine, morphine-related drugs, alcohol, benzodiazepines and antihistaminic drugs were also excluded because of their potential influence on proprioceptive testing. Pre-operative or post-operative use of walking aids was an exclusion criterion because of its influence on quadriceps muscle.
Baseline characteristics of the study groups like gender, age, body mass index (BMI), cause of osteoarthritis (OA), stage of OA according to Kellgren–Lawrence classification and time to follow-up are given in Table 1.
Patients were invited over phone to participate in this study. An informed consent and written explanation about the study was sent to their home. They were contacted a second time to organize their study visit on site where PROMS, clinical examination and the other study tests were performed. Primary outcome would be AP femorotibial translations measured during AP testing of both knees with a KT-1000 device (MedMetric, San Diego, CA, USA), as well as proprioceptive testing. Both outcomes would be correlated to patient-reported outcome measurement scores (PROMS) and compared among different implant designs.
The following tests were performed for study purposes:
Anteroposterior stability measurements under static conditions
AP displacement of the knee was measured with a knee arthrometer type KT-1000 (MedMetric, San Diego, CA, USA). Both knees of each patient were tested by the same observer (DW) at 30°, 60° and 90° of flexion. These flexion angles were chosen because 30° allows testing according to the Lachman test, 60° because this angle is most cited as important for mid-flexion instability and finally 90° of flexion which allows testing according to the anterior drawer test [15, 17]. A goniometer was utilized to confirm the intended degree of flexion for each test. The method of testing with KT-1000 arthrometer was described by Daniel et al. [8] and Ishii et al. [17].
Each test was performed three times on both sides by the same single observer allowing to calculate the intra-observer variability. The mean (SD) value of the three measurements was calculated for each, and used for the evaluation. Accuracy of testing was 0.1 mm.
Proprioceptive testing
The ability of patients to maintain a fixed position of the knee in space (position sense) was tested by means of three simple tests. Each test was repeated three times both for the operated and contralateral side. Accuracy was 1 cm and 2° for each measurement. The mean value for each angular position was used for the evaluation and the result was compared to the patient’s contralateral side.
Line test
Patient is standing, feet together 10 cm from a line drawn on the floor. The evaluator asks the patient, first under visual control and then with the eyes closed, to touch with his foot the line with the tip of their toes. The test performed with closed eyes is taken into account. The distance between the tip of the foot and the line is measured in cm.
Fixed knee flexion at 60°
Patient is placed in a supine position. The healthy knee rests on the table, and the operated knee is flexed to 60° as confirmed with a goniometer. Then the patient is asked to extend the knee completely and flex it back to the starting position. The final position angle is measured with a goniometer positioned on the leg. Deviations in both directions from the initial 60° position are registered.
Hip and knee flexed at 90°
Patient is placed in a supine position. Hip and knee on the operated side are flexed at 90° as confirmed with a goniometer. The patient is asked to remember this position in space and then to extend the knee fully. They need to find the 90° knee and 90° hip position back in space. Deviations in both directions in degrees from the initial 90° position are registered.
Three different patient-reported outcome measurement scores (PROMS) were collected according to the guidelines from Thienpont et al. [40] to evaluate the subjective outcome with the “Knee Society Score”, “Knee Osteoarthritis Outcome Score” and “Forgotten Joint Score”.
Ethical approval for this study was obtained from the institutional review board (IRB) before starting the study. The ethics board of the Saint Luc University hospital (Brussels, Belgium) approved this study under IRB approval number (2014/18DEC/605). The study was registered at https://clinicaltrials.gov/.
Statistical analysis
Sample characteristics are presented as numbers, means and standard deviations. Categorical variables are presented as frequencies and percentages. For continuous variables, violations of the normality assumption were tested using the Shapiro–Wilk test. Normally distributed data are presented as means and standard deviations, and between-group differences were tested using one-way ANOVA tests. In case one-way ANOVA yielded a significant finding, post hoc testing using Tukey’s honest significant difference (HSD) was performed for further assessment.
Non-normally distributed data are presented as median and interquartile ranges; between-group differences were tested using Kruskal–Wallis tests.
For the endpoints involving repeated measurements and side-to-side comparison (e.g. AP stability and proprioception), the respective measurements for each side were averaged. Mean values were compared for each treatment group using paired t tests. For proprioception, side-to-side differences in variance were tested using Levene’s tests for homogeneity of variances.
Intra-class correlation coefficients (ICCs) were used to determine intra-session reliability [34]. Each subject was evaluated by the same examiner (DW) three times. ICCs indicated variations in the population sample within and between patients ICC consistency parameters. According to Shrout and Fleiss, an ICC > 0.75 indicates excellent reliability, ICC of 0.40–0.75 indicates fair to good reliability, and ICC < 0.40 indicates poor reliability [34].
The ICC for the three measurements of AP laxity were 0.94 for 30° of flexion, 0.93 for 60° of flexion and 0.94 for 90° of flexion.
A pilot study in our hospital had found that for AP stability measurements the total variance accounted for by prosthetic design varied between 63 and 70 %. These numbers served as estimates for the effect size for the current study. With a power of 80 % and a significance level of 5 % and based on the estimated effect size, a sample size of 8–10 patients per group was sufficient for one-way ANOVA.
Sample size calculation was performed with G*Power 3.1 (University Düsseldorf, Düsseldorf, Germany). All other analyses were performed using Stata 12.1 (StataCorp LP, College Station, TX, USA). A p value of <0.05 was considered significant.
Results
The results of pre-operative and post-operative radiological measurements are given in Table 2.
The results of the KT-1000 testing comparing the operated side with the non-operated side are given in Table 3. These results showed that UKA was significantly more stable at 30°, 60° and 90° compared to both Vanguard and Persona. No difference between UKA and Sphere was observed at 30° and 90°. However, the post hoc test showed no difference among Vanguard, Persona and Sphere (Table 4).
The results for the three different PROMS are given in Table 5, but no between-group difference was observed with Kruskal–Wallis testing (n.s.).
The results of the proprioceptive testing are given in Table 6. All tests were inconclusive. An important SD both for Vanguard and Sphere at 90° of flexion was observed during proprioceptive testing but without significance (Levene test).
Discussion
The most important finding of this study was that any type of knee arthroplasty influences anteroposterior stability of the knee depending on its design, but UKA and medial pivot TKA show more AP stability at 30° and 90° of flexion than PS TKA when evaluated with a KT-1000 test.
Anteroposterior stability has been studied in the ageing native knee with KT-1000 devices. Dayal et al. [10] found that the natural AP laxity in the elderly, with a KL-score <2 as for our control group, was 7.1 ± 2.6 mm. Brage et al. [7] found an AP translation of 12.2 mm in the non-arthritic population. Dargel et al. [9] showed that using the contralateral side as an anatomic control is an acceptable model. In this study an AP laxity ranging from 3 to 6 mm was observed for the non-operated knee. Laxity was most important at 30° of flexion and decreased with more flexion resulting in the least AP translation at 90° of flexion.
Brage et al. [7] showed that AP laxity decreases with osteoarthritis. This observation could explain why less AP translation was observed in the UKA group at 30° of flexion when compared to the contralateral side. The osteoarthritic process might have decreased AP laxity over time while awaiting UKA.
Aside the obvious reason of the resection of both ACL and PCL, other aspects of knee arthroplasty surgery could influence the observed differences in AP laxity between UKA and TKA. Ligament releases can influence the measured laxity. Ishii et al. found that other structures that might end up released in the varus knee also play a role. The released medial collateral ligament and the posteromedial capsule will influence AP laxity too [17]. This might explain the important and significant differences in AP stability that are observed in this study between UKA and PS TKA.
Abdel et al. [1] showed that a reduction in the posterior slope, correction of malalignment in flexion and reconstruction of the native posterior condylar offset will stabilize the flexion gap. The opposite was observed for increased tibial slope by Oka et al. [27]. In this study all patients had femoral rotation matched with the epicondylar axis, and the PCO was measured and compared to be equal on pre- and post-operative radiographs. The intended posterior slope was 3° for all cases and obtained within 1°.
Suggs et al. [37] found that after UKA the knee exhibits tibial translations and forces in the ACL similar to the native knee. Suero et al. [36] showed that levelling of the posterior slope reduces the anterior tibiofemoral translation after sectioning of the ACL. Voos et al. [44] observed a reduction in pivot shift after reduction in the posterior slope. This study showed that on the contralateral side increased AP laxity is observed in the elderly and that this can be reduced by opting for less posterior tibial slope. Hernigou and Deschamps [13] showed that excessive posterior slope (>8°) can lead to ACL tears in UKA as well as aseptic loosening. In ACL-deficient UKA a posterior slope less than 5° would stabilize the knee. Bai et al. [3] found that a posterior tibial slope between 0° and 3° provided the greatest tibial component stability. In this study 2.5° ± 1° was measured as the average slope for UKA.
Ishii et al. performed a similar study to ours but in PS mobile TKA and in a 75° flexion position. A median AP displacement of 7.3 mm (range 5.5–8.3 mm) was observed. They furthermore analysed the same patients under general anaesthesia and found an increased AP translation of 9.2 mm (range 6.5–11.1 mm) with a positive correlation of r = 0.620 (p < 0.001) under narcosis [16]. In their paper they suggested that in retrospect the joint should have been evaluated at 30° of flexion too [16]. In this study testing was performed at 30°, 60° and 90° of flexion. A significant difference in AP laxity compared to the normal contralateral knee was observed for Vanguard and Persona both at 30° and 90° but not for ZUK and Sphere. This finding cannot confirm the hypothesis of Ishii et al. [16] that no anteroposterior laxity would be observed up to 30° of flexion because of the full contact between the femoral component and the tibial insert between 0° and 30°. This is probably only true for a medial pivot design with increased medial AP constraint, as observed in this study for Sphere. At 60° of flexion all knee designs except ZUK showed increased laxity, therefore suggesting that mid-flexion instability is present for all of them under non-load-bearing conditions. Stability throughout the different flexion angles in UKA was also observed by Becker et al. [4].
The importance of coronal stability in TKA has been proven in the past with low functional outcome scores in case of instability and good results obtained in knees with <5 mm of mediolateral laxity. None of the patients included in this study had complaints of subjective instability, and all obtained comparable and good-to-excellent outcomes as measured with PROMS. In this selected study population either PROMS were not sensitive enough to identify AP laxity-induced limitations at specific angles of flexion or this observed AP laxity has no or limited functional consequences under these study conditions. Van Hal et al. [43] could not observe any difference when comparing AP stability to KSS outcome. Due to a limited amount of studies on residual AP laxity of implants, it is difficult to conclude what should be considered normal and abnormal stability after knee arthroplasty. Jones et al. [19] concluded that AP laxity over 10 mm would result in lower functional scores and Seon et al. [32] made the same observation. None of the implants evaluated in this study presented more than 10 mm of AP laxity.
In this study, proprioception of the operated and non-operated contralateral knee was compared. Koralewicz and Engh [22] and Pai et al. [29] found that proprioception declines with age and is further impaired by arthritis. In this study the contralateral knee was not affected by arthritis, but the operated knee had gone through a degenerative process before surgery. Therefore, an observed difference between both might be normal. Joint position sense (JPS) is determined by measuring the accuracy of joint angle replication. During these tests the ability to reposition a joint to a pre-determined position is evaluated. The tests can be performed under weight-bearing (line test) and non-weight-bearing conditions.
The important proprioceptive elements are muscle spindles and Golgi tendon organs. After knee arthroplasty the articular mechanoreceptors are excised. Therefore, Pacinian corpuscles, Ruffini endings, Golgi receptors and bare nerve endings are influenced and proprioception is reduced [35]. Muscle weakness might interfere with the former two tests [20]. In this study no significant differences were observed with the line test. During this test the load-bearing standing proprioception is tested. An important SD was observed for Vanguard and Sphere with the proprioceptive test performed at 90° of flexion. Both ZUK and Persona had comparable proprioception to the contralateral knee. Wada et al. [45] observed that coronal plane ligament balancing influences proprioception and all knees, except the UKA, underwent some type of medial release. Swanik et al. [38] observed better proprioception because of reduced pain and inflammation after knee arthroplasty. This type of observation could not be made in this study because we did not compare before and after surgery, but only with the contralateral healthy side.
The first limitation of this study is that stability testing was performed under awake conditions for the patient. Potential anxiety for the unknown and reflex muscle contraction can influence the study results. Ishii et al. did anteroposterior laxity testing under general anaesthesia when they were performing surgery on the contralateral side. In this study, TKA was compared with a normal, non-arthritic joint, so therefore the same conditions of testing under narcosis were never possible. Everything was set up to create an as relaxed as possible study condition because performing this study under general anaesthesia would have been difficult ethically. Furthermore, patients are awake when they experience anteroposterior translation of their joint during daily activities.
A second limitation could be the small groups, and the findings must therefore be interpreted cautiously. But the inclusion criteria both clinically and radiologically were very strict. The study population had to have a non-arthritic joint on the contralateral side and had to be able to perform the different tests selected for the purpose of this study. Patient selection for inclusion into a similar study will therefore remain difficult.
A third limitation is that the patients in the UKA group were selected by the surgeon to be good candidates for that type of surgery. This bias can have an influence on the study results. However, the surgeon’s volume and experience could also have helped to select the right patient for each indication therefore allowing a correct analysis of AP translation for each group.
A fourth limitation is that the potential clinical impact of AP laxity and decreased proprioception was evaluated with PROMS and not with functional testing. Heyse et al. [14] showed that AP stability influences the quadriceps force after knee arthroplasty. Furthermore, to avoid the bias of a bad outcome on the different tests, patients with a Knee Score of at least 80 points were invited to participate in this study.
A fifth limitation was that study groups were not perfectly balanced in terms of follow-up time. Sphere has a slightly shorter follow-up time compared to the other groups. In case a time effect exists between 15 and 20 months of follow-up, the study would be too small to detect such an effect.
A final limitation is that all observations were performed by the same physician not allowing us to calculate an inter observer reliability for these tests. The examiner (DW) is right handed, and this might lead to increased AP laxity for the right knees included in this study [33]. The advantage is that the KT-1000 is a validated way of testing static instability and that the tests were performed in a standardized way. Another advantage was that the examiner had obtained enough experience to perform all tests accurately. A comparable mix of right and left knees was included to counter that bias.
The clinical importance of this study is that it showed that AP laxity changes with the type of implant used and that PS designs have more AP translation than UKA or medial pivot designs at 30° and 90° of flexion. The observations of AP laxity made here can be considered a register of normal AP translations after arthroplasty since all included patients had good-to-excellent outcome as reported by PROMS.
Conclusion
UKA is able to retain AP stability as in the native knee. The same type of stability can be recreated at 30° and 90° of flexion with a medial pivot design. None of the TKA designs showed stability at 60° of flexion as tested under non-load-bearing conditions. Despite of significant differences in AP translation in between the different types of knee arthroplasty, no differences in clinical outcome were observed when using PROMS to evaluate subjective results in selected patients.
References
Abdel MP, Pulido L, Severson EP, Hanssen AD (2014) Stepwise surgical correction of instability in flexion after total knee replacement. Bone Joint J 96-B(12):1644–1648
Arellano CJ, Layne CS, O’Connor DP, Scott-Pandorf M, Kurz MJ (2009) Does load carrying influence sagittal plane locomotive stability? Med Sci Sports Exerc 41(3):620–627
Bai B, Baez J, Testa N, Kummer FJ (2000) Effect of posterior cut angle on tibial component loading. J Arthroplasty 15(7):916–920
Becker R, Mauer C, Starke C, Brosz M, Zantop T, Lohmann CH, Schulze M (2013) Anteroposterior and rotational stability in fixed and mobile bearing unicondylar knee arthroplasty: a cadaveric study using the robotic force sensor system. Knee Surg Sports Traumatol Arthrosc 21(11):2427–2432
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27(3):430–436
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84(1):50–53
Brage ME, Draganich LF, Pottenger LA, Curran JJ (1994) Knee laxity in symptomatic osteoarthritis. Clin Orthop Relat Res 304:184–189
Daniel DM, Stone ML, Sachs R, Malcom L (1985) Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med 13(6):401–407
Dargel J, Feiser J, Gotter M, Pennig D, Koebke J (2009) Side differences in the anatomy of human knee joints. Knee Surg Sports Traumatol Arthrosc 17(11):1368–1376
Dayal N, Chang A, Dunlop D, Hayes K, Chang R, Cahue S, Song J, Torres L, Sharma L (2005) The natural history of anteroposterior laxity and its role in knee osteoarthritis progression. Arthritis Rheum 52(8):2343–2349
Dunbar MJ, Richardson G, Robertsson O (2013) I can’t get no satisfaction after my total knee replacement: rhymes and reasons. Bone Joint J 95-B(11 Suppl A):148–152
Hart HF, Culvenor AG, Collins NJ, Ackland DC, Cowan SM, Machotka Z, Crossley KM (2015) Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med. doi:10.1136/bjsports-2015-094797
Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 86-A(3):506–511
Heyse TJ, Becher C, Kron N, Ostermeier S, Hurschler C, Schofer MD, Fuchs-Winkelmann S, Tibesku CO (2010) Quadriceps force in relation of intrinsic anteroposterior stability of TKA design. Arch Orthop Trauma Surg 130(1):1–9
Hino K, Ishimaru M, Iseki Y, Watanabe S, Onishi Y, Miura H (2013) Mid-flexion laxity is greater after posterior-stabilised total knee replacement than with cruciate-retaining procedures: A computer navigation study. Bone Joint J 95-B(4):493–497
Ishii Y, Matsuda Y, Ishii R, Sakata S, Omori G (2005) Sagittal laxity in vivo after total knee arthroplasty. Arch Orthop Trauma Surg 125(4):249–253
Ishii Y, Noguchi H, Takeda M, Sato J, Toyabe S (2014) Anteroposterior translation does not correlate with knee flexion after total knee arthroplasty. Clin Orthop Relat Res 472(2):704–709
Johal P, Hassaballa MA, Eldridge JD, Porteous AJ (2012) The posterior condylar offset ratio. Knee 19(6):843–845
Jones DP, Locke C, Pennington J, Theis JC (2006) The effect of sagittal laxity on function after posterior cruciate-retaining total knee replacement. J Arthroplasty 21(5):719–723
Knoop J, Steultjens MP, van der Leeden M, van der Esch M, Thorstensson CA, Roorda LD, Lems WF, Dekker J (2011) Proprioception in knee osteoarthritis: a narrative review. Osteoarthr Cartil 19(4):381–388
Koninckx A, Schwab PE, Deltour A, Thienpont E (2014) The minimally invasive far medial subvastus approach for total knee arthroplasty in valgus knees. Knee Surg Sports Traumatol Arthrosc 22(8):1765–1770
Koralewicz LM, Engh GA (2000) Comparison of proprioception in arthritic and age-matched normal knees. J Bone Joint Surg Am 82-A(11):1582–1588
Krackow KA, Mihalko WM (1999) Flexion-extension joint gap changes after lateral structure release for valgus deformity correction in total knee arthroplasty: a cadaveric study. J Arthroplasty 14(8):994–1004
Meric G, Gracitelli GC, Aram LJ, Swank ML, Bugbee WD (2015) Variability in distal femoral anatomy in patients undergoing total knee arthroplasty: measurements on 13,546 computed tomography scans. J Arthroplasty. doi:10.1016/j.arth.2015.04.024
Nguyen LC, Lehil MS, Bozic KJ (2015) Trends in total knee arthroplasty implant utilization. J Arthroplasty 30(5):739–742
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Oka S, Matsumoto T, Muratsu H, Kubo S, Matsushita T, Ishida K, Kuroda R, Kurosaka M (2014) The influence of the tibial slope on intra-operative soft tissue balance in cruciate-retaining and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(8):1812–1818
Okamoto S, Mizu-Uchi H, Okazaki K, Hamai S, Nakahara H, Iwamoto Y (2015) Effect of tibial posterior slope on knee kinematics, quadriceps force, and patellofemoral contact force after posterior-stabilized total knee arthroplasty. J Arthroplasty 30(8):1439–1443
Pai YC, Rymer WZ, Chang RW, Sharma L (1997) Effect of age and osteoarthritis on knee proprioception. Arthritis Rheum 40(12):2260–2265
Paternostre F, Schwab PE, Thienpont E (2014) The combined Whiteside’s and posterior condylar line as a reliable reference to describe axial distal femoral anatomy in patient-specific instrument planning. Knee Surg Sports Traumatol Arthrosc 22(12):3054–3059
Scott CE, Howie CR, MacDonald D, Biant LC (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 92(9):1253–1258
Seon JK, Park SJ, Yoon TR, Lee KB, Moon ES, Song EK (2010) The effect of anteroposterior laxity on the range of movement and knee function following a cruciate-retaining total knee replacement. J Bone Joint Surg Br 92(8):1090–1095
Sernert N, Helmers J, Kartus C, Ejerhed L, Kartus J (2007) Knee-laxity measurements examined by a left-hand- and a right-hand-dominant physiotherapist, in patients with anterior cruciate ligament injuries and healthy controls. Knee Surg Sports Traumatol Arthrosc 15(10):1181–1186
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428
Stan G, Orban H, Orban C, Petcu D, Gheorghe P (2013) The influence of total knee arthroplasty on postural control. Chirurgia (Bucur) 108(6):874–878
Suero EM, Citak M, Cross MB, Bosscher MR, Ranawat AS, Pearle AD (2012) Effects of tibial slope changes in the stability of fixed bearing medial unicompartmental arthroplasty in anterior cruciate ligament deficient knees. Knee 19(4):365–369
Suggs JF, Li G, Park SE, Steffensmeier S, Rubash HE, Freiberg AA (2004) Function of the anterior cruciate ligament after unicompartmental knee arthroplasty: an in vitro robotic study. J Arthroplasty 19(2):224–229
Swanik CB, Lephart SM, Rubash HE (2004) Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am 86-A(2):328–334
Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R (2015) Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am 97(9):715–720
Thienpont E, Opsomer G, Koninckx A, Houssiau F (2014) Joint awareness in different types of knee arthroplasty evaluated with the forgotten joint score. J Arthroplasty 29(1):48–51
Thienpont E, Schwab PE, Omoumi P (2014) Wear patterns in anteromedial osteoarthritis of the knee evaluated with CT-arthrography. Knee 21(Suppl 1):S15–S19
Valkering KP, Breugem SJ, van den Bekerom MP, Tuinebreijer WE, van Geenen RC (2015) Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop 86(4):432–439
van Hal CT, van Hellemondt GG, Wymenga AB, Jacobs WC (2007) The anterior-posterior laxity after total knee arthroplasty inserted with a ligament tensor. Knee Surg Sports Traumatol Arthrosc 15(8):1019–1022
Voos JE, Suero EM, Citak M, Petrigliano FP, Bosscher MR, Citak M, Wickiewicz TL, Pearle AD (2012) Effect of tibial slope on the stability of the anterior cruciate ligament-deficient knee. Knee Surg Sports Traumatol Arthrosc 20(8):1626–1631
Wada M, Kawahara H, Shimada S, Miyazaki T, Baba H (2002) Joint proprioception before and after total knee arthroplasty. Clin Orthop Relat Res 403:161–167
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wautier, D., Thienpont, E. Changes in anteroposterior stability and proprioception after different types of knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 1792–1800 (2017). https://doi.org/10.1007/s00167-016-4038-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4038-9