Abstract
Purpose
To evaluate the relationship between patellofemoral osteoarthritis (OA) and varus OA of the knee with a focus on the location of joint space narrowing.
Methods
Eighty-five patients scheduled to undergo total knee arthroplasty caused by varus OA were enrolled in this study. The relationship between patellofemoral OA and varus knee malalignment was elucidated. To determine the alignment of the patellofemoral joint in varus knees, patellar tilt, and the tibial tuberosity–trochlear groove (TT–TG) distance were measured, and patellofemoral OA was classified using computed tomography.
Results
The femorotibial angles in patients with stage II–IV patellofemoral OA were significantly larger than those in patients with stage I patellofemoral OA, and the patellar tilt in patients with stage II–IV patellofemoral OA and the TT–TG distance in patients with stage IV patellofemoral OA were significantly larger than those in patients with stage I patellofemoral OA. The TT–TG distance was strongly correlated with patellar tilt (R 2 = 0.41, P < 0.001). Patellofemoral joint space narrowing was mainly noted at the lateral facet, and it was found on both sides as patellofemoral OA worsened.
Conclusion
Varus knee malalignment was induced by patellofemoral OA, especially at the lateral facet. Patellar tilt and the TT–TG distance are considered critical factors for the severity of patellofemoral OA. Understanding the critical factors for patellofemoral OA in varus knees such as the TT–TG distance and patellar will facilitate the prevention of patellofemoral OA using procedures such as high tibial osteotomy and total knee arthroplasty to correct knee malalignment.
Level of evidence
Retrospective cohort study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee alignment is a key determinant of load distribution, and both varus and valgus alignment contribute to the progression of osteoarthritis (OA) [17, 30]. Malalignment of the knee influences both the femorotibial and patellofemoral joints in a compartment-specific manner [4, 28], and previous reports indicated that 49 % of all cases of knee OA arise as patellofemoral OA [22].
Malalignment, which includes abnormal tilt, torsion, and Q angles, has a greater predisposition towards patellofemoral OA [15]. In the lower limbs, genu valgum increases the Q angle and the subsequent force on the lateral patellar facet. By contrast, genu varus decreases the Q angle and increases the force on the medial patellar facet [17]. Lateral patellofemoral OA is more commonly observed in individuals with valgus malalignment, and varus malalignment is more likely to arise in subjects with medial patellofemoral OA [10]. On the contrary, some researchers reported no significant relationship between the Q angle and the position of the patella [2]. Although patellofemoral OA is induced by excessive loading and cartilage damage progresses in the lateral patellofemoral compartment, especially in valgus knees, the relationship between patellofemoral OA and varus knee malalignment is unclear. The hypothesis of this study was that femorotibial knee malalignment is correlated with the severity of patellofemoral OA in varus knees, and the purpose of this study was to evaluate the severity and location of patellofemoral OA in subjects with varus OA of the knee.
Materials and methods
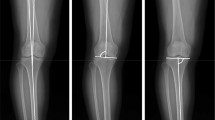
Eighty-five patients (21 males, 64 females) scheduled to undergo total knee arthroplasty (TKA) because of varus OA were enrolled in this study. The average patient age, body mass index (BMI), and femorotibial angle (FTA) were 73.8 (SD ± 6.4) years, 25.9 (SD ± 3.5), and 183.7 (SD ± 4.8) degrees, respectively. Femorotibial OA was analysed using the Kellgren–Lawrence scoring system, and 8, 29, and 48 patients were diagnosed with grade II, III, and IV OA, respectively (Table 1). Knee malalignment was assessed using the FTA, which was defined as the lateral angle between the centreline of the femur and the tibia on the coronal radiograph in a standing position, and an FTA exceeding 175° was defined as varus alignment. Computed tomography (CT) was performed using a TOSHIBA Aquilion®, and a CT examination was conducted with the subjects in the supine position with their knees in extension and their lower limbs in neutral rotation. An axial view of a CT slice, which included the centre of the patella, was used for the evaluation performed by two orthopaedic surgeons, who were blinded to the patients’ backgrounds. The location of joint space narrowing, which was classified as medial, lateral, or both, was also evaluated. The patellofemoral joint space was measured both medially and laterally, and narrowing was defined as a joint space of <5 mm. We defined patellofemoral OA stages using CT based on Iwano’s radiographic classification [18] as follows: stage I, normal to early OA; stage II, mild OA, as typified by a joint space of more than 5 mm; stage III, moderate OA, which was defined as a joint space of <5 mm; and stage IV, severe patellofemoral OA, as typified by bone contact (Fig. 1). The interobserver and intraobserver reliability of this classification were 0.771 and 0.835, respectively. The patellar tilt angle was measured using a line through the long axis of the patella and a line parallel to one through the posterior femoral condyles [14], and the tibial tuberosity–trochlear groove (TT–TG) distance, which is the deepest point of the trochlear groove and the central point of the tibial tubercle on a line tangential to the posterior femoral condyles, was measured to determine its relationship with patellofemoral OA progression (Fig. 2) [7]. The interobserver accuracy of patellar tilt and the TT–TG distance were 0.90 and 0.73, respectively, which were similar to previously described values [6, 21]. This study was performed in accordance with a protocol approved by the Institutional Review Board of Osaka Medical College (No. 1291).
Measurements of the femorotibial angle (FTA) (a), patellar tilt (b), and TT–TG distance (c). The patellar tilt is the angle between the transverse axis of the patella and the posterior femoral condyles. The TT–TG distance is the deepest point of the trochlear groove and the central point of the tibial tubercle on a line tangential to the posterior femoral condyles
Statistical analysis
A power analysis was performed for the primary comparison of interest (the difference of patellar tilt among the stages of patellofemoral OA). For a large effect size, an α of 0.05, and a power of 0.8, a total of 78 participants were required for the groups. Non-repeated measures analysis of variance was performed to compare the four groups via multivariate analysis. Then, comparisons between two groups were performed by the Wilcoxon test using JMP Pro (version 10.0.2). P < 0.05 was considered significant.
Results
Regarding the severity of patellofemoral OA, 20 (23.5 %), 33 (38.8 %), 19 (22.4 %), and 13 (15.3 %) knees exhibited stage I, II, III, and IV disease, respectively, and no significant difference was found in the mean age of the patients among the different stages of patellofemoral OA (Table 2). Regarding the severity of varus knee deformity, the FTA in patients with stage II–IV patellofemoral OA was significantly higher than that in patients with stage I patellofemoral OA, indicating that the progression of patellofemoral OA was correlated with varus knee deformity (Fig. 3, P < 0.05). Concerning the correlation between patellar tilt and rotational deformity about the tibia, the relationship between patellar tilt and the TT–TG distance was elucidated. Stage I patellofemoral OA was associated with less patellar tilt than stage II–IV patellofemoral OA (Fig. 4a, P < 0.05), and stage IV patellofemoral OA was linked to a longer TT–TG distance than stage I–III patellofemoral OA (Fig. 4b, P < 0.05). The TT–TG distance was strongly correlated with patellar tilt in knees with varus OA (Fig. 4c, P < 0.001, R 2 = 0.41). Regarding the location of joint space narrowing in patients with patellofemoral OA, 75 % of subjects were classified into stage I displayed normal joint spaces, but others exhibited mild patellofemoral OA at the lateral facet. As patellofemoral OA worsened, joint space narrowing progressed both laterally and medially on both sides (Table 3, P < 0.001, R 2 = 0.38).
The correlation between the TT–TG distance and patellar tilt. a The patellar tilt was greater for stage II–IV patellofemoral osteoarthritis (PFOA) than for stage I PFOA (P < 0.05). b Stage IV PFOA was associated with a longer TT–TG distance than stage I–III PFOA (P < 0.05). c The TT–TG distance was correlated with patellar tilt in the knees of subjects with varus osteoarthritis (P < 0.001, R 2 = 0.41)
Discussion
Although patellofemoral OA of the lateral facet of patellofemoral OA was induced in valgus knees, the mechanism behind the progression of patellofemoral OA is unclear, especially in varus knees [16]. The most important finding of this study was that varus knee deformity was associated with worsening of patellofemoral OA, and severe varus deformity mainly induced OA of the lateral facet. Several cohort studies such as the Boston OA of the knee [20], Framingham OA [12], and multicentre OA studies [13] evaluated the severity of patellofemoral OA with knee alignment, and Gross et al. [16] reported that knees with varus malalignment exhibited a higher prevalence of medial rather than lateral patellofemoral damage in all cohorts, which was different from our findings. In this study, lateral patellofemoral OA was detected in almost 47 % of subjects with early- to end-stage patellofemoral OA. The reason for this difference may be the background of the subjects. This study focused on patients with severe varus OA with an average FTA of 183.7°, whereas the cohort studies mainly included subjects with mild knee malalignment.
CT has great importance in the analysis of the patellofemoral joint, and patellar kinematics plays a role in the initiation and progression of patellofemoral OA [23]. The relationship between tibial torsion and medial OA was previously analysed using CT [31]; however, the effect of varus malalignment on patellofemoral OA is unclear. To evaluate patellofemoral malalignment with varus, the relationship between patellar tilt and the TT–TG distance was elucidated because these factors are associated with patellar instability [25]. Both variables increased with increasing severity of patellofemoral OA in varus knees. In particular, patellar tilt tended to increase in the early stage of disease, and the TT–TG distance most notably increased in the end stage, indicating that the mechanism of patellofemoral OA might differ between early- and end-stage patellofemoral OA. Femoral internal rotation has been demonstrated to be the primary contributor to lateral patellar tilt [26].
An abnormal TT–TG distance can result from lateralization of the tibial tuberosity or excessive rotation [8, 19], and no prior reports described the effect of TT–TG on patellofemoral OA. These results indicated that external rotation of the lower limbs might induce patellofemoral OA, especially end-stage disease. Rotational deformity might play a critical role in the severity of patellofemoral OA.
Knees with varus OA can be treated using various surgical techniques, such as high tibial osteotomy (HTO), unicompartmental knee arthroplasty, and TKA. Patellofemoral complications, such as patellofemoral OA, patella infera, and patellofemoral malalignment, can commonly occur, especially after opening-wedge valgus HTO, because patellofemoral contact pressure may be elevated [1, 29]. Patellofemoral complications have also been reported in TKA after correcting knee malalignment [3, 24]. Surgeons need to pay attention to the femorotibial alignment and proper patellar preparation to decrease the risk of patellofemoral complications, such as lateral release [11] or tibial rotation with tibial tuberosity transfer [5, 9]. Bicompartmental knee arthroplasty, which is performed medially, and patellofemoral arthroplasty might also be useful options to prevent patellofemoral complications after surgery [27]. Understanding the critical factors for patellofemoral OA in varus knees such as the TT–TG distance and patellar tilt will facilitate the prevention of patellofemoral OA using procedures such as HTO and TKA to correct knee malalignment.
This study has some limitations. First, all patients in this study underwent TKA because of knee pain, which involved severe inflammatory conditions, and femorotibial OA may have affected the deterioration of the patellofemoral joint. Second, this study lacked a control group. However, we analysed 20 gender- and BMI-matched subjects with no knee symptoms, and these individuals exhibited no significant differences in terms of patellar tilt and the TT–TG distance compared to patients with stage I patellofemoral OA, indicating that group I patients can serve as a control group. Third, the number of samples might have been insufficient, as more than 200 samples may have been needed to analyse the TT–TG distance based on the power analysis (α = 0.05, power = 0.8). Finally, this study did not evaluate femoral anteversion. The entire lower limb should be considered in future patellofemoral research.
Conclusion
Varus knee malalignment was induced by patellofemoral OA, especially at the lateral facet. Patellar tilt and the TT–TG distance are considered critical factors for the severity of patellofemoral OA. Understanding the mechanism of patellofemoral OA in varus knee might result in good outcomes for knee-reconstructed surgery.
References
Beck P, Brown NAT, Greis PE, Burks RT (2007) Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med 35:1557–1563
Biedert RM, Warnke K (2001) Correlation between the Q angle and the patella position: a clinical and axial computed tomography evaluation. Arch Orthop Trauma Surg 121:346–349
Boyd AD, Ewald FC, Thomas WH, Poss R, Sledge CB (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 75:674–681
Cahue S, Dunlop D, Hayes K, Song J, Torres L, Sharma L (2004) Varus–valgus alignment in the progression of patellofemoral osteoarthritis. Arthritis Rheum 50:2184–2190
Caton JH, Dejour D (2010) Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop 34:305–309
Delgado-Martínez AD, Rodríguez-Merchán EC, Ballesteros R, Luna JD (2000) Reproducibility of patellofemoral CT scan measurements. Int Orthop 24:5–8
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S (2013) Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med 41:51–57
Drexler M, Dwyer T, Dolkart O, Goldstein Y, Steinberg EL, Chakravertty R, Cameron JC (2013) Tibial rotational osteotomy and distal tuberosity transfer for patella subluxation secondary to excessive external tibial torsion: surgical technique and clinical outcome. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2561-5
Elahi S, Cahue S, Felson DT, Engelman L, Sharma L (2000) The association between varus–valgus alignment and patellofemoral osteoarthritis. Arthritis Rheum 43:1874–1880
Fabbriciani C, Panni AS, Delcogliano A (1992) Role of arthroscopic lateral release in the treatment of patellofemoral disorders. Arthroscopy 8:531–536
Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP (1975) The Framingham offspring study. Design and preliminary data. Prev Med 4:518–525
Felson DT, Nevitt MC (2004) Epidemiologic studies for osteoarthritis: new versus conventional study design approaches. Rheum Dis Clin North Am 30:783–797
Fulkerson JP, Schutzer SF, Ramsby GR (1987) Computerized tomography of the patellofemoral joint before and after lateral release or realignment. Arthroscopy 3:19–24
Grelsamer RP, Dejour D, Gould J (2008) The pathophysiology of patellofemoral arthritis. Orthop Clin North Am 39:269–274
Gross KD, Niu J, Stefanik JJ, Guermazi A, Roemer FW, Sharma L, Nevitt MC, Segal NA, Lewis CE, Felson DT (2012) Breaking the law of valgus: the surprising and unexplained prevalence of medial patellofemoral cartilage damage. Ann Rheum Dis 71:1827–1832
Huberti HH, Hayes WC (1984) Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am 66:715–724
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis: with special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res 252:190–197
Izadpanah K, Weitzel E, Vicari M, Hennig J, Weigel M, Südkamp NP, Niemeyer P (2013) Influence of knee flexion angle and weight bearing on the tibial tuberosity–trochlear groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2537-5
Karlson EW, Sanchez-Guerrero J, Wright EA, Lew RA, Daltroy LH, Katz JN, Liang MH (1995) A connective tissue disease screening questionnaire for population studies. Ann Epidemiol 5:297–302
Lin YF, Jan MH, Lin DH, Cheng CK (2008) Different effects of femoral and tibial rotation on the different measurements of patella tilting: an axial computed tomography study. J Orthop Surg Res 3:5
McAlindon T, Zhang Y, Hannan M, Naimark A, Weissman B, Castelli W, Felson D (1996) Are risk factors for patellofemoral and tibiofemoral knee osteoarthritis different? J Rheumatol 23:332–337
McWalter EJ, Cibere J, MacIntyre NJ, Nicolaou S, Schulzer M, Wilson DR (2007) Relationship between varus–valgus alignment and patellar kinematics in individuals with knee osteoarthritis. J Bone Joint Surg Am 89:2723–2731
Meding JB, Fish MD, Berend ME, Ritter MA, Keating EM (2008) Predicting patellar failure after total knee arthroplasty. Clin Orthop Relat Res 466:2769–2774
Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P (2011) Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc 19:663–670
Powers CM (2003) The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther 33:639–646
Rolston L, Bresch J, Engh G, Franz A, Kreuzer S, Nadaud M, Puri L, Wood D (2007) Bicompartmental knee arthroplasty: a bone-sparing, ligament-sparing, and minimally invasive alternative for active patients. Orthopedics 30:70–73
Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD (2001) The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 286:188–195
Stoffel K, Willers C, Korshid O, Kuster M (2007) Patellofemoral contact pressure following high tibial osteotomy: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 15:1094–1100
Tetsworth K, Paley D (1994) Malalignment and degenerative arthropathy. Orthop Clin North Am 25:367–377
Yagi T, Sasaki T (1986) Tibial torsion in patients with medial-type osteoarthritic knee. Clin Orthop Relat Res 213:177–182
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Otsuki, S., Nakajima, M., Okamoto, Y. et al. Correlation between varus knee malalignment and patellofemoral osteoarthritis. Knee Surg Sports Traumatol Arthrosc 24, 176–181 (2016). https://doi.org/10.1007/s00167-014-3360-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3360-3