Abstract
Purpose
This study aimed to investigate the morphological patterns of remnant anterior cruciate ligament bundles after injury (ACL remnant) on three-dimensional computed tomography (3DCT) and compare them with those on arthroscopy.
Methods
Sixty-three patients (33 males and 30 females; mean age 25.2 ± 10.1 years) who had undergone primary ACL reconstruction between March 2011 and December 2012 were included in this study. The average durations between traumas and 3DCT and between 3DCT and surgery were 101.7 ± 87.2 and 38.2 ± 38.7 days, respectively. ACL remnants were classified into four morphological patterns on 3DCT. 3DCT findings were compared with arthroscopic findings with and without probing.
Results
The morphological patterns of the ACL remnants on 3DCT were well matched with those on arthroscopy without probing (the concordance rate was 77.8 %). However, the concordance rate was reduced to 49.2 % when arthroscopic probing was used to confirm the femoral attachment of ACL remnants (p ≤ 0.05).
Conclusions
This study demonstrates that the morphological patterns of ACL remnants on 3DCT were well matched with those on arthroscopy without probing. Therefore, the technique can be useful for preoperative planning of the ACL reconstruction or informed consent to the patients. However, for definitive diagnosis, arthroscopic probing is required.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Several treatment options are available for anterior cruciate ligament (ACL) reconstruction with hamstring tendons, such as single-bundle, double-bundle, or remnant-preserving reconstructions [3, 24, 29]. When relatively thick ACL remnants after injury are left in certain conditions, we have performed ACL augmentation to preserve the remnants [1, 20, 21]. Recently, remnant-preserving ACL reconstruction has become popular because this procedure was proven to provide biomechanical, vascular, and proprioceptive advantages for patients [9, 25]. Although preoperative assessment of ACL remnants is important, the clinical diagnosis of an ACL partial tear is still subject to debate. Some cadaveric studies have shown that it is difficult to know the percentage of injured fibres determined only by a Lachman test or an anterior drawer test [8, 14]. Magnetic resonance imaging (MRI) is undoubtedly the most popular diagnosis imaging for an injured ACL. MRI can provide important information of not only the ACL itself but also other intra- or extra-articular structures such as meniscus, articular cartilage, muscle, or tendons. However, it is difficult to evaluate the three-dimensional (3D) morphology of the ACL remnants on MRI.
Recently, it has been reported that 3D computed tomography (CT) imaging with volume rendering can be used for diagnosing several soft tissues, such as muscles, hand and wrist tendons, or anterior talofibular ligament of the ankle [17, 18, 23, 26, 30]. This was the first study that investigated the morphological patterns of ACL remnants on three-dimensional computed tomography (3DCT) and compared them with those on arthroscopy with and without probing. It was hypothesized that the morphological patterns of ACL remnants on 3DCT are well matched with those on arthroscopy.
Materials and methods
Between 2011 and 2012, 120 patients underwent arthroscopy-assisted ACL reconstruction with multistranded hamstring tendon at our institute. Among them, 63 patients whose preoperative 3DCT scan of the ACL-injured knee was available were included in this study. Patients with multiligamentous injuries such as medial collateral ligament, posterior cruciate ligament, or posterolateral corner injuries were excluded. Patients whose preoperative periods were >2 years were also excluded because their ACL remnants usually have disappeared. The included patients consisted of 33 males and 30 females with the average age of 25.2 ± 10.1 years at the time of the operation. The cause for all ACL injuries was trauma, such as a sports-related injury or a traffic accident. The average durations between traumas and 3DCT and between 3DCT and surgery were 101.7 ± 87.2 and 38.2 ± 38.7 days, respectively.
3DCT was conducted on the ACL-injured knee in all cases. 3DCT images were obtained with a multidetector row CT scanner (LightSpeed Ultra 16; General Electric Medical Systems, Milwaukee, WI, USA). The patient was placed in a supine position with the knee joint at a 90° flexed position. Then, 3D volume data sets of the knee joint were obtained. The scanning parameters were as follows: a gantry rotation speed of 0.6 s/rotation, 1.25-mm collimation width × 16 detectors, CT pitch factor of 0.562, and field of view of 25–30 cm. The CT dose index volume was 7.67 mGy. Then, 2D images were reconstructed with 12–25 cm field of view, 1.25-mm retrospective slice thickness, and 0.63-mm overlap. The total table motion was 20–30 cm, and finally, 200–400 slices were obtained. Images were rendered qualitatively with the volume-rendering technique by using a commercially available workstation (Virtual Place; AZE, Tokyo, Japan) to take the 3D images. The scanning time ranged from 40 to 60 s, and another 10 to 15 min was needed for postprocessing.
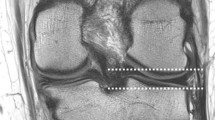
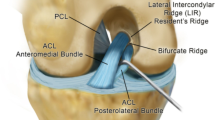
The ACL remnants on 3DCT were classified into four morphological patterns according to the classification by Crain et al. [10]: type I, bridging between the posterior cruciate ligament and tibia; type II, bridging between roof of the intercondylar notch and tibia; type III, bridging between the lateral wall of the intercondylar notch and tibia; and type IV, no substantial ACL remnants (Fig. 1).
Anterior cruciate ligament (ACL) remnants on three-dimensional computed tomography (3DCT) and on arthroscopy were classified into four morphological patterns according to the classification by Crains et al. Type I (PCL), bridging between the posterior cruciate ligament and tibia; type II (roof), bridging between roof of the intercondylar notch and tibia; type III (wall), bridging between the lateral wall of the intercondylar notch and tibia; and type IV (rupture), no substantial ACL remnants
All ACL surgeries were performed by the senior author (M.O.). Routine arthroscopic inspection was performed through lateral and medial infrapatellar portals with a 30°-oblique arthroscope with the knee flexed at 90°. First, the whole ACL remnant was evaluated while the scope was inserted from the lateral portal without probing. Then, the femoral attachment of the ACL remnant was inspected with the probe inserted through the medial portal. The images of the ACL remnant with and without probing were digitally recorded using an image capture system. The ACL remnants on arthroscopy were also classified into four patterns as the 3DCT images.
The morphological pattern of the ACL remnant on 3DCT and arthroscopy was reviewed by two of the authors (N.A. and M.D., who had >20 years of experience as knee surgeons) individually; both authors were blinded to the clinical information of the patients. In case of an interobserver difference, the authors evaluated the results together to reach an agreement.
The 3DCT findings were compared with the arthroscopic findings with and without probing. The concordance rate was calculated.
The institutional review board of Hiroshima University approved the use of human subjects for this study (ID number: EKI-523). Written informed consent was obtained from all patients before their participation, and their rights were protected.
Statistical analysis
The χ 2 test for independence was used for comparative evaluation of the correlation between the morphological pattern of the ACL remnants on 3DCT and those on arthroscopy. A p value of <0.05 was considered statistically significant. All statistical analyses were conducted using Statview 5.0 (SAS Institute, Cary, NC, USA). As for the sample size of this study, the patients who had met the inclusion criteria were collected as many as possible during the study periods. The calculation showed that this sample size indicated adequate power (≥0.80) to detect a significant difference.
Results
On 3DCT, 11.1 % (n = 7) of the ACL remnants were classified as type I, 17.5 % (n = 11) type II, 46.0 % (n = 29) type III, and 25.4 % (n = 16) type IV.
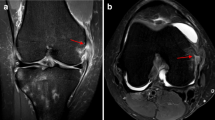
Correlation between the morphological patterns on 3DCT and those on arthroscopy without and with probing is summarized in Tables 1 and 2, respectively. The morphological patterns of the ACL remnants on 3DCT were well matched with those on arthroscopy without probing in 77.8 % of the patients. However, the concordance rate was reduced significantly to 49.2 % when arthroscopic probing was used to confirm the femoral attachment of the ACL remnants (p < 0.05) (Fig. 2).
a Anterior cruciate ligament (ACL) remnant was classified as type III on three-dimensional computed tomography (3DCT). b Arthroscopic finding of the ACL remnant was classified as type III without probing. c Arthroscopic finding of the ACL remnant was classified as type II when the femoral attachment of the remnant with probing was evaluated
Discussion
The most important finding of this study was that the morphological patterns of ACL remnants on 3DCT with the volume-rendering technique were well matched with those on arthroscopy without probing. Therefore, this technique can be useful for preoperative assessments of ACL remnants. However, importantly, for a definitive diagnosis of the ACL attachment, arthroscopic probing is required.
Several ACL reconstruction techniques have been reported, such as single- or double-bundle reconstruction with multistranded hamstring tendons, and reconstruction with bone-patella-tendon bone or quadriceps tendons [3, 24, 29]. Recently, ACL reconstruction with remnant-preserving techniques has received much attention. It is reported that remnant-preserving ACL reconstructions have potential advantages in terms of biomechanical function, revascularization of the graft, or promotion or maintenance of the proprioceptive function of the knee [1, 2, 4, 5, 7, 9, 10, 12, 16, 20, 21, 25].
It is important to know the status of the injured ACL preoperatively for the planning of ACL reconstruction, especially for ACL remnant-preserving techniques. Muneta et al. [15] reported that the ACL remnant volume at the time of remnant-preserving double-bundle ACL reconstruction well correlated with the postoperative knee laxity. To evaluate the status of the ruptured ACL, clinical examinations, instrumental laxity testing, or MRI can be used. Some cadaveric studies have shown that it is difficult to know the percentage of injured fibres determined only by a Lachman test or an anterior drawer test [8, 14]. Some authors used a knee arthrometer or an electromagnetic measurement system and showed less laxity in the partial ACL rupture than in the complete rupture [6, 22]. However, of course, morphological examinations cannot be done in those instrument testing. There is no doubt that MRI is the most popular diagnostic imaging technique for an injured ACL. MRI can provide important information of not only the ACL itself but also other intra- or extra-articular structures, such as the meniscus, articular cartilage, muscle, or tendons. Recently, several reports have been published on the diagnosis of partial ACL. In 2013, Delin et al. [11] conducted a prospective study to evaluate the diagnostic accuracy of apparent diffusion coefficient (ADC) mapping with conventional MRI in differentiating complete and partial ACL tears. They concluded that additional ADC mapping helps differentiate between complete and partial tears with high reliability. In 2012, Lefevre et al. [13] compared the conventional 2D and 3D fast spin echo (3D-FSE-Cube) MRI for diagnosing partial ACL tears. They demonstrated higher accuracy in diagnosing partial ACL tears. Ng et al. [19] recommended adding oblique axial imaging to standard MRI images to improve the diagnostic accuracy for partial ACL tears. On the other hand, van Dyck et al. [28] stated that MR imaging at 3.0 T represents a highly accurate method for the diagnosis of the ACL tears, but it was difficult to differentiate between complete and partial tears of the ACL at this magnetization. Thus, although the diagnosis of partial ACL tears has been a recent topic in skeletal radiology, even with advanced MRI techniques, it is difficult to evaluate the 3D morphology or partial tears of the ACL on MRI.
Recently, it has been reported that 3DCT imaging with volume rendering can be used for diagnosing several soft tissues, such as muscles, hand and wrist tendons, or anterior talofibular ligament of the ankle, and this method has received much attention in the field of orthopaedic surgery [17, 18, 23, 26, 29]. Sunagawa et al. [26] used 3DCT with volume rendering for the evaluation of flexor and extensor tendons in the hand and wrist. They stated that 3DCT imaging was useful for the diagnosis of those tendons and was helpful in preoperative surgical planning because the location of the ruptured tendon stump could be identified easily with this technique. Nakasa et al. [18] also demonstrated that 3DCT could evaluate the condition of talofibular ligament remnants much better than MRI. As for the evaluation of injured ACL using 3DCT, Uozumi et al. [27] evaluated the features of the tibial side of the ACL remnant preoperatively. However, the femoral attachment of the ACL remnant which is very important information for ACL surgery was not evaluated.
3DCT allows the evaluation of the overall 3D structure of soft tissue in one image. As for the assessment of an injured ACL, it is possible to know the volume and 3D position of the remnant. These are important information for preoperative planning and obtaining informed consent from the patients if ACL reconstruction with a remnant-preserving procedure could be performed. However, as shown in this study, because the attachment of the ACL to the femur could not be clearly visualized on 3DCT images, arthroscopic assessment is indispensable. The status of the attachment of the injured ACL to the femur is another important aspect to consider when performing ACL reconstruction with remnant preservation.
This study has several limitations. First, the images of ACL remnants on 3DCT were not compared with other diagnostic tools such as clinical tests or MRI. Therefore, this study does not show any superiority of the 3DCT over other tools. It is necessary to perform a comparative study to show the definite usefulness of 3DCT for diagnosing ACL remnants. Second, the correlation between the morphological status of ACL remnants and the anterior or rotational laxity of the knee joint was not evaluated. Future studies that integrate the information of morphological status of ACL remnant on 3DCT and MRI and involve joint laxity will provide a more precise status of the ACL remnant and help decide the indication of remnant-preserving ACL surgery preoperatively. Third, using CT has the potential disadvantage of exposing the patient to ionizing radiation. In this study, we used a multidetector row CT scanner that irradiates small milligray doses during the scan. Recently, 3DCT imaging techniques have become less invasive than ever. Fourth, the test–retest reliability of evaluating 3DCT images and arthroscopic findings was not conducted.
Conclusion
This study clearly demonstrated that that the morphological patterns of ACL remnants on 3DCT were well matched with those on arthroscopy without probing. Therefore, the technique can be useful for the preoperative planning of the ACL reconstruction or informed consent to the patients. However, because arthroscopic probing is required for a definitive diagnosis, routine 3DCT examination is not recommended.
References
Adachi N, Ochi M, Uchio Y, Sumen Y (2000) Anterior cruciate ligament augmentation under arthroscopy: a minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 120:128–133
Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M (2002) Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scan 73:330–334
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y (2004) Reconstruction of the anterior cruciate ligament: single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86:515–552
Ahn JH, Lee YS, Ha HC (2009) Anterior cruciate ligament reconstruction with preservation of remnant bundle using hamstring autograft: technical note. Arch Orthop Trauma Surg 129:1011–1015
Ahn JH, Lee SH, Choi SH, Lim TK (2010) Magnetic resonance imaging evaluation of anterior cruciate ligament reconstruction using quadrupled hamstring tendon autografts: comparison of remnant bundle preservation and standard technique. Am J Sports Med 38:1768–1777
Araki D, Kuroda R, Matsushita T, Matsumoto T, Kubo S, Nagamune K, Kurosaka M (2013) Biomechanical analysis of the knee with partial anterior cruciate ligament disruption: quantitative evaluation using an electromagnetic measurement system. Arthroscopy 29:1053–1062
Bali K, Dhillon MS, Vasistha RK, Kakkar N, Chana R, Prabhakar S (2012) Efficacy of immunohistological methods in detecting functionally viable mechanoreceptors in the remnant stumps of injured anterior cruciate ligaments and its clinical importance. Knee Surg Sports Traumatol Arthrosc 20:75–80
Christel PS, Akgun U, Yasar T, Karahan M, Demirel B (2012) The contribution of each anterior cruciate ligament bundle to the Lachman test: a cadaver investigation. J Bone Joint Surg Br 94:68–74
Colombet P, Dejour D, Panisset JC, Siebold R (2010) The French Arthroscopy Society (2010) current concept of partial anterior cruciate ligament ruptures. Orthop Traumatol Surg Res 965:S109–S118
Crain EH, Fithian DC, Paxton EW, Luetzow WF (2005) Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy 21:19–24
Delin C, Silvera S, Coste J, Thelen P, Lefevre N, Ehkirch FP, Le Couls V, Oudjit A, Radier C, Legmann P (2013) Reliability and diagnostic accuracy of qualitative evaluation of diffusion-weighted MRI combined with conventional MRI in differentiating between complete and partial anterior cruciate ligament tears. Eur Radiol 23:845–854
Gohil S, Annear PO, Breidahl W (2007) Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br 89:1165–1171
Lefevre N, Naouri JF, Bohu Y, Klouche S, Herman S (2014) Partial tears of the anterior cruciate ligament: diagnostic performance of isotropic three-dimensional fast spin echo (3D-FSE-Cube) MRI. Eur J Orthop Surg Traumatol 24:85–91
Lintner DM, Kamaric E, Moseley JB, Noble PC (1995) Partial tears of the anterior cruciate ligament: are they clinically detectable? Am J Sports Med 23:111–118
Muneta T, Koga H, Ju YJ, Horie M, Nakamura T, Sekiya I (2013) Remnant volume of anterior cruciate ligament correlates preoperative patients’ status and postoperative outcome. Knee Surg Sports Traumatol Arthrosc 21:906–913
Nakamae A, Ochi M, Deie M, Adachi N, Kanaya A, Nishimori M, Nakasa T (2010) Biomechanical function of anterior cruciate ligament remnants: how long do they contribute to knee stability after injury in patients with complete tears? Arthroscopy 26:1577–1585
Nakamura E, Mizuta H, Kadota M, Katahira K, Kudo S, Takagi K (2004) Three-dimensional computed tomography evaluation of semitendinosus harvest after anterior cruciate ligament reconstruction. Arthroscopy 20:360–365
Nakasa T, Fukuhara K, Adachi N, Ochi M (2006) Evaluation of anterior talofibular ligament lesion using 3-dimensional computed tomography. J Comput Assist Tomogr 30:543–547
Ng AW, Griffith JF, Hung EH, Law KY, Yung PS (2013) MRI diagnosis of ACL bundle tears: value of oblique axial imaging. Skeletal Radiol 42:209–217
Ochi M, Adachi N, Deie M, Kanaya A (2006) Anterior cruciate ligament augmentation procedure with a 1-incision technique: anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy 22(463):e1–e5
Ochi M, Adachi N, Uchio Y, Deie M, Kumahashi N, Ishikawa M, Sera S (2009) A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy 25:117–122
Panisset JC, Ntagiopoulos PG, Saggin PR, Dejour D (2012) A comparison of Telos™ stress radiography versus Rolimeter™ in the diagnosis of different patterns of anterior cruciate ligament tears. Orthop Traumatol Surg Res 98:751–758
Pelc JS, Beaulieu CF (2001) Volume rendering of tendon-bone relationships using unenhanced CT. AJR Am J Roentgenol 176:973–977
Samuelsson K, Desai N, McNair E, van Eck CF, Petzold M, Fu FH, Bhandari M, Karlsson J (2013) Level of evidence in anterior cruciate ligament reconstruction research: a systematic review. Am J Sports Med 41:924–934
Siebold R, Fu FH (2008) Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy 24:1289–1298
Sunagawa T, Ochi M, Ishida O, Ishiburo M, Suzuki O, Yasunaga Y, Ochi M (2003) Three-dimensional CT imaging of flexor tendon ruptures in the hand and wrist. J Comput Assist Tomogr 27:169–174
Uozumi H, Aizawa T, Sugita T, Kunii T, Abe S, Itoi E (2013) Visualization of torn anterior cruciate ligament using 3-dimensional computed tomography. Orthop Rev (Pavia) PMID: 24191182
Van Dyck P, Vanhoenacker FM, Gielen JL, Dossche L, Van Gestel J, Wouters K, Parizel PM (2011) Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skeletal Radiol 40:701–707
Van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH (2010) “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 26:S2–S12
Yamamoto T, Kurosaka M, Soejima T, Fujii M (2001) Contrast-enhanced three-dimensional helical CT for soft tissue tumors in the extremities. Skeletal Radiol 30:384–387
Conflict of interest
The authors report that they have no conflict of interest in the authorship and publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adachi, N., Ochi, M., Takazawa, K. et al. Morphologic evaluation of remnant anterior cruciate ligament bundles after injury with three-dimensional computed tomography. Knee Surg Sports Traumatol Arthrosc 24, 148–153 (2016). https://doi.org/10.1007/s00167-014-3354-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3354-1