Abstract
Objectives
To assess the reliability and diagnostic accuracy of qualitative evaluation of apparent diffusion coefficient (ADC) mapping with magnetic resonance imaging (MRI) in differentiating between complete and partial anterior cruciate ligament (ACL) tears.
Methods
This prospective study protocol was approved by the institutional ethics review board and informed consent was obtained from all the patients. Eighty-five patients (35 women and 50 men, mean age 34.1 years) with recent (<4 months) knee trauma with suspected ACL injury underwent conventional MRI (T1-weighted and T2-weighted sequences with fat saturation) associated with ADC mapping. MR images were read qualitatively without and then with ADC mapping by three radiologists, with analysis of direct signs of a traumatic ACL tear and a second-reading. Dynamic X-rays (43 patients) or arthroscopies (42 patients) were used as reference standards.
Results
For complete ACL tear diagnosis (67 patients), sensitivity and specificity were 87% and 50% respectively with conventional MRI, and 96% and 94% respectively with ADC mapping (P < 0.01 for specificity). Inter-observer correlations between musculoskeletal radiologists were almost perfect (κ = 0.81) with ADC mapping and fair with conventional MRI on the second-reading.
Conclusions
ADC mapping associated with conventional MR sequences is a reproducible method to better differentiate complete and partial ACL tears.
Key Points
• MRI is widely used for assessing the problematic knee
• Additional diffusion-weighted sequences help differentiate between complete and partial ACL tears
• DW-MRI for ACL requires a reader-dependent learning curve
• Reliable visualisation of complete ACL tears allows more appropriate management of patients
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance imaging (MRI) is widely used for the diagnosis of anterior cruciate ligament (ACL) tears [1]. MRI signs of ACL tears on T2-weighted or proton density-weighted (TW2) sequences are well known [1–6]. Many studies have shown their accuracy in diagnosing ACL injuries, although without discriminating between complete and partial tears.
However, these studies have mostly been retrospective, with a population of arthroscopy patients with fully torn or intact ACLs, or with unspecified ACL tears including both complete and partial. Arthroscopic studies [7–9] have shown that more than 70% of patients with acute traumatic haemarthrosis present with an ACL tear, 15–30% of which are partial. Partial ACL tears are therefore frequent. Nonetheless, the few studies specifically covering their MRI diagnosis [2, 4, 10–12] have found standard MRI sequences to be relatively ineffective for this purpose, because they do not really show the ligament fibres in the oedema. Resorting to indirect signs of an ACL tear or fine slices or 3-Tesla MRI does not improve diagnostic effectiveness very much [1, 12–14]. Kinetic MRI tests [15, 16] are interesting but not easy to apply routinely. One study reported that oblique MRI slices improved diagnostic effectiveness for traumatic ACL injuries, but it did not distinguish between complete and partial tears [17].
Since its first applications in brain imaging [18], diffusion-weighted MRI (DW-MRI) has proven useful for other organs [19, 20]. We sought to assess the reliability and diagnostic accuracy of diffusion sequences with apparent diffusion coefficient (ADC) mapping in differentiating between complete and partial ACL tears, compared with conventional MRI alone.
Materials and methods
Study population
Our study protocol was approved by the institutional ethics review board and all patients provided informed consent.
We conducted a prospective study of 85 consecutive patients: 50 men (age range, 18–61 years; mean age, 33.6 years) and 35 women (age range, 15–60 years; mean age, 34.9 years) who underwent DW-MRI between May 2006 and October 2009.
All patients presented with all three of the following inclusion criteria: (1) a traumatic injury of the knee sustained less than 4 months earlier with clinical signs suggesting an ACL tear (Lachmann test assessed at + to +++); (2) an ACL tear on the initial MRI with standard T1- and T2-weighted sequences read by the musculoskeletal radiologist responsible for patient recruitment (CD); (3) no previous history of ACL trauma or surgery of the injured knee.
A control group included 30 patients with normal ACLs: 19 men (age range, 16–64 years; mean age, 42 years) and 11 women (age range, 16–56 years; mean age, 38 years) with intra-articular pathological features and intra-articular effusion, requiring therapeutic arthroscopy that made it possible to check the ACL (DW-MRI cannot show a normal ACL if there is no fluid in the intercondylar notch) (Fig. 1).
Normal anterior cruciate ligaments (ACLs). a–d Knee with abundant intra-articular effusion (black star) secondary to a meniscal tear in a 46-year-old woman. Sagittal (a) and axial (c) T2-weighted slices with fat saturation: the ACL shows as a hypointense signal running parallel to the roof of the notch (fine arrows) with a discrete fibrillary structure (thick arrows). Sagittal (b) and axial (d) slices with ADC mapping: the ligament shows a strong hypointense signal due to the low water content of collagen-rich ligament fibres (thick arrows) and is silhouetted by the intra-articular fluid. e–h Normal knee with no intra-articular effusion in a 22-year-old woman. Sagittal (e) and axial (g) T2-weighted slices with fat saturation: the ACL is normal (fine arrows) with little intra-articular fluid visible in the notch. Sagittal (f) and axial (h) slices with ADC mapping: the ACL is not silhouetted by intra-articular fluid and is not discernible. (Technical characteristics of the sequences are given in Table 1)
ACL tears were diagnosed based on the results of a reference standard: arthroscopy or a comparative study of stress radiographs with a TELOS device (Telos, Laubscher, Hölstein, Switzerland). Forty-two patients had therapeutic arthroscopy (for ligamentoplasty and/or to treat a meniscal injury) a mean of 2.3 months (range, 7 days to 6 months) after the DW-MRI examination. The short time to arthroscopy combined with the absence of a new traumatic episode prevented the extension of partial tears to full thickness [9]. TELOS was the only basis for diagnosis in 43 cases. TELOS assessment was performed with 20° flexion of the knee: a difference of 5 mm or more between the injured leg and the contralateral healthy leg in anterior tibial subluxation with the application of 200-N pressure was the diagnostic criterion for a complete ACL tear [21–23]. The TELOS procedure was used and its findings were the base of diagnosis here when the following criteria were met: (1) no pain and complete muscular relaxation; (2) no (either longstanding or recent) tear of the ACL or any other ligament in the contralateral knee; (3) a difference between the anterior drawer values of each patient’s knees greater than or equal to 5 mm or less than or equal to 3 mm (lack of specificity of differential TELOS measurements between 3 and 5 mm) [24].
MRI
The conventional MRI evaluation was performed with our osteo-articular department’s 1.5-Tesla Siemens Symphony MR system (Siemens, Erlangen, Germany) and its knee coil (extremity coil-single element transmit/receive coil, Siemens) to identify patients with traumatic ACL injuries. T1-weighted (T1W) spin-echo images were acquired in the sagittal plane. T2W fast spin-echo images were acquired with fat saturation in the true sagittal (perpendicular to the posterior edge of the condyles), coronal and transversal (parallel to the tibial plateau) planes.
DW images were obtained with a 1.5-Tesla Siemens Avento MR system (Siemens, Erlangen, Germany), which is generally used for visceral imaging, with its knee coil (eight-channel high resolution knee array, Siemens Medical Systems). Patients were placed in the same position as for the initial MR examination. DW images (and ADC image maps) were obtained in the sagittal and transversal planes in the identical positions used in the T2 sequences. The MR sequence parameters are summarised in Table 1. The DWI-MRI sequence used was the vendor standard echo-planar imaging single-shot sequence and was acquired with three orthogonal directions only. The scheme used was a bipolar set of diffusion gradients, less prone to artefacts. It used a spectral fat saturation technique. No triggering, no radiofrequency (RF) spoiling, and no flow compensation were applied. The ADC algorithm was a simple linear regression that used the two b-values measured. The ADC maps were not exponential ADC maps. The algorithm used a threshold value to display only “high” ADC values (here above 20 s/mm²). The formula used was: ADC = −1/b·ln[S(b)/S(0)].
Image interpretation
Three radiologists, two with 11 (C.D.) and 20 (P.T.) years of experience in musculoskeletal radiology and the third with 7 years of experience in gastrointestinal radiology (S.S.), separately reviewed all images.
During the reading sessions, the readers, who were blinded to the information obtained on clinical examination, TELOS and arthroscopy, first reviewed the conventional MR image set and then the combined set of conventional and DW-MR images.
For the first set of conventional imaging, the readers assessed the ACL based on the following criteria: (1) poor or no visualisation of the ACL on the images; (2) an amorphous oedematous mass with focally increased signals on the T2W images; (3) irregular contours with wavy redundant fibres; (4) completely or partially disrupted fibres with tears midsubstance or at the tibial or femoral attachment; (5) clearly abnormal orientation of the ACL in the intercondylar notch; (6) irregular thinning of part or all of the ligament without complete disruption of the ligament fibres; (7) common oedema consecutive to bruising although all the ligament fibres remain intact, with no cystic image or balloon appearance that might point to mucinous degeneration of the ACL. Their conclusions were classified as complete or partial ACL tear.
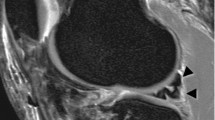
When the second set of images (combining the conventional MRI images and ADC maps) was analysed, the ADC mapping were treated as anatomical images (i.e., the readers looked only at the morphological aspect of the ACL without analysing the absolute value of the signal) and were evaluated qualitatively, although they were in fact parametric. The ADC mapping criteria of ACL injuries were: a complete interruption in the dark signal from the ACL showing a complete tear (Fig. 2), and a partial interruption a partial tear. The T1W and T2W sequences were used only to locate the anatomical landmarks; only the DW-MR images were used to conclude whether the ACL was completely torn or not. This study did not quantitatively measure either the ACL signal or that of the lesional oedema. Our preliminary trials before this study showed how difficult it is to place a region of interest (ROI) precisely on an ACL without extending into the oedema and causing error. Moreover, ADC mapping on our machine found the same ACL signal value, 0, for the ACL (or one of its fragments), for fatty synovial villi, the fat of Hoffa’s triangle and for spongy bone. This mapping is thus not discriminatory.
Complete ACL tear in a 42-year-old man. a–c Sagittal (a, b) and axial (c) T2-weighted slices with fat saturation, heterogeneity of the ligament fibres (white arrows) compatible with a partial ligament tear. d–f Sagittal (d, e) and axial (f) slice ADC mapping, complete discontinuity of ACL fibres (white arrows). g Arthroscopy 7 days later, complete ACL tear; the lacerated lower ligament stump is clearly visible (black arrows). MC medial condyle. (Technical characteristics of the sequences are given in Table 1)
A second reading session with the same methods was conducted for each reader 4 months later. The readers were blinded to the results of the first reading and to each other’s results.
If the two specialised musculoskeletal radiologists disagreed on the second reading, a joint reading was set up to reach a consensus conclusion.
Images of the normal ACLs were read more than a year later. They were mixed with images of the injured ACLs in the study and re-read by readers 2 and 3 separately as a control. Reader 1 had recruited the normal ACLs and therefore did not participate in their reading.
Statistical analysis
The inter-observer reproducibility of the readings for the two techniques was assessed using standard kappa statistics [25, 26].
The sensitivity and specificity of the techniques and readings, with TELOS and/or arthroscopy findings as the reference standard, were computed and compared with paired samples and the two-tailed pairwise MacNemar chi-squared test [25]. Sensitivity and specificity were computed for the readings and the consensus interpretations. The consensus interpretation was considered the best possible performance, whereas individual readings were presumed to better reflect the performance of the techniques in routine practice. The main analysis set a threshold difference of 5 mm or more between the injured and the healthy contralateral leg for positive TELOS diagnosis. To test sensitivity, thresholds of 3 and 10 mm were also used.
Statistical analyses were performed with SAS Version 8.02 statistical software (SAS Institute, Cary, NC, USA).
Results
Diagnosis of complete ACL tears by arthroscopy or TELOS
Overall, 67 patients showed signs of a complete ACL tear, 35 on arthroscopic findings and 32 on TELOS findings (mean anterior dislocation, 8.7 mm; range, 5–15 mm) and 18 had signs of a partial tear or no signs of tearing at all, 7 on arthroscopic findings and 11 on TELOS findings (mean anterior dislocation, 1 mm; range, 3 to −3 mm).
Diagnostic accuracy of MRI
Table 2 details the accuracy of MRI in diagnosing complete ACL tears.
The results for consensus reading showed significant differences between conventional MRI alone and MRI with ADC mapping (P < 0.01): the latter was more specific (50% vs 94%) and had a higher positive likelihood ratio (LR+ = 1.73 vs 17.19) and a lower negative likelihood ratio (LR− = 0.27 vs 0.05). When assessing complete ACL tears, the positive predictive value (PPV or accuracy) of 87% and the negative predictive value (NPV) of 50% (equivalent to a PPV of 50% and a NPV of 87% for assessing partial tears) obtained with conventional MRI rose to 98% and 85% respectively with ADC mapping. The positive likelihood ratio increased for all readers for MRI with ADC mapping. Despite the trend, however, there was no significant difference (P = 0.08) in diagnostic sensitivity between conventional MRI alone (87%) or interpreted with ADC mapping (96%).
There was no significant difference in specificity for the musculoskeletal radiologists’ findings (Table 2) at the first and second reading sessions with ADC mapping (identical findings for the first reader and P < 0.08 for the second reader) (Table 3). However, their sensitivity improved significantly (Table 2) at the second reading with ADC mapping (P < 0.05 and P < 0.0001 respectively) (Table 3).
Readings by the visceral radiologist did not differ significantly for the MRI with ADC mapping (P = 0.65 and P = 0.10 respectively).
The sensitivity analysis with a TELOS threshold greater than 3 mm yielded identical values. The sensitivity analysis with a TELOS threshold greater than or equal to 10 mm showed no significant changes in sensitivity (Appendix Table 5). Only the specificity values were reduced, with consensus reading of diffusion sequences showing a greater specificity (49%) than consensus reading of sequences with no ADC (36%).
All the normal ACLs in the control group were recognised as continuous by readers 2 and 3 on T1 and T2 sequences with ADC mapping. Neither reader successfully identified one conventional (T1 and T2 sequences alone) MRI image of a normal ACL as continuous.
Analysis of inter- and intra-observer agreement
The values in Table 4 show the inter- and intra-observer agreement for all three readers.
Intra-observer agreement
The intra-observer agreement for readers 1 and 2 was almost perfect for the reading of conventional MRI alone; their kappa values were respectively 1.00 and 0.85. However, when interpreting the images with ADC mapping, the second reader’s kappa value dropped to 0.45, although the value for the first reader remained almost perfect at 0.87.
Regardless of the reading method used, with or without ADC mapping, the third reader’s intra-observer correlation values remained low.
Inter-observer agreement
The inter-observer kappa values for readers 1 and 2 for conventional MRI images alone were fair, at 0.39 in both readings (21 cases needed rereading to achieve a consensus). However, the inter-observer agreement between them improved in the second reading with ADC mapping; their values were assessed at 0.35 in the first reading and 0.81 in the second (only six cases required rereading to reach a consensus).
On the whole, the agreement between the third reader and readers 1 and 2 remained low for conventional MRI and did not change between the first and second readings (Table 4). However, although reader 3’s inter-observer kappa values were very low for the first reading (respectively 0.29 and 0.39), they clearly improved in the second reading with ADC mapping (respectively 0.61 and 0.52).
Discussion
Diffusion sequences are generally used to ascertain the diffusion of free water in tissue. This property has long been employed for early diagnosis of ischaemic strokes [27] but also, more recently, during efforts to characterise neoplastic tissue [28], for these sequences can reflect cellular richness. Tissue rich in free water (interstitial or intra-articular fluid or infiltrated between damaged tissue) has a high diffusion coefficient (hyperintense signal in ADC mapping). Inversely, tissue containing bound water (e.g. the cytotoxic cell oedema observed in arterial vascular accidents) has a reduced diffusion coefficient and tissue containing very little water (bone, fat, and ligament tissue rich in collagen) has none at all. A ligament fragment (rich in collagen and very poor in water) has a hypointense signal on ADC mapping. It is surrounded by a hyperintense signal corresponding to the fluid infiltration induced by traumatic tear of the ligament and its surrounding tissue. Within this post-traumatic oedema, usually bothersome for analysing the ACL on T2W sequences, we hypothesised that ACL collagen fibres would be more visible on ADC mapping and would thus enable us to verify whether the ligament is or is not continuous.
Our results show that applying ADC mapping to standard T1 and T2 sequences significantly enhances the specificity of MRI for diagnosing complete ACL tears, compared with using the T1 and T2 sequences alone. We also found an increase in sensitivity, non-significant probably because standard MRI sensitivity is already very high. The high positive likelihood ratio clearly demonstrates the advantage of ADC mapping in the positive diagnosis of complete ACL tears, just as the low negative likelihood ratio allows it to be ruled out. ADC mapping applied to traumatic ACLs also improves differentiation between complete and partial tears, compared with previous studies [2, 10, 11, 13] that used only conventional T1 and T2 sequences.
Our results with these conventional MRI sequences alone showed satisfactory sensitivity, but their specificity was only fair (50%), close to the values reported in the literature. Chen et al. [2] reported a sensitivity of 73.3% and a specificity of 64.7% for diagnosis of complete tears, but their population included both recent tears and chronic injuries. Umans et al. [11] reported a sensitivity of 55% and a specificity of 70% for diagnosis of partial tears. Tsai et al. [10] reported a 67% PPV only for the MRI diagnosis of partial ACL tears. Recently, using a 3-T MRI machine and a population of both traumatic and non-traumatic injuries (and 132 normal ACLs in 172 patients), Van Dyck et al. [13] reported better results: with a sensitivity of 77% and a specificity of 97% in diagnosing partial ACL tears, but 13% of the injuries remained misdiagnosed. In a more recent paper on partial ACL tears, with readers blinded to whether ACL injuries resulted from trauma or not, Van Dyck et al. [29] reported that standard T1 and T2 MRI sequences had an accuracy of 25–53% for the diagnosis of partial ACL tears. Our results therefore agree with the literature: standard MRI is not sufficiently accurate to differentiate satisfactorily between complete and partial tears (Figs. 3, 4, and 5).
Bruised and distended ACL in a 25-year-old woman. a Sagittal T2-weighted slice with fat saturation, heterogeneous ACL, fibres not visible in some areas (fine arrows), positive Lachmann test. b Sagittal slice ADC mapping; the ACL is continuous (large white arrows), with no break. c Arthroscopy 1 month later, the ACL is continuous (black star) up to the lateral condyle (LC). MC medial condyle. d Sagittal T2-weighted slice with fat saturation 5 months later, the ACL looks normal (white arrows), Lachmann test still positive (one +) but with a firm anterior endpoint. (Technical characteristics of the sequences are given in Table 1)
Complete ACL tear in a 60-year-old woman, not easily visible with T2-weighted sequences only. a, b Sagittal T2-weighted slices with fat saturation, partial ACL tear with some continuous ligament fibres (fine arrows) visible within the oedema. c, d Sagittal slice ADC mapping, showing complete ACL tear (large arrows) confirmed by TELOS with a 7-mm anterior drawer. (Technical characteristics of the sequences are given in Table 1)
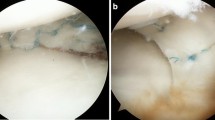
Partial ACL tear in a 43-year-old woman. Sagittal (a), axial (b) and coronal (c) T2-weighted slices with fat saturation, heterogeneity of the ligament fibres (fine arrows) with no visible continuous fibre. Sagittal (d) and axial (e) slice ADC mapping; some ACL fibres seem continuous (arrowheads) as confirmed by TELOS with a 3-mm anterior drawer. (Technical characteristics of the sequences are given in Table 1)
The almost perfect intra-observer agreement between the musculoskeletal radiologists (1 for R1 and 0.85 for R2) in diagnosing complete ACL tears from standard sequences was combined with identical but only fair (0.39) inter-observer agreement on the first and second readings. Krampla et al. [30] had already observed moderate inter-observer correlation (seemingly independent of magnetic field intensity) in diagnosing traumatic ACL injuries with conventional MR sequences. Recently, Van Dyck et al. [29] also observed a substantial difference between intra- and inter-observer correlations in using conventional MR sequences to explore traumatic ACLs. In view of these results, we believe that the reading criteria for standard sequences vary little for an experienced radiologist, but are assessed differently by them and thus give rise to consistent differences in interpretation. For the third reader, the average intra-observer agreement for standard sequences shows a lack of experience.
When diffusion mapping was added, only one reader, R1, had almost perfect intra-observer agreement, undoubtedly because of his greater experience: he was the first to use it and he took part in the development and preliminary experiments. For reader 2, the intra-observer agreement remained moderate (0.45) for the diffusion sequences. However, his sensitivity and specificity improved markedly between the first and second readings of diffusion sequences, with an inter-observer R1–R2 agreement (0.35) that was fair in the first reading and almost perfect (0.81) in the second. R2’s improvement between the two readings was very significant for sensitivity and approached statistical significance for specificity. His improved performance shows the existence of a learning curve, which can also be observed, in R1, whose sensitivity score increased significantly between the first and second readings (91% and 97%), while specificity remained unchanged and equal to the consensus (94%).
For reader 3 (the visceral radiologist), the improvement in inter-observer correlations between the first and second readings of diffusion sequences might also be due to the existence of a learning curve. However, the lack of significant differences in the sensitivity and specificity ratios between the two readings prevents any clear-cut conclusion.
Several limitations to this study require discussion. The first is the association of two different reference standards: arthroscopy and TELOS. Because of its invasive nature, arthroscopy is not usually performed for diagnostic purposes alone. Proposing this procedure to patients with only mild clinical signs or MRI findings raises ethical issues. Although patients with arthroscopic verification had more complete tears (35 of the 42 arthroscopies in our study, i.e. 83%) than reported in the literature [7–9, 31], the difference might introduce a verification bias with both sensitivity and specificity overestimated [31]. Surgical treatment is proposed for partial ACL tears only if it is likely to have significant clinical consequences. Other partial ACL tears are treated with physical rehabilitation alone. Partial tears with clinical consequences that justify surgery constitute a separate group, one that no study has shown to be representative of all partial tears. Combining arthroscopy with a less invasive reference assessment method made it possible to obtain a distribution of complete and partial tears close to that reported in the literature [7–9] without affecting the diagnostic specificity of MRI [31]. Moreover, this procedure eliminates observer bias due to the recruitment of a single type of partial tear. The combination of these two reference methods does not seem to have negatively affected the reliability of MRI sensitivity in our study, as the statistical sensitivity test performed with different TELOS positivity thresholds showed no noticeable differences.
The second limitation is the possibility of recall bias in the second reading of the sets, 4 months later. Thus, precautions were taken to redistribute the sets randomly. The third limitation of the study is the low spatial resolution of the ADC images. However, increasing spatial resolution would require a markedly longer examination time, incompatible with routine radiological practice. A fourth limitation should be mentioned: the possible influence of T1W and T2W sequences (less effective) when read jointly with the DW-MR images. This influence cannot be formally eliminated, but the reading instructions were strict: the appearance of the ACL on the DW-MR images was the only factor that should have determined the diagnosis of a partial or complete tear: the T1W and T2W sequences were read only to provide anatomical landmarks to the readers.
This study of the qualitative use of DW-MR sequences (ADC mapping) associated with conventional MR sequences to assess traumatic ACL injuries shows a clear improvement in diagnostic specificity for differentiating between complete and partial ACL tears with only a short increase in examination time (2 min for each sequence) and a variable reader-dependent learning curve. Reliable visualisation of partial tears will make it possible to propose non-surgical orthopaedic treatment straightaway [32] or to plan single-bundle reconstruction surgery [33].
Abbreviations
- ACL:
-
Anterior cruciate ligament
- DW-MRI:
-
Diffusion-weighted magnetic resonance imaging
- ADC:
-
Apparent diffusion coefficient
References
McCauley TR, Moses M, Kier R et al (1994) MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR Am J Roentgenol 162:115–119
Chen WT, Shih TT, Tu HY et al (2002) Partial and complete tear of the anterior cruciate ligament. Acta Radiol 43:511–516
Gentili A, Seeger LL, Yao L et al (1994) Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology 193:835–840
Lawrance JA, Ostlere SJ, Dodd CA (1996) MRI diagnosis of partial tears of the anterior cruciate ligament. Injury 27:153–155
Robertson PL, Schweitzer ME, Bartolozzi AR et al (1994) Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology 193:829–834
Tung GA, Davis LM, Wiggins ME et al (1993) Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology 188:661–667
Bomberg BC, McGinty JB (1990) Acute hemarthrosis of the knee: indications for diagnostic arthroscopy. Arthroscopy 6:221–225
DeHaven KE (1980) Diagnosis of acute knee injuries with hemarthrosis. Am J Sports Med 8:9–14
Noyes FR, Bassett RW, Grood ES et al (1980) Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am 62(687–95):757
Tsai KJ, Chiang H, Jiang CC (2004) Magnetic resonance imaging of anterior cruciate ligament rupture. BMC Musculoskelet Disord 5:21
Umans H, Wimpfheimer O, Haramati N et al (1995) Diagnosis of partial tears of the anterior cruciate ligament of the knee: value of MR imaging. AJR Am J Roentgenol 165:893–897
Yao L, Gentili A, Petrus L et al (1995) Partial ACL rupture: an MR diagnosis? Skeletal Radiol 24:247–251
Van Dyck P, Vanhoenacker FM, Gielen JL et al (2011) Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skeletal Radiol 40:701–707
Yoon YC, Kim SS, Chung HW et al (2007) Diagnostic efficacy in knee MRI comparing conventional technique and multiplanar reconstruction with one-millimeter FSE PDW images. Acta Radiol 48:869–874
Logan M, Dunstan E, Robinson J et al (2004) Tibiofemoral kinematics of the anterior cruciate ligament (ACL)-deficient weightbearing, living knee employing vertical access open “interventional” multiple resonance imaging. Am J Sports Med 32:720–726
Niitsu M (2001) Kinematic MR imaging of the knee. Semin Musculoskelet Radiol 5:153–157
Kwon JW, Yoon YC, Kim YN et al (2009) Which oblique plane is more helpful in diagnosing an anterior cruciate ligament tear? Clin Radiol 64:291–297
Le Bihan D, Breton E, Lallemand D et al (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 168:497–505
Baur A, Stabler A, Bruning R et al (1998) Diffusion-weighted MR imaging of bone marrow: differentiation of benign versus pathologic compression fractures. Radiology 207:349–356
Friedrich KM, Mamisch TC, Plank C et al (2010) Diffusion-weighted imaging for the follow-up of patients after matrix-associated autologous chondrocyte transplantation. Eur J Radiol 73:622–628
Garces GL, Perdomo E, Guerra A et al (1995) Stress radiography in the diagnosis of anterior cruciate ligament deficiency. Int Orthop 19:86–88
Kobayashi S, Terayama K (1993) Quantitative stress radiography for diagnosis of anterior cruciate ligament deficiency. Comparison between manual and instrumental techniques and between methods with knee flexed at 20 degrees and at 90 degrees. Arch Orthop Trauma Surg 112:109–112
Mononen T, Alaranta H, Harilainen A et al (1997) Instrumented measurement of anterior-posterior translation in knees with chronic anterior cruciate ligament tear. Arch Orthop Trauma Surg 116:283–286
Beldame J, Bertiaux S, Roussignol X et al (2011) Laxity measurements using stress radiography to assess anterior cruciate ligament tears. Orthop Traumatol Surg Res 97:34–43
Fleiss JL (1981) Statistical methods for rates and proportions, 2nd edn. Wiley, New York
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Le Bihan D, Turner R, Douek P et al (1992) Diffusion MR imaging: clinical applications. AJR Am J Roentgenol 159:591–599
Cieszanowski A, Anysz-Grodzicka A, Szeszkowski W et al. (2012) Characterization of focal liver lesions using quantitative techniques: comparison of apparent diffusion coefficient values and T2 relaxation times. Eur Radiol. doi:10.1007/s00330-012-2519-x
Van Dyck P, De Smet E, Veryser J et al (2012) Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc 20:256–261
Krampla W, Roesel M, Svoboda K et al (2009) MRI of the knee: how do field strength and radiologist’s experience influence diagnostic accuracy and interobserver correlation in assessing chondral and meniscal lesions and the integrity of the anterior cruciate ligament? Eur Radiol 19:1519–1528
Nishikawa H, Imanaka Y, Sekimoto M et al (2010) Verification bias in assessment of the utility of MRI in the diagnosis of cruciate ligament tears. AJR 195:W357–W364
Barrack RL, Buckley SL, Bruckner JD et al (1990) Partial versus complete acute anterior cruciate ligament tears. The results of nonoperative treatment. J Bone Joint Surg Br 72:622–624
Bellier G, Christel P, Colombet P et al (2004) Double-stranded hamstring graft for anterior cruciate ligament reconstruction. Arthroscopy 20:890–894
Acknowledgments
We thank all the patients who agreed to take part in this study. We also thank Irène Boulloche for her editorial assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Delin, C., Silvera, S., Coste, J. et al. Reliability and diagnostic accuracy of qualitative evaluation of diffusion-weighted MRI combined with conventional MRI in differentiating between complete and partial anterior cruciate ligament tears. Eur Radiol 23, 845–854 (2013). https://doi.org/10.1007/s00330-012-2633-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2633-9