Abstract
Purpose
To provide a systematic review of the literature regarding five topics in meniscal allograft transplantation (MAT): optimal timing for transplantation, outcomes, return to competition, associated procedures, and prevention of osteoarthritis.
Methods
A systematic literature search was conducted using the PubMed (MEDLINE), ScienceDirect, and EBSCO-CINAHL databases. Articles were classified only in one topic, but information contained could be reported into other topics. Information was classified according to type of study (animal, in vitro human, and in vivo human) and level of evidence (for in vivo human studies). Specific inclusion criteria were determined for the outcomes and prevention of osteoarthritis topics.
Results
Twenty-four studies were finally included: two optimal timing, seven outcomes, three return to competitive sport, 16 MAT and associated procedures, and 5 MAT and prevention of osteoarthritis (some studies were categorized in more than one topic). These studies corresponded to 2 animal studies and 31 in vivo human studies (1 level II, 1 level III, and 29 level IV).
Conclusions
The principal conclusions were as follows: (a) there is no evidence to support that MAT has to be performed at the same time or immediately after meniscectomy to prevent development of postmeniscectomy syndrome; (b) MAT successfully improves symptoms, function, and quality of life at 7-to-14 years of follow-up (level IV evidence); (c) the overall failure rate (need for knee arthroplasty) is 10–29 % at long-term follow-up; (d) MAT allows return to same level of competition in 75–85 % of patients at short- to mid-term follow-up (only three studies level IV evidence with small sample size); (e) associated cartilage procedures or anterior cruciate ligament reconstruction to MAT does not worsen the results; (f) MAT may prevent progression of cartilage damaged at long-term follow-up, but may not prevent degeneration in previously healthy cartilage.
Level of evidence
Systematic review of level II–IV studies, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal injuries are very common injuries in the world [38]. Many meniscal tears cannot be repaired, and partial or total meniscectomy is the only management option to improve the patient’s symptoms. However, the loss of meniscal tissue has been associated with early onset knee osteoarthritis due to a decrease in tibiofemoral contact area and an increase in joint contact pressures, especially among active people [10, 17, 44]. Meniscal allograft transplantation (MAT) has become a powerful tool in experienced hands with proven clinical and functional efficacy in relatively young and active meniscectomized symptomatic patients; however, there are many controversial aspects not clearly elucidated yet.
Most of the original and review studies available in humans have focused on the outcomes but very few on specifically reviewing the optimal timing for MAT, return to competitive sports, MAT and associated procedures, and prevention of osteoarthritis with MAT [15, 22, 23, 29]. Moreover, review studies regarding the outcomes of MAT have not been restrictive enough in terms of minimum follow-up and sample size as inclusion criteria [15, 22, 23, 29]. In addition, there has been a huge increase in the number of studies related to MAT in the last decade. Therefore, an updated systematic review on the optimal timing for MAT, outcomes, return to competition, MAT and associated procedures, and prevention of osteoarthritis with MAT (with studies reviewed based on its methodological quality and level of evidence) is timely. This article may help the surgeon on the decision-making regarding several aspects related to MAT that may influence the final clinical outcome and may also serve to generate ideas for future research regarding areas with still controversy.
This is part two of a two parts review article addressing controversial questions in MAT. The purpose of this study was to provide a comprehensive and updated systematic review of the literature regarding five controversial topics: optimal timing for MAT, outcomes, return to competitive sports, associated procedures, and prevention of osteoarthritis.
Materials and methods
The methodology of this study was reported in a concomitant article (Part 1 of this systematic review on MAT) [43] and following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement for systematic reviews [31].
Eligibility criteria
All studies investigating aspects related to MAT were initially approached for eligibility. Studies were included if they were animal or human studies, in vitro or in vivo studies, level of evidence between I and IV for clinical human studies, written in English language, and contained information on the topics targeted for this study. The 5 topics were selected in consensus among all co-researchers and were based on own experience and existing literature. Specific inclusion criteria were established for clinical studies evaluating the outcomes of MAT and the relationship between MAT and osteoarthritis: minimum follow-up of 5 years and minimum sample size of 20 patients. Other systematic review and meta-analyses were excluded from the systematic search but taken into account to assist in discussion and conclusions on each topic.
Information sources and search
Electronic and other search strategies
The initial electronic literature search has been described in the concomitant article (Part 1) [43]. The same databases for the same period of time and the same keywords were used by the same researcher. Also, the reference lists of all included articles and systematic review/meta-analyses encountered were reviewed to search for potential studies not previously identified.
Data collection and analysis
Study selection
Study selection methodology was the same as the Part 1 article and also conducted by the same researchers [43].
Data collection process
The data collection process was the same as the Part 1 article, but for the other topics included [43]. Information regarding the 5 topics included in Part 2 of this systematic review on MAT was extracted in a systematic fashion from included studies by 1 researcher. Data extraction was then verified by the rest of the researchers. Articles were classified in each topic according to the principal purpose of the investigation. Articles were classified in more than one topic only if secondary purposes were reported with enough quality and extension. For each topic, information was classified according to the type of study (animal study, in vitro human studies, and in vivo human studies) and level of evidence (for in vivo human studies). Conclusions were established for each topic. This decision was made in consensus between 2 researchers. The topics included:
-
1.
Immediate versus delayed MAT: What is the optimal timing?
-
2.
Outcomes: What happens in the long-term follow-up?
-
3.
Competitive sports: Is MAT an effective option for athletes at a competitive level?
-
4.
Associated procedures: Does it make a difference when MAT is associated with concomitant procedures?
-
5.
Osteoarthritis: What is the role of MAT in the prevention of knee osteoarthritis?
Assessment of the risk of bias
The methodological quality of the included studies was evaluated through a summary table of several important aspects potentially related to bias in the investigation of MAT, as previously reported in more detail in Part 1 of this systematic review [43]. This assessment was performed by answering yes, no, unknown, or not clearly reported to the following information from each study: purpose clearly stated, prospective nature clearly defined, concealed allocation, similarities at baseline between groups, blinding of participants, blinding of data collectors, blinding of outcome assessor, similar distribution of athletes and/or athletes at competitive level between groups, similar distribution of associated procedures between groups, similar distribution of previous major knee injuries and/or osteoarthritic changes between groups, no graft irradiation reported and comparable distribution between groups, similar surgical technique between groups, similar graft preservation techniques between groups, acceptable compliance, acceptable dropout rate, duration of intervention comparable between groups, and intention-to-treat analysis. A final quality score was given for each study, where yes was 1 point and any other responses (no, unknown, not clearly reported) were 0 points. The assessment of the risk of bias in included studies was based on the articles by Aaltonen et al. [3] and Slim et al. [46].
Results
Study selection
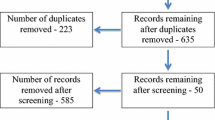
The literature search elicited a total of 1,548 references (PubMed = 753; ScienceDirect = 570; EBSCO-CINAHL = 225), from which 1,407 were excluded because of duplicates, non-English articles, case reports, review articles, technical notes, unrelated studies, studies not reporting on the topics considered for the present study (Fig. 1). A total of 141 studies were reviewed in full text: 61 were excluded because were related to topics included in Part 1 of this systematic review [43], and 56 were excluded because did not meet specific inclusion criteria for the targeted topics. Therefore, 24 articles met the final inclusion criteria for the current systematic review.
Characteristics of the Studies
The number of studies included in each topic was as follows: MAT timing 2, MAT outcomes 7, MAT in competitive athletes 3, MAT and associated procedures 16, and MAT and osteoarthritis 5. Of the 24 studies, 2 were animal studies, and 22 were in vivo human studies. Further characteristics of included studies are specified in each section. Table 1 summarizes the assessment of the risk of bias for the included studies. The information extracted from all included studies in each of the 5 topics was as follows:
Immediate versus delayed MAT: What is the optimal timing?
Only two studies were found focusing on this topic, which specifically compared the immediate versus delayed MAT [2, 36].
Animal studies
Aagaard et al. [2] conducted an animal study in sheep comparing the effects of immediate and delayed MAT on articular cartilage. There were 4 groups evaluated 6 months after surgery: control knees, meniscectomized knees (all medial menisci), immediate MAT, and 3-month delayed MAT. The authors fixed the medial menisci horns with sutures through bone tunnels. They found that articular cartilage degeneration was higher in the meniscectomized and delayed MAT groups compared to controls and immediate MAT, but the latter was higher than control knees. The authors concluded that immediate MAT reduced but did not prevent articular cartilage degeneration and immediate MAT was more effective at preventing cartilage degeneration compared to delayed MAT. Rijk et al. [36] observed in rabbits that immediate MAT provided a protective effect on articular cartilage at 1 year of follow-up, whereas delayed transplantation leads to more degenerative changes than meniscectomy only.
Outcomes of MAT
The initial literature search elicited 46 studies reporting clinical, functional, and radiographic outcomes after MAT. However, after applying the more restrictive inclusion criteria, only 7 studies (all but 1 were case series, level IV evidence) were finally included in this systematic review.
In vivo human studies
Level evidence: 2
Wirth et al. [55] reported the long-term results of MAT plus anterior cruciate ligament (ACL) reconstruction in a series of 23 patients followed at 14 years postoperatively. The authors compared these patients to two control groups consisting of ACL reconstruction with intact menisci and with meniscectomy. At 14 years, the mean Lysholm was 75 points. They used 17 lyophilized and 6 deep-frozen allografts. It was found that, overall, deep-frozen meniscal allografts had better results than lyophilized allografts. In fact, the latter demonstrated a reduction in size at second look, showing results more comparable to the meniscectomy group. In contrast, the deep-frozen allografts were more comparable to the intact meniscus group.
Level evidence: 4
Verdonk et al. [50] have reported 1 study with long-term follow-up related to case series of MAT. In 2006, this group reported the long-term clinical and radiological results of MAT in a series of 41 patients (minimum follow-up of 10 years). All patients were divided into 3 groups: lateral MAT, medial MAT, medial MAT plus associated high tibial osteotomy. All groups improved the modified HSS score at final follow-up, but the KOOS revealed disability, symptoms, and reduced quality of life. Forty-one per cent had no progression of joint space narrowing assessed by radiographs, and 35 % assessed with magnetic resonance imaging (MRI). A total of 7 patients (18 %) had to undergo total knee arthroplasty during the follow-up.
Hommen et al. [24] reported the results of MAT using cryopreserved allograft with a follow-up of 10 years. The authors observed a failure rate of 25 and 50 % for the medial and lateral MAT, respectively. There was a significant improvement in Lysholm score and pain. The overall improvement in Lysholm score and pain occurred in 90 % of patients. The authors observed no differences between medial and lateral MAT and between the use of bone plugs or soft tissue fixation. Sixty-six per cent of cases available for MRI showed joint space narrowing and 80 % progression to degenerative joint disease.
Van der Wal et al. [48] reported their long-term results of MAT in 57 patients using cryopreserved grafts. The overall failure rate was 29 %. Overall, the Lysholm score significantly improved in the post-operative compared to preoperative values. There were no differences in Lysholm score between non-failed and failed cases undergoing knee arthroplasty. Although function improvements decrease in the long term, the authors concluded that this is an appropriate procedure for younger patients to delay total knee arthroplasty.
González-Lucena et al. [20] reported the results of MAT without bone blocks at 5- to 8-year follow-up in 33 patients. The authors observed that the Lysholm and Tegner scores significantly improved after surgery. Also, pain significantly decreased and joint space narrowing was not significantly impaired. They reported a survival rate of 87 % at a mean of 6.5 years post-operatively and 33 % of complications.
Vundelinckx et al. [54] published a medium-term subjective, clinical, and radiographic outcome evaluation of 49 patients undergoing MAT at a 5- to 15-year follow-up. The failure rate was 10 %, which corresponded to 5 patients that needed a total knee arthroplasty. The authors found a significant decrease in pain and increase in KOOS, Lysholm, and SF-36 score, with no modifications in Tegner score. The outcomes were not different for medial and lateral MAT and did not correlate with alignment deviation, gender, and body mass index.
Saltzman et al. [42] reported their results with MAT with a minimum follow-up of 7 years in 22 patients. All patients significantly improved the quality of life, Lysholm, IKDC, and KOOS, with excellent satisfaction (8.8 out of 10 points). The overall successful rate was 88 %. The improvements were comparable when comparing the medial and lateral MAT.
Return to competitive sports
There were only 3 studies (all of them were case series) that performed MAT in competitive athletes and evaluated the return to competition [6, 11, 28].
In vivo human studies
Level evidence: 4
Alentorn-Geli et al. [6] reported the return to competition (among other outcomes) of soccer players undergoing MAT with a follow-up of 2 to 5 years (mean 3 years). The sample was composed of 14 players with Tegner scores 9 and 10 and a mean age of 28 years. The authors reported a return to competition in 12 of 14 players (85.7 %).
Chalmers et al. [11] reported the return to sports in high school, collegiate, and professional athletes (mean Tegner score of 8) in 13 patients after MAT. The athletes had a mean age of 19.8 years and a mean follow-up of 3.3 years. The authors observed that 10 of 13 patients (77 %) returned to their desired level of play after MAT.
Finally, Marcacci et al. [28] reported the return to sports in 12 professional (Tegner score 10) soccer players after MAT at a mean follow-up of 3 years. The sample included players with a mean age of 24 years and corresponded to 6 medial MAT and 6 lateral MAT. The authors found that 11 of 12 patients (92 %) returned to play soccer after MAT. Of these 11 patients, 9 patients (75 %) returned to the same professional level (Tegner score 10), and 2 patients (17 %) returned to a semi-professional level (Tegner score 9) at a mean of 3 years post-operatively. The mean time to return to competition was 10 months.
MAT and associated procedures
Sixteen studies were found specifically reporting the results of MAT in combination with other surgical procedures, all level IV (except one level III evidence) studies in humans.
In vivo human studies
Level evidence: 3
Rueff et al. [40] reported a study comparing ACL reconstruction with or without medial MAT with a minimum follow-up of 5 years and a sample size 16 of patients. The patients without medial MAT had meniscal repair or partial meniscectomy. The authors found that both groups had comparable improvements in Lysholm score, pain, and subjective IKDC, with the exception of swelling which better improved in the non-MAT group. Eighty-seven per cent of patients in the MAT group and 100 % in the non-MAT group considered their procedure a success.
Level evidence: 4
Graf et al. [21] reported the results of MAT combined with ACL reconstruction at a minimum of 8.5 years of follow-up. The authors included 8 patients and found that the IKDC symptoms were normal in 2 patients, nearly normal in 5 patients, and abnormal in 1 patient. The IKDC function was normal in 5, nearly normal in 1, and abnormal in 2 patients. Six of the 8 patients were pleased with the function level of the knee and were involved in recreational sports. This study concluded that MAT plus ACL reconstruction produces adequate results in terms of function and satisfaction in long-term follow-up.
Binnet et al. [9] reported 19-year follow-up results of lyophilized medial MAT in 4 ACL-deficient patients with ligament reconstruction. Comparing preoperative and post-operative values at 19 years of follow-up, the authors found that the median Tegner score decreased from 3 to 2.5, the median Lysholm score increased from 60.5 to 62.5, and the median total KSS score decreased from 60.5 to 59.5, respectively. No patients demonstrated symptoms of instability. All patients had Outerbridge grade IV osteoarthritis by X-ray examination.
Sekiya et al. [45] reported the clinical outcomes of MAT and ACL reconstruction in a retrospective case series involving 28 patients at an average of 2.8 years. The subjective IKDC score was normal or nearly normal in 86, and 90 % for the objective IKDC (Lachman and pivot shift tests). The quality of life (assessed with the physical and mental component summaries of the SF-36) was higher than age- and sex-matched reference population. The authors found no changes in joint space narrowing compared to the contralateral knee.
Wirth et al. [55] reported the long-term results of MAT plus ACL reconstruction in a series of 23 patients followed at 14 years post-operatively. The authors compared these patients to two control groups consisting of ACL reconstruction with intact menisci and with meniscectomy. At 14 years, the mean Lysholm was 75 points. They used 17 lyophilized and 6 deep-frozen allografts. It was found that overall, deep-frozen meniscal allografts had better results than lyophilized allografts. In fact, the latter demonstrated a reduction in size at second look, showing results more comparable to the meniscectomy group. In contrast, the deep-frozen allografts were more comparable to the intact meniscus group.
Regarding MAT associated with articular cartilage procedures, there are also several studies included. Bhosale et al. [8] reported the results of MAT combined with autologous chondrocyte implantation. The sample was 8 patients with a mean age of 43 years with kissing chondral defects. Mean Lysholm score increased from 49 to 66 at 1 year, with all patients achieving an active lifestyle. However, although only 5 patients could maintain the improvements at 3.2 years of follow-up, the authors reported no deleterious effects of this combination of procedures.
The same procedures were combined by Farr et al. [18] in a case series initially involving 36 patients with a minimum follow-up of 2 years. The authors found that patients significantly improved the Browne Cincinnati score and Lysholm score and significantly improved their pain assessed with the visual analogue scale. The patients were satisfied with the procedure. They found no differences for medial or lateral femoral condyle cartilage procedure.
Rue et al. [39] reported a prospective case series involving 31 patients at a minimum of 2 years of follow-up who underwent MAT plus autologous chondrocyte implantation or osteochondral allograft. At a mean follow-up of 3.1 years, there was a significant improvement in Lysholm, IKDC, and SF-12. Seventy-six per cent of patients were completely or mostly satisfied with their results, and, overall, 48 % of patients were classified as normal or nearly normal in the IKDC.
Gomoll et al. [19] reported the results of 7 patients treated with a combination of MAT, chondral repair, and osteotomy followed for a mean of 2 years. The authors found significant improvements in IKDC, Lysholm, and KOOS functional scores. In addition, 6 of 7 patients were able to return to their normal activities with no restriction.
There are some studies previously reviewed in the “outcomes” topic that can also be shortly included in the present topic. Verdonk et al. [50] observed that the combination of medial MAT and high tibial osteotomy demonstrated better improvements in terms of pain, HSS score, and KOOS score compared to isolated medial MAT. Also, Saltzman et al. [42] reported their results in a subgroup analysis compared isolated MAT versus MAT and associated procedures. The authors found that the “combined” group had greater Lysholm, KOOS pain, and KOOS quality of life compared to the “isolated” group.
There were 5 studies (all level IV evidence) that were initially classified in the “outcomes” topic but could not be finally included because they did not meet the specific inclusion criteria set for this topic. These studies were not specifically aimed to compare MAT and MAT plus associated procedures, but reported this subgroup comparison [12, 24, 33, 35, 41]. All 5 studies did not compare any specific associated procedure, but reported isolated MAT compared to MAT and any associated procedure (including mostly ACL reconstruction, cartilage repair procedures, and osteotomies). Therefore, no conclusions could be elaborated for any specific associated procedure. Essentially, these studies found that the association of other procedures did not elicit significantly worst clinical, functional, and radiographic outcomes compared to isolated MAT, except for greater improvement in role physical in “combined” group compared to “isolated” group [35].
MAT and osteoarthritis
All of the included studies in this section have been previously reviewed in the “outcomes” topic. Whenever possible, only studies reporting isolated MAT were considered for this section to avoid the influence of concomitant injuries or procedures on the risk of osteoarthritis. Five studies were finally included in this section, all of them level IV evidence.
In vivo human studies
Level of evidence: 4
Verdonk et al. [50] found that 52 % of patients did not show any change in join space width in a cohort of patients followed for a mean of 12 years, but all patients considered failure cases who needed total knee arthroplasty had progression of joint space narrowing. The join space remained unchanged in 41 % of patients considering both the success and failure cases. Most patients (34 %) had only 1 degree of progression. Regarding MRI, 47 % of patients demonstrated no progression of degeneration of the femoral cartilage at a mean of 12 years of follow-up, and 29 % demonstrated progression of only 1 grade. In the tibial articular cartilage, 41 % demonstrated no progression of cartilage degeneration. Regarding the subgroup of isolated medial MAT, 31 % had grade III degenerative changes, but all of them were already present just 1 year after surgery and did not progress at final follow-up. For the lateral MAT, there was a progression of articular degeneration in 13 % of patients.
Hommen et al. [24] observed that 10 of 15 patients (66 %) had significant narrowing of the tibiofemoral compartment of a mean of 1 mm. Their study had a mean follow-up of 141 months. Fifty-four per cent of patients had progression of Fairbank degenerative joint disease score in the transplanted compartment. Regarding the use of MRI in the 7 patients available for this imaging study (30 %), 1 was classified as normal cartilage, 2 of mild degeneration, 3 as moderate, and 1 as severe degeneration.
Gonzalez-Lucena et al. [20] reported their results of MAT without bone blocks in 33 patients with a follow-up between 5 and 8 years. On Rosenberg’s view of plain radiographs, they observed no significant narrowing of the join space in the preoperative (mean join space 3.19 mm) and post-operative periods (mean join space 3.21 mm).
Vundelinckx et al. [54] reported the results of MAT in 49 patients with a follow-up between 5 and 15 years. The authors employed the Kellgren-Lawrence radiographic classification to assess knee osteoarthritic changes. They found a significant increase in the level of osteoarthritis in the post-operative compared to preoperative period. Fifty-eight per cent of patients had no increase in the degree of osteoarthritis, but 24 % of patients increased by 1 degree, 18 % by 2 degrees, and no patients with increase in 3 degrees (Kellgren-Lawrence grade IV osteoarthritis).
Saltzman et al. [42] reported their results of MAT with a mean follow-up of 8.5 years (minimum 7 years) in 22 patients. Only 6 of the 22 patients were evaluated with radiographs at last follow-up. At last follow-up of these patients (range from 7.46 years to 10 years), the authors observed progression of joint space narrowing with mild-to-moderate changes in 2 patients (both had combined MAT plus osteochondral allograft procedure), minor-mild joint space narrowing in 2 patients, and preservation of joint space narrowing in 2 patients. Of the 3 failed cases, 2 were not related to progression of osteoarthritis (but with graft rupture or degeneration) and 1 had persistent pain and symptoms with already focal grade IV tibial plateau changes at the time of MAT.
Discussion
The principal findings of this systematic review have been summarized in the conclusions section. The methodological quality of the included studies is, in general, suboptimal. Conclusions mostly come from in vivo clinical studies with level IV evidence. In fact, nearly all studies are case series that have made subgroup comparisons for specific issues.
There are a lot of references reporting the clinical outcomes of MAT. Generally, most of the current “outcome-focused” studies are showing consistent good clinical and functional results in relatively young and active meniscectomized symptomatic patients. However, the most valuable and meaningful conclusions are obtained from studies with longest follow-up and appropriate sample size. In general, studies with shorter follow-up have reported very good outcomes regardless of the surgical technique employed, fixation method, type of patients, or associated procedures [4–7, 11, 15, 22, 23, 29, 33, 51]. The most relevant information regarding the outcomes of MAT procedure has to do with the long-term follow-up. The study with the longest follow-up was reported by von Lewinski et al. [52], but the sample size was only 5 patients. The study was a case series where the patients underwent MAT plus ACL reconstruction and advancement of the medial collateral ligament. In this study, the authors found that the Lysholm score increased from 21 to 97 points, the KOOS from 28 to 91, and the IKDC was nearly normal in 2, abnormal in 2, and severely abnormal in 1 patient. They observed that all patients had progression of radiographically assessed knee osteoarthritic changes although they did demonstrated relatively good clinical and functional outcomes. It is important when evaluating the effects of MAT to have at least one group of patients undergoing isolated MAT, controlling for most of the factors than can influence the results (Table 1). It might be argued that differences in demographic characteristics, distribution of athletes, associated surgical procedures, previous major knee injuries associated with the meniscal “problem”, or differences in graft sterilization, preservation, or the surgical technique itself could influence, among other factors, the outcomes of MAT. The control of all these parameters in a study with long-term follow-up and relatively large sample size has not been reported to date. Despite these limitations, it can be concluded from the available literature that MAT produces good outcomes in the long term and this procedure is, therefore, worthwhile and justified in well-selected individuals, whenever any associated condition is concomitantly or beforehand corrected. Interestingly, Verbruggen et al. [49] reported the revision of MAT in the long-term follow-up. Eighty-nine transplants in 87 patients were performed, and at a mean of 16.2 years follow-up, 68 transplants in 68 patients survived and the rest had to be converted to knee arthroplasty because of progression of osteoarthritis. The authors found that patients undergoing knee arthroplasty for failed MAT had a tendency for lower scores than patients with primary knee arthroplasty, but the former group still had better clinical outcomes than prior to MAT. Therefore, MAT would be justified because it may delay the need for knee arthroplasty for many years without a clear impact on subsequent clinical outcomes for the knee replacement procedure.
The most common associated procedures with MAT are ACL reconstruction and cartilage-related procedures, although high tibial osteotomy is also commonly performed. Overall, the evidence clearly indicates that the association of other procedures does not worsen the results of MAT. This is especially true for ACL reconstruction and cartilage procedures [22, 23]. However, many studies have not compared isolated versus combined procedures but, instead, are case series where patients underwent MAT and other surgical procedures aimed to correct other disorders [22, 23, 29]. Some studies have a low number of patients with associated procedures, so no clear conclusions can be drawn without a risk of type II error if a statistical analysis is purported. The recommendation clearly points out to correct any disorder before or during the MAT. The association of high tibial osteotomy or distal femoral osteotomy has been less investigated, but it is accepted that any axial malalignment has to be corrected in order to indicate a MAT [51]. It is not clear whether MAT and osteotomy are better than osteotomy alone, so further research is necessary.
There are numerous studies investigating the effects of MAT on articular cartilage integrity, preservation, or contact area and pressure mechanics in both the animal and in vitro human model (human cadaver studies). However, this evidence may not be related to what actually happens in the long-term follow-up of patients. It has been demonstrated that MAT in sheep [1, 26, 47, 53] and rabbits [13, 36] protects the articular cartilage from degeneration. However, other studies have reported no benefit of MAT on the prevention of knee osteoarthritis in sheep [14, 32] and rabbits [37], whereas others have reported only partial protection in dogs [16, 32]. In vitro human studies have demonstrated the biomechanical benefits of MAT in terms of reduced peak contact pressure compared to meniscectomized knees [25, 30, 34] and increased contact area [34], but MAT does not restore contact mechanics to that of normal knees [27]. Positive findings in terms of articular cartilage benefits in animals and in vitro human studies seem to agree with some clinical studies [20, 50], but other studies in humans have not reported clear benefits on articular cartilage [24, 54]. Overall, there are only few studies with long-term follow-up evaluating the effects of MAT in articular cartilage in humans. It should be noted that studies with the longest follow-up are also those with the smallest sample size. Therefore, in many cases, no statistical analysis was provided because of this limited sample size in each subgroup of radiographic degeneration. Another important issue has to do with the control of other causes of osteoarthritis in these studies. Investigations regarding osteoarthritis have to be conducted with isolated MAT to assess adequately the effects of meniscal transplant, as ACL reconstruction and cartilage restoration procedures, may contribute to the development of osteoarthritis.
This study has some limitations. First, it only used three databases for literature search and only English-written articles were included which may increase the risk of missing some interesting references. Second, there is a risk of publication bias by not including “negative” studies that were finally not published. Third, the high heterogeneity of the measurement methods, methodological quality, and way to report the results make any comparison highly difficult. Fourth, it is difficult to draw significant conclusions due to the limited sample sizes for some of the topics reviewed. Despite these limitations, this systematic review provides a comprehensive and updated review of the literature regarding five relevant topics in MAT and provides evidence-based statements that may be helpful to draw conclusions on each topic and identify areas for future research.
Conclusions
The principal conclusions of this systematic review (provided according to the level of evidence whenever available) for each topic included are as follows:
-
1.
Immediate versus delayed MAT:
-
There is minimal information available regarding the optimal timing for MAT to prevent postmeniscectomy syndome or cartilage degeneration (only animal studies with short follow-up). Future studies are needed, especially for this topic.
-
-
2.
Outcomes:
-
MAT is a successful surgical procedure to improve symptoms, function, and quality of life at 7 to 14 years of follow-up (level IV evidence).
-
The overall failure rate (need for knee arthroplasty) ranges from 10 to 29 % in the long-term follow-up (level IV evidence).
-
There are no differences in the clinical and functional outcomes between the medial and lateral MAT (level IV evidence).
-
-
3.
Competitive sports:
-
MAT allows return to the same level of competition in 75–85 % of patients in the short- to mid-term follow-up (level IV evidence).
-
MAT does not preclude returning to soccer at high-level professional competition (Tegner score 10) level (level IV evidence).
-
The number of studies and samples size regarding return to sports and results in competitive sports is very limited. Further research is needed.
-
-
4.
MAT and associated procedures:
-
The association of cartilage procedures (level IV evidence) or ACL reconstruction (level III evidence) with MAT does not worsen the results.
-
The evidence for the effects of associated osteotomies in MAT is not conclusive.
-
Most studies have not specifically compared isolated MAT versus combined procedures, but have reported good results in case series with MAT and associated procedures (level IV evidence).
-
-
5.
Osteoarthritis:
-
Many patients have focal chondral lesions or some degree of diffuse compartment cartilage degeneration at the time of MAT (level IV evidence).
-
It seems that MAT may prevent progression of cartilage degeneration in the long-term follow-up (level IV evidence).
-
The prevention effect of MAT on the development of knee osteoarthritis in cartilage injury-free individuals has not been demonstrated.
-
Studies with longest follow-up (included in this topic) were also those with smallest sample sizes. Therefore, no definitive conclusions can be drawn.
-
References
Aagaard H, Jorgensen U, Bojsen-Moller F (1999) Reduced degenerative articular cartilage changes after meniscal allograft transplantation in sheep. Knee Surg Sports Traumatol Arthrosc 7:184–191
Aagaard H, Jorgensen U, Bojsen-Moller F (2003) Immediate versus delayed meniscal allograft transplantation in sheep. Clin Orthop Relat Res 406:218–227
Aaltonen S, Karjalainen H, Heinonen A, Parkkari J, Kujala UM (2007) Prevention of sports injuries: systematic review of randomized controlled trials. Arch Intern Med 167:1585–1592
Abat F, Gelber PE, Erquicia JI, Pelfort X, Gonzalez-Lucena G, Monllau JC (2012) Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med 40:1591–1596
Abat F, Gelber PE, Erquicia JI, Tey M, Gonzalez-Lucena G, Monllau JC (2013) Prospective comparative study between two different fixation techniques in meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc 21:1516–1522
Alentorn-Geli E, Seijas R, Alvarez P, Cuscó X, Cugat R (2010) Arthroscopic meniscal transplants in soccer players: outcomes at 2- to 5-year follow-up. Clin J Sport Med 20:340–343
Alentorn-Geli E, Seijas R, García M, Álvarez P, Steinbacher G, Cuscó X, Rius M, Cugat R (2011) Arthroscopic meniscal allograft transplantation without bone plugs. Knee Surg Sports Traumatol Arthrosc 19:174–182
Bhosale AM, Myint P, Roberts S, Menage J, Harrison P, Ashton B, Smith T, McCall I, Richardson JB (2007) Combined autologous chondrocyte implantation and allogenic meniscus transplantation: a biological knee replacement. Knee 14:361–368
Binnet MS, Akan B, Kaya A (2012) Lyophilised medial meniscus transplantations in ACL-deficient knees: a 19-year follow-up. Knee Surg Sports Traumatol Arthrosc 20:109–113
Burke DL, Ahmed AH, Miller J (1978) A biomechanical study of partial and total medial meniscectomy of the knee. Trans Orthop Res Soc 3:91
Chalmers PN, Karas V, Sherman SL, Cole BJ (2013) Return to high-level sport after meniscal allograft transplantation. Arthroscopy 29:539–544
Cole BJ, Dennis MG, Lee SJ, Nho SJ, Kalsi RS, Hayden JK, Verma N (2006) Prospective evaluation of allograft meniscus transplantation: a minimum 2-year follow-up. Am J Sports Med 34:919–927
Cummins JF, Mansour JN, Howe Z, Allan DG (1997) Meniscal transplantation and degenerative articular cartilage: an experimental study in the rabbit. Arthroscopy 13:485–491
Edwards DJ, Whittle SL, Nissen MJ, Cohen B, Oakeshott RD, Keene GC (1996) Radiographic changes in the knee after meniscal transplantation. An experimental study in a sheep model. Am J Sports Med 24:222–226
ElAttar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P (2011) Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc 19:147–157
Elliott DM, Jones R 3rd, Setton LA, Scully SP, Vail TP, Guilak F (2002) Joint degeneration following meniscal allograft transplantation in a canine model: mechanical properties and semiquantitative histology of articular cartilage. Knee Surg Sports Traumatol Arthrosc 10:109–118
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg Br 30:664–670
Farr J, Rawal A, Marberry KM (2007) Concomitant meniscal allograft transplantation and autologous chondrocyte implantation: minimum 2-year follow-up. Am J Sports Med 35:1459–1466
Gomoll AH, Kang RW, Chen AL, Cole BJ (2009) Triad of cartilage restoration for unicompartmental arthritis treatment in young patients: meniscus allograft transplantation, cartilage repair and osteotomy. J Knee Surg 22:137–141
Gonzalez-Lucena G, Gelber PE, Pelfort X, Tey M, Monllau JC (2010) Meniscal allograft transplantation without bone blocks: a 5- to 8-year follow-up of 33 patients. Arthroscopy 26:1633–1640
Graf KW Jr, Sekiya JK, Wojtys EM (2004) Long-term results after combined medial meniscal allograft transplantation and anterior cruciate ligament reconstruction: minimum 8.5-year follow-up study. Arthroscopy 20:129–140
Harris JD, Cavo M, Brophy R, Siston R, Flanigan D (2011) Biological knee reconstruction: a systematic review of combined meniscal allograft transplantation and cartilage repair on restoration. Arthroscopy 27:409–418
Hergan D, Thut D, Sherman O, Day MS (2011) Meniscal allograft transplantation. Arthroscopy 27:101–112
Hommen JP, Applegate GR, Del Pizzo W (2007) Meniscus allograft transplantation: ten-year results of cryopreserved allografts. Arthroscopy 23:388–393
Huang A, Hull ML, Howell SM (2003) The level of compressive load affects conclusions from statistical analyses to determine whether a lateral meniscal autograft restores tibial contact pressure to normal: a study in human cadaveric knees. J Orthop Res 21:459–464
Kelly BT, Potter HG, Deng X, Pearle AD, Turner AS, Warren RF, Rodeo SA (2006) Meniscal allograft transplantation in the sheep knee. Evaluation of chondroprotective effects. Am J Sports Med 34:1464–1477
Kim JG, Lee YS, Bae TS, Ha JK, Lee DH, Kim YJ, Ra HJ (2013) Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc 21:2121–2125
Marcacci M, Marcheggiani Muccioli GM, Grassi A, Ricci M, Tsapralis K, Nanni G, Bonanzinga T, Zaffagnini S (2014) Arthroscopic meniscus allograft transplantation in male professional soccer players: a 36-month follow-up study. Am J Sports Med 42:382–388
Matava MJ (2007) Meniscal allograft transplantation. A systematic review. Clin Orthop Relat Res 455:142–157
McDermott ID, Lie DT, Edwards A, Bull AM, Amis AA (2008) The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc 16:553–560
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 18:264–269
Mora G, Alvarez E, Ripalda P, Forriol F (2003) Articular cartilage degeneration after frozen meniscus and Achilles tendon allograft transplantation: experimental study in sheep. Arthroscopy 19:833–841
Noyes FR, Barber-Westin SD, Rankin M (2004) Meniscal transplantation in symptomatic patients less than fifty years old. J Bone Joint Surg Am 86:1392–1404
Paletta GA, Manning T, Snell E, Parker R, Bergfeld J (1997) The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med 25:692–698
Rath E, Richmond JC, Yassir W, Albright JD, Gundogan F (2001) Meniscal allograft transplantation. Two- to eight-year results. Am J Sports Med 29:410–414
Rijk PC, Tigchelaar-Gutter W, Bernoski FP, Van Noorden CJ (2004) Histologic changes in articular cartilage after medial meniscus replacement in rabbits. Arthroscopy 20:911–917
Rijk PC, Van Eck-Smit BL, Van Noorden CJ (2003) Scintigraphic assessment of rabbit knee joints after meniscal allograft transplantation. Arthroscopy 19:506–510
Rodkey WG (2000) Basic biology of the meniscus and response to injury. Instr Course Lect 49:189–193
Rue JP, Yanke AB, Busam ML, McNickle AG, Cole BJ (2008) Prospective evaluation of concurrent meniscus transplantation and articular cartilage repair: minimum 2-year follow-up. Am J Sports Med 36:1770–1778
Rueff D, Nyland J, Kocabey Y, Chang HC, Caborn DN (2006) Self-reported patient outcomes at a minimum of 5 years after allograft anterior cruciate ligament reconstruction with or without medial meniscus transplantation: an age-, sex-, and activity level matched comparison in patients aged approximately 50 years. Arthroscopy 22:1053–1062
Ryu RK, Dunbar VWH, Morse GG (2002) Meniscal allograft replacement: a 1-year to 6-year experience. Arthroscopy 18:989–994
Saltzman BM, Bajaj S, Salata M, Daley EL, Strauss E, Verma N, Cole BJ (2012) Prospective long-term evaluation of meniscal allograft transplantation procedure: a minimum of 7-year follow-up. J Knee Surg 25:165–176
Samitier G, Alentorn-Geli E, Taylor DC, Rill B, Lock T, Moutzouros V, Kolowich P (2014) Meniscal allograft transplantation. Part 1: systematic review of graft biology, graft shrinkage, graft extrusion, graft sizing, and graft fixation. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3334-5
Seedhom BB, Hargreaves DJ (1979) Transmission of load in the knee joint with special reference to the role of the menisci: part II: experimental results, discussions, and conclusions. Eng Med Biol 8:220–228
Sekiya JK, Griffin JR, Irrgang JJ, Fu FH, Harner CD (2003) Clinical outcomes after combined meniscal allograft transplantation and anterior cruciate ligament reconstruction. Am J Sports Med 31:896–906
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Szomor ZL, Martin TE, Bonar F, Murrell GA (2000) The protective effects of meniscal transplantation on cartilage. An experimental study in sheep. J Bone Joint Surg Am 82:80–88
van der Wal RJ, Thomassen BJ, van Arkel ER (2009) Long-term clinical outcome of open meniscal allograft transplantation. Am J Sports Med 37:2134–2139
Verbruggen D, Verschueren T, Tampere T, Almqvist K, Victor J, Verdonk R, Verdonk P (2014) Revision of meniscal transplants: long-term clinical follow-up. Knee Surg Sports Traumatol Arthrosc 22:351–356
Verdonk PC, Verstraete KL, Almqvist KF, Cuyper K, Veys EM, Verbruggen G, Verdonk R (2006) Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc 14:694–706
Verdonk R, Volpi P, Verdonk P, van der Bracht H, van Laer M, Almqvist KF, Vander Eecke S, Prospero E, Quaglia A (2013) Indications and limits of meniscal allografts. Injury 44:S21–S27
von Lewinski G, Milachowski KA, Weismeier K, Kohn D, Wirth CJ (2007) Twenty-year results of combined meniscal allograft transplantation, anterior cruciate ligament reconstruction and advancement of the medial collateral ligament. Knee Surg Sports Traumatol Arthrosc 15:1072–1082
von Lewinski G, Pressel T, Hurschler C, Witte F (2006) The influence of intraoperative pretensioning on the chondroprotective effect of meniscal transplants. Am J Sports Med 34:397–406
Vundelinckx B, Bellemans J, Vanlauwe J (2010) Arthroscopically assisted meniscal allograft transplantation in the knee. A medium-term subjective, clinical, and radiographical outcome evaluation. Am J Sports Med 38:2240–2247
Wirth CJ, Peters G, Milachowski KA, Weismeier K, Kohn D (2002) Long-term results of meniscal allograft transplantation. Am J Sports Med 30:174–181
Author information
Authors and Affiliations
Corresponding author
Additional information
Gonzalo Samitier and Eduard Alentorn-Geli have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Samitier, G., Alentorn-Geli, E., Taylor, D.C. et al. Meniscal allograft transplantation. Part 2: systematic review of transplant timing, outcomes, return to competition, associated procedures, and prevention of osteoarthritis. Knee Surg Sports Traumatol Arthrosc 23, 323–333 (2015). https://doi.org/10.1007/s00167-014-3344-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3344-3