Abstract
Purpose
The treatment of meniscal tears has changed since the early 1980s. Meniscus transplantation emerged as a treatment option during that period. This study aims to present the long-term results of the first lyophilised meniscus allograft transplants in Turkey.
Methods
Between 1990 and 1992, four transplants of the medial meniscus combined with anterior cruciate ligament (ACL) reconstruction were performed on patients with a history of medial meniscectomy and anterior knee instability at our institution. For all patients who underwent meniscus lyophilised allograft transplantation and revision ACL reconstruction, clinical outcomes were evaluated over a mean period of 19 years of postoperative follow-up by clinical assessment, Tegner score, Lysholm score, Knee Society Score, radiography and magnetic resonance imaging (MRI).
Results
The median value of Tegner score was 3 before index surgery and 2.5 at year 19 postoperatively. The median value of Lysholm score was 60.5 before index surgery and 62.5 at year 19. All of the patients had Outerbridge grade IV osteoarthritis by X-ray examination at year 19.
Conclusion
Successful meniscus transplantation depends on many factors. This study examines the effect of allografts on these factors and describes experiences with lyophilised allografts in four male patients.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of the meniscus was described by Fairbank [5]. Many experimental and clinical studies have shown that the absence of the meniscus results in osteoarthritis and joint deterioration in the long term; as a result, meniscus transplantation is considered following total meniscectomy [10, 16]. Furthermore, the meniscus is an important secondary stabiliser against anterior and lateral tibial translations and should be preserved or replaced in the setting of ACL reconstruction, for the restoration of optimal knee kinematics and function [21, 23]. The first clinical meniscal allograft transplantation in humans was performed by Milachowski et al. [11] in 1984.
Indications for meniscal transplantation include patient age of 40 years or less and a totally absent meniscus [4, 10, 13, 16, 20, 26]. Patients with a totally absent meniscus present with localised pain in the affected area during daily activities and sports and have Outerbridge grade I or II articular changes but normal alignment [20]. Considering these findings, and as a result of the promising short-term results published in the late 1980s and early 1990s, meniscus transplantation was initiated in Turkey at approximately the same time that it was started worldwide [3]. Long-term outcomes of meniscal transplantation are affected by many factors, especially the type of allograft. This study reviews the effect of allograft type with examples of long-term outcomes in four cases.
Materials and methods
Four male patients who underwent the first meniscus lyophilised allograft transplantations in Turkey between 1990 and 1992 were included in the study. The average age at index surgery was 24.5 ± 3.1 years (range: 20–27 years). Each patient had previously undergone an open total meniscectomy (mean 4.2 ± 1.5 years prior), and anterior cruciate ligament (ACL) reconstruction proved to be unsuccessful. In all patients, injury to the knee occurred while participating in a sporting activity. Preoperatively, the main complaints were the following: knee pain, swelling and instability after total meniscectomy and ACL reconstruction. Two patients had undergone intra-articular iliotibial band transfer for ACL reconstruction and total meniscectomy before index surgery [7]. One patient had surgery for ACL reconstruction using synthetic ligament and total meniscectomy, and another patient had undergone total meniscectomy and ACL reconstruction with a bone-patellar tendon-bone autograft.
Clinically, all patients had ACL deficiency and were pivot-shift and Lachmann positive before index surgery. Each patient was evaluated with non-weight-bearing lateral and anteroposterior (AP) radiographs and lower extremity weight-bearing radiographs. There was no evidence of osteoarthritis or misalignment at the time of transplantation. Surgical indications were progressive instability and functional deficiency. Patients were treated concomitantly with medial lyophilised meniscal allograft transplantation and revision of ACL reconstruction. Whole medial meniscus allografts were implanted in three right knees and one left knee. Three patients underwent reconstruction with bone-patellar tendon-bone allograft, and one patient underwent reconstruction with bone-patellar tendon-bone autograft during index surgery. Patients were evaluated with KT-1000, Lysholm Score and Tegner Activity Scale at approximately year 1, year 2 and year 19. In the evaluation of the data, descriptive statistic and Friedman test on the SSPS 13.0 statistical package programme was used.
Surgical technique
All surgical procedures were performed by the senior author (Binnet, MS.). Plain radiographs were used to determine allograft size. Meniscus width was determined by AP radiography, and meniscus length was determined by lateral radiography. Donors were matched with recipients according to skeletal size, as measured by standard AP radiography of the distal femur, and matching to within 5% was achieved in every case.
From 1990 to 1992, lyophilised allografts sterilised with ethylene oxide were obtained from the Florida Tissue Bank (University of Florida College of Medicine, Gainesville, Fl, USA). General anaesthesia and tourniquets were used in all patients. Arthroscopy was not used during index surgery, and all patients underwent open surgery. Joints were visualised through medial parapatellar arthrotomy. The posterior portion of the allograft was attached to the remnant wall of the original meniscus. Localisation of the anterior meniscus insertion site was slightly medial to midline and in front of the ACL’s insertion. Localisation of the posterior meniscus insertion side was slightly medial to midline and in front of the posterior cruciate ligament (PCL) insertion. Multiple 0 and 2-0 non-absorbable sutures were used in a vertical fashion to attach the allograft to the rim. In-side-out and out-side-in techniques were combined for the fixation of allografts, and bone block fixations were not used.
After ensuring sufficient stabilisation in the front and back horns, ACL revision was performed on all patients using the transtibial approach (9,11). Allograft bone-patellar tendon-bone was used in three patients, and autograft bone-patellar tendon-bone was used in one patient. There were no complications during surgery.
A restrictive rehabilitation programme was initiated. Patients remained non-weight bearing for 6 weeks after surgery. Flexion was not permitted for the first 2 weeks. We used a plaster cast during that time. At week four, ranges of motion between 00 and 900 were observed in all patients. Jogging was allowed 4 months later, and sporting activities, such as recreational soccer, were permitted 1 year later.
Results
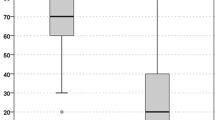
The mean follow-up duration was 19 ± 0.8 years (range: 18–20 years). The median value of Tegner score was 3 before index surgery, with a median value of 4 at year two postoperatively and a median value of 2.5 at year 19 postoperatively. The median value of Lysholm score was 60.5 before index surgery, with a median value of 74 at year two and a median value of 62.5 at year 19. The median value of Knee Society Score was 60.5 before index surgery, with a median of 74 at year two and a median of 59.5 at year 19 postoperatively. No instability symptoms were observed during clinical examinations and KT-1000 assessments.
Two patients underwent a second arthroscopy due to swelling, medial compartment pain and mechanical symptoms exacerbated by physical activity. One of them had surgery twice following the index surgery, at years 5 and 18 of follow-up. Five years later, the allograft was visible and functional (Fig. 1a). Eighteen years later, we did not see the allograft (Fig. 1b). The other patient also underwent a second arthroscopy, but at year 12 of follow-up (Fig. 2). In both patients, meniscal transplants were reduced in size early during follow-up and also at the time of the second arthroscopy. As a result, the function of the meniscus was not preserved. At the same time, advanced degenerative arthritis was observed when the interference screws were removed.
Discussion
The most important finding of the present study was the effect of allograft preparation steps on outcomes. There are many causes for the development of degenerative arthritis. Loss of meniscal tissue can lead to lack of protection of the articular cartilage of the femoral and tibial condyles and result in osteoarthritis. In the case of large meniscal defects, replacing the defects with tissue can be accomplished successfully. Currently, there are many procedures for replacing these defects, including the use of meniscal allografts and scaffolds.
The prevalence of meniscus tears seems to be high in ACL-deficient patients [12]. For meniscus transplantation, ligament stabilisation is recommended either before or concomitantly during meniscus transplantation in an unstable knee because meniscus repairs result in superior healing in stable knees [14, 15, 23]. Spang et al. [23] evaluated the effect of meniscectomy and meniscal allograft transplants on anterior cruciate ligament and knee biomechanics in 10 human cadaveric knees. They showed that meniscectomy produced a significant increase in tibial displacement relative to the femur, and meniscal allograft transplantation restored displacement values to normal. Instability and mechanical meniscus deficiencies are among the main causes of degenerative arthritis [10, 15, 16, 23].
Allograft preparation steps affect the results of allograft transplantation in short- and long-term follow-up. The four main methods of preserving meniscal allografts are as follows: fresh, fresh-frozen (deep-frozen), lyophilised and cryopreserved [10, 13, 14, 16, 20, 24]. Due to transportation problems, it is impossible to provide fresh grafts in countries such as Turkey, which have no tissue banks. Fresh-frozen allografts are easier to store, but during the freezing process, donor cells are destroyed, resulting in denatured histocompatibility antigens, which may in turn decrease immunogenicity [14]. Cryopreserved allografts maintain a cell viability of 10–40% [2, 20, 24]. Cryopreservation allows prolonged allograft storage [1, 24], but this technique is more expensive. Lyophilised allografts result in collagen scaffold destruction as well as antigens and enzymes. The allografts are then thawed and rehydrated before transplantation. Although this method allows for indefinite storage, it also produces alterations in biomechanical properties and size of the allografts.
The sterilisation step of allografts is also important. Sterilisation involves two different processes as follows: gamma irradiation and ethylene oxide. Ethylene oxide produces a metabolic by-product, ethylene chlorohydrin, which results in a significant cell response and synovial inflammation [1, 2, 8, 9, 18, 24]. Gamma irradiation with at least 3.0 Mrad is necessary to inactivate HIV-1 DNA as determined by testing with PCR [9, 15, 24]. As a result, when irradiation exceeds 3 Mrad, graft sterilisation is improved, but this is at the risk of compromising the material properties of the graft [9].
Many factors can affect the progression of degenerative changes in the knee following meniscal transplantation in the long term, such as initial cartilage damage, surgical indications and technique, preservation methods of the allograft, sterilisation methods of the allograft and postoperative rehabilitation [6, 17, 22, 27]. However, the authors of this study believe that the most important cause of degeneration observed in these young patients (average age 42.5 ± 2.4; range 39–44 years) is the shrinkage of the meniscal allografts because of lyophilisation techniques. Wirth et al. [28] examined the results of a lyophilised meniscal allograft procedure performed on 17 cases and a deep-frozen meniscal allograft performed on six cases. The follow-up period was 14 years, and they showed that patients with deep-frozen meniscal transplants generally had better clinical outcomes than patients receiving lyophilised meniscal transplants.
One of the important findings of this study is that the clinical symptoms of these patients were limited, even though there were significant radiological changes observed in all patients. ACL reconstruction results in the most significant improvements in stability, which may explain the low level of clinical complaints. Clinical improvement in four patients over a period of 19 years indicates that transplantation was successful. However, sterilisation methods and allograft choices remain important issues because they affect the clinical results of the allograft, and their future improvement may provide better results [6, 27].
There were several limitations to this study. First, the sample size was very small (n = 4). Second, there was no control group. Currently, allografts were performed according to new developments in meniscus transplantation surgery; lyophilised allografts had been discarded.
Conclusion
Although meniscal transplantation can prevent joint degeneration in the short term, whether meniscal grafts can delay or prevent the progression of degenerative changes in the long term remains unclear [15, 19, 23, 25]. Nevertheless, experimental studies that have compared fresh cryopreserved and fresh-frozen meniscal allografts have revealed no clear differences in biological incorporation of the grafts or in clinical outcomes [24].
References
Arnoczky SP, McDewitt CA, Schmidt MB, Mow VC, Warren RF (1988) The effect of cryopreservation on canine menisci: a biomechanical, morphologic and biomechanical evaluation. J Orthop Res 6:1–12
Arnoczky SP, Warren RF, McDewitt CA (1990) Meniscal replacement using a cryopreserved allograft an experimental study in dog. Clin Orthop Relat Res 252:121–128
Binnet MS (1992) Allograft meniscus and ACL transplantation. Acta Orthop Traumatol Turc 26:300–306
Chang CH, Teh KL, Leong KL, Mak SL, Karim SA (2008) Clinical evaluation of arthroscopic-assisted allograft meniscal transplantation. Ann Acad Med Singapore 37:266–272
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Jt Surg Br 30:664–670
Indelli PF, Dillingham MF, Fanton GS, Schurman DJ (2004) Anterior cruciate ligament reconstruction using cryopreserved allografts. Clin Orthop Relat Res 420:266–275
Insall J, Joseph DM, Aglietti P, Campbell RD (1981) Bone-block iliotibial-band transfer for anterior cruciate insufficiency. J Bone Jt Surg Am 63:560–568
Jackson DW, Windler GE, Simon TM (1990) Intraarticuler reaction associated with the use of freeze-dried ethylene oxide sterilized bone-patellar tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med 18:1–10
Johnson DL, Bealle D (1999) Meniscal allograft transplantation. Clin Sports Med 18:93–108
Lubowitz JH, Verdonk PCM, Reid JB, Verdonk R (2007) Meniscus allograft transplantation: a current concepts review. Knee Surg Sports Traumatol Arthrosc 15:476–492
Milachowski KA, Weismeier K, Wirth CJ (1989) Homologous meniscus transplantation: experimental and clinical results. Int Orthop 13:1–11
Naranje S, Mittal R, Nag H, Sharma R (2008) Arthroscopic and magnetic resonance imaging evaluation of meniscus lesions in the chronic anterior curiciate ligament deficient knee. Arthroscopy 24:1045–1051
Noyes FR, Barber-Westin SD (2005) Meniscus transplantation: indications, techniques, clinical outcomes. AAOS Instr Course Lect 54:341–353
Packer JD, Rodeo SA (2009) Meniscal allograft transplantation. Clin Sports Med 28:259–283
Perning J, Verdonk P, Selmi TAS, Massin P, Neyret P (2010) Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med 38:1094–1102
Peters G, Wirth CJ (2003) The current state of meniscal allograft transplantion and replacement. Knee 10:19–31
Rijk PC (2004) Meniscal allograft transplantation part I background, results, graft selection, and preservation, and surgical considerations. Arthroscopy 20:728–743
Rodeo SA (2001) Current concepts: meniscal allografts: where do we stand? Am J Sports Med 29:246–261
Rue JPH, Yanke AB, Busam ML, McNickle AG, Cole BJ (2008) Prospective evaluation of concurrent meniscus transplantation and articular cartilage repair minimum 2-year follow-up. Am J Sports Med 36:1770–1778
Sekiya JK, Ellingson CI (2006) Meniscal allograft transplantation. J Am Acad Orthop Surg 14:164–174
Seon KJ, Gadikota HR, Kozanek M, Luke SO, Gill TJ, Guoan L (2009) The effect of anterior cruciate ligament reconstruction on kinematics of the knee with combined anterior curicate ligament injury and subtotal medial meniscectomy: an in vitro robotic investigation. Arthroscopy 25:123–130
Sohn DH, Toth AP (2008) Meniscus transplantation: current concept. J Knee Surg 21:163–172
Spang JT, Dang ABC, Mazzocca A, Rincon L, Obopilwe E, Beynnon B, Arciero RA (2010) The effect of medial meniscectomy and meniscal allograft transplantation on knee and anterior cruciate ligament biomechanics. Arthroscopy 26:192–201
Tom JA, Rodeo SA (2002) Soft tissue allografts for knee reconstruction in sports medicine. Clin Orthop Relat Res 402:135–156
Verdonk P, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R (2005) Transplantation of viable meniscal allograft. J Bone Jt Surg 87:715–724
Verdonk R, Almqvist KF, Wouter H, Verdonk PC (2007) Meniscal allografts: indications and outcomes. Sports Med Arthrosc Rev 15:121–125
Wang Y, Yu J, Yu CL, Ao Y, Xie X, Jiang D, Zhang J (2009) An anatomical and histological study of human meniscal horn bony insertions and peri-meniscal attachments as a basis for meniscal transplantation. Chin Med J 122:536–540
Wirth CJ, Peters G, Milachowski KA, Weismeier KG, Kohn D (2002) Long-term results of meniscal allograft transplantation. Am J Sports Med 30:174–181
Acknowledgments
The authors wish to thank R. Verdonk for help with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Binnet, M.S., Akan, B. & Kaya, A. Lyophilised medial meniscus transplantations in ACL-deficient knees: a 19-year follow-up. Knee Surg Sports Traumatol Arthrosc 20, 109–113 (2012). https://doi.org/10.1007/s00167-011-1556-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1556-3