Abstract
Introduction
Clinical assessments do not accurately reflect the status of meniscal transplants and cannot evaluate the graft condition itself and joint preservation effects of meniscal allograft transplantation correctly. The purpose of this review was to assess the need and to ascertain the indication and the role of second-look arthroscopy for objective evaluation after MAT.
Materials and methods
We performed a literature search to identify all published clinical studies on MAT with the following medical subject heading (MeSH) terms: “meniscus,” “meniscal transplant,” “transplantation and allograft,” “meniscal and transplant.” Include in the review are studies with at least 6 months clinical, radiological, and/or histological follow-up in human subjects. Evaluation method of MAT was reviewed with an aim to describe the frequency of second-look arthroscopy, its feasibility, patient compliance, purposes, and results.
Results
We identified 15 clinical studies that satisfied our inclusion and exclusion criteria. Only two studies always performed second-look arthroscopies. Most of the second-look arthroscopy was conducted mainly for the objective evaluation of meniscal allograft transplantation but, in several studies, arthroscopy was performed to treatment of other knee problem.
Conclusions
Although second-look arthroscopy has inevitably ethical issues, especially for asymptomatic and well-functioning knees, in this review, it could be a more dependable method available to detect meniscal healing if performed for certain indications such as a symptomatic patient with a magnetic resonance image indicating abnormalities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the late 1980s, Milachowski et al. [1] reported on the experimental and short-term clinical results of meniscus allograft transplantation (MAT). Since then, numerous reports on MAT have been published. Most of the reported results have demonstrated a significant improvement in function and pain relief after MAT [2–4]. However, there have been limitations in evaluating the status of MAT, such as meniscal extrusion and shrinkage. In addition, because of a lack of consensus regarding many variables, such as preservation techniques, associated procedures, graft fixation methods, and follow-up duration, effectively comparing the results of MAT remains an area of concern. So far, with respect to evaluation methods, in most studies, the MAT evaluation only involved clinical parameters [5, 6] such as the Lysholm score, International Knee Documentation Committee score, and visual analog scale. However, few studies have used objective methods to evaluate, such as MRI or second-look arthroscopy [4, 7, 8].
Clinical assessments do not accurately reflect the status of meniscal transplants and cannot correctly evaluate the graft condition itself or the joint preservation effects of MAT. In addition, it is difficult to compare outcomes among studies. Accordingly, objective methods such as plain radiographs, ultrasound, MRI, or second-look arthroscopy have been suggested [8]. MRI has been most commonly used as a relatively accurate and reliable evaluation method for MAT.
Although second-look arthroscopy is an invasive procedure, it has several advantages for evaluating the results of MAT. It could provide the dynamic status of the allograft by allowing the performance of range of motion during arthroscopy, and it could show the actual graft appearance, such as shrinkage, capsular healing, allograft detachment, tears, and extrusion.
The purpose of this review was to assess the need and to ascertain the indication and the role of second-look arthroscopy for objective evaluation after MAT.
The hypothesis of our literature review was that there would be no definite indication for second-look arthroscopy after MAT.
Materials and methods
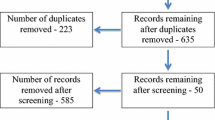
In January 2014, we performed a literature search using Embase and PubMed to identify all published clinical studies on MAT with the following medical subject heading (MeSH) terms: “meniscus,” “meniscal transplant,” and “transplantation and allograft.” We found that the combination of “meniscal and transplant” yielded the largest number of results. We meticulously reviewed every single abstract. Our inclusion criteria were as follows: studies involving human subjects who had more than 6 months of follow-up after MAT including clinical, radiological, arthroscopic, histological examinations, or any combination of these, as well as articles written in English. Exclusion criteria included duplicate data of patients reviewed at multiple intervals or from different perspectives; a mean follow-up of less than 6 months; case reports; and a MAT assessment with clinical scores, MRI, and other subjective methods. All inclusion and exclusion criteria were defined before the literature search. The initial search identified 473 citations. Of these 473 studies, 126 were excluded because of duplication. Then, 236 were excluded because they were not directly related to MAT. After exclusion, 15 papers were reviewed to assess the role of second-look arthroscopies after MAT (Fig. 1). The MAT evaluation method was reviewed with an aim to describe the frequency of second-look arthroscopy, as well as its feasibility, patient compliance, purposes, and results. The frequency of performing second-look arthroscopy was recorded for each study.
Results
For this review, 15 studies [4, 6, 9–21] reported their observations from second-look arthroscopies (Tables 1, 2). However, there was no mention of clear recommendations regarding “when second-look arthroscopy should be performed” and “why second-look arthroscopy should be performed.” All studies were performed using a clinical scoring system to allow for subjective evaluation; however, the type of scoring system was different in the studies.
In all studies, MAT was performed in 541 patients who were under the age of 60 years (15–57 years) with disabling compartmental osteoarthritis after a meniscectomy. It was difficult to determine the average time interval between MAT and second-look arthroscopy because several studies did not indicate these details, and their range of duration was wide. In many studies, second-look arthroscopy was performed an average of 12 months (minimum) after MAT [9, 11–13, 21].
There were two studies in which second-look arthroscopy was performed alone, without any tools for the objective evaluation of MAT [10, 20]. In all the other studies, second-look arthroscopy was performed along with MRI or other radiographic studies. Garrett [10] subjectively evaluated the symptoms only and performed second-look arthroscopy alone as an objective evaluation tool for symptomatic patients. Veltri et al. [20] also objectively evaluated meniscal allografts using second-look arthroscopy only for patients with symptoms.
Based on a literature review, only two studies always performed second-look arthroscopies after MAT [9, 19]. The rest of the authors performed second-look arthroscopies, on average, for approximately 46 % of the patients undergoing MAT (except for a study by Verdonk et al. [6] that did not mention the number of patients who underwent second-look arthroscopy). van Arkel et al. [19] performed an arthroscopic evaluation for all 16 consecutive patients who underwent MAT. Voluntary participation and informed consent were obtained for all patients. There were 13 men and three women, with an average age of 40 years (range 30–54 years). The medial meniscus was transplanted in three patients, while the lateral meniscus was transplanted in 10 patients and both menisci were transplanted in three patients. Upon examination, 15 allografts were completely healed to the capsule, while three were partially detached and one was totally detached. According to the author’s failure criteria, four patients were considered an arthroscopic failure. They concluded that the arthroscopic results correlated better with the clinical outcomes than MRI. Bhosale et al. [9] reported on eight patients who underwent MAT with autologous chondrocyte implantation (ACI). Second-look arthroscopy was performed as a routine procedure for the objective evaluation of all patients, and a biopsy of the new tissue was obtained. Seven patients who had second-look arthroscopy demonstrated a stable meniscal allograft with healed peripheral margins. One patient had meniscal thinning, but with no evidence of rejection.
Second-look arthroscopy was conducted mainly for the objective evaluation of MAT, but in several studies, arthroscopy was performed to treat other knee problems [14, 15] and to assess failure cases [6, 18]. Verdonk et al. [6] evaluated 100 meniscal transplantations that were performed for 96 patients. At the time of the MAT, their mean age was 35 ± 6.7 years (range 16–50 years). Thirty-nine medial allografts and 61 lateral allografts were implanted into 70 men and 26 women. Second-look arthroscopy was performed for failure cases or evaluation purposes. During second-look arthroscopy, there were a total of 21 failed allografts: eight demonstrated severe degeneration, 12 demonstrated only minor degenerative changes, and one had a normal meniscal allograft. van Arkel and de Boer [18] also performed second-look arthroscopy only for failure cases with persistent pain, a poor Lysholm score, or an unsuccessful knee assessment scoring system (KASS) result. Some studies described that meniscal biopsies were obtained during second-look arthroscopies to document the histological features of the meniscal allograft [9, 13, 15, 17].
Two studies indicated that second-look arthroscopies were performed more than once to assess the meniscal allograft objectively over time and to treat other knee problems [17, 21]. Wirth et al. [21] reported on 23 medial meniscus transplantations combined with an anterior cruciate ligament reconstruction. The first follow-up second-look arthroscopy was performed an average of 3.8 years after MAT for 19 patients. Complete healing was confirmed in 17 patients. Just two patients had incomplete healing or allograft detachment. Most patients refused further arthroscopic evaluation at a long-term follow-up; only two patients had a second arthroscopy 14 years after MAT. van Arkel and de Boer [17] performed post-MAT arthroscopy in 12 patients. Seven had one arthroscopy, while four had two, and one had three arthroscopies at different time intervals; these arthroscopies occurred 6–40 months after MAT. The first arthroscopy was performed for investigational purposes. Then, second and third arthroscopy was performed to confirm the meniscal status after a previous arthroscopy.
Discussion
With improved knowledge regarding the need to preserve as much meniscal tissue as possible, meniscal repair is now a preferred treatment over meniscectomy; however, a meniscectomy may be inevitable depending upon the severity of damage [2, 3, 22–24]. In such instances, MAT is regarded as a promising approach [1, 4] for the reconstruction of meniscal biomechanical properties in knees with meniscal deficits and is aided by advanced arthroscopic equipment, instruments, and techniques [25, 26].
As the benefits of MAT, including pain relief and functional improvement, have been demonstrated, many methods have been performed to evaluate the clinical outcomes of MAT. However, any proper guidelines remain unclear regarding second-look arthroscopy, as well as the interpretation of the outcomes.
We reviewed 15 articles regarding second-look arthroscopy to evaluate post-MAT outcomes. In most studies, second-look arthroscopy was performed for objective evaluation, without any consistent standards. In two studies [10, 20], second-look arthroscopy was conducted based on clinical symptoms only.
In our review, second-look arthroscopies were usually performed with a mean of 48.8 % per study group. This result is because of the invasiveness of arthroscopy. van Arkel et al. [19] and Bhosale et al. [9] always performed second-look arthroscopy after MAT. Although it is difficult to quantify accurately, second-look arthroscopy was mostly performed for the objective evaluation of MAT, and the minimum average duration was greater than 12 months from MAT to second-look arthroscopy.
In a review of previous studies, Rodeo [27] reported that more than 90 % of MAT was accompanied by other procedures. In our review, MAT was mostly performed with a concomitant procedure such as a ligament reconstruction or an articular cartilage treatment. In such cases, however, it is difficult to compare their MAT results to other studies.
In addition, a variable scoring system and MRI were used as evaluation tools, and the criteria of success and failure were different. Thus, a direct comparison is difficult.
Clinical scoring systems are simple and easy evaluation tools for MAT. However, for MAT, success cannot be measured with a clinical scoring system only. Clinical scoring systems are based on subjective evaluation, and there is no specific scoring system for MAT. Rath et al. [14] evaluated 10 of their 18 MAT patients with arthroscopy and found eight allograft tears. However, the majority of patients experienced a significant improvement in their SF-36 score.
Thus, a more accurate and objective evaluation method for MAT is necessary.
Several authors performed an MRI evaluation during MAT follow-up visits [3, 19, 28] and believe that MRI could be a gold standard to evaluate meniscal allograft status [29]. It has been demonstrated that it is worthwhile to assess the graft and joint preservation effect thoroughly with high-level evidence. However, the role of MRI in the post-operative evaluation of MAT is unclear, and no significant correlation was reported between MRI and clinical outcomes in a recent study [30]. There are several shortcomings with the use of MRI for objective evaluation. First, MRI has variable signal intensities and artifacts that could affect the interpretation of the results. Increased signal intensities were mostly considered attributable to scar response, revascularization, or host-cell repopulation. MRI was unable to distinguish the intensity of meniscal tears [19]. Another drawback is that intra-substance degeneration could be seen with MRI. Intra-substance degeneration could be seen in the normal menisci of older patients, so it could be difficult to distinguish from normal findings. Finally, MRI could not be employed for the dynamic evaluation of meniscal allografts utilizing range of motion [21, 31, 32]. Therefore, this study intended to report the need and role of second-look arthroscopy as an objective evaluation method after MAT.
As previously mentioned, even though MRI and clinical scoring systems have been extensively used to evaluate MAT, more detailed and objective methods for the investigation and description of meniscus allografts, as well as the adjacent cartilage, are necessary.
Second-look arthroscopy is the most accurate objective evaluation method. It can provide the dynamic status of the meniscus, and it is possible to analyze the histological status through biopsy. Additionally, arthroscopy shows the actual status of the allograft, as well as the status of the other intraarticular structures. van Arkel et al. [19] evaluated meniscal allografts with MRI and second-look arthroscopy and concluded that the arthroscopic results correlated better with the clinical results than MRI. In addition, they reported that sensitivity, positive predictive value, negative predictive value, and the likelihood ratio for a positive test were better for arthroscopy than MRI. Moreover, during second-look arthroscopy, the healing of the meniscal transplant to the joint capsule could be inspected and tested directly with a probe (Fig. 2).
MRI and second-look arthroscopic findings of a 38-year-old patient who received a lateral meniscal allograft 2 years ago. a, b The MRI scan indicates extrusion of the lateral meniscus allograft and a high signal intensity (white circle) as demonstrated by a gap between the graft and capsule. c By testing with a probe, separation of the allograft and capsule was detected, indicating that the peripheral aspect of the meniscus was not healed. d The meniscal tear and separation were repaired with sutures during the same visit
However, it was not always feasible because some patients without disabling discomfort were unwilling to undergo invasive and expensive second-look arthroscopy. In this case, an invasive arthroscopic procedure could cause ethical issues. Additionally, it could not be used as a weight-bearing evaluation method for an allograft, and conflicting bias concerning interpretation of arthroscopic observations exists [31].
Therefore, it is important to determine whether second-look arthroscopy is necessary considering patients’ symptoms and MRI findings (Fig. 3). An MRI scan should be performed as a first-line evaluation; however, for a symptomatic patient with positive MRI findings, go for second-look arthroscopy. Similarly, for symptomatic patients with negative MRI findings, the role of second-look arthroscopy may be valuable for further evaluation. However, if you are in doubt, go for second-look arthroscopy. For asymptomatic patients with positive MRI findings, the role of second-look arthroscopy is questionable.
A potential limitation of this review includes the heterogeneity of studies that we reviewed. All the studies had their own criteria and purpose, as well as definitions of failure of MAT on second-look arthroscopy, frequency of performing second-look arthroscopy, follow-up period, and number of patients.
Another limitation of this review is that second-look arthroscopy has not yet been definitively established as an evaluation method for MAT.
Finally, not all studies provided the data necessary for our review.
Conclusion
In conclusion, if patients have pain or other problems on knee following MAT, the objective evaluation such as MRI or second-look arthroscopy are necessary. However, until now, many methods have been performed to evaluate the only clinical outcomes of MAT, and second-look arthroscopy was performed without any proper guidelines. In this review, there was no clear mention of indication for second-look arthroscopy after MAT. Thus, we assessed the need and role of second-look arthroscopy for objective evaluation after MAT.
Although second-look arthroscopy has inevitably ethical issues, especially for asymptomatic and well-functioning knees, in this review, it could be a more dependable method available to detect meniscal healing if performed for certain indications such as a symptomatic patient with an MRI indicating abnormalities.
References
Milachowski KA, Weismeier K, Wirth CJ (1989) Homologous meniscus transplantation. Experimental and clinical results. Int Orthop 13:1–11
DeHaven KE (1999) Meniscus repair. Am J Sports Med 27:242–250
Kim CW, Kim JM, Lee SH, Kim JH, Huang J, Kim KA, Bin SI (2011) Results of isolated lateral meniscus allograft transplantation: focus on objective evaluations with magnetic resonance imaging. Am J Sports Med 39:1960–1967
Kim JM, Lee BS, Kim KH, Kim KA, Bin SI (2012) Results of meniscus allograft transplantation using bone fixation: 110 cases with objective evaluation. Am J Sports Med 40:1027–1034
LaPrade RF, Wills NJ, Spiridonov SI, Perkinson S (2010) A prospective outcomes study of meniscal allograft transplantation. Am J Sports Med 38:1804–1812
Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R (2005) Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am 87:715–724
Gonzalez-Lucena G, Gelber PE, Pelfort X, Tey M, Monllau JC (2010) Meniscal allograft transplantation without bone blocks: a 5- to 8-year follow-up of 33 patients. Arthroscopy 26:1633–1640
Lee DH, Kim SB, Kim TH, Cha EJ, Bin SI (2010) Midterm outcomes after meniscal allograft transplantation: comparison of cases with extrusion versus without extrusion. Am J Sports Med 38:247–254
Bhosale AM, Myint P, Roberts S, Menage J, Harrison P, Ashton B, Smith T, McCall I, Richardson JB (2007) Combined autologous chondrocyte implantation and allogenic meniscus transplantation: a biological knee replacement. Knee 14:361–368
Garrett JC (1993) Meniscal transplantation: a Review of 43 Cases with 2- to 7-Year Follow-up. Sports Med Arthrosc Rev 1:164–167
Ha JK, Shim JC, Kim DW, Lee YS, Ra HJ, Kim JG (2010) Relationship between meniscal extrusion and various clinical findings after meniscus allograft transplantation. Am J Sports Med 38:2448–2455
Kim JM, Bin SI (2006) Meniscal allograft transplantation after total meniscectomy of torn discoid lateral meniscus. Arthroscopy 22:1344–1350
Potter HG, Rodeo SA, Wickiewicz TL, Warren RF (1996) MR imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology 198:509–514
Rath E, Richmond JC, Yassir W, Albright JD, Gundogan F (2001) Meniscal allograft transplantation. Two- to eight-year results. Am J Sports Med 29:410–414
Rodeo SA, Seneviratne A, Suzuki K, Felker K, Wickiewicz TL, Warren RF (2000) Histological analysis of human meniscal allografts. A preliminary report. J Bone Joint Surg Am 82:1071–1082
Ryu RK, Dunbar VW, Morse GG (2002) Meniscal allograft replacement: a 1-year to 6-year experience. Arthroscopy 18:989–994
van Arkel ER, de Boer HH (1995) Human meniscal transplantation. Preliminary results at 2 to 5-year follow-up. J Bone Joint Surg Br 77:589–595
van Arkel ER, de Boer HH (2002) Survival analysis of human meniscal transplantations. J Bone Joint Surg Br 84:227–231
van Arkel ER, Goei R, de Ploeg I, de Boer HH (2000) Meniscal allografts: evaluation with magnetic resonance imaging and correlation with arthroscopy. Arthroscopy 16:517–521
Veltri DM, Warren RF, Wickiewicz TL, O’Brien SJ (1994) Current status of allograft meniscal transplantation. Clin Orthop Relat Res 303:44–55
Wirth CJ, Peters G, Milachowski KA, Weismeier KG, Kohn D (2002) Long-term results of meniscal allograft transplantation. Am J Sports Med 30:174–181
Alford JW, Lewis P, Kang RW, Cole BJ (2005) Rapid progression of chondral disease in the lateral compartment of the knee following meniscectomy. Arthroscopy 21:1505–1509
Lee SJ, Aadalen KJ, Malaviya P, Lorenz EP, Hayden JK, Farr J, Kang RW, Cole BJ (2006) Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med 34:1334–1344
Raber DA, Friederich NF, Hefti F (1998) Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg Am 80:1579–1586
Chang HC, Teh KL, Leong KL, Mak SL, Karim SA (2008) Clinical evaluation of arthroscopic-assisted allograft meniscal transplantation. Ann Acad Med Singapore 37:266–272
Lee BS, Kim JM, Sohn DW, Bin SI (2013) Review of meniscal allograft transplantation focusing on long-term results and evaluation methods. Knee Surg Relat Res 25:1–6
Rodeo SA (2001) Meniscal allografts—where do we stand? Am J Sports Med 29:246–261
Noyes FR, Barber-Westin SD, Rankin M (2004) Meniscal transplantation in symptomatic patients less than fifty years old. J Bone Joint Surg Am 86:1392–1404
Hergan D, Thut D, Sherman O, Day MS (2011) Meniscal allograft transplantation. Arthroscopy 27:101–112
Verdonk PC, Verstraete KL, Almqvist KF, De Cuyper K, Veys EM, Verbruggen G, Verdonk R (2006) Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc 14:694–706
Miao Y, Yu JK, Ao YF, Zheng ZZ, Gong X, Leung KK (2011) Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med 39:735–742
Miao Y, Yu JK, Zheng ZZ, Yu CL, Ao YF, Gong X, Wang YJ, Jiang D (2009) MRI signal changes in completely healed meniscus confirmed by second-look arthroscopy after meniscal repair with bioabsorbable arrows. Knee Surg Sports Traumatol Arthrosc 17:622–630
Acknowledgement
This paper was supported by KonKuk University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest. None of the authors are affiliated to or have any financial relationship with organizations, which sponsor or conduct research. No benefits or funds were received in support of this study/article.
Rights and permissions
About this article
Cite this article
Oh, KJ., Sobti, A.S., Yoon, JR. et al. Current status of second-look arthroscopy after meniscal allograft transplantation: review of the literature. Arch Orthop Trauma Surg 135, 1411–1418 (2015). https://doi.org/10.1007/s00402-015-2274-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2274-y