Abstract
Purpose
To compare the outcomes between hamstring tendon autograft and tibialis anterior allograft in arthroscopic transtibial single-bundle posterior cruciate ligament (PCL) reconstruction.
Methods
Thirty-seven patients undergoing isolated single-bundle PCL reconstruction were enrolled in this study, and their data were retrospectively analyzed. They were divided into group A [4-strand hamstring tendon autograft (4SHG), n = 18] and group B [2-strand tibialis anterior allograft (2STAG), n = 19] and followed up for 2 years at least. Several parameters including the International Knee Documentation Committee score, Lysholm knee score, Tegner activity rating and knee laxity arthrometer were evaluated, and physical examination was performed preoperatively and postoperatively, and postoperative complications were also observed in all patients. Meanwhile, the postoperative posterior instability was compared between the affected knee and the contra-lateral knee.
Results
Compared with preoperative knee laxity and function, both groups had significant improvement postoperatively (P < 0.01). However, there were no significant differences in knee laxity and function between both groups (n.s.). Compared with contra-lateral knee, the posterior stability was worse in the affected knee (P < 0.01).
Conclusions
The outcomes were similar between 4SHG or 2STAG in PCL reconstruction. Compared with contra-lateral knees, the affected knees have slight residual knee laxity in both groups.
Level of evidence
Retrospective comparative study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical reconstruction for symptomatic chronic posterior cruciate ligament (PCL) lesions has been gradually recommended to improve posterior knee laxity and knee joint function [19]. There are various autografts and allografts that can be used for PCL reconstruction. However, to date, no superior graft has been identified due to a significant lack of comparative studies on the choice of various grafts for PCL reconstruction [15]. Generally, many surgeons prefer allografts including Achilles tendon and tibialis anterior, because these allografts have sufficiently large diameter and long length and cannot lead to donor-site morbidity. However, allograft tissues are not widely available due to the limited source in some areas, and the hospitalization cost is usually expensive [9, 33]. At present, bone-patellar tendon-bone (BPTB) and hamstring tendon were most commonly used as autografts. It is reported that the maximum strength of hamstring tendon is not less than that of BPTB graft [15], and the donor-site morbidity caused by the use of BPTB graft such as anterior knee pain, risks of patellar fracture and weakening of the extensor mechanism has increased [15, 33]. Therefore, there is a trend to prefer the use of hamstring tendons for PCL and ACL reconstruction. To the best of our knowledge, the Achilles tendon allograft is commonly used for PCL reconstruction, while the tibialis anterior allograft is limitedly applied in PCL reconstruction [27], despite its larger diameter compared with that of hamstring tendons. Moreover, the comparison of therapeutic effects in PCL reconstruction between tibialis anterior allograft and other grafts has not been reported. In this study, the outcomes in PCL reconstruction between 4-strand hamstring tendon autograft (4SHG) and 2-strand tibialis anterior allograft (2STAG) were compared in order to provide a clinical guidance for the treatment of PCL injury. The hypothesis of this study was that both grafts could afford good ligament reconstruction results.
Materials and methods
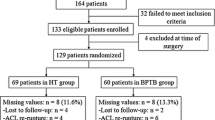
From 2005 to 2009, 49 consecutive patients with isolated PCL rupture underwent surgical reconstruction using 4SHG or 2STAG in our hospital, and their data were retrospectively analyzed. The inclusion criteria were (1) grade III PCL injury; (2) grade II PCL injury combined with persistent symptoms, such as pain which was not relieved by conservative treatment (medication and physical therapy) for more than 3 months; and (3) follow-up of more than 2 years. The exclusion criteria were (1) combined with ligament injury; (2) radiographically visible degenerative changes; and (3) contra-lateral knee ligament injury. Of the 49 patients, 37 patients were consistent with the inclusion criteria and were enrolled in this study. Each patient was fully informed of the disease details and the surgical procedures, especially graft selection including the advantages and disadvantages of different types of grafts. Eighteen patients selected 4SHG for PCL reconstruction. Of the 18 patients, 8 selected 4SHG in order to avoid allograft-related complications, 6 selected 4SHG in order to relieve the economic burden, and 4 patients had to select 4SHG because the allograft was unavailable in the perioperative period. Nineteen patients selected 2STAG for PCL reconstruction. Therefore, these patients were divided into two groups: Group A (4SHG, n = 18) and Group B (2STAG, n = 19).
Twenty-five patients were men and 12 women, with a mean age of 31.8 years (range, 18–55 years). Thirteen patients underwent PCL reconstruction on their left knees and 24 on their right knees. The interval between injury and PCL reconstruction was 8.9 months in group A and 9.3 months in group B (range 3 weeks to 12 months). The causes of PCL injury included traffic accidents in 14 patients, sports injuries in 12 patients, accidents during activities of daily living in 9 patients, and work-related injuries in 2 patients. There were no statistical differences in patients’ demographics between the two groups (Tables 1, 2). All the surgical procedures were performed by the same one surgeon (Lun-hao Bai).
Surgical technique
After adequate anesthetization, standard anterolateral and anteromedial portals were fashioned. Preliminary diagnostic arthroscopy was performed to evaluate the relevant anatomical structures and to identify the extent of the ligament tear and injuries of meniscus or cartilage. The associated injuries in both groups are shown in Table 1, and there were no statistical differences in the associated injuries between the two groups (n.s). Meniscal lesions were treated by partial meniscectomy.
In group A, the semitendinosus and gracilis tendons were harvested with a length of 22 cm. Then they were folded in half and sutured together using no. 1 absorbable sutures to form a four-strand graft with a median diameter of 7 mm (range 5–9) (Table 3). In group B, tibialis anterior allografts were used. These tibialis anterior allografts, originating from eligible tibialis anterior tendon tissue donated by humans, were provided by Shanxi OsteoRad Biomaterial Company (Taiyuan, China). The main procedures to treat these tissues include washing, radiation sterilization and deep freezing, which allow these tissues to reach sterile assurance level and to have low immunogenicity and excellent histocompatibility. The tibialis anterior tendon was trimmed to retain its original size normally with a length of 26–30 cm. Then it was folded in half and sutured together using no. 1 absorbable sutures to form a two-strand graft with a median diameter of 9 mm (range 8–10) (Table 3). The folded end of the graft, including 4SHG and 2STAG, was fixed proximally with EndoButton Fixation System (Smith & Nephew, Inc. Endoscopy Division, USA). The distal end was fixed with a cannulated interference screw (Smith & Nephew, Inc. Endoscopy Division, USA). The grafts were pretensioned with 60–80 N force for a minimum of 5 min.
The femoral tunnel was made using inside-out method. The center of the femoral tunnel was located in 6–8 mm from the posterior border of the articular cartilage. A posteromedial portal was created to fashion PCL tibial tunnel under direct arthroscopic vision. PCL stump was retained, and necessary debridement was performed to gain access to the insertion sites. The exit point of the tibial tunnel was located at 1–1.5 cm below the joint surface and was lateral to the midline of the posterior recess of the tibia (Fig. 1; Table 3). The surgeon allowed the graft to pass through the tunnels, including femoral tunnel and tibia tunnel using the inside-out method. The femoral end of the graft was fixed with EndoButton Fixation System. The knee was then placed in 70° flexion, and a strong anterior drawer force was applied to the proximal tibia. The distal end of the grafts was fixed to the anteromedial tibia using a cannulated interference screw.
Radiograph after PCL reconstruction. Red lines indicate femoral and tibial tunnels; line a the region of the posterior recess of the tibia; line b the midline of the posterior recess of the tibia; point c the central point of the exit point of the tibial tunnel; line d the joint surface; and line e the vertical distance from point c to line d
Postoperative rehabilitation
All patients wore a knee brace for 12 weeks after PCL reconstruction in both groups. First, the affected knee was maintained in a brace in full extension for 4 weeks and then was unlocked three times daily for progressive passive knee flexion exercise in the prone position during the next 8 weeks. During the first 12 weeks, crutches were used insistently with the affected knee in full extension to support their weight until patients could walk without the requirement of crutches. Patients usually returned to normal daily activity 3 months after PCL reconstruction, to light sports activity 6 months and to full pre-injury sports activities 9–12 months.
Evaluations
Clinical evaluations were performed preoperatively and 6, 12 and 24 months after PCL reconstruction. The last follow-up review was arranged between 2 and 3 years after PCL reconstruction according to the patients’ convenience, and the mean duration of follow-up was 2.3 years in group A and 2.4 years in group B. The last follow-up data were gathered and statistically analyzed. Lysholm knee scores, Tegner activity score and International Knee Documentation Committee (IKDC) were used to examine functional outcomes of the affected knee, and manual Posterior drawer test and knee laxity arthrometer measurements (side-to-side difference) to evaluate the knee laxity. Posterior drawer test was graded as grade 0 (no laxity), grade 1 (laxity <5 mm), grade 2 (laxity 5–10 mm) and grade 3 (laxity >10 mm) compared with contra-lateral knee. According to Ahlback classification, degenerative changes in the affected knee were evaluated based on knee radiographs [1]. To minimize susceptibility bias, all evaluations were performed by the same examiner who was not involved in the surgery.
All study methods were approved by the Ethics Committee of Shengjing Hospital of China Medical University. All the subjects enrolled into the study gave written formal consent to participate.
Statistical analysis
A power analysis was performed to determine the number of patients necessary to distinguish significant differences in knee laxity arthrometer measurements at the follow-up intervals. It was presumed that the population mean differences and the overall standard deviations represented by the samples of both groups were equal, and all were 2 mm, then the sample size to detect the difference with a confidence level of 95 % and a power of 80 % required 16 knees per group.
SPSS software (Version 13.0; SPSS Inc, Chicago, Illinois) was used for statistical treatment. Continuous data with normal distribution were expressed as mean ± standard deviation and non-normal distribution as median (range). A chi-square test was used for the comparison of nominal data, and an unpaired Student’s t test was used for the comparisons of continuous data when the data were normally distributed. The Wilcoxon signed rank test was used for data when the data were in non-normal distribution. Statistical significance was established at P value <0.05.
Results
In both groups, there were no immediate postoperative complications such as revision or readmission. In group A, two patients had paresthesia on the medial side of the knee, and the paresthesia completely disappeared about 6 months after PCL reconstruction. Three patients in group A and four patients in group B felt uncomfortable on the medial side of the knee during activities, and this symptom was partially or completely relieved by removing the mini-plate of the femoral fixation about 1 year after PCL reconstruction.
Preoperative and postoperative results of functional scores are showed in Table 2. There were no significant differences in preoperative items including Lysholm score, Tegner activity level and IKDC rating between both groups (n.s.). Meanwhile, compared with preoperative assessment, postoperative functional examination was significantly improved in both groups (P < 0.01). Furthermore, there were no significant differences in the postoperative functional examination between both groups (n.s.).
Preoperative and postoperative results of posterior drawer test and the knee laxity arthrometer side to side test (90° flexion and 132 N) used to evaluate posterior instability are shown in Table 4. There were no significant difference in preoperative posterior instability between group A and group B (n.s.). Meanwhile, compared with preoperative knee laxity arthrometer side to side test (11.7 ± 1.9 mm for group A and 11.9 ± 1.7 mm for group B), postoperative knee laxity arthrometer side to side test was significantly improved in both groups (4.1 ± 1.7 mm for group A and 3.3 ± 1.8 mm for group B) (P < 0.01). There was no statistical difference in postoperative knee laxity arthrometer side to side test between both groups (4.1 ± 1.7 mm for group A and 3.3 ± 1.8 mm for group B) (n.s.). However, compared with the contra-lateral knee (1.3 ± 0.6 mm for group A and 1.2 ± 0.5 mm for group B), postoperative knee laxity arthrometer side to side test was worse in both groups (4.1 ± 1.7 mm for group A and 3.3 ± 1.8 mm for group B) (P < 0.01). As to posterior drawer test, 17 % of knees in group A and 42 % of knees in group B had no posterior laxity; 61 % of knees in group A and 47 % of knees in group B exhibited grade 1 laxity; 22 % of knees in group A and 11 % of knees in group B showed grade 2 laxity; and grade 3 laxity was not found in both groups. There were no significant differences in postoperative posterior drawer test between both groups (n.s.). Two patients (11 %) in group A and one (5 %) in group B were found to have stage I radiographic degeneration at the final follow-up (n.s.).
Discussion
The most important findings of this study were that although 4SHG had comparatively short length and small diameter, the 4SHG was as good as 2STAG in PCL reconstruction. However, compared with the contra-lateral knee, the posterior stability was worse in both 4SHG and 2STAG groups.
In recent years, hamstring tendon autograft has been more used in PCL reconstruction compared with BPTB graft, because it produces less morbidity, particularly kneeling pain and extension deficit. 4SHG was usually used in clinical practice due to the length limitation of the hamstring tendon. The therapeutic effects of 4SHG in PCL reconstruction were different in the available studies. Some authors reported that the hamstring tendon autograft was better than the patellar tendon autograft in PCL reconstruction [21]; some found that the hamstring tendon autograft was similar to Achilles tendon allograft or BPTB autograft in PCL reconstruction [3, 31]; and some confirmed that 4SHT autograft was significantly poorer than BPTB autograft and LARS ligament, respectively [20, 26].
The maximum tensile stress of PCL and 4SHG are 1,800 and 4,000 N, respectively [12, 13]. The initial strength of 4SHG looks enough to reconstruct the injured PCL. However, in fact, the tendon–bone interface cannot be restored to its normal histological structure after ligament reconstruction using the existing treatment methods, leading to decreased strength of grafts [7]. In addition, it is well known that autografts have to undergo ‘ligamentization’ process including revascularization, cell proliferation and remodeling about 1 year after reconstruction, and they are prone to collapse and laxity in this course. There have not been reports about mechanical strength of grafts during or after ‘ligamentization’ and comparison between reconstructed knee and normal knee in PCL reconstruction. Janssen and Scheffler [16] reported that after the hamstring tendon grafts was used in ACL reconstruction, and the properties of ACL were improved, but a full restoration of either the biological or biomechanical properties of the ACL could not be obtained. Similar changes may occur in PCL reconstruction, which may be a cause that reconstructed PCL cannot return to normal completely.
Compared with ACL, PCL possesses more potential of spontaneous healing due to its better synovium coverage and blood supply [2, 17]. Therefore, during operation, PCL stump and its surrounding synovium are retained in order to promote grafts healing and incorporation, and moreover, PCL stump may provide mechanical support for the reconstructive ligament. PCL reconstruction using 4SHG alone can obtain better therapeutic effects because the mechanical strength of 4SHG combined with PCL stump is enough to act as PCL role [3, 21]. In this study, compared with preoperative assessment, the stability and function of the affected knee were significantly improved after PCL reconstruction using 4SHG by remnant preservation technique. Our results are consistent with those of some other results [3, 21].
The tibialis anterior allograft is commonly used in ACL reconstruction [4, 8, 24]; little research has been done about the application of tibialis anterior allograft in PCL reconstruction. Min et al. [27] used 2STAG in PCL reconstruction in 21 patients, and 2-year follow-up indicated that Lysholm knee score was 61–97, IKDC rating was normal in 8 patients, nearly normal in 9, abnormal in 3 and severely abnormal in one, and KT-2000 arthrometer was 3.4 ± 0.8 mm. These results were significantly improved compared with preoperative assessment, so they believed that tibialis anterior allograft was worth recommending in PCL reconstruction. At present, there have not been the reports about the comparison between tibialis anterior allograft and other grafts in PCL reconstruction. In this study, we compared the outcomes between 2STAG and 4SHG in PCL reconstruction, and 2-year follow-up indicated that both 2STAG and 4SHG obtained better therapeutic effects, and there was no significant difference in therapeutic effects between 2STAG and 4SHG. Our results cannot be compared with the results reported by Min et al. [27], because patient demographics, surgical technique and fixation were different in the two studies, but our results about 2STAG application in PCL are similar to that reported by Min et al. [27].
In this study, compared with the contra-lateral knee, the affected knee was worse in posterior stability of the knee joint including posterior drawer test and knee laxity arthrometer in both groups. This may be related to the following two aspects: (1) Zhao and Huangfu [37] compared 4SHT autograft with 7SHT autograft in PCL reconstruction with 2-year follow-up and found that the stability and functional outcomes of the affected knee were all significantly improved in 7SHT group. Therefore, they concluded that the diameter of grafts might be related to the results of PCL reconstruction, and increasing the diameter of grafts may compensate intensity strength loss of grafts during ‘ligamentization’ process. (2) In this study, only single-bundle reconstruction, mainly PCL anterolateral bundle, was performed. It is reported that single-bundle PCL reconstruction can allow the affected knee immediately to restore the mechanical stability, but with time extension, the posterior instability gradually occurs [10]. This may be that single-bundle reconstruction cannot anatomically rebuild the injured PCL, and the posterior stress force of the affected knee joint cannot uniformly be loaded to the grafts, leading to grafts laxity [14]. Moreover, in single-bundle reconstruction, the posterior stability of the affected knee joint is maximum in knee flexion 90° and is small in knee flexion <30°, and the rotational stability of the affected knee joint is also small in knee flexion more than 90° [11, 25]. Double-bundle PCL reconstruction may avoid these problems [36]. (3) When the patient is in supine position, the tibia always has a tendency to shift back due to calf gravity and stretching effects of the hamstring [18]. The continuous backward stress may lead to grafts laxity; especially during ‘ligamentization’ process, the backward stress is more dangerous for the grafts because the strength of grafts is decreased.
Traditionally, isolated PCL tears are treated with non-operative method, which shows favorable results [5, 28, 29, 32]. However, some studies have found that with time extension, some patients with isolated PCL have osteoarthritis and exhibit deterioration in knee function [5, 28]. With the progress in arthroscopic technology, PCL reconstruction has become the first choice of surgeons for the treatment of completely disrupted PCL in order to restore knee stability and prevent knee osteoarthritis. However, which therapeutic effects between conservative and surgical strategies for PCL injuries are better has so far proved inconclusive, especially in restoring knee stability and preventing knee osteoarthritis. Arthroscopic PCL reconstruction with single-bundle graft, which is relatively simple and effective, has become the most common method for PCL reconstruction at present. A few studies related to osteoarthritis in conservative treatment and single-bundle reconstruction were reviewed (Table 5) [5, 6, 21–23, 28–30, 32, 34, 35]. In these literatures, compared with conservative treatment, the follow-up duration is shorter and mostly <10 years in surgical treatment, but data indicate that surgical treatment still has no vantage to prevent knee osteoarthritis. This may be that (1) in PCL reconstruction, the most basic factor to prevent osteoarthritis is to restore knee stability, but it is difficult to make knee joint return to previous healthy condition due to complex anatomy and the limitation of current surgical conditions, so the degenerative osteoarthritis can gradually occur after PCL reconstruction and (2) PCL injury commonly combines with injuries of meniscus injury and/or articular cartilage, which can trigger joint degeneration. It is difficult to identify whether the degenerative changes are caused by the injuries of meniscus and/or articular cartilage or by PCL reconstruction. In this study, PCL single-bundle reconstruction was performed, and degenerative changes only occurred in three patients (8 %), which is less than that reported in these literatures [5, 6, 21–23, 28–30, 32, 34, 35]. However, in this study, the follow-up duration was only 2 years, which is too short for osteoarthritis development, so PCL single-bundle reconstruction preventing knee osteoarthritis cannot be fully confirmed only by our data.
The limitation in this study was relatively short follow-up and limited cohort. Meanwhile, this study was a retrospective study, and the patients were not assigned randomly, but according to grafts type selected by patients, increasing selection bias. However, there were several strengths in this study, including the matched demographic features of these patients, same surgeon, surgical techniques, fixation method and rehabilitation program, which increased the power of statistical results.
Conclusions
In this study, relatively good functional and mechanical results were obtained in PCL reconstruction by using both 4SHG and STAG, and no significant differences were identified in functional and mechanical results of the affected knees between 4SHG and STAG, but both groups exhibit slight residual knee laxity in affected knees compared with contra-lateral knees.
References
Ahlbäck S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 277:7–72
Ahn JH, Yang HS, Jeong WK, Koh KH (2006) Arthroscopic transtibial posterior cruciate ligament reconstruction with preservation of posterior cruciate ligament fibers: clinical results of minimum 2-year follow-up. Am J Sports Med 34:194–204
Ahn JH, Yoo JC, Wang JH (2005) Posterior cruciate ligament reconstruction: double-loop hamstring tendon autograft versus Achilles tendon allograft—clinical results of a minimum 2-year follow-up. Arthroscopy 21:965–969
Almqvist KF, Jan H, Vercruysse C, Verbeeck R, Verdonk R (2007) The tibialis tendon as a valuable anterior cruciate ligament allograft substitute: biomechanical properties. Knee Surg Sports Traumatol Arthrosc 15:1326–1330
Boynton MD, Tietjens BR (1996) Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med 24:306–310
Chan YS, Yang SC, Chang CH, Chen AC, Yuan LJ, Hsu KY, Wang CJ (2006) Arthroscopic reconstruction of the posterior cruciate ligament with use of a quadruple hamstring tendon graft with 3- to 5-year follow-up. Arthroscopy 22:762–770
Chen CH (2009) Strategies to enhance tendon graft—bone healing in anterior cruciate ligament reconstruction. Chang Gung Med J 32:483–493
Cooper MT, Kaeding C (2010) Comparison of the hospital cost of autograft versus allograft soft-tissue anterior cruciate ligament reconstructions. Arthroscopy 26:1478–1482
Díaz-de-Rada P, Barriga A, Barroso JL, García-Barrecheguren E, Alfonso M, Valentí JR (2003) Positive culture in allograft ACL-reconstruction: what to do? Knee Surg Sports Traumatol Arthrosc 11:219–222
Galloway MT, Grood ES, Mehalik JN, Levy M, Saddler SC, Noyes FR (1996) Posterior cruciate ligament reconstruction: an in vitro study of femoral and tibial graft placement. Am J Sports Med 24:437–445
Gill TJ, DeFrate LE, Wang C, Carey CT, Zayontz S, Zarins B, Li G (2003) The biomechanical effect of posterior cruciate ligament reconstruction on knee joint function: kinematic response to simulated muscle loads. Am J Sports Med 31:530–536
Hamner DL, Brown C, Steiner ME, Hecker AT, Hayes WC (1999) Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 81:549–557
Harner CD, Xerogeanes JW, Livesay GA, Carlin GJ, Smith BA, Kusayama T, Kashiwaguchi S, Woo SL (1995) The human posterior cruciate ligament complex: an interdisciplinary study. Ligament morphology and biomechanical evaluation. Am J Sports Med 23:736–745
Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin TM, Woo SL (2000) Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med 28:144–151
Höher J, Scheffler S, Weiler A (2003) Graft choice and graft fixation in PCL reconstruction. Knee Surg Sports Traumatol Arthrosc 11:297–306
Janssen RP, Scheffler SU (2013) Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2634-5
Jung YB, Jung HJ, Yang JJ, Yang DL, Lee YS, Song IS, Lee HJ (2008) Characterization of spontaneous healing of chronic posterior cruciate ligament injury: analysis of instability and magnetic resonance imaging. J Magn Reson Imaging 27:1336–1340
Jung YB, Tae SK, Lee YS, Jung HJ, Nam CH, Park SJ (2008) Active non-operative treatment of acute isolated posterior cruciate ligament injury with cylinder cast immobilization. Knee Surg Sports Traumatol Arthrosc 16:729–733
Kim YM, Lee CA, Matava MJ (2011) Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 39:425–434
Li B, Wen Y, Wu H, Qian Q, Wu Y, Lin X (2009) Arthroscopic single-bundle posterior cruciate ligament reconstruction: retrospective review of hamstring tendon graft versus LARS artificial ligament. Int Orthop 33:991–996
Lin YC, Chen SK, Liu TH, Cheng YM, Chou PP (2013) Arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction using patellar tendon graft compared with hamstring tendon graft. Arch Orthop Trauma Surg 133:523–530
MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF (2006) Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy 22:320–328
Mariani PP, Adriani E, Santori N, Maresca G (1997) Arthroscopic posterior cruciate ligament reconstruction with bone-tendon-bone patellar graft. Knee Surg Sports Traumatol Arthrosc 5:239–244
Mariscalco MW, Magnussen RA, Mehta D, Hewett TE, Flanigan DC, Kaeding CC (2014) Autograft versus nonirradiated allograft tissue for anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 42:492–499
Markolf KL, Feeley BT, Jackson SR, McAllister DR (2006) Biomechanical studies of double-bundle posterior cruciate ligament reconstructions. J Bone Joint Surg Am 88:1788–1794
Maruyama Y, Shitoto K, Baba T, Kaneko K (2012) Evaluation of the clinical results of posterior cruciate ligament reconstruction—a comparison between the use of the bone tendon bone and semitendinosus and gracilis tendons. Sports Med Arthrosc Rehabil Ther Technol 4:30
Min BH, Lee YS, Lee YS, Jin CZ, Son KH (2011) Evaluation of transtibial double-bundle posterior cruciate ligament reconstruction using a single-sling method with a tibialis anterior allograft. Am J Sports Me 39:374–379
Parolie JM, Bergfeld JA (1986) Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med 14:35–38
Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT (2007) The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term followup study. HSS J 3:137–146
Sekiya JK, West RV, Ong BC, Irrgang JJ, Fu FH, Harner CD (2005) Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy 21:1042–1050
Seon JK, Song EK (2006) Reconstruction of isolated posterior cruciate ligament injuries: a clinical comparison of the transtibial and tibial inlay techniques. Arthroscopy 22:27–32
Shelbourne KD, Clark M, Gray T (2013) Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med 41:1526–1533
Tom JA, Rodeo SA (2002) Soft tissue allografts for knee reconstruction in sports medicine. Clin Orthop Relat Res 402:135–156
Wang CJ, Chan YS, Weng LH, Yuan LJ, Chen HS (2004) Comparison of autogenous and allogenous posterior cruciate ligament reconstructions of the knee. Injury 35:1279–1285
Wu CH, Chen AC, Yuan LJ, Chang CH, Chan YS, Hsu KY, Wang CJ, Chen WJ (2007) Arthroscopic reconstruction of the posterior cruciate ligament by using a quadriceps tendon autograft: a minimum 5-year follow-up. Arthroscopy 23:420–427
Yoon KH, Bae DK, Song SJ, Cho HJ, Lee JHA (2011) Prospective randomized study comparing arthroscopic single-bundle and double-bundle posterior cruciate ligament reconstructions preserving remnant fibers. Am J Sports Med 39:474–480
Zhao J, Huangfu X (2007) Arthroscopic single-bundle posterior cruciate ligament reconstruction: retrospective review of 4- versus 7-strand hamstring tendon graft. Knee 14:301–305
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, B., Wang, Js., He, M. et al. Comparison of hamstring tendon autograft and tibialis anterior allograft in arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 23, 3077–3084 (2015). https://doi.org/10.1007/s00167-014-3267-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3267-z