Abstract
Purpose
Opening wedge high tibial osteotomy (HTO) is an accepted treatment option for medial compartment knee osteoarthritis with associated varus lower limb axis in younger, more active patients. A concern with the use of this technique is that posterior tibial slope (PTS) and tibial rotation can be altered. We hypothesized that there is a tendency to increase the PTS and internal rotation of the distal tibia during the procedure and that certain intra-operative parameters may influence the amount of change that can be expected.
Methods
A cadaveric model and surgical navigation system were used to evaluate the influence of certain intra-operative factors of the degree of PTS and tibial rotation change observed during medial opening HTO. Parameters evaluated included: degree of osteotomy opening, knee flexion angle, location of limb support (thigh versus foot), performance of a posteromedial release, the status of the lateral cortical hinge, and the degree of osteoarthritis present in the knee.
Results
Combining measurements of all specimens and parameters, a mean PTS increase of 2.7° ± 3.9° and a mean tibial internal rotation of 1.5° ± 2.9° were observed. Clinically, significant changes in tibial slope (>2°) occurred in 50.4 % of corrections, while significant changes in tibial rotation (>5°) occurred in only 11.9 % of corrections. Patients with significant osteoarthritis and concomitant flexion contracture, cases where large corrections were required, and procedures in which the lateral cortical hinge was disrupted were associated with increased PTS change. The other factors evaluated did not exert a significant influence of the degree of PTS change observed.
Conclusions
Surgeons should be vigilant for possible PTS change, particularly in high-risk situations as outlined above. Routine use of an intra-operative measure of PTS is recommended to avoid inadvertent slope change.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One frequently reported problem associated with opening wedge high tibial osteotomy (HTO) is that posterior tibial slope (PTS) can be altered [1–11]. In clinical follow-up studies, an unintended increase in slope of up to a mean of 4.4° has been reported [3, 9, 12–14]. While such an increase can be beneficial in cases of posterior cruciate ligament deficiency, incidental slope increase is generally avoided as it can lead to anterior translation of the tibia relative to the femur, especially if anterior cruciate ligament deficiency is present [15, 16].
Several theories exist regarding the etiology of PTS change following HTO. One widely discussed theory is that the triangular shape of the proximal tibia is responsible for the PTS increase. The bone’s shape demands as a matter of geometry a smaller opening of the osteotomy anteriorly (which is closer to the osteotomy hinge) than posteriorly if the PTS is to remain unchanged [2, 11, 17]. Anterior plate placement may compound this problem by more effectively opening the osteotomy anteriorly [17–20]. Another factor affecting the PTS is the location of the cortical hinge on the lateral side. If the osteotomy is not performed in the frontal but rather in an oblique plane with the hinge posterolateral, the PTS can be increased [21]. According to Marti, an incomplete posterior osteotomy cut and inappropriate release of posterior soft tissues can be responsible for a PTS increase, resulting in increased opening anteriority [9]. In addition to the PTS change, tibial rotation can also be modified during opening wedge HTO; however, very little evidence about this subject is available in literature [22, 23]. Change of rotation cannot be reliably evaluated on standard radiographs, and clinical examination is not sensitive for small changes up to 5°.
Intra-operative PTS and tibial rotation control can be measured by different methods including computer navigation [23–26] and control with two parallel K-wires proximal and distal of the osteotomy [27]. Moreover, the PTS change can be estimated intra-operatively by judging the anterior osteotomy gap to be one half to two thirds of the posterior gap [11, 25] and by ensuring that there is no change in the degree of extension possible before osteotomy and after fixation [25].
Based clinical concern for unintended PTS change and tibial rotation during opening wedge HTO, this project was designed to study in a cadaveric setting factors responsible for PTS and tibial rotation change. Based on prior clinical observations, we hypothesized that there is a tendency to increase the PTS and the internal rotation of the distal tibia during the procedure and that certain intra-operative parameters may influence the amount of change that can be expected.
Materials and methods
This cadaveric study was performed in seven fresh cadavers with a total of eleven knees that could be used. Only specimens without surgical scars around the knee were used. The mean age of the knees was 80 (67–92) years and included seven male and four female knees. The other three knees had surgical scars and were excluded.
Setting and preparation
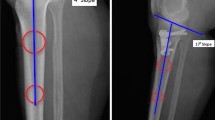
To mimic a realistic intra-operative setting, the cadavers were placed in supine position. A longitudinal anteromedial incision was made and utilized to create a medial arthrotomy and a standard anteromedial approach to the proximal tibia. The arthrotomy was required for referencing for the navigation system and allowed assessment of the degree of degenerative change present in the knee joint. The arthrotomy was closed with sutures after referencing. The distal part of the incision was then continued below the pes anserinus insertion, and the pes tendons, patellar tendon insertion, and medial collateral ligament (MCL) were identified. The osteotomy site was marked just proximal to the pes anserinus and included sectioning of the superficial MCL just above the upper pes anserinus margin. The descending insertion of the semimembranosus and the proximal part of the superficial MCL insertion remained intact. An ACL guide was then used to place a K-wire from the medial starting point laterally to the desired location of the hinge on the lateral tibia. This point was located 1–2 cm distal to the lateral joint line in all cases. To secure the lateral hinge during the measurements, an external fixator was placed laterally, bridging the lateral hinge location (Fig. 1). The reference markers for the computer navigation system were placed as detailed below.
Computer navigation
The computer navigation system used included PLEOS® Knee software and the PLEOS® platform (TORNIER, Saint-Ismier, France). The system has previously validated precision to within 1° of rotation around 3 axes and 1 mm of translation along three axes [28]. Software modification was done specifically for this study to allow assessment of the motion of the proximal and distal segments of the tibia independently. Three trackers were fixed with two-threaded pins on the femur, proximal tibia, and distal tibia (Fig. 1). The setup allowed real-time measurement of the hip–knee–ankle angle and knee flexion angle. Software modification allowed measurement of motion between the proximal and distal tibia trackers, including the osteotomy opening angle (rotation around the z-axis), PTS change (rotation around the x-axis), and rotational change (rotation around the y-axis). Acquisitions were stored as screen capture and were later migrated to statistics software.
Measurement parameters
Different intra-operative parameters were tested to evaluate their influence on PTS and rotation change. As far as possible, all parameters were combined with each other. However, certain steps were irreversible such as the posteromedial corner release. Furthermore, the bone quality did not allow an unlimited repetition of measurements. The following parameters were evaluated:
-
Osteotomy opening (degrees): Three amounts of correction were studied (5° small correction, 10° medium correction, and 15° large correction). The amount of correction was verified with the navigation system.
-
Knee position: Measurements were taken in 90°, 45° and 0° of knee flexion. The amount of knee flexion was controlled with the navigation system.
-
Posteromedial corner release: Measurements were taken before and after section of the descending insertion of the semimembranosus.
-
Location of support: Measurements were taken with the leg supported under the thigh as well as with support from under the foot.
-
Osteotomy hinge: The lateral hinge was initially secured by an external fixator to avoid hinge fracture [27]. As this method is not utilized by most surgeons, measurements were repeated without the fixator in place and finally after the hinge was completely cut with an osteotome.
-
Position of spreader: The influence of an anteriorly versus posteriorly placed spreader was tested.
-
Influence of osteoarthritis (OA): Each specimen was classified according to the ICRS classification (0–4) according to area of most advanced degeneration in the tibiofemoral joint. The knees were divided into mild OA (grades 0–2) and significant OA (grades 3–4) groups. If there was an extension deficit associated with the OA, it was documented with the navigation system.
Surgery and measurement course
After referencing and calibration of the navigation system, the arthrotomy was closed with sutures. Subperiosteal posterior tibial preparation was performed at the osteotomy site. The osteotomy was performed with an oscillating saw and osteotomies below the K-wires. The main osteotomy plane was in relation to the frontal plane oblique, rising from the pes anserinus level to the tip of the fibula. In relation to the sagittal plane, it was perpendicular to the tibial axis and in relation to the axial plane the osteotomy was parallel to the frontal plane. An additional oblique frontal plane osteotomy was performed to protect the tibial tuberosity and the patellar tendon insertion [29]. The osteotomy was slowly and carefully opened, initially with several osteotomies and then with a spreader. The osteotomy was held open with spacers with millimetre increments. The measurements were thereafter started with different osteotomy corrections, knee positions, and other parameters as detailed above. Each measurement point was triggered by the precise amount of osteotomy correction and knee flexion, based on data from the navigation system. During the measurements, the leg was placed on the support (either thigh or foot) without influencing the PTS or the rotation. Each measurement point was stored as a screen capture.
IRB approval
No IRB approval was required for this cadaveric study.
Statistical analysis
Arithmetic means along with standard deviations and ranges were calculated for each continuous variable. Based on the data characteristics, comparisons were made using the Wilcoxon signed-rank test or the Friedman test. A p value of <0.05 was considered statistically significant. Statistical analyses were carried out using MedCalc Software, Version 12.3.0, Broekstraat 52, 9030 Mariakerke, Belgium.
Results
Global data
The mean initial hip–knee–ankle angle of the 11 knees was 176 ± 2.2 (172–179). Four of the specimens where rated to have grade 3–4 osteoarthritis while seven had only slight osteoarthritic changes (grade 0–2) according to Outerbridge [30]. Combining measurements of all specimens and parameters (n = 363; 33 per knee), a mean PTS increase of 2.7° ± 3.9° with a range of −4° to 17° was observed. The mean overall rotation change was internal rotation of the distal tibia by 1.5° ± 2.9° with a range of −4.5° to 15°. Assuming rotation changes >5° are clinically relevant, 11.9 % of measurements resulted in clinically significant rotational changes. Assuming that a PTS changes >2° are clinically relevant, 50.4 % of measurements resulted in a clinically significant change.
Influence of the knee flexion and osteotomy opening (Measurements with 5°, 10° and 15° osteotomy opening and with 90°, 45° and 0° knee flexion)
PTS change was influenced primarily by the degree of osteotomy opening. Increasing the correction from 5 to 10 to 15° resulted in a significant increase of the PTS (p < 0.0001, Fig. 2). Knee flexion had only a minor influence as greater extension resulted in slightly smaller PTS changes (p = 0.0235, Fig. 2). No significant influence of knee extension or degree of osteotomy opening on tibial rotation was noted.
Boxplots showing the PTS change grouped by the amount of osteotomy opening and clustered by the amount of knee flexion (significances are reported in Table 1)
Influence of posteromedial corner release [31] (Measurements with 5°, 10° and 15° osteotomy opening and with 90°, 45° and 0° flexion)
Measurements done before and after release of the posteromedial corner revealed no significant differences in PTS change or tibial rotation change (Table 1). A qualitative observation was that opening of the osteotomy to 15° of correction prior to release was very difficult in several knees due to excessive tension, whereas opening was facilitated following the release.
Influence of the lateral hinge (Measurements with 5°, 10° and 15° osteotomy opening and with 90°, 45° and 0° flexion)
Measurements were first done with an external fixator in place securing the lateral hinge, repeated after removal of the fixator, and then repeated again after complete disruption of the lateral hinge. There was no significant change in PTS or tibial rotation change after removal of the external fixator. However, after complete hinge disruption, the PTS change was significantly increased (p = 0.0012) while tibial rotation change was not affected (Table 1). Complete disruption of the lateral hinge was always the last step in the series.
Influence of thigh or foot support (Measurements with 10° osteotomy opening and with 90°, 45° and 0° flexion)
The difference between foot and thigh support was compared with 10° of osteotomy opening. There was no significant difference in PTS change or in tibial rotation change between the two conditions (Table 1).
Influence of spreader position (Measurements with 10° osteotomy opening and with 90°, 45° and 0° flexion)
There was no significant difference in PTS change or in tibial rotation change between the two spreader positions (Table 1).
Influence of osteoarthritis (Measurements with 5°, 10° and 15° correction and with 90°, 45° and 0° flexion)
Four of the specimens had grade 3–4 osteoarthritis while seven had only slight osteoarthritic changes (grade 0–2) according to Outerbridge [30]. The specimens with osteoarthritis had at baseline a mean flexion contracture of 5° ± 1.4°, while those with mild OA all reached full extension. Advanced OA was associated with a significantly increased PTS change (p < 0.0001) and a decreased tibial rotation change (p < 0.0001, Fig. 3; Table 1).
Boxplots showing the PTS change grouped by the degree of osteoarthritis (OA) and clustered by the amount of osteotomy opening (significances are reported in Table 1)
Discussion
The main finding of this study is that there is a spontaneous and unintended tendency to increase the PTS and to increase internal rotation of the distal tibia during opening wedge HTO. The changes are highly variable and frequently the amount of change is too small to be clinically significant; however, the maximum measured changes during this study (maximal PTS change 17° and maximal rotation change 15°) highlight the need to be vigilant for these problems. It only can be hypnotized why such a high variation was observed. Possible factors are variable stability of the lateral hinge, variable tension of posterior soft tissues and other undefined reasons.
Several parameters have been identified that affect the amount of PTS and tibial rotation that can be expected. The presence of osteoarthritis in the tibiofemoral joint in particular played a large role. All 4 knees in our study with significant OA did have a concomitant flexion contracture. The presence of contracted posterior soft tissues may have contributing to the observed increased PTS change and decreased tibial rotation in this group. Based on our findings, it is questionable if observation of maximum extension pre- and post-osteotomy as suggested by Song is sufficient to monitor PTS [25]. A second parameter affecting both tibial rotation and PTS change was the amount of correction performed. It is clear that the larger the correction, the more freedom is present for PTS or tibial rotation change. This explanation is supported by our finding that larger corrections yielded not only increased mean values for PTS and tibial rotation change, but also increased variability in the observed values. The changes noted in small corrections were generally below clinical significance; however, in cases with concomitant ACL deficiency, even small changes may be important. A third factor that influenced the results was the knee position (flexion/extension). Whereas change to internal rotation was more pronounced in extension then in flexion, PTS was altered less in full extension.
The findings of this study are clinically relevant, as evidence by numerous reports of unintended increases in slope after open wedge HTO in the clinical literature [3, 9, 12–14]. While such an increase can be beneficial in cases of posterior cruciate ligament deficiency, incidental slope increase is generally avoided as it can lead to anterior translation of the tibia relative to the femur, especially if anterior cruciate ligament deficiency is present [15, 16].
The strengths of our study are the use of a realistic intra-operative setting and precise measurements of PTS and tibial rotation change with a navigation system, which has a validated precision of <1° [28]. The study clearly outlines which parameters tend to influence PTS and tibial rotation change the most and which ones have relatively little impact. Such information is quite useful to surgeons performing osteotomies, particularly in cases with ACL deficiency. This study also has several limitations. First, the cadavers we utilized may not necessarily represent the tissue quality and pathological situation (age, osteoarthritis pattern) of patients typically undergoing medial opening wedge HTO. Second, as the study protocol included multiple measurement points, the osteotomy was repeatedly manipulated. This repeated manipulation led to tissue fatigue and eventually failure over time. Generally, about 50 measurements could be done on each knee. Steps were performed in different orders in different knees when possible to minimize potential bias from this limitation.
Conclusion
Special attention to avoid unintended PTS change in opening wedge HTO is necessary in patients with significant osteoarthritis and concomitant flexion contracture, in cases where large corrections are required, and procedures in which the lateral cortical hinge is disrupted. These patients are at high risk for significant PTS change. Routine use of an intra-operative measure of PTS is recommended to avoid inadvertent slope change.
References
Amendola A, Fowler PJ, Litchfield R, Kirkley S, Clatworthy M (2004) Opening wedge high tibial osteotomy using a novel technique: early results and complications. J Knee Surg 17(3):164–169
Asada S, Akagi M, Mori S, Matsushita T, Hashimoto K, Hamanishi C (2012) Increase in posterior tibial slope would result in correction loss in frontal plane after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 20(3):571–578
Bombaci H, Canbora K, Onur G, Gorgec M (2005) The effect of open wedge osteotomy on the posterior tibial slope. Acta Orthop Traumatol Turc 39(5):404–410
Dejour H, Neyret P, Boileau P, Donell ST (1994) Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthop 299:220–228
Ducat A, Sariali E, Lebel B, Mertl P, Hernigou P, Flecher X, Zayni R, Bonnin M, Jalil R, Amzallag J, Rosset P, Servien E, Gaudot F, Judet T, Catonne Y (2012) Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res 98(1):68–74
El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S (2010) Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med 38(2):323–329
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 69(3):332–354
Lustig S, Scholes CJ, Costa AJ, Coolican MJ, Parker DA (2013) Different changes in slope between the medial and lateral tibial plateau after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):32–38
Marti CB, Gautier E, Wachtl SW, Jakob RP (2004) Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy 20(4):366–372
Matar WY, Boscariol R, Dervin GF (2009) Open wedge high tibial osteotomy: a roentgenographic comparison of a horizontal and an oblique osteotomy on patellar height and sagittal tibial slope. Am J Sports Med 37(4):735–742
Noyes FR, Goebel SX, West J (2005) Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med 33(3):378–387
Brouwer RW, Bierma-Zeinstra SM, van Koeveringe AJ, Verhaar JA (2005) Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br 87(9):1227–1232
El-Azab H, Halawa A, Anetzberger H, Imhoff AB, Hinterwimmer S (2008) The effect of closed- and open-wedge high tibial osteotomy on tibial slope: a retrospective radiological review of 120 cases. J Bone Joint Surg Br 90(9):1193–1197
Ribeiro CH, Severino NR, Cury Rde P, de Oliveira VM, Avakian R, Ayhara T, de Camargo OP (2009) A new fixation material for open-wedge tibial osteotomy for genu varum. Knee 16(5):366–370
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76(5):745–749
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2):376–382
Hernigou P (2002) Open wedge tibial osteotomy: combined coronal and sagittal correction. Knee 9(1):15–20
Amendola A (2003) Unicompartmental osteoarthritis in the active patient: the role of high tibial osteotomy. Arthroscopy 19(Suppl 1):109–116
Pape D, Madry H (2013) The preclinical sheep model of high tibial osteotomy relating basic science to the clinics: standards, techniques and pitfalls. Knee Surg Sports Traumatol Arthrosc 21(1):228–236
Rodner CM, Adams DJ, Diaz-Doran V, Tate JP, Santangelo SA, Mazzocca AD, Arciero RA (2006) Medial opening wedge tibial osteotomy and the sagittal plane: the effect of increasing tibial slope on tibiofemoral contact pressure. Am J Sports Med 34(9):1431–1441
Wang JH, Bae JH, Lim HC, Shon WY, Kim CW, Cho JW (2009) Medial open wedge high tibial osteotomy: the effect of the cortical hinge on posterior tibial slope. Am J Sports Med 37(12):2411–2418
Baumgarten KM, Meyers KN, Fealy S, Wright TM, Wickiewicz TL (2007) The coronal plane high tibial osteotomy. Part II: a comparison of axial rotation with the opening wedge high tibial osteotomy. HSS J 3(2):155–158
Kendoff D, Lo D, Goleski P, Warkentine B, O’Loughlin PF, Pearle AD (2008) Open wedge tibial osteotomies influence on axial rotation and tibial slope. Knee Surg Sports Traumatol Arthrosc 16(10):904–910
Akamatsu Y, Mitsugi N, Mochida Y, Taki N, Kobayashi H, Takeuchi R, Saito T (2012) Navigated opening wedge high tibial osteotomy improves intraoperative correction angle compared with conventional method. Knee Surg Sports Traumatol Arthrosc 20(3):586–593
Song EK, Seon JK, Park SJ (2007) How to avoid unintended increase of posterior slope in navigation-assisted open-wedge high tibial osteotomy. Orthopedics 30(10 Suppl):S127–S131
Yamamoto Y, Ishibashi Y, Tsuda E, Tsukada H, Kimura Y, Toh S (2008) Validation of computer-assisted open-wedge high tibial osteotomy using three-dimensional navigation. Orthopedics 31(10 Suppl 1):256–261
Jacobi M, Wahl P, Jakob RP (2010) Avoiding intraoperative complications in open-wedge high tibial valgus osteotomy: technical advancement. Knee Surg Sports Traumatol Arthrosc 18(2):200–203
Lustig S, Fleury C, Goy D, Neyret P, Donell ST (2011) The accuracy of acquisition of an imageless computer-assisted system and its implication for knee arthroplasty. Knee 18(1):15–20
Pape D, Dueck K, Haag M, Lorbach O, Seil R, Madry H (2013) Wedge volume and osteotomy surface depend on surgical technique for high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):127–133
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43-B:752–757
Okal F, Hart R, Komzak M (2012) The effect of releasing the medial stabilisers of the knee on the magnitude of correction in opening-wedge high-tibial valgus osteotomy. Anatomy study on cadavers. Acta Chir Orthop Traumatol Cech 79(4):355–360
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacobi, M., Villa, V., Reischl, N. et al. Factors influencing posterior tibial slope and tibial rotation in opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 23, 2762–2768 (2015). https://doi.org/10.1007/s00167-014-3100-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3100-8