Abstract
Purpose
To identify patient concomitant injury and surgical characteristics associated with 6-month excellent functional and isokinetic testing results following anterior cruciate ligament (ACL) reconstruction.
Methods
Patients that underwent ACL reconstruction by a single surgeon had isokinetic and functional testing performed with excellent 6-month outcome defined as greater than 85 % in isokinetic strength and 90 % in functional tests (excellent 6-month group vs. delayed 6-month group). Patient concomitant injury and surgical factors were then analysed in univariate and multivariate statistical models to assess which characteristics predicted the excellent 6-month group.
Results
The 224 patients included 93 males and 131 females, with median age of 22 (range 12–59) years, body mass index (BMI) of 25.4 (range 17–44), and median Tegner activity score of 6 (range 2–10). Fifty-two patients (23 %) were included in the excellent 6-month group, while 172 patients (77 %) were in the delayed 6-month group. In univariate analysis, favourable factors with the excellent 6-month outcome group were younger age (24 vs. 27; p = 0.01), lower BMI (24.5 vs. 26.2; p = 0.03), and minimal articular cartilage damage (71 vs. 56 %; p = 0.048). In multivariate analysis, a negative effect was observed for patients older than 30 years that had ACL reconstruction with autograft (p = 0.0004).
Conclusion
Factors significantly associated with excellent 6-month functional and isokinetic test results following ACL reconstruction included younger age, lower BMI, and minimal cartilage degeneration. The use of allograft was associated with improved functional and strength testing after ACL reconstruction in patients over 30 years of age.
Level of evidence
Prognostic/therapeutic study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tear of the anterior cruciate ligament (ACL) is a common knee injury that has been reported at 81 ruptures per 100,000 people [16]. These injuries require rehabilitation, and in many cases reconstructive surgery. A survey by American Academy of Orthopedic Surgeons about current trends in ACL reconstruction disclosed that most surgeons report return to sport between 5 and 6 months following ACL reconstruction [13]. However, patient surveys reveal that the average time for return to sports following ACL reconstruction is often greater than 6 months [44]. Shah and Andrews et al. report that only sixty-three per cent (31 of 49) of NFL athletes returned to NFL game play at an average of 10.8 months after surgery [43].
While ACL reconstruction has been shown to demonstrate excellent results in terms of biomechanics [30] and functional outcomes [10], controversy remains in regard to graft type (autograft vs. allograft [14, 35, 49], and hamstring vs. patellar tendon autograft) [1]. Heterogeneity of patient demographics and intra- and post-operative practices makes it challenging to predict which patients will be able to recover quickly and return to sports at 6 months. Accelerated return-to-play programmes by Shelbourne and Nitz advocate that early post-operative rehabilitation has been effective [10, 30, 43, 45], although surgeons lack well-defined factors to help identify the patients for which early rehabilitation is best suited. Objective measurements of functional and isokinetic testing are often used to guide decision-making regarding clearance for sport and risk of reinjury. These measurements have recently been validated following ACL reconstruction to correlate with traditional knee function tests and have determined return to sports activities [25].
Currently, surgeons have little information to identify which factors contribute to recovery of function and strength following ACL reconstruction at an early time point (6 months). It would be helpful to know why some athletes recover quickly and others tend to take a longer period of time to regain strength and function. This information is valuable in helping to counsel patients about the impact of graft choice on early recovery, how meniscus status, articular cartilage status, patient age, and body mass index (BMI) all can play a role in potential length of recovery and anticipated clearance for return to activity. To our knowledge, there are no data analysing potential causes for differences in regaining early function in this setting.
Therefore, a retrospective comparative study was designed to include patients with early excellent 6-month functional and isokinetic testing results (excellent 6-month group) versus a group that did not meet criteria for early excellent functional and isokinetic results (delayed 6-month group) following ACL reconstruction. The purpose of this study was to identify patient concomitant injury and surgical characteristics associated with early excellent functional and isokinetic testing results at 6 months following ACL reconstruction surgery. To our knowledge, this is the first study to evaluate factors that may play a role in early return of isokinetic strength and function following ACL reconstruction.
Materials and methods
For this retrospectively matched case–control study, we searched our institutional computerized database to identify all patients with a history of primary ACL reconstruction performed between 1998 and 2005 for a single surgeon (DLD). Patient demographic information including preinjury Tegner score, age, gender, BMI, and surgical data relating to graft type employed and concomitant injuries, such as cartilage degeneration and meniscal injury, were recorded. Other concomitant injuries such as bone bruises were evaluated with MRI. Medial collateral ligament (MCL) sprain was diagnosed on physical examination. Cartilage damage was graded 0–4 using the Outerbridge chondral knee lesion classification [8]. All patients gave written consent to participate in the study, and the study was approved by our institutional review board.
Inclusion/exclusion criteria
The study population included patients undergoing primary one-incision, arthroscopically assisted ACL reconstruction. Patients were excluded from the study if they had previous ipsilateral knee surgery or contralateral ACL reconstruction, or had a concurrent procedure performed on the knee at the time of ACL reconstruction that altered their post-operative crutch use or rehabilitation (i.e. other ligament repair or reconstruction, cartilage procedure). Patients requiring concomitant meniscal or minor chondral procedures (i.e. chondroplasty) were included in the study as their rehabilitation was not modified following surgery.
Surgical procedure
All patients had similar primary one-incision, arthroscopically assisted ACL reconstructions. A transtibial technique was utilized in all cases during the time period of the study. Tourniquet use was similar in all patients, and all surgeries were performed on an outpatient basis. Graft type was per patient choice following an informed discussion with the surgeon. Femoral nerve blocks were not utilized.
Post-operative rehabilitation
Patients in both groups were treated with identical rehabilitation protocols. Post-operative visit intervals were at 1, 2, 6 weeks with radiographs, 3 and 6 months. Patients were mobilized in a knee brace with crutches for 2 weeks with weight-bearing as tolerated and then progressed to discontinue the crutches and knee brace as quadriceps function returned. Early progressive range of motion and strengthening exercises were allowed as tolerated [45]. Jogging was initiated at 3–4 months, and the decision for return to sport was made based on strength and functional testing at a minimum of 6 months following ACL reconstruction.
Assessment of strength and function
Criteria for testing at 6 months included the absence of knee effusion, patellofemoral pain or pain with weight-bearing, a subjective sense of stability, and patient agreement to perform testing in that time frame. At 6 months following ACL reconstruction, isokinetic strength testing was performed with a Biodex machine (Biodex Medical Systems, Shirley, NY). A satisfactory outcome was defined as performing at least 85 % of the contralateral leg [11]. Functional testing involved performance of a vertical jump, single hop, and triple jump, which have demonstrated reliability as markers of functional outcomes after ACL reconstruction [20, 22, 34, 37], and a satisfactory outcome was defined as performing at least 90 % of the contralateral leg [34]. An “excellent” outcome at 6 months was defined as a satisfactory outcome in at least six of seven isokinetic strength and functional testing categories (excellent 6-month group). This category was representative of patients that were allowed to return to full activities. Patients who met these criteria were compared against the remaining group of patients who did not meet these criteria (delayed 6-month group).
This study was approved by the Institutional Review Board at our institution (Study number 10-7334).
Statistical analysis
The excellent 6-month group was compared to the delayed 6-month group in univariate analysis using two-sample t tests or Wilcoxon rank-sum tests as appropriate for continuous/ordinal variables and χ 2 tests for nominal variables. Multivariable models for the response of excellent functional and isokinetic outcomes at 6 months were created using logistic regression and are reported using odds ratios with 95 % confidence intervals and p values. Analysis was performed using JMP software (Version 7, SAS Institute, Inc., Cary, NC). All tests were two-sided, and p values <0.05 were considered statistically significant.
Results
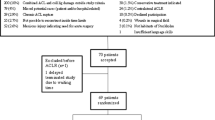
Three hundred eighty-eight patients were identified in the surgical database at our institution that had received ACL reconstruction performed by a single surgeon between 1998 and 2005. Of these patients, 224 met inclusion criteria (Fig. 1). The patients in this study included 93 males and 131 females. The median age at the time of surgery was 22 (range 12–59) years. The median BMI was 25.4 (range 17–44). There were three graft types used, including 134 bone-patellar tendon-bone (BTB) autografts (60 %), 62 BTB allografts (28 %), and 28 hamstring autografts (12 %). The median preinjury Tegner activity score was 6 (range 2–10).
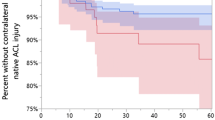
Functional and isokinetic testing was performed at a median of 182 (range 169–204) days post-operatively. Fifty-two patients (23 %) met the criteria for excellent 6-month functional and isokinetic results at 6 months, while 172 patients (77 %) were in the delayed 6-month group (Table 1). In univariate analysis, favourable factors for the excellent 6-month outcome group compared to the delayed 6-month group were younger age (24 vs. 27; p = 0.01), lower BMI (24.5 vs. 26.2; p = 0.03), and minimal articular cartilage (Outerbridge 1 or less) damage (71 vs. 56 %; p = 0.048). Although graft type overall was not found to be associated with outcome, patients older than 30 were more likely to do worse with autograft than with allograft (Fig. 2). Further analysis showed selection bias in that patients who received an allograft were significantly older (mean age 40 vs. 21 years) and had higher BMIs (mean 28 vs. 25; p < 0.0001). These findings are important because both older age and higher BMI were found to be associated with decreased odds of excellent 6-month outcome in univariate analysis and are thus potential confounders.
However, in multivariate analysis, younger age (OR 0.95 per one-year increase, p = 0.02) and lower BMI (OR 0.90 per 1-unit increase, p = 0.01) remained significantly associated with excellent 6-month outcome. Evaluation of each graft type based on age demonstrated no significant effect on outcomes of patients receiving allograft when considering the group as a whole; however, a significant negative effect was observed for autograft patients older than 30 years (p = 0.0004; Fig. 3).
Discussion
The most important finding of the present study was the correlation of patient characteristics, injury characteristics, and graft choice with early excellent functional results following ACL reconstruction. Wide variation in patient demographics and concomitant injuries makes it difficult to predict which patients will regain function and strength quickly following ACL reconstruction. To date, only anterior knee pain and preoperative activity level have been shown to demonstrate any significance as predictors of functional outcomes after these procedures [19], while others have been reported inadequate predictors [18, 26, 33, 41]. The purpose of this study was to assess patient concomitant injury and surgical factors for excellent 6-month functional and strength outcomes following ACL reconstruction. In this study, younger age, lower BMI, and minimal articular cartilage degeneration were significantly associated with excellent functional and isokinetic test results at 6 months following ACL reconstruction. Further, patients over 30 who underwent allograft reconstruction were more likely to demonstrate excellent 6-month results.
In this study, younger age was a significant predictor of early excellent isokinetic and functional scores after ACL reconstruction. Recently, Iriuchishima et al. [21] also reported that older age was a significant factor for weaker muscle strength following ACL reconstruction with either single-bundle or double-bundle reconstruction with hamstring autograft. Richardson et al. [38] assessed the effects of aging and also ACL reconstruction on quadriceps muscle weakness. They postulated that the common link between age-related loss of muscle fiber number and size, and loss of intraligamentous mechanoreceptors observed post-ACL reconstruction may be the gamma loop. They concluded that the gamma spindle system impairment with older age is possibly due to loss of mechanoreceptors or decreased muscle spindle sensitivity [38]. This may be a “double-hit” phenomenon in older patients undergoing ACL reconstruction, leading to more muscle weakness and delay in strength recovery following surgery. Kobayashi and colleagues assessed isokinetic strength testing and found that age itself did not affect muscle performance, but only that return of muscle strength was delayed in patients with anterior knee pain [24]. One recent study reported both lack of preoperative anterior knee pain and high level of function to be significant predictors of better outcomes after ACL reconstruction [19]. It may also be that anterior knee pain delays the return of quadriceps function due to inhibition following surgery and may surpass age in this setting.
In this study, patients older than 30 years were more likely to have excellent 6-month outcomes when allografts were used. Utilizing allograft avoids the post-operative morbidity associated with autograft harvest in terms of weakness in knee flexion [5, 9, 12, 15, 17, 23, 32, 42, 47], extension [9, 17, 31, 39, 40, 51], and internal/external rotation [2, 48]. This difference may also represent the decreased ability to compensate as patients age or the ability to participate in post-operative rehab sooner without the added morbidity. Moreover, donor site morbidity associated with harvest of autograft has been associated with post-operative weakness and deficit in knee flexion or extension (depending on graft chosen), which can persist as long as 2 years post-reconstruction or longer [5, 9, 12, 15, 17, 23, 31, 39, 42, 47]. A recent systematic review of Level III evidence demonstrated that muscle strength deficits were correlated with location of the donor site, with hamstring ACL grafts having weaker knee flexion and patellar tendon grafts having weaker knee extension [50]. It stands to reason then that allograft tissue, without donor site morbidity, would have better strength following ACL reconstruction. Use of allograft in ACL reconstruction has been associated with a relatively high rate of failure (7–13 %) compared with autograft rerupture rate. Based on these findings, allograft patients may be cleared “too early” while excellent early functional and strength testing, but the biologic incorporation and remodelling are delayed compared to autograft tissue [3]. This may contribute to the higher failure rate of allograft versus autograft ACL reconstruction, especially in higher-demand athletes.
Lower BMI was a significant predictive factor of early excellent return of strength and function following ACL reconstruction. Previously, Kowalchuk et al. assessed preoperative and intraoperative factors that predicted patient-oriented outcome following ACL reconstruction and found that BMI greater than 30 was a negative risk factor for an inferior IKDC score. Spindler et al. observed that weight gain greater than 7 kg resulted in worse Western Ontario and McMaster Universities Osteoarthritis Index and IKDC scores [46]. Additional previous studies have shown that a higher BMI at the time of reconstruction is predictive of meniscal damage, osteoarthritis, and medial chondrosis [6, 27, 29]. All of these findings may suggest that the increased weight places excessive stress on the knee, which may in the short term lead to a delayed recovery of strength and function, but may also accelerate the rate of degenerative changes in the long term.
In this study, less articular cartilage degeneration was associated with early return of strength and function. While osteoarthritis as a result of ACL reconstruction has been evaluated and shown to have no specific association with either autograft or allograft [28], the characteristics of the articular cartilage prior to ACL reconstruction have not been examined as a predictor for outcomes. In a longitudinal MRI study over 11 years, Potter et al. [36] found that each increase in the medial femoral condyle Outerbridge score resulted in a 13-point decrease in the International Knee Documentation Committee subjective knee score. Shelbourne also found that articular cartilage damage correlated with outcome following ACL reconstruction [44]. Only 67 or 76 % of patients undergoing ACL reconstruction using hamstring or bone-patellar tendon-bone autograft, respectively, return to preinjury activities post-operatively, and many of these athletes have cartilage injuries [4]. Brophy et al. [7] found that meniscus tears leading to cartilage injury may shorten playing careers, even when controlling for ACL reconstruction.
The main strength of the present study is that it is the first to demonstrate statistically significant predictors of early excellent functional and isokinetic outcomes after ACL reconstruction. There are several limitations to the present study. The first is that this study does not include any long-term follow-up. The study was designed specifically to assess early return of isokinetic strength and function, which led to return to play. This has been previously shown to correlate well with traditional knee scores [25], but further work needs to be done to determine how early 6-month outcome correlates with long-term outcome. Second, the statistically significant difference in BMI may not be clinically significant. Third, the study included a relatively small number of patients, and some of the subgroup analyses may have been affected by the limited number of patients in the excellent 6-month group. Despite these limitations, this manuscript helps to counsel patients on factors associated with early recovery of strength and function following ACL reconstruction and also may help in the decision of graft choice. This is clinically relevant as patients over the age of 30 desiring a quicker return of function may do better in this regard with allograft over autograft tissue.
Conclusion
In this study, factors significantly associated with excellent 6-month functional and isokinetic test results following ACL reconstruction included younger age, lower BMI, and minimal cartilage degeneration. The use of allograft was associated with improved excellent functional and strength testing after ACL reconstruction in patients over 30 years of age.
References
Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F (2004) Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am 86-A(10):2143–2155
Armour T, Forwell L, Litchfield R, Kirkley A, Amendola N, Fowler PJ (2004) Isokinetic evaluation of internal/external tibial rotation strength after the use of hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med 32(7):1639–1643
Bhatia S, Bell R, Frank RM, Rodeo SA, Bach BR Jr, Cole BJ, Chubinskaya S, Wang VM, Verma NN (2012) Bony incorporation of soft tissue anterior cruciate ligament grafts in an animal model: autograft versus allograft with low-dose gamma irradiation. Am J Sports Med 40(8):1789–1798
Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R (2007) ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res 458:180–187
Bizzini M, Gorelick M, Munzinger U, Drobny T (2006) Joint laxity and isokinetic thigh muscle strength characteristics after anterior cruciate ligament reconstruction: bone patellar tendon bone versus quadrupled hamstring autografts. Clin J Sport Med 16(1):4–9
Bowers AL, Spindler KP, McCarty EC, Arrigain S (2005) Height, weight, and BMI predict intra-articular injuries observed during ACL reconstruction: evaluation of 456 cases from a prospective ACL database. Clin J Sport Med 15(1):9–13
Brophy RH, Gill CS, Lyman S, Barnes RP, Rodeo SA, Warren RF (2009) Effect of anterior cruciate ligament reconstruction and meniscectomy on length of career in National Football League athletes: a case control study. Am J Sports Med 37(11):2102–2107
Cameron ML, Briggs KK, Steadman JR (2003) Reproducibility and reliability of the Outerbridge classification for grading chondral lesions of the knee arthroscopically. Am J Sports Med 31(1):83–86
Carter TR, Edinger S (1999) Isokinetic evaluation of anterior cruciate ligament reconstruction: hamstring versus patellar tendon. Arthroscopy 15(2):169–172
Cooley VJ, Deffner KT, Rosenberg TD (2001) Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. Arthroscopy 17(8):795–800
Daniel D, Malcolm L, Stone ML (1982) Quantification of knee stability and function. Contemp Orthop 5:83–92
Dauty M, Tortellier L, Rochcongar P (2005) Isokinetic and anterior cruciate ligament reconstruction with hamstrings or patella tendon graft: analysis of literature. Int J Sports Med 26(7):599–606
Duquin TR, Wind WM, Fineberg MS, Smolinski RJ, Buvea CM (2009) Current trends in ACL reconstruction. J Knee Surg 22(1):7–12
Edgar CM, Zimmer S, Kakar S, Jones H, Schepsis AA (2008) Prospective comparison of auto and allograft hamstring tendon constructs for ACL reconstruction. Clin Orthop Relat Res 466(9):2238–2246
Elmlinger BS, Nyland JA, Tillett ED (2006) Knee flexor function 2 years after anterior cruciate ligament reconstruction with semitendinosus-gracilis autografts. Arthroscopy 22(6):650–655
Frobell RB, Lohmander LS, Roos EM (2007) The challenge of recruiting patients with anterior cruciate ligament injury of the knee into a randomized clinical trial comparing surgical and non-surgical treatment. Contemp Clin Trials 28(3):295–302
Gobbi A, Mahajan S, Zanazzo M, Tuy B (2003) Patellar tendon versus quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a prospective clinical investigation in athletes. Arthroscopy 19(6):592–601
Goradia VK, Grana WA, Pearson SE (2006) Factors associated with decreased muscle strength after anterior cruciate ligament reconstruction with hamstring tendon grafts. Arthroscopy 22(1):80
Heijne A, Ang BO, Werner S (2008) Predictive factors for 12-month outcome after anterior cruciate ligament reconstruction. Scand J Med Sci Sports 19(6):842–849
Hopper DJ, Jaatinen E (2008) Optimizing modulation transfer spectroscopy signals for frequency locking in the presence of depleted saturating fields. Appl Opt 47(14):2574–2582
Iriuchishima T, Shirakura K, Horaguchi T, Wada N, Sohmiya M, Tazawa M, Fu FH (2012) Age as a predictor of residual muscle weakness after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20(1):173–178
Jarvela T, Kannus P, Latvala K, Jarvinen M (2002) Simple measurements in assessing muscle performance after an ACL reconstruction. Int J Sports Med 23(3):196–201
Keays SL, Bullock-Saxton J, Keays AC, Newcombe P (2001) Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee 8(3):229–234
Kobayashi A, Higuchi H, Terauchi M, Kobayashi F, Kimura M, Takagishi K (2004) Muscle performance after anterior cruciate ligament reconstruction. Int Orthop 28(1):48–51
Kong DH, Yang SJ, Ha JK, Jang SH, Seo JG, Kim JG (2012) Validation of functional performance tests after anterior cruciate ligament reconstruction. Knee Surg Relat Res 24(1):40–45
Kramer J, Nusca D, Fowler P, Webster-Bogaert S (1993) Knee flexor and extensor strength during concentric and eccentric muscle actions after anterior cruciate ligament reconstruction using the semitendinosus tendon and ligament augmentation device. Am J Sports Med 21(2):285–291
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med 36(7):1275–1282
Liden M, Sernert N, Rostgard-Christensen L, Kartus C, Ejerhed L (2008) Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy 24(8):899–908
Lohmander LS, Englund PM, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35(10):1756–1769
Markolf KL, Park S, Jackson SR, McAllister DR (2009) Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am 91(1):107–118
Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC 3rd (2002) Strength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. J Athl Train 37(3):262–268
O’Neill DB (1996) Arthroscopically assisted reconstruction of the anterior cruciate ligament. A prospective randomized analysis of three techniques. J Bone Joint Surg Am 78(6):803–813
Ott SM, Ireland ML, Ballantyne BT, Willson JD, McClay Davis IS (2003) Comparison of outcomes between males and females after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 11(2):75–80
Petschnig R, Baron R, Albrecht M (1998) The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 28(1):23–31
Poehling GG, Curl WW, Lee CA, Ginn TA, Rushing JT, Naughton MJ, Holden MB, Martin DF, Smith BP (2005) Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: allograft versus autograft. Arthroscopy 21(7):774–785
Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S (2012) Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med 40(2):276–285
Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR (2007) Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 87(3):337–349
Richardson MS, Cramer JT, Bemben DA, Shehab RL, Glover J, Bemben MG (2006) Effects of age and ACL reconstruction on quadriceps gamma loop function. J Geriatr Phys Ther 29(1):28–34
Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A (1999) Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 29(7):400–412
Rosenberg TD, Franklin JL, Baldwin GN, Nelson KA (1992) Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. Am J Sports Med 20 (5):519–525; discussion 525–516
Saupe N, White LM, Chiavaras MM, Essue J, Weller I, Kunz M, Hurtig M, Marks P (2008) Anterior cruciate ligament reconstruction grafts: MR imaging features at long-term follow-up–correlation with functional and clinical evaluation. Radiology 249(2):581–590
Segawa H, Omori G, Koga Y, Kameo T, Iida S, Tanaka M (2002) Rotational muscle strength of the limb after anterior cruciate ligament reconstruction using semitendinosus and gracilis tendon. Arthroscopy 18(2):177–182
Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ (2010) Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med 38(11):2233–2239
Shelbourne KD, Gray T (2000) Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med 28(4):446–452
Shelbourne KD, Nitz P (1990) Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med 18(3):292–299
Spindler KP, Warren TA, Callison JC Jr, Secic M, Fleisch SB, Wright RW (2005) Clinical outcome at a minimum of five years after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am 87(8):1673–1679
Tadokoro K, Matsui N, Yagi M, Kuroda R, Kurosaka M, Yoshiya S (2004) Evaluation of hamstring strength and tendon regrowth after harvesting for anterior cruciate ligament reconstruction. Am J Sports Med 32(7):1644–1650
Torry MR, Decker MJ, Jockel JR, Viola R, Sterett WI, Steadman JR (2004) Comparison of tibial rotation strength in patients’ status after anterior cruciate ligament reconstruction with hamstring versus patellar tendon autografts. Clin J Sport Med 14(6):325–331
Tow BP, Chang PC, Mitra AK, Tay BK, Wong MC (2005) Comparing 2-year outcomes of anterior cruciate ligament reconstruction using either patella-tendon or semitendinosus-tendon autografts: a non-randomised prospective study. J Orthop Surg (Hong Kong) 13(2):139–146
Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD (2011) The influence of graft choice on isokinetic muscle strength 4–24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19(5):768–780
Yasuda K, Ohkoshi Y, Tanabe Y, Kaneda K (1992) Quantitative evaluation of knee instability and muscle strength after anterior cruciate ligament reconstruction using patellar and quadriceps tendon. Am J Sports Med 20(4):471–475
Acknowledgment
We would like to acknowledge Jessica Ruff for contributions to data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krych, A.J., Woodcock, J.A., Morgan, J.A. et al. Factors associated with excellent 6-month functional and isokinetic test results following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 23, 1053–1059 (2015). https://doi.org/10.1007/s00167-014-2869-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-2869-9