Abstract
Purpose
To evaluate the long-term clinical, patient-reported and radiological outcome of patients reconstructed for anterior cruciate ligament (ACL) insufficiency. We wanted to examine the relationship between clinical findings and patient-reported scores.
Methods
The 96 first successive patients that underwent ACL reconstruction using transtibial technique, hamstrings autograft and tunnel placement ad modum Howell were evaluated 10 years post-operatively. Subjective outcomes were Lysholm score, IKDC 2000 subjective score and Tegner activity scale. The clinical examination included evaluation of rotational and sagittal laxity. Evaluation of osteoarthritis was done radiologically.
Results
Eighty-three patients (86 %) were available for follow-up at mean 10.2 years post-operatively. Three patients had revision ACL surgery prior to the 10-year evaluation. The mean Lysholm score, subjective IKDC 2000 score and Tegner activity scale were 89 (SD 13), 83 (SD 15) and 5 (range, 3–9), respectively. Six patients (8 %) had moderate or severe osteoarthritis. Eighty-six per cent of patients had normal or near-normal anterior–posterior ACL laxity. Twenty per cent of patients had positive pivot shift and 42 % had a pivot glide. The former group had a significant lower Lysholm score compared to the rest of the patients.
Conclusions
Although the mean Lysholm score was classified as good (89) at the 10-year follow-up, a positive pivot shift was found in 20 % of these patients. Compared to patients with normal rotational laxity or pivot glide, this patient group reported significant lower subjective satisfaction at the long-term follow-up.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction is regarded as a successful surgical intervention and is one of the most common procedures in sports medicine [7, 13]. The choice of graft, method of fixation and surgical technique has been under constant evolution the last decade [11, 12, 15, 23, 24, 38, 40]. The recent debate has been focusing on the “anatomical” placement of the femoral and tibial graft tunnels [5, 24, 44]. Biomechanical and cadaver studies have provided information about important properties of the ACL [28, 39, 42, 44], and a restoration of the native anatomy and function of the ACL has been emphasised.
The transtibial approach, which gained popularity in the 1990s, utilises a technique where the femoral tunnel is created via a pre-drilled tibial tunnel. The transtibial reaming of the femoral tunnel is predetermined by the placement of the tibial tunnel, and recent studies have shown that this technique tends to place the graft tunnel outside the native femoral footprint of the ACL [22, 24, 40]. Even so, long-term evaluations of these techniques have shown good results [1, 11, 15, 31].
The current study evaluates the long-term outcome after ACL reconstruction ad modum Howell using hamstrings autograft, the 70° tibial guide and transtibial drilling of the femoral tunnel. The 70° tibial guide was developed to standardise the placement of the femoral tunnel at 70° in the coronal plane. This was achieved with the locking of the tip of the guide against the femoral roof in full extension and adjustment of the coronal angle by a horizontal alignment rod. There are only a few studies evaluating the outcomes after reconstructions using this technique [11, 17], and only one study with medium- to long-term evaluation [11]. The hypothesis of this study was that good long-term results and a high degree of patient satisfaction can be found after using this technique. The aims were to establish what kind of clinical findings that could be related to inferior subjective scores and to identify potential early predictors of the long-term outcome.
Materials and methods
All patients were invited in writing to participate in a clinical follow-up examination. They completed a Lysholm reporting form, the subjective part of the IKDC 2000 and Tegner forms without the involvement of the examiner. Data from the surgery were collected from an internal prospectively registered ACL database. From the routine post-operative evaluations, we used the 12-month Lysholm score or 24-month score (if the former was not available), in a variable called the “early Lysholm score.” The regional ethical review board (Regional Etisk Komite: ID REK3366) approved the study. All patients gave their informed written consent prior to participating in the study.
Patient selection
All patients that underwent ACL reconstruction in the period 1999–2001, with the use of the later described method, were eligible for inclusion in the study. Exclusion criteria were revision surgery (n = 14), reconstruction with a different technique (e.g. patellar tendon grafts) or if the ACL reconstruction was combined with other knee ligament surgery (n = 48).
Radiographic evaluation
Patients were examined with standardised weight-bearing AP radiographs of both knees in 30° of flexion. Lateral radiographs were taken with the knee in full extension. All images were graded for OA according to the IKDC 2000 classification into 1 out of 4 groups (A through to D, with D representing most severe OA) [45]. An experienced orthopaedic radiologist assessed and classified the OA.
Surgical procedure
Following an initial arthroscopic examination, the semitendinosus and gracilis tendons were harvested through a longitudinal medial incision. The tibial tunnel was drilled with the knee in full extension using a 70° tibial guide (Howell tibial guide, Arthrotek Inc., Warsaw, IN, USA) [18, 25]. Depending on the graft size, a 7-, 8- or 9-mm reamer was used. An impingement rod (Arthrotek Inc., Warsaw, IN, USA) was used to avoid the femoral roof to impinge on the graft with the knee in full extension. A moderate notchplasty was performed in all knees. The femoral tunnel was drilled aided by size-specific femoral aimers (Arthrotek Inc., Warsaw, IN, USA) placed through the tibial tunnel with the knee held at a flexion angle of about 70–80°.
An additional femoral U-guide (Arthrotek Inc., Warsaw, IN, USA) was used to ream a transverse tunnel for the femoral graft fixation. Femoral fixation of the graft was done with the Bone Mulch screw (Biomet, Warsaw, IN, USA).
The knee was repeatedly extended and flexed to allow stress relaxation of the graft. A moderate tension load was applied to the graft while the ends were fixed outside the tibial tunnel with both a multi-spiked WasherLoc (Biomet, Warsaw, IN, USA) and a compression screw. The knee was held in full extension during fixation. Finally, the graft was assessed arthroscopically and the stability was tested clinically.
Rehabilitation
During the first 2–3 days, an Aircast Knee Cryo/Cuff (DJO, CA, USA) was applied to reduce pain and swelling. Compression stockings were used as DVT prophylaxis. Patients were weight bearing as tolerated from the first post-operative day. Instructions were given in closed kinetic chain exercises. Six weeks post-operatively, patients were allowed light non-pivoting exercise like jogging. At 6 months, the patients could freely return to normal activity levels without any restrictions.
Post-operative follow-up at 10 years
A clinician not involved in patient treatment performed clinical follow-up assessments. Physician-assessed Lysholm score was completed, and a clinical examination was undertaken. Knee range of motion (ROM) was measured using a goniometer and classified according to IKDC criteria [45].
The anterior laxity was examined in both knees with a KT-1000 device (MEDmetric, CA, USA) at 15, 20, 30 lb and with max manual force. The max manual force difference between injured and normal (I–N) was calculated and used for analysis. The flexion-rotation drawer test (FRD), as described by Noyes, was used for the assessment of anterolateral rotational instability (ALRI) [30]. If muscular guarding prevented accurate classification of ALRI, the result was registered as “not gradable.”
Statistical analysis
All statistical calculations were done with the SPSS 19.0 (SPSS Inc., Chicago, IL, USA). The a priori significance level was set at 0.05. For the descriptive analysis, we calculated mean, range, standard deviation (SD) and frequency distribution. A two-tailed paired t test was used to compare repeated data from the same patient. A two-tailed unpaired t test was used to test for differences in mean between groups defined in this study. ANOVA analysis was used for the comparison of equality of the mean values between these groups.
The linear relationship between the Lysholm score, at 10 years post-operatively, and age, sex, Tegner activity score before injury, smoking status, weight and Lysholm score at 1–2 years were examined with bivariate correlations. Chi-square statistics were used to test for differences in frequency of osteoarthritis in patients grouped according to meniscal surgery at time of reconstruction and presence of rotational instability at the follow-up.
Results
Eighty-three patients (86 % of those eligible), 47 males and 36 females, completed our follow-up investigations (Fig. 1); demographic data are presented in Table 1.
Concomitant surgery
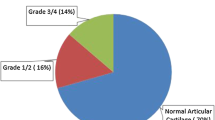
At the time of surgery, concomitant or former partial meniscal resection was performed or found to have been performed in 29 patients on the medial side and 18 on the lateral side. Suture repairs of longitudinal meniscal tear were done medially in four patients and laterally in one patient. In total, 30 patients (38 %) had no meniscal pathology and 63 (79 %) patients had normal articular cartilage.
Secondary operations
During the 10-year follow-up period, 12 patients had additional surgery to the same knee. Three patients had a revision of the ACL at a median time of 74 months (range, 11–133 months). Two patients had hardware removed. Four patients had a meniscal resection. The rest underwent a second-look arthroscopy due to various symptoms.
Clinical outcome
At the 10-year follow-up, the mean Lysholm score, obtained by an interview (88.9, SD 13.1), was significantly higher than the patient-reported Lysholm (87.4, SD 11.3, P = 0.01). We found a high linear correlation between the two Lysholm scores (R = 0.80, P = 0.00). IKDC subjective scores had a mean value of 83.3 (SD 14.9).
There was no significant difference (n.s.) between the mean patient-reported Lysholm score at the 10-year follow-up and the early Lysholm scores obtained at 12 months and 2 years in 49 patients (85.1, SD 13.7).
The results from Lachman, KT-1000 and pivot shift testing are presented in Table 2. Flexion deficits and extension deficits are presented according to IKDC criteria (Table 2) [41]. ANOVA testing showed a significant difference in the mean Lysholm scores between patients with 0, 1+ and 2+ pivot shift (P = 0.01). The mean Lysholm scores in these groups were, respectively, 92, 87 and 79. When doing post hoc pairwise Bonferroni comparisons, patients with 2+ pivot shift had significant lower scores than those with no pivot shift (P = 0.03). Patients with 1+ pivot shift did, however, not differ significantly in scores from the other two groups.
Of those patients who were eligible in the study but did not participate (n = 13), 2 patients had a KT-1000 I–N difference ≥5 mm as recorded from the 12- or 24-month routine follow-up. None of the other patients had clinical or radiological signs of graft failure as we know of.
Osteoarthritis
Both knees were examined for osteoarthritis (Table 3). There were significant more OA in patients that had a meniscal resection at the time of the ACL reconstruction (P = 0.05). Comparing patients with 2+ pivot shift at the follow-up and patients with pivot glide or a stable knee, we found no significant difference (P = 0.47) in the incidence of OA.
Early predictors of long-term outcome
A moderate linear correlation was found between the Lysholm score at the last follow-up and the Lysholm score at 1–2 years (R = 0.44, P < 0.00). A weak correlation was found between the Lysholm score at follow-up and the age of the patient at the time of the surgery (R = 0.23, P = 0.05). There was a significant difference in Lysholm score at 10 years depending on which knee was reconstructed: 89 (SD 9.7) for left knees and 82 (SD 14.8) for right knees (P = 0.03). No significant correlations were found between the Lysholm score at the last follow-up and smoking, meniscal resection, pre-injury Tegner score and overweight. When comparing 2+ pivot shift in patient who had undergone meniscal surgery compared to those with no meniscal surgery, no significant difference was found between these groups (n.s.).
Discussion
The most important finding in this study was the high incidence of rotational instability. The patients with a 2+ pivot shift had significant lower Lysholm and IKDC subjective scores as compared to the rest of the patients. Patients with 1+ pivot glide, however, had no different scores than those who were classified as having no rotational laxity. Existing short- to mid-term follow-up studies report considerable variation in rotational instability after similar operative techniques. Gorschewsky et al. [12] found “positive pivot shift” in 15 % when evaluating ACL reconstructed patients 6 years post-operatively. In a study by Ibrahim et al. [21], a pivot glide was found in 12.5 %, while the rest of the patients had a stable knee. Kleipool et al. [23] reported pivot glide in 23 % and 2+ pivot shift in 3.8 % of ACL reconstruction patients at the 4-year follow-up examination. Hussein et al. [20] randomised the patients to one out of three techniques of ACL reconstruction [transtibial single bundle (CSB), anatomical single bundle (ASB) and anatomical double bundle (ADB)]. In the transtibial group, they found pivot glide in as many as 48 %, while 2+ pivot shift was found in 10 % of the patients. This was significantly more than in the other two groups. The mean follow-up time in this study was 4.3 years. Gifstad et al. [11] reported on outcomes on patients reconstructed with the same technique as this present study, but with a 7-year follow-up. They presented data on anterior–posterior laxity, but did not evaluate the pivot shift.
When comparing the mean subjective scores (Lysholm, IKDC) between the groups with 0, 1+ and 2+ pivot shift, we found a significant lower mean score in those with 2+ pivot shift. These results are not surprising since the main goal of ACL reconstruction is to restore the stability of the knee. Instability and “giving way” is one of the main complaints of ACL-deficient patients [4, 26, 41]. Somewhat surprising was the finding of no significant difference in the reported subjective IKDC (n.s.) and Lysholm scores (n.s.) between patients with 1+ pivot shift (pivot glide) and those with no rotational instability.
A variety of techniques are described for evaluating the rotational instability. A high inter-rater variability in performing clinical tests and grading the test results is believed to be present [2, 16, 29]. The lack of standardisation makes the comparison across studies difficult. In the present study, we used the FRD test as described by Noyes [30]. In the original publication by Noyes, he claims the FRD test to be more sensitive in detecting subtle rotational instabilities, compared to “the lateral pivot shift” as described by Galway and MacIntosh [9]. This might be one explanation why we found a high incidence of pivot glide in our patients.
Patients with muscular guarding can be a problem when classifying rotational instability [2]. It was not possible to correctly grade rotational instability in eight (10.5 %) of the examined patients in our study, due to muscular defence. In the statistical analysis, we had to exclude these patients.
There are a growing number of studies on possible shortcomings of ACL reconstruction using a transtibial drilling of the femoral tunnel [5, 14, 36, 37, 40, 43]. The difficulty of reproducing an anatomical insertion of the ACL graft is the main limitation of the coupled drilling technique; the result is a non-anatomical placement of the femoral burr tunnel above the native insertion of the ACL [32, 34]. A vertical orientation of the ACL graft can explain the increase in rotational instability with this technique [20, 32]. Our follow-up findings of a high degree of ALRI confirm the persistence of rotational instability in patients reconstructed with the transtibial drilling technique. The original 70° tibial guide used in this study was later redesigned to a 65° coronal guide due to findings of increased graft tensions at steep coronal angles [35]. This was thought to be caused by the impingement of ACL onto PCL, thus causing graft failure.
Briggs et al. [6] validated the Lysholm score for the use as a self-reporting questionnaire. The original Lysholm score was based on physicians filling out the questionnaire. We used both self-reporting and physician-reported Lysholm scores. At the 10-year follow-up, the mean Lysholm score obtained by an interview (88.9, SD 13.0) was significantly higher than the self-reporting Lysholm score (87.4, SD 11.3, P = 0.01). However, the difference was small (1.5 points) and the clinical significance is debatable. We found a high linear correlation between the self-reporting and physician-reported Lysholm scores (R = 0.80, P = 0.00). This contradicts the findings of Briggs et al. [6].
When examining the bivariate correlations between Lysholm score and multiple pre- and per-operative factors, we found no relation between meniscal resection and the subjective scoring at the follow-up. This is in contrast to Shelbourne who found meniscal surgery as a significant factor explaining variation in the subjective score [33]. We believe that 10 years post-operatively is a bit early in evaluating the effect of meniscectomy on development of osteoarthritis. Also, we are not sure if the sample size is large enough to detect subtle differences in the subjective scores.
There is only one other study that reports on mid- to long-term results using the same surgical technique [11]. This study reported a mean Lysholm score of 91 at the 7-year follow-up. There was no significant change in the Lysholm scores from the early (1- and 2-year) evaluations to the 7-year follow-up. Our findings support these results. In the randomised study by Hussein et al. [20], the mean Lysholm scores were 91, 92 and 93, respectively, in the CSB, ASB and ADB groups. There was a statistically significant difference between the CSB and ADB group (P = 0.03), though hardly of clinical importance. The IKDC subjective scores for the same groups were 90, 91 and 92. Other studies with similar length follow-up [3, 8, 10, 15, 27] report mean Lysholm scores in the range 84–96. When comparing the results in these studies to the mean subjective scores in our patient group, we have found good, but not excellent results. A surprising finding, when examining pre-operative factors predicting the long-term Lysholm score, was the significant higher mean value in those with a left-sided ACL reconstruction. We have currently no explanation for this difference.
The strengths of this study include using an independent examiner at the clinical follow-up reducing the possible bias that occurs when a surgeon examines his own patients [19] and a high follow-up rate of 86 %. The most important limitations of our study include a retrospective design, the lack of a control group and the inclusion of patients operated upon by several different surgeons. The latter gives rise to an inter-surgeon variability that could to some extent be corrected for by statistical stratification. Due to the relatively small number of patients in the study, we have not undertaken such an analysis. Although they were experienced surgeons, this was early in the learning curve of this method, and one could perhaps expect improved results over time.
The clinical relevance of this study relates to the importance of the restoration of rotational stability after an ACL rupture. The “giving way” typically experienced by patients where pivot shift is persistent after reconstruction is probably one of the main reasons for inferior subjective scores. This knowledge should point to the importance of restoring native biomechanical properties when choosing method for surgical reconstruction.
Conclusion
At 10 years post-operatively, most of the patients with ACL reconstruction using hamstrings autograft, the 70° tibial guide and transtibial femoral tunnel placement have both satisfactory clinical and self-reported outcomes. The outcomes are comparable to those described for similar techniques. There was a low incidence of radiographic OA, and few had restrictions in ROM. A high incidence of 1+ and 2+ pivot shift adds to the critique of the transtibial drilling of the femoral tunnel. The positive pivot shift was correlated to significantly lower Lysholm and IKDC subjective scores.
References
Alentorn-Geli E, Lajara F, Samitier G, Cugat R (2009) The transtibial versus the anteromedial portal technique in the arthroscopic bone-patellar tendon-bone anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18:1013–1037
Anderson AF, Rennirt GW, Standeffer WC (2000) Clinical analysis of the pivot shift tests: description of the pivot drawer test. Am J Sports Med 13:19–24
Apostolopoulos A, Nakos A, Nikolopoulos D, Theofanopoulos F, Liarokapis S, Mihos I (2009) Anterior cruciate ligament reconstruction with hamstring tendon autografts. EEXOT 60:48–52
Arbes S, Resinger C, Vécsei V, Nau T (2006) The functional outcome of total tears of the anterior cruciate ligament (ACL) in the skeletally immature patient. Int Orthop 31:471–475
Bedi A, Musahl V, Steuber V et al (2011) Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy 27:380–390
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37:890–897
Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AHS (2012) Incidence and risk factors for injuries to the anterior cruciate ligament in National Collegiate Athletic Association football: data from the 2004–2005 through 2008–2009 National Collegiate Athletic Association Injury Surveillance System. Am J Sports Med 40:990–995
Ferretti A, Monaco E, Giannetti S, Caperna L, Luzon D, Conteduca F (2010) A medium to long-term follow-up of ACL reconstruction using double gracilis and semitendinosus grafts. Knee Surg Sports Traumatol Arthrosc 19:473–478
Galway HR, MacIntosh DL (1980) The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 147:45–50
Gerhard P, Bolt R, Dück K, Mayer R, Friederich NF, Hirschmann MT (2012) Long-term results of arthroscopically assisted anatomical single-bundle anterior cruciate ligament reconstruction using patellar tendon autograft: are there any predictors for the development of osteoarthritis? Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2001-y
Gifstad T, Sole A, Strand T, Uppheim G, Grøntvedt T, Drogset JO (2012) Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-1947-0
Gorschewsky O (2005) Clinical comparison of the tutoplast allograft and autologous patellar tendon (bone-patellar tendon-bone) for the reconstruction of the anterior cruciate ligament: 2- and 6-year results. Am J Sports Med 33:1202–1209
Granan LP, Forssblad M, Lind M, Engebretsen L (2009) The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop 80:563–567
Heming JF, Rand J, Steiner ME (2007) Anatomical limitations of transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med 35:1708–1715
Holm I, Oiestad BE, Risberg MA, Aune AK (2010) No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med 38:448–454
Hoshino Y, Araujo P, Ahlden M et al (2011) Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc 20:732–736
Howell SM, Gittins ME, Gottlieb JE, Traina SM, Zoellner TM (2001) The relationship between the angle of the tibial tunnel in the coronal plane and loss of flexion and anterior laxity after anterior cruciate ligament reconstruction. Am J Sports Med 29:567–574
Howell SM, Wallace MP, Hull ML, Deutsch ML (1999) Evaluation of the single-incision arthroscopic technique for anterior cruciate ligament replacement. A study of tibial tunnel placement, intraoperative graft tension, and stability. Am J Sports Med 27:284–293
Höher J, Bach T, Münster A, Bouillon B, Tiling T (1997) Does the mode of data collection change results in a subjective knee score? Self-administration versus interview. Am J Sports Med 25:642–647
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 40:512–520
Ibrahim SA-R, Al-Kussary IM, Al-Misfer ARK, Al-Mutairi HQ, Ghafar SA, El Noor TA (2005) Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy 21:412–417
Kaseta MK, DeFrate LE, Charnock BL, Sullivan RT, Garrett WE Jr (2008) Reconstruction technique affects femoral tunnel placement in ACL reconstruction. Clin Orthop Rel Res 466:1467–1474
Kleipool A, Zijl J, Willems WJ (1998) Arthroscopic anterior cruciate ligament reconstruction with bone-patellar tendon-bone allograft or autograft. A prospective study with an average follow up of 4 years. Knee Surg Sports Traumatol Arthrosc 6:224–230
Larson AI, Bullock DP, Pevny T (2012) Comparison of 4 femoral tunnel drilling techniques in anterior cruciate ligament reconstruction. Arthroscopy 28:972–979
Lawhorn KW, Howell SM (2003) Scientific justification and technique for anterior cruciate ligament reconstruction using autogenous and allogeneic soft-tissue grafts. Orthop Clin North Am 34:19–30
Melnyk M, Faist M, Gothner M, Claes L, Friemert B (2007) Changes in stretch reflex excitability are related to “giving way” symptoms in patients with anterior cruciate ligament rupture. J Neurophysiol 97:474–480
Murray JRD, Lindh AM, Hogan NA et al (2012) Does anterior cruciate ligament reconstruction lead to degenerative disease? Thirteen-year results after bone-patellar tendon-bone autograft. Am J Sports Med 40:404–413
Musahl V (2005) Varying femoral tunnels between the anatomical footprint and isometric positions: effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med 33:712–718
Musahl V, Hoshino Y, Ahlden M et al (2012) The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc 20:724–731
Noyes FR, Bassett RW, Grood ES, Butler DL (1980) Arthroscopy in acute traumatic hemarthrosis of the knee. J Bone Jt Surg 62:687–695
Oiestad BE, Holm I, Aune AK et al (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38:2201–2210
Scanlan SF, Lai J, Donahue JP, Andriacchi TP (2011) Variations in the three-dimensional location and orientation of the ACL in healthy subjects relative to patients after transtibial ACL reconstruction. J Orthop Res 30:910–918
Shelbourne KD, Gray T (2009) Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med 37:471–480
Silva A, Sampaio R, Pinto E (2011) ACL reconstruction: comparison between transtibial and anteromedial portal techniques. Knee Surg Sports Traumatol Arthrosc 20:896–903
Simmons R, Howell SM, Hull ML (2003) Effect of the angle of the femoral and tibial tunnels in the coronal plane and incremental excision of the posterior cruciate ligament on tension of an anterior cruciate ligament graft: an in vitro study. J Bone Jt Surg 85:1018–1029
Steiner ME (2009) Independent drilling of tibial and femoral tunnels in anterior cruciate ligament reconstruction. J Knee Surg 22:171–176
Strauss EJ, Barker JU, McGill K, Cole BJ, Bach BR, Verma NN (2011) Can anatomic femoral tunnel placement be achieved using a transtibial technique for hamstring anterior cruciate ligament reconstruction? Am J Sports Med 39:1263–1269
Sujay DK, Khan WS, Rohit S (2012) Anterior cruciate ligament graft choices: a review of current concepts. Open Orthop J 6:281–286
Tashman S, Kopf S, Fu FH (2008) The kinematic basis of anterior cruciate ligament reconstruction. Oper Tech Sports Med 16:116–118
Tompkins M, Milewski MD, Brockmeier SF, Gaskin CM, Hart JM, Miller MD (2012) Anatomic femoral tunnel drilling in anterior cruciate ligament reconstruction: use of an accessory medial portal versus traditional transtibial drilling. Am J Sports Med 40:1313–1321
Wagemakers HP, Luijsterburg PA, Boks SS et al (2010) Diagnostic accuracy of history taking and physical examination for assessing anterior cruciate ligament lesions of the knee in primary care. Arch Phys Med Rehabil 91:1452–1459
Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler HH (2011) Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy 27:653–665
Xu Y, Ao Y, Wang J, Yu J, Cui G (2011) Relation of tunnel enlargement and tunnel placement after single-bundle anterior cruciate ligament reconstruction. Arthroscopy 27:923–932
Zantop T, Kubo S, Petersen W, Musahl V, Fu FH (2007) Current techniques in anatomic anterior cruciate ligament reconstruction. Arthroscopy 23:938–947
International Knee Documentation Committee (2000). IKDC forms available at: http://www.sportsmed.org/research/IKDC_forms
Conflict of interest
No conflict of interest reported from any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inderhaug, E., Strand, T., Fischer-Bredenbeck, C. et al. Long-term results after reconstruction of the ACL with hamstrings autograft and transtibial femoral drilling. Knee Surg Sports Traumatol Arthrosc 21, 2004–2010 (2013). https://doi.org/10.1007/s00167-012-2330-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2330-x