Abstract
Purpose
The transepicondylar axis (TEA) has been used as a flexion axis of the knee and a reference of the rotational alignment of the femoral component. However, no study has showed dynamic normal knee kinematics employing TEA as the evaluation parameter throughout the full range of motion in vivo. The purpose of this study was to analyze dynamic kinematics of the normal knee through the full range of motion via the 3-dimensional to 2-dimensional registration technique employing TEA as the evaluation parameter.
Methods
Dynamic motion of the right knee was analyzed in 20 healthy volunteers (10 female, 10 male; mean age 37.2 years). Knee motion was observed as subjects squatted from standing with knee fully extended to maximum flexion. The following parameters were determined: (1) Anteroposterior translations of the medial and lateral ends of the TEA; and (2) changes in the angle of the TEA on the tibial axial plane (rotation angle).
Results
The medial end of the TEA demonstrated anterior translation (3.6 ± 3.0 mm) from full extension to 30° flexion and demonstrated posterior translation (18.1 ± 3.7 mm) after 30°, while the lateral end of the TEA demonstrated consistent posterior translation (31.1 ± 7.3 mm) throughout knee flexion. All subjects exhibited femoral external rotation (16.9 ± 6.2°) relative to the tibia throughout knee flexion.
Conclusion
Compared to previously used parameters, the TEA showed bicondylar posterior translation from early flexion phase. These results provide control data for dynamic kinematic analyses of pathologic knees in the future and will be useful in the design of total knee prostheses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Motion analyses of normal knees provide references for analyzing pathologic knees as in cases of osteoarthritis or ligament injury. Additionally, these analyses could prove useful in the design of total knee prostheses. To describe normal knee motion, methods employing anatomically defined axes at the femur have been utilized in many previous studies.
The transepicondylar axis (TEA) is a line connecting medial and lateral femoral epicondyles and has been used as a flexion axis of the knee [3, 5, 6, 8] and reference of the rotational alignment of the femoral component [1, 4, 16, 17, 19, 21, 27] of total knee arthroplasty (TKA). The goal of TKA is now not only to treat pain, but also to restore function that is more similar to the normal knee. In this situation, it is important to evaluate the normal knee kinematics using TEA to understand that movement throughout the full range of motion. This will be useful data for designing a TKA to restore function, especially for regaining deep flexion by TKA.
Some studies have shown normal knee kinematics using cadavers and employing TEA as an evaluation parameter [5, 7, 15]. Then, Kozanek et al. [12] reported in vivo dynamic normal knee gait analysis employing TEA. However, no study to date has studied in vivo dynamic normal knee kinematics employing TEA as an evaluation parameter throughout the full range of motion.
Other studies have shown in vivo dynamic kinematics of the normal knee through the wide range of motion [11, 14, 23]. These studies employed the contact-point or Geometric center axis (GCA) as an evaluation parameter. However, there is a possibility that similar movement is not seen if TEA is employed as an evaluation parameter in vivo dynamic knee kinematics as cadaver studies have shown a different movement between the TEA and the GCA [15].
The purpose of this study was to analyze in vivo dynamic kinematics of the normal knee through the full range of motion via the 3D-to-2D registration technique [2, 3, 10–12, 14, 15, 23, 26] employing TEA as an evaluation parameter, and to compare the results with previous reports employing GCA as an evaluation parameter.
It is hypothesized that if a different axis is used to evaluate in vivo dynamic kinematics of normal knees, different motion may be observed, even if these result from the same knee motions.
Materials and methods
20 healthy volunteers (10 male, 10 female) with no knee-related symptoms (pain, instability, click, locking, or limited range of motion), history of major trauma, or obvious deformity in the lower extremities participated in this study. The mean age was 37.2 years (range 24–61 years).
This study was performed according to the protocol approved by the Investigational Review Board of our institutions. All subjects provided informed consent to participate in this study.
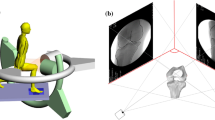
Motion of the right knee was analyzed in all subjects. Computed tomography (CT) (SOMATOM® Sensation 16; Siemens, Munich, Germany) of the femur and tibia was obtained for each subject, with a 1-mm interval. A 3D digital model of the femur and tibia was constructed from CT data using 3D visualization and modeling software (ZedView®; LEXI, Tokyo, Japan) and the anatomic coordinate systems were established referencing several bony landmarks [20]. The tibial Z-axis was defined by a line connecting the midpoint of the tibial eminence and the midpoint of the medial and lateral tops of the talar dome. The tibial Y-axis (positive anteriorly) was defined as a line drawn perpendicularly from the medio-lateral center of the insertion of the posterior cruciate ligament to the Z-axis. The tibial X-axis was defined as the cross product of the Z-axis and Y-axis. The XY plane in this coordinate system was defined as the tibial axial plane (Fig. 1).
Knee motion was observed as subjects squatted from a standing position (knee fully extended to maximum flexion) and was recorded via a flat panel detector (AXIOM Artis® dTA; Siemens). All subjects stood with their feet in a comfortable rotation position (neutral rotation). The sampling frequency was 15 Hz, with an image area of 380 × 300 mm and resolution of 1,240 × 960 pixels. The mean duration of one flexion of the knee was 8.4 s. The mean angular velocity and sampling rate were 17.2 degrees/second and 1.2 images/degree of knee flexion, respectively. The series of static lateral images were stored digitally. After the contours of the femur and tibia were manually detected in these images, a 3D-to-2D technique using an automated shape-matching algorithm was employed to determine the relative 3D positions of the femur and tibia in each fluoroscopic image (KneeMotion®; LEXI, Tokyo, Japan) (Fig. 2). By performing this procedure for all images, relative motion between the femur and tibia could be obtained. The root mean square error (RMSE) was 0.3–0.8 mm for in-plane translation, 2.2 mm for out-of-plane translation, and 0.2°–0.6° for rotation [10, 23].
Relative motion between the femur and tibia was quantified as the movement of TEA projected onto the axial (XY) plane of the tibial coordinate system. Since the medial sulcus is not always detected [22, 24, 27], we used clinical (or anatomical) TEA, which connects the prominent points of medial and lateral femoral epicondyles, as the evaluation parameter (Fig. 3). We also set the medial and lateral prominence in separate slices because the bony landmarks are not always present in one slice [22].
We determined the following parameters: (1) Anteroposterior (AP) translations of the medial and lateral ends of the TEA; and (2) changes in the angle of the TEA on the tibial axial plane (rotation angle). AP locations of the medial and lateral ends of all projected TEAs were evaluated as Y values of the tibial coordinate system (Fig. 4).
To examine the reproducibility of knee motion patterns, changes to the angle of the TEA (rotation angle) and AP translations of the medial and lateral ends of the TEA, three subjects in this series were chosen for examination on two different days. At the time of the second examination, all subjects were asked to repeat the activities of the first examination while being recorded and examined using the same techniques. The intra-observer reproducibility of our parameters was then examined via intra-class correlation coefficient (ICC). The mean and maximum differences in rotation angle of TEA between the two examinations were 1.7° and 3.0°, respectively. The mean and maximum differences in total AP translation of the medial and lateral ends of the TEA were 3.5 and 6.6 mm (medial) and 2.2 and 2.9 mm (lateral), respectively. The ICC of the TEA rotation angle, AP translation of the medial end of the TEA, and that of the lateral end of the TEA were 0.98, 0.91, and 0.85, respectively. The inter-observer errors were also examined. Two observers analyzed five subjects in this series. The mean and maximum differences in rotation angle of TEA between the two examinations were 2.6° and 3°, respectively. The mean and maximum differences in total AP translation of the medial and lateral ends of the TEA between two examinations were 1.5 and 4.6 mm (medial), and 0.8 and 2.2 mm (lateral), respectively. The ICC of the TEA rotation angle, AP translation of the medial end of the TEA, and AP translation of the lateral end of the TEA were 0.92, 0.86, and 0.99, respectively.
Statistical analysis
All data is expressed as mean ± SD. The difference between changes in the angle of the TEA on the tibial axial plane (rotation angle) and those of the GCA were obtained by a previous study using Student’s t test with a significance level of P < 0.05.
Results
AP translations of the medial and lateral ends of the TEA
With regard to these parameters, the values in the range of knee flexion angle (0°–140°) that could be obtained by all subjects were employed for calculations. Figure 4 show the AP translations of the medial and lateral ends of the TEA in that range. The medial end of the TEA demonstrated anterior translation from 0° to nearly 30° flexion (mean translation 3.6 ± 3.0 mm, range 0.9 mm posterior to 8.9 mm anterior) and demonstrated posterior translation after nearly 30°–140° (mean translation, 18.1 ± 3.7 mm, range, 13.4 mm posterior to 26.8 mm posterior), while the lateral end demonstrated consistent posterior translation throughout knee flexion (mean translation 31.1 ± 7.3 mm, range 19.8–45.4 mm posterior) (Fig. 5). Compared to the movement of the GCA [23], both lateral ends showed similar movement that were consistent with posterior translation throughout knee flexion. Regarding the medial ends, the peak of anterior translation of the TEA was earlier (30°) than that of the GCA (100°) (Fig. 6).
Changes in the angle of the TEA on the tibial axial plane (rotation angle)
In all subjects, the TEA exhibited external rotation on the axial plane of the tibial coordinate system throughout knee flexion. This indicates that all subjects demonstrated internal rotation of the tibia relative to the femur throughout knee flexion. The mean ± SD rotation angle was 16.9 ± 6.2° (range 5.0°–26.0°; female 18.3° ± 6.2°; male 15.5° ± 6.2°). Compared to the GCA, the GCA also exhibited external rotation on the axial plane of the tibial coordinate system throughout knee flexion. Mean rotation angle was 26.1 ± 6.3° (range 11.8°–40.3°; female 28.3° ± 6.1°; male 23.9° ± 6°) [23]. The angle of the TEA was significantly smaller than the angle of the GCA (P < 0.001).
Discussion
The most important finding of the present study was that the medial end of the TEA showed posterior translation from 30° knee flexion and this medial side’s early posterior translation made bicondylar posterior translation after mid-flexion. In our study, in vivo 3D dynamic kinematics of normal knees was evaluated through the full range of motion using the TEA as an evaluating parameter. The results were then compared with those of previous studies using the GCA as an evaluating parameter.
Regarding the AP translations of the medial and lateral ends of the TEA in our study, the medial end demonstrated an anterior translation of 3.6 mm from full extension to nearly 30° flexion followed by a posterior translation of 18.1 mm after nearly 30° to full flexion, while the lateral end demonstrated consistent posterior translation (31.1 mm) throughout knee flexion. The notable difference with GCA is the peak of anterior translation and the amount of posterior translation of the medial end. The medial end of the GCA does not reach the peak of anterior translation until nearly 100°. On the other hand, the medial end of the TEA reaches earlier (at nearly 30°). Regarding the amount of posterior translation, the medial end of the TEA moved 18.1 mm posteriorly after reaching the peak of the anterior translation (30°), while the GCA moved only 3.9 mm posteriorly. This result supported our hypothesis. Additionally, this result confirmed the results of past cadaveric studies. Most et al. [15] evaluated the passive motion kinematics of cadaveric knees from full extension to 150° flexion by the 3D-to-2D registration technique utilizing the GCA and TEA as evaluation parameters. In their study, the medial end of the TEA demonstrated a posterior translation from nearly 30° flexion to 150°, while the medial end of the GCA maintained anterior translation from full extension to 120°.
In the sagittal view, the lateral end of the TEA and GCA showed similar posterior movement throughout knee flexion because of roll-back of the lateral femoral condyle. The medial end of the TEA is located more anterior than the medial end of the GCA at full extension. Then, the medial end of the TEA moved posteriorly over the medial end of the GCA that itself showed less movement throughout knee flexion (Fig. 7). This is because the medial end of the TEA is anatomically located more anterior than the medial end of the GCA. If the surgical TEA was used as an evaluating parameter, this might show similar movement to the GCA because the medial end of the surgical TEA that is connecting the sulcus of the medial condyle and the prominent point of the lateral femoral condyle is located more posterior than that of the clinical TEA and closer to the medial end of the GCA. Victor et al. [25] evaluated geometrical references of the distal femur. In this study, the surgical TEA was almost parallel to the GCA (They expressed it femoral transverse axis) with a mean relative external rotation of 0.21° while the clinical TEA had a mean external rotation relative to GCA of 3.40°. From this result, it is expected that the surgical TEA shows similar movement to the GCA.
a The relationship between the medial end of the TEA and GCA are shown. The medial end of the TEA is located more anterior than the GCA at full extension. Then, the medial end of the TEA moved posteriorly over the GCA throughout knee flexion. Therefore, the medial end of the TEA is located more posterior than the GCA at 140°. b The relationship between the lateral end of the TEA and GCA are shown
Regarding the rotation angle, Most et al. reported the mean total rotation angles of the GCA and TEA were 19.9° and 7.2°, respectively [15]. In our study, the mean rotation angle of the TEA was 16.9°. This was also significantly smaller than the angle of the GCA (26.1°) and supported our hypothesis. So the results obtained in vivo dynamic active knee motion showed a similar tendency to the results obtained by cadaveric passive knee motion. The medial end of the GCA did not move significantly until nearly 120° knee flexion. On the other hand, the medial end of the TEA moved posteriorly, similar to the lateral end, beginning at nearly 30° knee flexion (Fig. 8). This made the rotation angle of the TEA smaller compared to the GCA.
There have been many studies regarding normal knee kinematics using various evaluating parameters [2, 3, 7, 9, 11–15, 23]. Kurosawa et al. [13] reported normal knee kinematics using the GCA as an evaluating parameter. In their study, from 0 to 120° the medial femoral condyle showed insignificant movement, the lateral moved posteriorly by 17 mm, and there was an axial rotation of 20°. Asano et al. [2] also evaluated in vivo normal knee kinematics using the GCA. In their study, the maximum length of the translation from hyperextension to flexion at an angle of 120° was 5.8 mm medially and 21.2 mm laterally. The maximum recorded axial rotation angle was 29.1°. Iwaki et al. [9] evaluated the stop-motion kinematics of cadaveric knees from full extension to 120° flexion by magnetic resonance imaging utilizing the FFC as an evaluation parameter. In their study, during flexion the combination of no anteroposterior movement medially and backward rolling laterally made a 20° internal rotation of the tibia around a medial axis with flexion. Komistek et al. [11] and Moro-oka et al. [14] analyzed the in vivo normal dynamic knee kinematics using the contact point as an evaluating parameter. They both showed the lateral condyle experienced more anteroposterior translation than the medial condyle during squatting motion.
Thus, in cases FFC, GCA and contact point were used as evaluating parameters, normal knee kinematics showed less medial motion, more anteroposterior translation laterally from full extension to nearly 120° knee flexion. Additionally, several studies showed bicondylar posterior translation. However, this phenomenon was observed after 120° knee flexion [18, 23]. On the contrary, our study found that the medial end of the TEA showed posterior translation from 30° knee flexion. It is important to understand that different motion patterns can be observed by using different evaluating parameters, even if the same knee movements are being measured.
The TEA has been used as a reference of the rotational alignment of the femoral component [1, 4, 16, 17, 19, 21, 27]. If the ultimate goal of TKA is to closely resemble the normal knee, the fact that TEA shows bicondylar posterior translation during midflexion may be an important aspect of normal knee kinematics, especially regarding gaining full flexion of the total knee. Then, the femoral component, the tibial insert, and the operation technique that represent the kinematics in this manner may be needed to achieve the goal.
This study has several limitations. First, the image registration technique using single-plane fluoroscopy is limited in out-of-plane accuracy. This reduced accuracy might influence the results when determining relative position between the femur and tibia. Second, we did not evaluate the knee motion using the surgical TEA as an evaluating parameter. This data might provide additional useful information.
The data of normal knees in this study provide references for analyzing pathologic knees as in cases of osteoarthritis or ligament injury. Additionally, these analyses could prove useful in the design of total knee prostheses. Especially, bicondylar posterior translation during midflexion of the TEA is a notable features.
Conclusions
When observing in vivo dynamic kinematics of the normal knee, the medial end of the TEA demonstrated anterior translation from 0° to nearly 30° flexion and demonstrated posterior translation after nearly 30°–140°, while the lateral end demonstrated consistent posterior translation throughout knee flexion. This medial side’s early posterior translation made bicondylar posterior translation after mid-flexion. As a result, the rotation angle of TEA was not very large (16.9°). Compared to the motion of the GCA, a different rotation angle and time that the medial side begins to translate posteriorly were observed.
References
Aglietti P, Sensi L, Cuomo P, Ciardullo A (2008) Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res 466:2751–2755
Asano T, Akagi M, Tanaka K, Tamura J, Nakamura T (2001) In vivo three-dimensional knee kinematics using a biplanar image-matching technique. Clin Orthop Relat Res 388:157–166
Asano T, Akagi M, Nakamura T (2005) The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image matching technique. J Arthroplasty 20:1060–1067
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118
Colle F, Bignozzi S, Lopomo N, Zaffagnini S, Sun L, Marcacci M (2012) Knee functional flexion axis in osteoarthritic patients: comparison in vivo with transepicondylar axis using a navigation system. Knee Surg Sports Traumatol Arthrosc 20:552–558
Eckhoff DG, Dwyer TF, Bach JM, Spitzer VM, Reining KD (2001) Three-dimensional morphology of the distal part of the femur viewed in virtual reality. J Bone Joint Surg Am 83(Suppl 2):43–50
Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J (2007) Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res 461:238–244
Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 82:1189–1195
Kobayashi K, Tanaka N, Odagawa K, Sakamoto M, Tanabe Y (2009) Image-based matching for natural knee kinematics measurement using single-plane fluoroscopy. J Jpn Soc Exp Mech 9:162–166
Komistek RD, Dennis DA, Mahfouz M (2003) In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res 410:69–81
Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G (2009) Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech 42:1877–1884
Kurosawa H, Walker PS, Abe S, Garg A, Hunter T (1985) Geometry and motion of the knee for implant and orthotic design. J Biomech 18:487–499
Moro-oka T, Hamai S, Miura H, Shimoto T, Higaki H, Fregly BJ, Iwamoto Y, Banks SA (2008) Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res 26:428–434
Most E, Axe J, Rubash H, Li G (2004) Sensitivity of the knee joint kinematics calculation to selection of flexion axes. J Biomech 37:1743–1748
Olcott CW, Scott RD (1999) The Ranawat Award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res 367:39–42
Olcott CW, Scott RD (2000) A comparison of 4 intraoperative methods to determine femoral component rotation during total knee arthroplasty. J Arthroplasty 15:22–26
Pinskerova V, Samuelson KM, Stammers J, Maruthainar K, Sosna A, Freeman MA (2009) The knee in full flexion. J Bone Joint Surg Br 91:830–834
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE (1996) Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res 331:35–46
Sato T, Koga Y, Omori G (2004) Three-dimensional lower extremity alignment assessment system. J Arthroplasty 19:620–628
Stiehl JB, Abbott BD (1995) Morphology of the transepicondylar axis and its application in primary and revision total knee arthroplasty. J Arthroplasty 10:785–789
Tan SP, Liau JJ, Chen WT, Cheng CK (2007) The accuracy of posterior condylar angles mesured by one MR images. Clin Orthop Relat Res 456:159–163
Tanifuji O, Sato T, Kobayashi K, Mochizuki T, Koga Y, Yamagiwa H, Omori G, Endo N (2011) Three-dimensional in vivo motion analysis of normal knees using single-plane fluoroscopy. J Orthop Sci 16:710–718
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 402:196–201
Victor J, Van Doninck D, Labey L, Van Glabbeek F, Parizel P, Bellemans J (2009) A common reference frame for describing rotation of the distal femur: a ct-based kinematic study using cadavers. J Bone Joint Surg Br 91:683–690
Yamazaki T, Watanabe T, Nakajima Y, Sugamoto K, Tomita T, Yoshikawa H, Tamura S (2004) Improvement of depth position in 2-D/3-D registration of knee implants using single-plane fluoroscopy. IEEE Trans Med Imaging 23:602–612
Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y (2001) Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 16:493–497
Acknowledgments
The authors would like to thank the entire staff of the Department of Radiology of the Niigata University Medical and Dental Hospital for their technical support and cooperation and Steve Lenio for his cooperation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanifuji, O., Sato, T., Kobayashi, K. et al. Three-dimensional in vivo motion analysis of normal knees employing transepicondylar axis as an evaluation parameter. Knee Surg Sports Traumatol Arthrosc 21, 2301–2308 (2013). https://doi.org/10.1007/s00167-012-2010-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2010-x