Abstract
The knee is a complex 3D joint whose normal function depends on the coordination of a supporting structure made of ligaments, muscles tendons, cartilage, menisci working together to preserve stability and gait. Any disruptions of these soft tissues lead to a mechanical disadvantage, pain, and knee pathologies such as cartilage defect that might require surgery. To preserve the integrity of the knee anatomy during TKA or ligament reconstruction, it is important that the biomechanics of the knee is well understood, the role each substructure plays in our daily activities and in achieving our performance goals. The knee articulation of the femur over the tibia is also guided and driven by the patellofemoral surface articulation and muscle producing forces to balance and regulate the energy-work expenditure by muscles. This chapter objective is to describe the biomechanics of the knee and its anatomy, modeling techniques, and gait analysis use in evaluation of knee performance. Finally, use of advance techniques in imaging, FEA, and multibody dynamics to understand the in-depth role of the knee mechanics for future clinical evaluation of new prostheses design and knee repairs to restore normal knee function.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Accurate knowledge of knee kinematics is critical to evaluate the knee joint and how it relates to changes in cartilage, ligament injuries, reconstruction or repairs and function. The knee is characterized by its geometry, forms and shapes of femoral condyles and their articulation on the tibia plateau, cartilage role in lubrication and support, and the balancing act of ligaments and muscle forces to accommodate different surface conditions during walking, and finally how the stability of the knee is maintained during flexion-extension under different loading conditions.
Clinical interest in the knee joint remains an interesting topic of research as biologics, nanotechnology, stem cells regenerative medicine is changing the fundamental role each of the knee substructure work and the ability to potentially being able to have them regenerated [32, 38, 20, 76].
The kinematics of the knee and its relation to different pathologies has been the subject of numerous research with different perspectives in light of the experiments conducted, models proposed, and outcome measures related to gait motion tracking analysis [43, 65, 50, 72, 53, 71, 45, 89]. To extract kinematic information in a single and dual plane, several researchers used fluoroscopy imaging techniques to analyze a quasi-static situation where a knee flexion is performed through a range of motion incrementally and radiographs were taken [100, 2, 27, 102]. Moreover, mobile fluoroscopic systems emerged and analysis of the knee during full dynamic flexion movements were examined during gait [42, 34].
The different joint rotations of the knee have been described from data collected by 3D camera and markers posted along the lower and upper part of the leg during gait. Most studies describe the knee flexion with a peak value observed after toe-off and the internal tibia rotation yielding its max at heel strike [44, 56, 34, 63, 64]. The tibia is shown to rotate externally through mid-stance, before rotating internally once again prior to toe-off [56, 54, 10, 81].
The tibiofemoral joint is still at the center stage of knee kinematic research and importantly, we still see different methods being used in describing the condylar anterior posterior translation following either the contact path, the condylar geometric center or other points on the condylar axis [88, 57, 73, 85, 91, 48].
The kinematics of a healthy knee or a knee with different pathologies or reconstruction depend great deal on the connective tissues around the knee in balancing and maintaining a stable and well-performing knee. The variation in knee analysis is also affected by other factors such as gender, anatomy, and articular surface behaviors which are all contributing factors to knee kinematics and kinetics.
Additional studies have investigated the tibia femoral joint contact surfaces during flexion-extension to investigate the cartilage effect on knee kinematics using both in vitro and in vivo experimental studies [35].
In silico 3D knee joint models were developed [37, 87], along with in vivo imaging measurements to provide a reliable validation of the results [13, 18, 92, 94, 61, 46]. These techniques have opened the door to advancing our understanding of modeling limitations, assumptions that clinically are relevant and acceptable versus additional knowledge needed to build better computational models on knee joint biomechanics.
The articular surface geometry as stated above at the contact area is also an important variable that affects the articular contact behaviors, such as contact stress and knee joint stability. Any changes to the cartilage contact area trigger a change in kinematics. Osteoarthritis (OA) of the knee is also a contributing factor to knee loading unbalance of forces and moments. The modulation of the knee joint results in large knee adduction moment and higher joint dynamic load during gait causally related to the severity of tibiofemoral OA [6, 52].
The complexity of the knee can also be seen in the role muscles in lower limb play in the knee joint stability and locomotion. To assess the contribution of different muscles to the knee, one needs to rely on 3D modeling techniques to evaluate contact pressure and forces generated from supporting structures at the knee using Opensim, life modeler among others [79, 84, 29]. Popular methods in gait analysis rely on knee joint flexion moment and knee joint power which are the predictors of load distribution across the tibiofemoral joint reflecting a special time point during gait stance phase.
The knee biomechanics teach us that optimization and coordination of the tibia femoral bones, patella-femoral articulating surface and muscles, ligament, and tendons interaction work together to achieve the desired joint movement. The complex interaction of these structures allows the knee to withstand tremendous forces during various normal movements.
Knee kinematics and its connective tissues was studied by Masouros, Parker, Hill, Amis, & Bull [67] and they pointed out its importance to diagnosis and treatments. Modeling and simulation methods used in the simulation of the knee during different walking conditions are studied by several researchers including to name a few [4, 106, 3, 1].
This chapter discusses the importance of the knee anatomy in joint biomechanics, provides a description of the knee joint kinematics and different methods used to assess knee performance and discusses the importance of the biomechanics of the knee, the current state of FE modeling and its clinical benefits. Understanding the knee biomechanics is an essential tool in designing prosthesis, provides guidance to rehabilitation exercises programs that will assist the patient knee stability, mobility and regain his or her knee normal function. A comprehensive understanding of the knee joint kinematics could significantly improve the future of patient’s knee injuries and treatment outcomes.
2 Basic Knee Anatomy
The knee joint consists of two basic articulations coordinated in a fashion to provide the knee muscles and ligaments the ability to power and drive its desired movements and function. The knee articulations are between the distal femur, proximal tibia, and patella riding on femoral groove. The geometry of the femoral condyles is asymmetric, with the medial condyle projecting more distal than the lateral femoral condyle. The medial condyle is also larger and wider and conforms to the tibia plateau condyle where it articulates, on the other hand, the lateral condyle projects more anteriorly. The condyles join through a femoral groove anteriorly and the femoral notch at their distal aspect to allow for the patella to slide, glide, and rotate to maintain the direction of the quadriceps and patella tendon forces. The lateral condyle can be identified by its terminal sulcus and groove of the popliteus insertion [26, 33].
The femoral condyles articulate on a tibia plateau that is also divided in two conforming surfaces: the medial tibial plateau is concave, whereas the lateral plateau has an anteroposterior convexity. This topography accounts for the so-called screw-home mechanism, or internal rotation, of the femur on the fixed tibia as the knee approaches extension [55, 104]. Load bearing on the tibia cartilage is usually due to excess stress on the knee which might lead to arthritis [23, 16, 47]. The distribution of the load on the tibia plateau is asymmetric, and occurs depending on the loading conditions not only centrally on the medial and lateral sides but also on the sloping edges on the medial and lateral part of the tibial eminences [83].
On each side of the tibia plateau, medial and lateral menisci help maintain conformity of the condyles during the knee flexion-extension and eliminate the high impact forces at the edges of the tibia plateau when subjected to high loads. Further description of the menisci shows that the anterior horn geometrical shape of the medial meniscus, the anterior cruciate ligament (ACL), and the anterior part of the lateral meniscus attach anterior to the tibial spine. The posterior cruciate ligament (PCL) and the posterior part of the medial and lateral menisci attach posterior to the tibial spine [33].
The patella consists of medial and lateral facets, separated by a vertical ridge to allow it to move within the prescribed femoral groove. The patella is totally embedded within the tendon. The front face of the patella is convex in shape and is divided up into 3 parts. The top surface is where the patella and the quadriceps tendon intersect and this lightly covers the anterior surface of the patella and forms a deep fascia, which acts as a protector to the bone [77]. The patella tendons and femoral contact reaction forces need to be balanced during knee motion to maintain knee stability. The patella contact stress makes it vulnerable to wear and potential injury [7, 70, 103].
3 Knee Joint Axis of Rotation
The primary knee joint motion is easily explained in the sagittal plane during flexion-extension. A joint used for such description is referred to as a hinge joint (see Fig. 21.1). In mechanical term describing such a joint with the context of reference Cartesian frame the knee is also a revolute joint as used in a few multibody dynamics modeling of locomotion where the angle of rotation is defined as the tibia rotation relative to the femur. The knee has six degrees of freedom and can rotate along three different planes as shown in Fig. 21.2. The complex three-dimensional motion also allows for translation along each of the axis of rotation. The ligaments act as supporting structure and constraint the knee joint motion by keeping it stable and limiting its range of motion.
Full extension is usually defined when the tibia is extended to become fully aligned with the femur in the sagittal plane. Active knee flexion is possible primarily through hamstring contraction and usually reaches 130°, whereas passive flexion can reach 160°.
To better understand the kinematics of the knee researchers used gait analysis to describe both human locomotion, and its relation to joint forces used to control such a movement. The position of the body upper part has always been an indicator of body posture in relation the body center of gravity. During gait ankle, knee and hip joint are actuators driven by muscles and hence generate torque necessary to move the body forward. Knee motion is dictated by the consideration of energy that requires the body center of gravity to move forward with ease.
During the swing phase of gait, the knee flexes to roughly 60° so the toe of the swinging leg does not be dragged on the ground. Also, during gait, as the swinging leg passes the standing leg and just before heel strike, the quadriceps muscle contracts which brings the knee to full extension and the foot forward. Flexion is not the only rotation that takes place during the gait cycle, as the knee extends 30° to 0°, the tibia externally rotates up to 30° before heel strike. The term used to describe this is “screw-home mechanism.” This mechanism occurs to tighten the soft tissue structures as well as locking the knee geometry before the impact load of weight bearing [66, 67].
4 Functional Role of Ligaments
The ACL is the main restraint to anterior tibial movement. The viscoelastic properties of the ligaments allow it to act against hyperextension to prevent injury, and act as a secondary restraint to prevent internal and valgus rotation when the knee is at full extension. The ACL essentially controls the “screw-home motion” of the knee joint [66]. The primary function of the ACL is to prevent anterior translation of the tibia and provide further knee stability. In full extension, the ACL absorbs 75% of the anterior translation load, and 85% between 30° and 90° of flexion [74, 59].
Knee injury can result into an ACL tear which lead to anterior knee instability and decrease in knee performance. ACL under load to failure testing reaches the ultimate stress at approximately 15% strain, and complete failure occurs between 15% and 30% strain, with a stretch close to 1 cm [60, 33]. The ACL has been reported to have an average maximal tensile stress to failure of 2100 N to 2500 N, but this is less under cyclic loading, creep, and age [93, 82, 19, 5].
The posterior tibia translation is controlled by the posterior cruciate ligament (PCL) and is most effective in mid to deep flexion. As stated by [66] the ACL and PCL together control the anterior posterior rolling and sliding kinematics of the TF joint during flexion and extension.
The PCL has an average tensile strength of 6.1 N at 0°, and a tensile strength of 112.3 N at 90°. [82]. The orientation of the PCL which inserts onto the lateral part of the medial femoral condyle allows for adequate tensioning of the PCL during the rolling of the lateral femoral condyle posteriorly in early flexion.
The interplay between the ACL and PCL is often referred to as the “four-bar cruciate linkage system” [39]. The intersection of the ACL and PCL shows that the center of joint rotation moves posterior with knee flexion. This allows both sliding and rolling movements of the femur during flexion and prevents the femur from rolling off the tibial plateau at extremes of flexion [11].
The axes of rotation of the knee are fundamental to kinematic models. The hinge model is not necessarily used for the current knee motion analysis as it is contradicted by the geometrical shape of the femoral condyles and the fact that the knee center of rotation is not fixed. The concept of “instant center of motion” has been linked to 4-bar mechanism where the ACL and PCL are viewed as rigid bars linking the tibia and femoral part the knee (see Fig. 21.3). The four-bar linkage theory can then be used to describe the knee motion and defines the instantaneous center of rotation associated with such mechanism. Assuming that the four bars are obliquely planar we can refer to such a system as a planar 4-bar linkage. The ligaments tension and stiffness alter the bars length and orientation in space which makes the 4-bar linkage not a reliable model for the knee. The cruciate ligaments can be assumed inextensible fibers and the IC can be tracked in relation to the tibia femoral joint as the knee flexes.
Different aspects of knee rotations and contact in both sagittal and coronal planes can be described assuming a center of rotation for the femoral component and tibia during the flexion-extension of the knee as shown in Fig. 21.4. The contact area is highlighted by the intersection of the tibial and femoral curvature radiuses. If the circles are tangent, we have a point contact otherwise there are two points of intersection defining a line contact. A surface contact is more realistic as both the line and point contacts are simply a representation of the contact area.
The role of the medial and lateral collateral ligaments can be described as follows: medial collateral ligament (MCL) is the restraint force to valgus angulation and internal tibial rotation and is a secondary restraint to external tibial rotation. It is also a secondary restraint to anterior tibial translations when the tibia is externally rotated. The lateral collateral ligament (LCL) on the hand is the restraint to varus angulation. It also assists in restraining the posterior translation, and becomes a restraining element with the PCL to external tibial rotation [66].
5 Function of the Menisci
The menisci wedge shape aids in providing conformity to the femoral and tibial articular surfaces. The primary functions of the menisci are to bear loads, to distribute the load of the knee joint medially and laterally passing the tibia–femur joint [105]. It also plays the role of a damper absorbing and damping energy during impact. This is done by the menisci inherent structure to deform under compressive loads by increasing the contact area [25]. The tensile stiffness and strength of the menisci are approximately 10 times greater than those of articular cartilage [101]. This allows the menisci to withstand the large hoop stresses generated by the knee joint [41, 68]. The menisci may also function as a secondary restraint to anterior translation in an ACL-deficient knee.
6 Gait Analysis of the Knee Joint
Gait analysis has gained popularity in the last decade due in part to better mathematical techniques and graphics display of the human musculoskeletal system with reliable solvers for inverse dynamics. Clinically gait analysis provides an insight into the motion limitations of the knee under different conditions, which when combined with imaging helps the physician develop a comprehensive idea on motion effects on patient problems. Hence, biomechanical gait analysis objective is the evaluation of the knee joint movement for a better understanding and diagnosis of knee joint injuries and pathologies. Several studies of OA have recognized the importance of biomechanical gait analysis in the pathogenesis of the knee joint and its supporting soft tissue structure.
Gait analysis combines both kinematical data of the lower and upper limbs collected through vision cameras and markers and uses mathematical models based on multibody dynamics to compute the inverse dynamics problem where it provides an estimation of the joint forces and moments. For this reason, biomechanical assessment has become important for knee joint problem diagnosis; it provides quantitative information about the structure and motion of the knee joint to complement the common orthopedic physical evaluation exam for more accurate diagnosis. Moreover, the experiments can be tailored such that gait phases can become indicators for sports and rehabilitation.
Walking, running, and stair climbing are activities that have been investigated by several researchers using gait analysis. While the main function of the knee joint is complex, gait simplified models can evaluate the joints forces and moments in relation to the body weight (BW) and walking speed. This of course is done for both the stance and swing phase of a gait cycle. The peak load at the knee joint varies from person to person and is estimated at 2–3 BW during walking, 4–6 BW during stair climbing, and 7–12 BW during running [23, 86, 40, 69].
The walking gait is characterized by two phases stance phase and swing phase as shown in Fig. 21.5. A full gait cycle is denoted by 100% and starts from the time foot heel strikes the ground and going through the swing phase to the time it strikes the ground again. The stance is the initial 65% of the gait cycle and the swing phase is the rest 35% of the cycle [49]. The stance phase consists of three sub-phases: initial (heel strike to foot flat), middle (foot flat to opposite heel strike), and terminal stance (opposite heel strike to toe-off) [22, 30, 49].
7 FEA Modeling of the Knee
Finite Element (FE) methods are widely used in orthopedics implant and prosthesis design. FEA is becoming a clinical tool for simulation of complex cases where new concepts or design are tested virtually before implementation. FE combined with imaging have provided considerable insight into understanding knee joint biomechanics, including ligament function, ligament reconstruction technique, and implant design. FEA is a mathematical tool that uses the law of mechanics to provide solutions to clinical problems in terms of stress-strains, force-deformations, work-energy, and other parameters used to describe the problem at hand. Due to inherent challenges associated with experiments (in vivo and ex vivo), FEA has long been recognized and trusted by researchers and government agencies such as the FDA as a reliable alternative method to the study of human joints-implant testing and validation.
Subject-specific FE modeling based on models obtained from CT-MRI data of that specific patient is useful in the study of OA as it can investigate the true interaction between multiple tissues and how changes in one can lead to implications in an adjacent tissue, which may lead to disease initiation or progression [17, 75]. Specifically, this FEA can investigate through different iterations of the same model by changing the material properties, the boundary conditions, and loading conditions (walk versus run) to assess such change on the model function. Sensitivity of design parameters associated with prostheses is studied without the burden of experiments cost [8, 14, 95].
FEA relies great deal on building realistic models and making the right assumptions to build high fidelity into the solutions provided by the FEA simulation studies (see Fig. 21.6). In the context of joint biomechanics, modeling of soft tissues such as ligaments becomes crucial to understanding how, to design corrective therapeutics and restore joint function [90, 21, 36].
FEA is still being developed to address multitude of questions and whether current models can be used to investigate a multiscale of substructure elements simultaneously while performing flexion-extension of the knee. Since multiple measurements are difficult and most experiments are designed for a specific purpose, additional techniques must be developed for validation purposes where both rigid, deformations and fluid-structure interaction are possible.
8 FEA Modeling of Knee Ligaments
Ligaments are complex viscoelastic structures that generate the necessary forces to maintain knee stability and smooth articulations within the kinematical range of motion they can sustain within injuries. How are these supporting structures-ligaments modeled in FEA. Models must be realistic, simple and capture the essential information for the task explored and analyzed. Early FE studies of the knee joint used uniaxial discrete line elements which can be viewed as springs with assigned material properties such as young modulus of elasticity found through testing and cadaveric experiments [9]. These models limitations can be overcome by high resolution imaging (MRI), and close look into the fibers alignments and mechanical testing to build a 3D ligament model that can be incorporated into the 3D FEA of the knee [9, 24]. A combination of accurate geometry, isotropic and transverse hyperelastic constitutive material models [51, 80] were developed in the study of the knee [97, 28, 12, 99]. The three ligaments models stated above are shown in Fig. 21.7.
The knee mathematical modeling seems to rely great deal on the understanding of the anatomy of ligaments, menisci, tendons, and patellofemoral and tibia articulations. While FEA and other dynamic tools have advanced the state of the art of modeling, the problem has become obviously important that additional computational tools are needed to appropriately diagnose and treat pathologies at early stage of their development.
9 Knee Biomechanics and Joint Acoustic Assessments
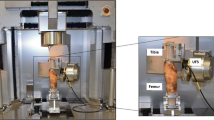
An area that needs further studies in knee biomechanics is acoustic and vibration. Knee joint sounds provide unique characteristics of how biomaterial structures respond to load. During the joint motion, the knee ligaments, tendons, cartilage and menisci inherent natural frequencies associated with their healthy geometry can be altered in the presence of injuries. Acoustic emissions are part of the knee biomechanics and their properties can be used as indicators when examining the knee (See Fig. 21.8). Vibration methods, such as acoustic and modal analysis, have been used in other industries with a lot of success to diagnose structural faults such as rattling effects, stress risers, and structural designs. Better understanding of the vibroacoustic characteristics of the knee must be developed. This work can pave the way for future studies aimed at employing acoustic emission and modal analysis approaches for knee health monitoring outside of clinical settings, such as for field-deployable diagnostics [15]. Other imaging techniques used to diagnose knee lesions expose the patient to potential radiation and are not suitable for outside clinical settings, such as on the sports field. Another example, the meniscus has shown to be an important factor impacting knee acoustic emissions, by influencing the width of joint space and, thus, the contact pressure of the tibiofemoral joint [98, 62].
Knee sound recording, Knee acoustic emissions were recorded using two high-performance, top port silicon acoustic sensors (size: 3 cm in diameter and 1 cm in depth, SPU0414HR5H-SB, Knowles Electronics, LLC. Itasca, IL, USA). One microphone was placed on the medial tibial plateau and one in the center of the patella. The sound signals were digitized with a sampling rate of 16,000 Hz. (Kalo et al. Journal of Biomechanics 109, 2020)
This acoustic tool is still a new research tool in knee biomechanics but it is a well-developed method in other industries. Possible predictors to the signal at the knee are still unknown due to the complexity of anatomy and how other elements can be elicited during the knee motion. Only when most of the contributing factors to the sound signal are identifiable and become known, proper diagnosis of the knee can be performed.
10 Advances, Challenges, and Future Directions in Knee Biomechanics
Today surgeons are regularly performing major complex reconstructive knee surgery, with highly encouraging results. Navigation and robotics are leading the way along with new operating scopes and devices assisting the surgeon achieve the most desirable outcome. Virtual reality and augmented reality are both being tested in the education and preparedness of surgeons in a world of complexity never seen before. Interactive surgery and access to vital information in real time is key to future advances.
Some of the knee challenges tend to be related to soft tissue repairs and regenerative cartilage. A simple ligament or menisci tear tends to raise questions on what procedure is most suitable.
The menisci can cause pain, clicking, giving way, locking, and swelling in the knee. If a meniscal tear is symptomatic, then it is likely to need surgery, and unfortunately only a minority of meniscal tears are repairable. The literature suggests that maybe only about 15 per cent of tears are repairable [58, 78, 31, 96]. The alternative of waiting then having knee replacement needs to be revisited. The idea of replacing the torn menisci with a new one is what is done by surgeons who perform menisci transplantation. This complex procedure allograft must be sized correctly and match the side of the knee. The meniscus itself is made of collagen, and everyone’s collagen is the same so there is no rejection. This area of research is improving, and each knee component plays an important role in the biomechanics of the knee.
The future of knee repair and surgery lies in advances in biological reconstruction, with allografts, with 3D printed biological scaffolds, with tissue engineering, growth factors and stem cells, augmented reality and artificial intelligence and simulation assisted surgeries. Knee biomechanics will play an important role in the future of knee repair and surgery which is set to be innovative and different from current practice.
Finite element methods together with other advance techniques in multibody dynamics, multiphysics will advance the state of simulation of the mechanical response of the complete knee under different loading and pathological conditions. FEA have benefited and will continue to benefit from increased computational power. However, the computer power never seems to be sufficient for real-time simulation of the load response of a knee joint. Improved numerical procedures or brand-new techniques are still necessary for better and faster understanding of surface contact solutions. The challenge to verify and validate a knee joint model is still work in progress.
Integrating FEA into gait analysis is required to determine the contact pressures in the knee in order to understand an abnormal gait. An FE knee model with a single-phase incompressible material law may be sufficient for the analysis of gait cycles but will not provide any information on the nutrient transport in articular cartilage that is performed by fluid flow in the tissue. A better FEA model will be needed to help understand the load share between the solid matrix and fluid pressurization, and the stress in the collagen.
Biomechanics in general is becoming a field of multi-disciplinary sciences and physics and mechanics working together to build anatomical realistic models to help us simulate conditions that are impossible in vivo or vitro. Another challenge remains on developing computationally and efficient parallel processing computers to meet future demands and challenges in knee biomechanics including surgical procedures.
Another aspects of biomechanics future studies are the classification of knee data into different diseases classes. Both clinical and modeling techniques including gait will benefit from the use of these large data samples. The use of AI (artificial intelligence) and deep learning neural networks could formulate a new knee joint biomechanical data classification that could easily be ready for access when diagnosis and treatments for complex cases are not available. Augmented reality, AI, biologics, and surgical innovations are the future for orthopedics.
References
Aburto-Barrera JM, Egure-Hidalgo M, Díaz-León C, Vázquez-Feijoo JA, Urriolagoitia-Sosa G. Mechanical design and numerical analysis of a femorotibial implant in patients with medial knee osteoarthritis; 2020. https://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/978-3-030-20801-1_23
Acker S, Li RM, Murray H, John PS, Banks SA, Mu S, et al. Accuracy of single-plane fluoroscopy in determining relative position and orientation of total knee replacement components. J Biomech. 2011;44(4):784–7. https://sciencedirect.com/science/article/pii/s0021929010005993
Adams MJ. Multi-scale modeling and analysis via surrogate modeling techniques for in vivo knee loading predictions; 2014. http://gradworks.umi.com/15/68/1568107.html
Amami A, Azouz ZB. Weakly supervised automatic segmentation and 3D modeling of the knee joint from MR images; 2013. https://spiedigitallibrary.org/conference-proceedings-of-spie/9067/1/weakly-supervised-automatic-segmentation-and-3d-modeling-of-the-knee/10.1117/12.2050908.full
Andrade A, Stock D, Costi JJ, Stanley RM, Kelly N, HearnTC, … Spriggins A. The in vivo intraoperative biomechanical properties of ACL grafts; 2002. https://online.boneandjoint.org.uk/doi/10.1302/0301-620x.84bsupp_iii.0840258
Astephen J, Deluzio KJ, Caldwell GE, Dunbar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J Orthop Res. 2008;26(3):332–41. https://onlinelibrary.wiley.com/doi/pdf/10.1002/jor.20496
Atsumi S, Arai Y, Kato K, Nishimura A, Nakazora S, Nakagawa S, et al. Transverse stress fracture of the proximal patella: a case report. Medicine. 2016;95(6) https://ncbi.nlm.nih.gov/pmc/articles/pmc4753884
Baldwin MA, Clary CW, Clary CW, Fitzpatrick CK, Deacy JS, Maletsky LP, Rullkoetter PJ. Dynamic finite element knee simulation for evaluation of knee replacement mechanics. J Biomech. 2012;45(3):474–83. https://sciencedirect.com/science/article/pii/s0021929011007469
Beidokhti HN, Janssen D, Groes SV, Boogaard TV, Verdonschot N. Subject-specific knee ligaments modeling approaches in finite element analysis: 1D and 3D; 2016. https://narcis.nl/publication/recordid/oai:ris.utwente.nl:publications/e30742a6-9658-45b3-8a8f-34c2d5878554
Bergfeld JA, McAllister DR, Parker RD, Valdevit A, Kambic H. The effects of tibial rotation on posterior translation in knees in which the posterior cruciate ligament has been cut. J Bone Joint Surg (Am Vol). 2001;83(9):1339–43. https://ncbi.nlm.nih.gov/pubmed/11568196
Bertin KC, Komistek RD, Dennis DA, Hoff W, Anderson DT, Langer T. In vivo determination of posterior femoral rollback for subjects having a NexGen posterior cruciate–retaining total knee arthroplasty. J Arthroplasty. 2002;17(8):1040–8. https://sciencedirect.com/science/article/pii/s0883540302002619
Beynnon BD, Yu J, Huston DR, Fleming BC, Johnson RJ, Haugh LD, Pope MH. A sagittal plane model of the knee and cruciate ligaments with application of a sensitivity analysis. J Biomech Eng Trans Asme. 1996;118(2):227–39. https://asmedigitalcollection.asme.org/biomechanical/article/118/2/227/397992/a-sagittal-plane-model-of-the-knee-and-cruciate
Bingham JT, Papannagari R, Velde SV, Gross C, Gill TJ, Felson DT, et al. In vivo cartilage contact deformation in the healthy human tibiofemoral joint. Rheumatology. 2008;47(11):1622–7. https://ncbi.nlm.nih.gov/pmc/articles/pmc2569133
Bo G, Laurent A. Measure TKA prosthesis constraint using computer simulation; 2018. https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992x.95bsupp_34.ista2013-062
Bolus NB, Jeong HK, Whittingslow DC, Inan OT. A glove-based form factor for collecting joint acoustic emissions: design and validation. Sensors. 2019;19(12):2683. https://mdpi.com/1424-8220/19/12/2683
Calder KM, Acker SM, Arora N, Beattie KA, Callaghan JP, Adachi JD, Maly MR. Knee power is an important parameter in understanding medial knee joint load in knee osteoarthritis. Arthritis Care Res. 2014;66(5):687–94. https://ncbi.nlm.nih.gov/pmc/articles/pmc4282060
Carey R, Zheng L, Aiyangar AK, Harner CD, Zhang X. Subject-specific finite element Modeling of the tibiofemoral joint based on CT, magnetic resonance imaging and dynamic stereo-radiography data in vivo. J Biomech Eng-Trans ASME. 2014;136(4):041004. https://ncbi.nlm.nih.gov/pubmed/24337180
Carter TE, Taylor K, Spritzer CE, Utturkar GM, Taylor DC, Moorman CT, et al. In vivo cartilage strain increases following medial meniscal tear and correlates with synovial fluid matrix metalloproteinase activity. J Biomech. 2015;48(8):1461–8. https://ncbi.nlm.nih.gov/pmc/articles/pmc4558182
Chakraborty S, Mondal D, Motalab M. Constitutive modeling of the human Anterior Cruciate Ligament (ACL) under uniaxial loading using viscoelastic prony series and hyperelastic five parameter Mooney-Rivlin model; 2016. https://aip.scitation.org/doi/abs/10.1063/1.4958358
Chevalier X, Kemta-Lepka F. Are biologics a treatment option in osteoarthritis. Therapy. 2010;7(6):675–83. https://openaccessjournals.com/articles/are-biologics-a-treatment-option-in-osteoarthritis.pdf
Grecu D, Pucalev I, Negru M, Tarniţă DN, Ionovici N, Diţă R. Numerical simulations of the 3D virtual model of the human hip joint, using finite element method. Romanian J Morphol Embryol. 2010;51(1):151–5. https://ncbi.nlm.nih.gov/pubmed/20191136
Davis R. Clinical gait analysis. IEEE Eng Med Biol Mag. 1988;7(3):35–40. https://sciencedirect.com/science/article/pii/b9780123969613000251
D'Lima DD, Fregly BJ, Patil S, Steklov N, Colwell CW. Knee joint forces: prediction, measurement, and significance; 2012. Retrieved March 10, 2020, from https://ncbi.nlm.nih.gov/pmc/articles/pmc3324308
Dousteyssier B, Molimard J, Hamitouche C, Han WS, Stindel E. Patient dependent knee modeling at several flexion angles: a study on soft tissues loadings. Ann Phys Rehabil Med. 2016;59. https://sciencedirect.com/science/article/pii/s1877065716301579
E, P. Studies on the tensile strength of knee joint menisci. Beitr Orthop Traumatol. 1965;12(10):668. http://europepmc.org/abstract/med/5881888
Flandry F, Perry CC. The anatomy and biomechanics of the posteromedial aspect of the knee; 2001. https://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/978-0-387-21601-0_3
Galvin CR, Galvin CR, Galvin CR, Perriman DM, Perriman DM, Perriman DM, et al. Age has a minimal effect on knee kinematics: a cross-sectional 3D/2D image-registration study of kneeling. Knee. 2019;26(5):988–1002. https://sciencedirect.com/science/article/pii/s0968016018306744
Germain F, Rohan P-Y, Rochcongar G, Rouch P, Thoreux P, Pillet H, Skalli W. Role of ligaments in the knee joint kinematic behavior: development and validation of a finite element model; 2016. https://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/978-3-319-28329-6_2
Ghazwan A. Muscle strategies and mechanical loading in patients with osteoarthritis; 2017. https://ethos.bl.uk/orderdetails.do?uin=uk.bl.ethos.732272
Gilchrist L, Winter DA. A multisegment computer simulation of normal human gait. IEEE Trans on Rehab Eng. 1997;5(4):290–9. Retrieved 10 4, 2020, from https://ncbi.nlm.nih.gov/pubmed/9422454
Gill TJ, R. M. Biologics and tissue engineering about the knee: biological repair. Foreword Knee Surgery. 2009:34–5.
Gill TJ, Randolph MA. Biologics and tissue engineering about the knee: biological repair. Foreword. J Knee Surg. 2009;22(1):34. https://ncbi.nlm.nih.gov/pubmed/19216351
Goldblatt JP, Richmond JC. Anatomy and biomechanics of the knee. Oper Tech Sports Med. 2003;11(3):172–86. https://sciencedirect.com/science/article/pii/1060187203800114
Guan S, Gray H, Schache AG, Feller JA, Steiger R d, Pandy MG. In vivo six-degree-of-freedom knee-joint kinematics in overground and treadmill walking following total knee arthroplasty. J Orthop Res. 2017;35(8):1634–43. https://onlinelibrary.wiley.com/doi/pdf/10.1002/jor.23466
Guettler JH, Demetropoulos CK, Yang KH, Jurist KA. Dynamic evaluation of contact pressure and the effects of graft harvest with subsequent lateral release at osteochondral donor sites in the knee. Arthroscopy. 2005;21(6):715–20. https://ncbi.nlm.nih.gov/pubmed/15944629
Guo H, Guo H, Maher SA, Spilker RL. A 3D biphasic finite element model of the human knee joint for the study of tibiofemoral contact and fluid pressurization; 2013. https://asmedigitalcollection.asme.org/sbc/proceedings/sbc2013/55614/v01bt55a005/287718
Halonen K, Mononen ME, Jurvelin JS, Töyräs J, Salo J, Korhonen RK. Deformation of articular cartilage during static loading of a knee joint – experimental and finite element analysis. J Biomech. 2014;47(10):2467–74. https://ncbi.nlm.nih.gov/pubmed/24813824
Hassan F, Murrell WD, Refalo A, Maffulli N. Alternatives to biologics in Management of Knee Osteoarthritis: a systematic review. Sports Med Arthrosc Rev. 2018;26(2):79–85. https://insights.ovid.com/sports-medicine-arthroscopy-review/smart/2018/06/000/alternatives-biologics-management-knee/9/00132585
Hernáiz-Alzamora A, Arza JI, Zarranz JU, Renovales FD. Anthropometry of the cruciate ligaments of the knee: MRI study of the human four-bar linkage device. Eur J Anat. 2017;21(1):1–11. https://dialnet.unirioja.es/servlet/articulo?codigo=6282266
Hirokawa S, MotookaT, Akiyama T, Morizono R, Tanaka R, Mawatari M, … Hotokebuchi T. Calculation of the forces acting on the knee joint during ascent from kneeling; 2012. https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992x.94bsupp_xxv.ista2010-094
Hopgood, P., Monk, J., & Nokes, L. D. (2004). O3074 Tensile testing of meniscal repair techniques. Retrieved 10 3, 2020, from http://bjjprocs.boneandjoint.org.uk/content/86-b/supp_iii/344.2.short
Hourlier H, Fennema P. Intraoperative fluoroscopy improves surgical precision in conventional TKA. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1619–25. https://ncbi.nlm.nih.gov/pmc/articles/pmc4059969
Jacofsky, D. J., McCamley, J. D., Bhowmik-Stoker, M., Jacofsky, M. C., & Shrader, M. (2011). A1017. Advanced osteoarthritic gait kinematics and kinetics. http://bjjprocs.boneandjoint.org.uk/content/jbjsbrproc/93-b/supp_iv/399.1.full.pdf
Jayabalan P, Gustafson J, Huang W, Piva SR, Sowa GA, Farrokhi S. The influence of continuous versus interval walking exercise on joint loading and serum biomarker profile in patients with knee osteoarthritis. Pm&r. 2015;7(9) https://pmrjournal.org/article/s1934-1482(15)00343-3/abstract
Jb S, R, K., & Da, D. A novel approach to knee kinematics. Am J Orthop. 2001;30(4):287. https://ncbi.nlm.nih.gov/pubmed/11334450
Jones MD, Tran CW, Li G, Maksymowych WP, Zernicke RF, Doschak MR. In vivo microfocal computed tomography and micro–magnetic resonance imaging evaluation of antiresorptive and antiinflammatory drugs as preventive treatments of osteoarthritis in the rat. Arthritis Rheum. 2010;62(9):2726–35. https://ncbi.nlm.nih.gov/pubmed/20533290
Jones R, Chapman GJ, Findlow AH, Forsythe L, Parkes MJ, Sultan J, Felson DT. A new approach to prevention of knee osteoarthritis: reducing medial load in the contralateral knee. J Rheumatol. 2013;40(3):309–15. http://jrheum.org/content/40/3/309
Kang K-T, Kwon SK, Kwon O-R, Lee J-S, Koh Y-G. Comparison of the biomechanical effect of posterior condylar offset and kinematics between posterior cruciate-retaining and posterior-stabilized total knee arthroplasty. Knee. 2019;26(1):250–7. https://ncbi.nlm.nih.gov/pubmed/30577956
Kasović, M., Mrđen, I., & Mejovšek, M. (2009). Biomechanics of normal gait. Retrieved 10 4, 2020, from http://bib.irb.hr/datoteka/409911.biomehanika_normalnog_hoda_zadar2009.pdf
Kaufman KR, Hughes CA, Morrey BF, Morrey MA, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001;34(7):907–15. https://sciencedirect.com/science/article/pii/s0021929001000367
Kiapour AM, Kaul V, Kiapour A, Quatman CE, Wordeman SC, Hewett TE, et al. The effect of ligament Modeling technique on knee joint kinematics: a finite element study. Appl Mathematics. 2013;4(5):91–7. https://ncbi.nlm.nih.gov/pmc/articles/pmc4160050
Knoop J, Dekker J, Leeden M v, Esch M v, Klein J-P, Hunter DJ, et al. Is the severity of knee osteoarthritis on magnetic resonance imaging associated with outcome of exercise therapy. Arthritis Care Res. 2014;66(1):63–8. https://ncbi.nlm.nih.gov/pubmed/23982988
Koo S, Andriacchi TP, Andriacchi TP. The knee joint Center of Rotation is predominantly on the lateral side during Normal walking. J Biomech. 2008;41(6):1269–73. https://ncbi.nlm.nih.gov/pmc/articles/pmc2481385
Kozanek M, Brodsky JW, Kane JM. The effect of ankle arthrodesis on the biomechanical function of the foot: a prospective, three-dimensional, multi-segment gait analysis with clinical correlation. Foot & Ankle Orthopaedics. 2017;2(3) https://journals.sagepub.com/doi/abs/10.1177/2473011417s000247
Lafortune MA, Cavanagh PR. ‘Screw home’ mechanism of the knee during walking. J Biomech. 1985;18(7):531. https://api.elsevier.com/content/article/pii:002192908590733x?httpaccept=text/xml
Lake M, Lafortune MA, Perry S. Heel plantar pressure distortion caused by discrete sensors. J Biomech. 1992;25(7):768. https://api.elsevier.com/content/article/pii:002192909290485j?httpaccept=text/xml
Landes CA, Sterz M. Evaluation of condylar translation by sonography versus Axiography in orthognathic surgery patients. J Oral Maxillofac Surg. 2003;61(12):1410–7. https://ncbi.nlm.nih.gov/pubmed/14663805
LaPrade CM, James EW, LaPrade RF, Engebretsen L. How should we evaluate outcomes for use of biologics in the knee. J Knee Surg. 2014;28(01):035–44. https://ncbi.nlm.nih.gov/pubmed/25260033
Laskowski ER. ACL injury and rehabilitation. Curr Phys Med Rehabil Rep. 2014;2(1):35–40. https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s40141-013-0036-8
Lu M, Johar S, Veenema K, Goldblatt JP. Patellar tendon rupture with underlying systemic lupus erythematosus: a case report. J Emerg Med. 2012;43(1) https://ncbi.nlm.nih.gov/pubmed/19959318
Lustig S, Scholes C, Balestro J-C, Parker D. In vivo assessment of weight-bearing knee flexion reveals compartment-specific alterations in meniscal slope. Arthroscopy. 2013;29(10):1653–60. https://sciencedirect.com/science/article/pii/s0749806313008153
Madeleine, P., Andersen, R. E., & Arendt-Nielsen, L. (2018). Spatial dependencies of knee vibroarthrograms during knee flexion-extension movement. https://vbn.aau.dk/da/publications/spatial-dependencies-of-knee-vibroarthrograms-during-knee-flexion
Mandeville D, Osternig LR, Chou L-S. The effect of total knee replacement surgery on gait stability. Gait Posture. 2008a;27(1):103–9. https://sciencedirect.com/science/article/abs/pii/s0966636207000719
Mandeville D, Osternig LR, Lantz BA, Mohler CG, Chou L-S. The effect of total knee replacement on the knee varus angle and moment during walking and stair ascent. Clin Biomech. 2008b;23(8):1053–8. https://sciencedirect.com/science/article/pii/s0268003308001599
Marcum ZA, Zhan HL, Perera S, Moore CG, Fitzgerald GK, Weiner DK. Correlates of gait speed in advanced knee osteoarthritis. Pain Med. 2014;15(8):1334–42. https://academic.oup.com/painmedicine/article-lookup/doi/10.1111/pme.12478
Masouros SD, Bull AM, Amis AA. A biomechanics of the knee joint. Orthop Trauma. 2010;24(2):84–91. https://sciencedirect.com/science/article/abs/pii/s1877132710000308
Masouros SD, Parker KH, Hill AM, Amis AA, Bull AM. Testing and modelling of soft connective tissues of joints: a review. J Strain Anal Eng Des. 2009;44(5):305–18. http://journals.sagepub.com/doi/10.1243/03093247jsa507
Mathur PD, McDonald JR, Ghormley RK. A study of the tensile strength of the menisci of the knee. J Bone Joint Surg (Am Vol). 1949;31(3):650–4. https://ncbi.nlm.nih.gov/pubmed/18153906
McLean SG, Su A, Bogert A v. Development and validation of a 3-D model to predict knee joint loading during dynamic movement. J Biomech Eng-Trans ASME. 2003;125(6):864–74. https://asmedigitalcollection.asme.org/biomechanical/article/125/6/864/459606/development-and-validation-of-a-3-d-model-to
Minns R, Birnie A, Abernethy P. A stress analysis of the patella, and how it relates to patellar articular cartilage lesions. J Biomech. 1979;12(9):699–711. https://sciencedirect.com/science/article/pii/0021929079900198
Na A, Buchanan TS. Self-reported walking difficulty and knee osteoarthritis influences limb dynamics and muscle co-contraction during gait. Hum Mov Sci. 2019;64:409–19. https://sciencedirect.com/science/article/pii/s0167945718303427
Naili JE, Broström EW, Clausen B, Clausen B, Holsgaard-Larsen A, Holsgaard-Larsen A. Measures of knee and gait function and radiographic severity of knee osteoarthritis – a cross-sectional study. Gait Posture. 2019;74:20–6. https://ncbi.nlm.nih.gov/pubmed/31442818
Nakamura S, Nakamura S, Sharma A, Ito H, Nakamura K, Zingde SM, Komistek RD. Kinematic difference between various geometric Centers and contact points for tri-condylar bi-surface knee system. J Arthroplasty. 2015;30(4):701–5. https://sciencedirect.com/science/article/pii/s0883540314008961
Nesbitt RJ, Herfat ST, Boguszewski DV, Engel AJ, Galloway MT, Shearn JT. Primary and secondary restraints of human and ovine knees for simulated in vivo gait kinematics. J Biomech. 2014;47(9):2022–7. https://ncbi.nlm.nih.gov/pmc/articles/pmc4032813
Nicolella, D. P., Bichon, B. J., Francis, W. L., & Eliason, T. D. (2011). Dynamic Modeling of Knee Mechanics. https://asmedigitalcollection.asme.org/imece/proceedings/imece2011/54884/517/354790
Parker D. ISAKOS knee committee: biologics in orthopaedics. Arthroscopy. 2015;31(4):714. https://ncbi.nlm.nih.gov/pubmed/25842232
Pastides P, Shenoy R, Nathwani D. The patella in total knee replacement. Orthopaedics and Trauma. 2013;27(6):372–8. https://sciencedirect.com/science/article/pii/s1877132713001231
Pot, M. W., Gonzales, V. K., Buma, P., IntHout, J., Kuppevelt, T. H., Vries, R. B., & Daamen, W. F. (2016). Improved cartilage regeneration by implantation of acellular biomaterials after bone marrow stimulation: a systematic review and meta-analysis of animal studies. Peer J, 4. https://peerj.com/articles/2243
Potvin, B. (2016). Predicting Muscle Activations in a Forward-Inverse Dynamics Framework Using Stability-Inspired Optimization and an In Vivo-Based 6DoF Knee Joint. http://ruor.uottawa.ca/bitstream/10393/34647/3/potvin_brigitte_2016_thesis.pdf
Reese, S. P., Ellis, B. J., & Weiss, J. A. (2013). Multiscale Modeling of Ligaments and Tendons. https://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/8415_2012_157
Reischl SF, Powers CM, Rao S, Perry J. Relationship between foot pronation and rotation of the tibia and femur during walking. Foot Ankle Int. 1999;20(8):513–20. https://journals.sagepub.com/doi/abs/10.1177/107110079902000809
Ristaniemi A, Stenroth L, Mikkonen S, Korhonen RK. Comparison of elastic, viscoelastic and failure tensile material properties of knee ligaments and patellar tendon. J Biomech. 2018;79:31–8. https://sciencedirect.com/science/article/pii/s0021929018306134
Rossom SV, Wesseling M, Smith CR, Smith CR, Thelen DG, Thelen DG, et al. The influence of knee joint geometry and alignment on the tibiofemoral load distribution: a computational study. Knee. 2019;26(4):813–23. https://sciencedirect.com/science/article/pii/s0968016018305258
Seipel, J. (2012). Towards Robustly Stable Musculo-Skeletal Simulation of Human Gait: Merging Lumped and Component-Based Modeling Approaches. https://proceedings.asmedigitalcollection.asme.org/proceeding.aspx?articleid=1736295
Sharma A, Dennis DA, Dennis DA, Dennis DA, Zingde SM, Mahfouz MR, Komistek RD. Femoral condylar contact points start and remain posterior in high flexing patients. J Arthroplasty. 2014;29(5):945–9. https://sciencedirect.com/science/article/pii/s0883540313007183
Shelburne KB, Torry MR, Pandy MG. Muscle, ligament, and joint-contact forces at the knee during walking. Med Sci Sports Exerc. 2005;37(11):1948–56. https://ncbi.nlm.nih.gov/pubmed/16286866
Shim VB, Shim VB, Besier TF, Lloyd DG, Lloyd DG, Mithraratne K, Fernandez J. The influence and biomechanical role of cartilage split line pattern on tibiofemoral cartilage stress distribution during the stance phase of gait. Biomech Model Mechanobiol. 2016;15(1):195–204. https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s10237-015-0668-y
Stiehl JB, Dennis DA, Komistek RD, Crane HS. In vivo determination of condylar Lift-off and screw-home in a Mobile-bearing Total knee arthroplasty. J Arthroplasty. 1999;14(3):293–9. https://ncbi.nlm.nih.gov/pubmed/10220182
Stiehl JB, Komistek RD, Haas BD, Dennis DA. Frontal plane kinematics after mobile-bearing total knee arthroplasty. Clin Orthop Relat Res. 2001;392(392):56–61. https://ncbi.nlm.nih.gov/pubmed/11716425
Sultan, S., Abdel-Malek, K., Arora, J. S., Bhatt, R., & Marler, T. (2017). An Integrated Computational Simulation System for Injury Assessment. https://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/978-3-319-41627-4_3
Takashi S, Yoshio K, Ten S, Go O, Yuji T. Three-dimensional knee kinematics analysis after tka-does the tilting of femoral component in coronal plane always indicate “condylar lift-off”?; 2018. https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620x.90bsupp_i.0880187
Tardy N, Marchand P, Kouyoumdjian P, Blin D, Demattei C, Asencio G. A preliminary in vivo assessment of anterior cruciate ligament–deficient knee kinematics with the KneeM device: a new method to assess rotatory laxity using open MRI. Orthop J Sports Med. 2014;2(3):–2325967114525583. https://ncbi.nlm.nih.gov/pmc/articles/pmc4555568
Torre M, Feo FD, Angelis GD, Ruspantini I, Frustagli G, Chistolini P. ACL reconstruction by bone-patellar tendon-bone graft: mechanical evaluation of the elastic modulus and failure modes. J Orthop Traumatol. 2003;4(2):69–75. https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s10195-003-0012-7
Wang L, Wu Y, Chang G, Oesingmann N, Schweitzer ME, Jerschow A, Regatte RR. Rapid isotropic 3D-sodium MRI of the knee joint in-vivo at 7T. J Magn Reson Imaging. 2009;30(3):606–14. https://ncbi.nlm.nih.gov/pmc/articles/pmc2759273
Wawro M, Fathi-Torbaghan M. A parallel framework for the FE-based simulation of knee joint motion. IEEE Trans Biomed Eng. 2004;51(8):1490–4. https://ncbi.nlm.nih.gov/pubmed/15311837
Wernecke GC, Constantinidis A, Harris IA, Seeto BG, Chen DB, MacDessi SJ. The diameter of a single bundle, hamstring autograft does not significantly influence revision rate or clinical outcomes after anterior cruciate ligament reconstruction. Knee. 2017;24(5):1033–1038. https://doi.org/10.1016/j.knee.2017.05.011.
Weiss JA, Weiss JA, Gardiner JC, Ellis BJ, Ellis BJ, Lujan TJ, et al. Three-dimensional finite element modeling of ligaments: technical aspects. Med Eng Phys. 2005;27(10):845–61. http://coen.boisestate.edu/ntm/files/2012/07/weiss_2005_mep-fe-techniques.pdf
Whittingslow DC, Whittingslow DC, Jeong H-K, Ganti VG, Kirkpatrick NJ, Kogler GF, Inan OT. Acoustic emissions as a non-invasive biomarker of the structural health of the knee. Ann Biomed Eng. 2020;48(1):225–35. https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s10439-019-02333-x
Woo SL, Abramowitch SD, Kilger R, Liang R. Biomechanics of knee ligaments: injury, healing, and repair. J Biomech. 2006;39(1):1–20. https://sciencedirect.com/science/article/pii/s0021929004005317
Yamazaki, T., Watanabe, T., Tomita, T., Sugamoto, K., Ogasawara, M., Sato, Y., … Tamura, S. (2007). 3D kinematics of normal knee using X-ray fluoroscopy and CT images. https://springerlink.bibliotecabuap.elogim.com/chapter/10.1007/978-3-540-36841-0_706
Yan S-H, Ou-Yang H-K, Shan Y-L, Luo D-Z, Wang H, Zhang K. Tensile biomechanical characteristics of human meniscus. Emerg Mater Res. 2016;5(1):44–9. https://icevirtuallibrary.com/doi/abs/10.1680/jemmr.15.00031
Zeller, I., Grieco, T., Meccia, B., Sharma, A., & Komistek, R. D. (2018). Development and implementation of a mathematical model to successfully predict normal knee kinematics. https://online.boneandjoint.org.uk/doi/10.1302/1358-992x.2018.5.024
Zhang, J., Jiang, K., & Chen, R. (1991). Stress analysis in patella by three-dimensional photoelasticity. https://spiedigitallibrary.org/conference-proceedings-of-spie/1554/0000/stress-analysis-in-patella-by-three-dimensional-photoelasticity/10.1117/12.49563.full
Zhang L-K, Wang X-M, Niu Y, Liu H-X, Wang F. Relationship between patellar tracking and the “screw-home” mechanism of tibiofemoral joint. Orthop Surg. 2016;8(4):490–5. https://onlinelibrary.wiley.com/doi/pdf/10.1111/os.12295
Zhou T. Analysis of the biomechanical characteristics of the knee joint with a meniscus injury. Healthc Technol Lett. 2018;5(6):247–9. https://ieeexplore.ieee.org/document/8556606
Zhu Y, Chen JX, Xiao S, Mahon EM. 3D knee modeling and biomechanical simulation. Comput Sci Eng. 1999;1(4):82–7. https://aip.scitation.org/doi/full/10.1109/5992.774845
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 ISAKOS
About this chapter
Cite this chapter
Amirouche, F., Koh, J. (2021). Biomechanics of the Knee. In: Koh, J., Zaffagnini, S., Kuroda, R., Longo, U.G., Amirouche, F. (eds) Orthopaedic Biomechanics in Sports Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-81549-3_21
Download citation
DOI: https://doi.org/10.1007/978-3-030-81549-3_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-81548-6
Online ISBN: 978-3-030-81549-3
eBook Packages: MedicineMedicine (R0)