Abstract
Purpose
This study aims to report the long-term results of lateral release and medial plication in patients with recurrent patellar dislocation.
Methods
In this study, 31 patients who underwent surgery for recurrent patellar dislocation were retrospectively reviewed between 1994 and 2004. Among the 31 patients were 12 male and 19 female patients. The average age was 23.9 ± 4.8 years, and the mean follow-up period was 11.6 ± 2.4 years.
Results
Three patients had postoperative dislocations. The mean Kujala score significantly improved from 57.5 ± 13.2 points preoperatively to 89.2 ± 8.7 points at the final follow-up (P < 0.0001). The median Tegner activity score significantly improved from 3 (range, 1–5) at preoperative examination to 7 (range, 3–9) at the final follow-up (P < 0.0001). Ten patients were rated as excellent, 18 as good, 2 as fair, and 1 as poor. The congruence angle improved from 16.5° ± 3.0° to −2.8° ± 2.7°, and the lateral patellofemoral angle improved from −4.2° ± 1.9° to 8.2° ± 2.5°. There was no case of osteoarthritis at the final follow-up.
Conclusions
Percutaneous lateral release and medial plication showed satisfactory results with limited morbidity in the long-term follow-up. This traditional method remains a simple and effective surgical procedure for recurrent patellar dislocation.
Level of evidence
Therapeutic, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent patellar dislocation and subluxation are commonly present in young and physically active people. Numerous etiological factors for this injury have been proposed [10]. Previous studies reported a prevalence of 0.043%, being more common among women than men [8]. Historically, patients diagnosed with primary patellar dislocation have been managed conservatively. A previous study suggested that between 40 and 60% of patients managed conservatively experience recurrent patellar dislocation and subluxation [37]. Recurrent instability often necessitates surgical intervention. Depending on the cause of dislocation, different operations are adopted. In instances of severe trochlear dysplasia, trochleoplasty is indicated. If extensor mechanism disorders are present, proximal realignment, distal realignment, or combined surgery is adopted. In case of lower limb malalignment (increase of Q-angle) or patella alta, distal realignment surgery is indicated. In most cases, proximal soft-tissue procedures are indicated. The ideal candidates for proximal soft-tissue procedures have a normal Q-angle, insufficient medial structures, and initial instability resulting from a traumatic event [19, 42]. Proximal soft-tissue procedures seek to balance the medial and lateral soft tissues. The rationale for these procedures is that recurrent patellar dislocation is due to anatomical vulnerability of the medial structures, including the medial patellofemoral ligament, medial retinaculum, vastus medialis obliquus, and tightness of the lateral structures such as the retinaculum or the iliotibial band [13, 17, 41]. Although various proximal soft-tissue procedures have been proposed, there is no consensus on the most effective procedure. Even though percutaneous lateral release and medial plication is an old-fashion procedure, good results have been numerously reported, citing its simplicity and relatively easy manipulation of tension [4, 27, 35]. However, studies on the long-term results of this procedure are still insufficient. Therefore, this study aimed to report the long-term results of lateral release and medial plication for the treatment of recurrent patellar dislocation. It was hypothesized that this surgical procedure would demonstrate good outcomes over 7 years of follow-up.
Materials and methods
Between 1994 and 2004, 56 patients underwent percutaneous lateral release and medial plication under arthroscopy for recurrent patellar dislocation. However, only 43 patients were able to be followed up for more than 7 years. Surgery was performed by the senior author of this study. The institutional review board of Gangnam Severance Hospital approved this study.
Surgical indications included patients who experienced recurrent patellar dislocation under low energy on history taking and whose apprehension test was positive on physical examination. Exclusion criteria were as follows: (1) Q-angle greater than 20°, (2) patella alta (Insall-Salvati ratio >1.2), (3) patients who had surgery immediately after trauma due to a large cartilage lesion, (4) a history of previous surgery for recurrent patellar dislocation, (5) a severe trochlear dysplasia (Dejour’s classification B, C, D) [15], and (6) a congenital patellar dislocation. We found 31 patients who met the above criteria for inclusion: 12 men and 19 women. In total, 12 patients were excluded. Ten patients were excluded because they underwent both the proximal and distal procedures due to an increased Q-angle (4 patients), patella alta (2 patients), previous surgery (1 patient), and combined causes (3 patients). The remaining two patients were excluded due to immediate surgery after trauma.
All patients were assessed with the Kujala knee score [25] and the Tegner activity scale [40] before and after the operation. In addition, the patient-rating questionnaire as described by Drez et al. [20] was used at the final follow-up to reflect the subjective evaluation of patients. On this subjective scale, patients selected one of the following statements: (1) The knee has markedly improved, and I have returned to all activities. (2) The knee has improved, but there is still occasional discomfort or problems during sports activities. (3) The knee has improved, but I am still unable to return to sports activities. (4) The knee is not better or worse than before surgery. The patients subjectively graded each item as excellent, good, fair, or poor. Radiographic examination consisted of the anterior–posterior view, the lateral view, and the Merchant axial view. An MRI was performed only when cartilage damage was suspected. Congruence angle, sulcus angle, and lateral patellofemoral angle were measured in the Merchant axial view. The shape of the patella was decided according to the Wiberg classification [44]. Trochlear dysplasia was defined by a positive crossing sign on a true lateral radiograph or a sulcus angle in the axial view greater than 145° [15]. In order to determine the stage of arthritis, the condition of the patellofemoral joint was assessed according to the Kellgren-Lawrence system. The femorotibial joint was also assessed to compare with the patellofemoral joint in order to distinguish arthritis due to surgery from arthritis due to aging. Patellofemoral joint arthritis was considered to have progressed after surgery when all three observers agreed that arthritis in the patellofemoral joint had progressed more than that in the femorotibial joint.
Surgical procedure
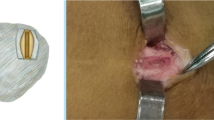
The patella was easily subluxed or completely dislocated in all cases with laterally directed passive pressure under anesthesia. A tourniquet was inflated, and standard knee arthroscopy was performed. Chondral and osteochondral loose bodies not amenable to reattachment were removed. The medial retinaculum was injured by an electrocautery device so that medial plication would be strengthened through adhesion. Using No. 1 Ethibond sutures (Ethicon Inc, Somerville, NJ), the medial retinaculum was advanced to the medial border of the patella using at least four mattress sutures. A generous lateral release was then performed from the superior pole of the patella to the inferior pole, avoiding the vastus lateralis under direct arthroscopic visualization. Lateral release was performed until the patella was tilted 90° to the plane of the trochlear surface with the knee fully extended [1]. An arthroscope was then reintroduced to confirm centralization of the patella within the trochlear groove, and suture tension was either increased or decreased as necessary. After the tourniquet was deflated, patellar tracking was grossly reevaluated to confirm that the initial contact was centralized and maintained throughout flexion (from 45° to 90°). Finally, after adjusting tension, the sutures were then tied with the knee at full extension. After surgery, the knee was immobilized at full extension for 4 weeks. At 1 day after surgery, patients were allowed to use crutches with partial weight bearing. Four weeks after surgery, passive and active range of motion and quadriceps-strengthening exercises were gradually initiated.
Statistical analysis
SPSS software (version 18; SPSS, Chicago, IL) was used for statistical analyses. The Wilcoxon signed rank test was used to compare the preoperative and postoperative Kujala knee scores, Tegner activity scores, congruence angles, and lateral patellofemoral angles. The level of significance was set at P < 0.05.
Results
The average age at the time of operation was 23.9 ± 4.8 years (range, 14–32). All patients had a history of trauma prior to the operation. The average number of dislocations before the operation was 9.5 ± 2.9 times, and the average time from trauma to operation was 37.6 ± 7.4 months. The mean follow-up period was 11.6 ± 2.4 years (range, 7–16.9 years). On the preoperative axial radiographs, Wiberg type II patella was found in 27 patients, and Wiberg type I patella was found in four patients. Sixteen patients (52%) were diagnosed with trochlear dysplasia. Eight patients (26%) had an osteochondral lesion that ranged from 0.8 to 1.6 cm (mean, 1.1 cm). The mean Kujala score significantly improved from 57.5 ± 13.2 points preoperatively to 89.2 ± 8.7 points at the final follow-up (P < 0.0001). The median Tegner activity score significantly improved from 3 (range, 1–5) at preoperative examination to 7 (range, 3–9) at the final follow-up (P < 0.0001). On the patient’s subjective evaluation, 10 knees (32%) were rated as excellent, 18 (58%) as good, two (6%) as fair, and one (3%) as poor. After surgery, the average congruence angle improved from 16.5° ± 3.0° to −2.8° ± 2.7°, and the average lateral patellofemoral angle improved from −4.2° ± 1.9° to 8.2° ± 2.5° (P < 0.0001). There was no case where progression of patellofemoral arthritis was agreed upon by all three observers (Fig. 1).
A preoperative radiograph (A-1) of a 14-year-old female patient and a radiograph taken 16.9 years after surgery (A-2). No progression of osteoarthritis was noted. A preoperative radiograph (B-1) of a 25-year-old male patient and a radiograph taken 7.5 years after surgery (B-2). Only two of three observers agreed that osteoarthritis had progressed due to the formation of a small osteophyte (black arrow)
In this study, three knees had recurrent instability and required a revision operation: two knees with trochlear dysplasia and one with generalized laxity defined by Carter and Wilkinson [11]. As minor complications, there were two knees with aspiration due to hematomas and one knee with superficial infection, which were treated with antibiotics for 2 weeks. There were three knees that had a loss of flexion of less than 135°; however, this did not cause any problem in daily life.
Discussion
The principal findings of this investigation were that the long-term clinical and radiographic results of percutaneous lateral release and medial plication were satisfactory, and there were no reports of progression of patellofemoral arthritis.
The frequency of recurrent dislocation after acute patellar dislocation was reported to be 40–60% with conservative treatment and 10–30% with operation. The most common causes are reported to be extensor mechanism disorders such as impairment of soft-tissue restraints, patella alta, genu valgum, and malrotation of the lower extremity [36, 37]. We excluded patients who needed distal realignment surgery due to patella alta and an increased Q-angle.
Although many proximal realignment operations have been proposed, there is no consensus on the most effective treatment. With the initial arthroscopic procedure for patellar dislocation as reported by Yamamoto [45], arthroscopy has been used either directly or indirectly in the treatment of patellar dislocation. After this technique, an all-inside technique was also introduced [3, 22]. However, in comparison with the all-inside technique, the procedure of mini-open medial plication and lateral release has the technical advantages of being a simple procedure and requiring a shorter operation time. This procedure also has an advantage with regard to dynamics in medial plication balancing, as the tensioning point is not from the front (anterior portal) but rather from the medial portion of the patella. Also, the procedure maintains a cosmetic advantage as it makes an incision smaller than 2 cm, except for the arthroscopic portal.
Ever since Warren et al. [43] reported on the medial patellofemoral ligament (MPFL) as the main static restraint against lateral dislocation of the patella in 1979, MPFL repair or reconstruction has been widely used [6, 18, 21, 31]. MPFL repair often may not be possible because it may be difficult to identify this ligament in chronic cases. In our case series, there were no cases possibly identified for MPFL repair. Arendt et al. [6] also reported that isolated MPFL repair for the treatment of recurrent patellar dislocations showed a high failure rate. Also, MPFL reconstruction has some limitations, including the lack of consensus over the insertion isometric point and graft choice [5, 30, 38]. It is also a technically demanding procedure, especially in terms of appropriate tensioning. Some investigators think medial plication, rather than MPFL repair, has greater mechanical strength as it grasps the entire width of the medial retinaculum, including the MPFL [27]. The two procedures cannot be directly compared by simply reviewing previous studies due to their differences in materials and methods of analysis. However, previous studies have reported good results with medial plication (Table 1), and this study has shown a similar functional score in comparison to previous ligament reconstruction surgery studies (Table 2). The long-term results of MPFL reconstruction by Nomura et al. reported a subjective satisfaction of 87.5% and a recurrence rate of 9.1%. Similarly, our study resulted in a subjective satisfaction of 90.3% and a recurrence rate of 9.7%.
Compared with ligament reconstruction surgery, one of the benefits of the lateral release and medial plication procedure is that it has a cosmetic advantage. Second, intra-articular lesions can be treated simultaneously. Third, postoperative pain and joint stiffness are much less severe than those after reconstruction surgery [24]. Last, its technique is comparatively simple, and it is easy to determine congruent tracking because the position and tracking of the patella are easily corrected during the procedure. Although some investigators argued that congruent tracking must be determined through arthroscopy [4, 27], we determined the final congruent tracking with flexion from 45° to 90° with the naked eye after tourniquet deflation. We made this determination based on the notion that patellofemoral tracking can change while the joint is inflated by fluid and the thigh is pressed by tourniquet and an arthroscopic view may be limited by bleeding after lateral release. Previous studies reported excessive medial plication [26], and we also had two cases that seemed to have been excessively corrected. This overcorrection disappeared spontaneously during the follow-up period (Fig. 2).
a and b A preoperative radiograph and a postoperative merchant view radiograph of a 19-year-old woman show overtightening after surgery. c The radiographs show that medial tightness has been naturally resolved 3 months after surgery. d A radiograph taken 9.5 years after surgery demonstrates that patellofemoral joint alignment is maintained. There is no evidence of osteoarthritis
Many investigators reported that a realignment procedure is likely to cause arthritis in the patellofemoral and femorotibial joints [9, 23, 34]. Nomura et al. [29] reported two cases of arthritis in the femorotibial and patellofemoral joints after MPFL reconstruction surgery. In this study, all three observers reported that five patients were found with progression of patellofemoral joint arthritis, but we did not deem the progression of this arthritis as a result of the surgical procedure because femorotibial joint arthritis had also progressed at the same time. We thought that realignment surgery increased the contact pressure of the patellofemoral joint more than that of the femorotibial joint. If arthritis had progressed in both joints at the same time, we believe that age, genetics, and the level of physical activity might have caused arthritis to develop in both joints rather than the surgical treatment. Nomura et al. reported progression of arthritis in both joints in two patients. They conjectured differently from us that realignment surgery might have equally affected both joints.
Trochlear dysplasia is one of the causes of patellar instability [16]. Nelitz et al. [28] proposed that trochlear dysplasia is a major risk factor for failure of operative stabilization of recurrent patellofemoral instability in a recent study. In the current study, two trochlear dysplasia patients had recurrence after surgery. Trocheoplasty was developed as a treatment for trochlear dysplasia [19, 42]; however, the procedure can disrupt cartilage surfaces and alter contact pressure, potentially leading to patellofemoral arthritis. As shown in this study, not all patients with dysplasia had recurrence. Therefore, it is difficult to say that dysplasia is the only cause of recurrence. Generalized laxity was also considered to be one of the risk factors for patellar instability; however, Atkin et al. [7] reported that laxity was not related to patellar dislocation. In the current study, one patient among those with recurrence had generalized laxity. However, we were unable to analyze the data regarding generalized laxity as laxity data for all patients were not available.
Some limitations of this study must be taken into consideration. First, this study lacks more detailed and consistent imaging modalities such as CT scans and/or MRI. These imaging modalities are more reliable than Q-angle for analyzing extensor mechanism alignment and simple radiography for analyzing trochlear dysplasia [28]. Second, this study is a retrospective case series without a control group. Third, all cases were performed at a single general hospital by a single surgeon. Lastly, this study presents a lower percentage of trochlear dysplasia (52%) than that reported by Dejour et al. [16] (96%). This is, however, a meaningful weakness because trochlear dysplasia can affect results. This may be attributable to our exclusion criteria, demographic differences between countries, or limitations in the case series. We are unable to explain the exact cause of the lower percentage of trochlar dysplasia.
Conclusions
Percutaneous lateral release and medial plication showed satisfactory results with limited morbidity in the long-term follow-up. This traditional method remains a simple and effective treatment modality compared with MPFL reconstruction surgery.
References
Aglietti P, Pisaneschi A, Buzzi R, Gaudenzi A, Allegra M (1989) Arthroscopic lateral release for patellar pain or instability. Arthroscopy 5:176–183
Ahmad CS, Brown GD, Stein BS (2009) The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med 37:2021–2027
Ahmad CS, Lee FY (2001) An all-arthroscopic soft-tissue balancing technique for lateral patellar instability. Arthroscopy 17:555–557
Ali S, Bhatti A (2007) Arthroscopic proximal realignment of the patella for recurrent instability: report of a new surgical technique with 1 to 7 years of follow-up. Arthroscopy 23:305–311
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10:215–220
Arendt EA, Moeller A, Agel J (2011) Clinical outcomes of medial patellofemoral ligament repair in recurrent (chronic) lateral patella dislocations. Knee Surg Sports Traumatol Arthrosc 19:1909–1914
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C (2000) Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28:472–479
Balcarek P, Jung K, Ammon J, Walde TA, Frosch S, Schuttrumpf JP, Sturmer KM, Frosch KH (2010) Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med 38:2320–2327
Barbari S, Raugstad TS, Lichtenberg N, Refvem D (1990) The Hauser operation for patellar dislocation. 3–32-year results in 63 knees. Acta Orthop Scand 61:32–35
Buchner M, Baudendistel B, Sabo D, Schmitt H (2005) Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med 15:62–66
Carter C, Wilkinson J (1964) Persistent joint laxity and congenital dislocation of the hip. J Bone Joint Surg Br 46:40–45
Christiansen SE, Jacobsen BW, Lund B, Lind M (2008) Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy 24:82–87
Conlan T, Garth WP Jr, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75:682–693
Deie M, Ochi M, Adachi N, Shibuya H, Nakamae A (2011) Medial patellofemoral ligament reconstruction fixed with a cylindrical bone plug and a grafted semitendinosus tendon at the original femoral site for recurrent patellar dislocation. Am J Sports Med 39:140–145
Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 15:39–46
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Dodson CC, Shindle MK, Dines JS, Altchek DW (2010) Arthroscopic suture anchor repair for lateral patellar instability. Knee Surg Sports Traumatol Arthrosc 18:143–146
Donell ST, Joseph G, Hing CB, Marshall TJ (2006) Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee 13:266–273
Drez D Jr, Edwards TB, Williams CS (2001) Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy 17:298–306
Fisher B, Nyland J, Brand E, Curtin B (2010) Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy 26:1384–1394
Halbrecht JL (2001) Arthroscopic patella realignment: an all-inside technique. Arthroscopy 17:940–945
Hampson WG, Hill P (1975) Late results of transfer of the tibial tubercle for recurrent dislocation of the patella. J Bone Joint Surg Br 57:209–213
Henry JH, Goletz TH, Williamson B (1986) Lateral retinacular release in patellofemoral subluxation. Indications, results, and comparison to open patellofemoral reconstruction. Am J Sports Med 14:121–129
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Miller JR, Adamson GJ, Pink M, Fraipont MJ, Durand P (2007) Arthroscopically assisted medial reefing without routine lateral release for patellar instability. Am J of Sports Med 35:622–629
Nam EK, Karzel RP (2005) Mini-open medial reefing and arthroscopic lateral release for the treatment of recurrent patellar dislocation: a medium-term follow-up. Am J Sports Med 33:220–230
Nelitz M, Theile M, Dornacher D, Wolfle J, Reichel H, Lippacher S (2011) Analysis of failed surgery for patellar instability in children with open growth plates. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-011-1599-5
Nomura E, Inoue M, Kobayashi S (2007) Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 35:1851–1858
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13:510–515
Panagopoulos A, van Niekerk L, Triantafillopoulos IK (2008) MPFL reconstruction for recurrent patella dislocation: a new surgical technique and review of the literature. Int J Sports Med 29:359–365
Schottle PB, Fucentese SF, Romero J (2005) Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc 13:516–521
Schottle PB, Scheffler SU, Schwarck A, Weiler A (2006) Arthroscopic medial retinacular repair after patellar dislocation with and without underlying trochlear dysplasia: a preliminary report. Arthroscopy 22:1192–1198
Sillanpaa PJ, Mattila VM, Visuri T, Maenpaa H, Pihlajamaki H (2011) Patellofemoral osteoarthritis in patients with operative treatment for patellar dislocation: a magnetic resonance-based analysis. Knee Surg Sports Traumatol Arthrosc 19:230–235
Small NC, Glogau AI, Berezin MA (1993) Arthroscopically assisted proximal extensor mechanism realignment of the knee. Arthroscopy 9:63–67
Smith TO, Davies L, Chester R, Clark A, Donell ST (2010) Clinical outcomes of rehabilitation for patients following lateral patellar dislocation: a systematic review. Physiotherapy 96:269–281
Smith TO, Song F, Donell ST, Hing CB (2011) Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc 19:988–998
Steensen RN, Dopirak RM, McDonald WG 3rd (2004) The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med 32:1509–1513
Steiner TM, Torga-Spak R, Teitge RA (2006) Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med 34:1254–1261
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Vainionpaa S, Laasonen E, Silvennoinen T, Vasenius J, Rokkanen P (1990) Acute dislocation of the patella. A prospective review of operative treatment. J Bone Joint Surg Br 72:366–369
von Knoch F, Bohm T, Burgi ML, von Knoch M, Bereiter H (2006) Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br 88:1331–1335
Warren LF, Marshall JL (1979) The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am 61:56–62
Wiberg G (1941) Roentgenographic and anatomic studies on the patellofemoral joint: with special reference to chondromalacia patella. Acta Orthop Scand 12:319
Yamamoto RK (1986) Arthroscopic repair of the medial retinaculum and capsule in acute patellar dislocations. Arthroscopy 2:125–131
Conflict of interest
There is no conflict of interest to disclose for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, JJ., Lee, SJ., Won, YG. et al. Lateral release and medial plication for recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc 20, 2438–2444 (2012). https://doi.org/10.1007/s00167-012-1937-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1937-2