Abstract
Purpose
The clinical role of patellofemoral (PF) osteoarthrosis (OA) in the outcome after PF stabilizing surgery is poorly understood. The study hypothesis was that PF cartilage lesions and OA are associated with a poor long-term outcome after PF stabilizing surgery.
Methods
The study cohort included thirty-seven patients who underwent PF stabilizing surgery by traditional nonanatomic procedures and were evaluated a minimum of 10 years (range 10–21) after surgery. PF OA was assessed by magnetic resonance (MR) images and plain radiographs obtained at follow-up. Median patient age at follow-up was 33 years (29–43).
Results
At the final follow-up, PF full-thickness cartilage lesions were observed on MR images in 29 (78%) patients. Only 46% of the patients reported satisfaction at follow-up, and dissatisfaction was associated with PF OA (full-thickness articular cartilage loss on MR images; P = 0.022). Especially high incidence, 89%, of medial patellar facet cartilage lesions were found among the patients dissatisfied with the result (16/18 patients) (n.s.). Eight (22%) of the 37 patients reported recurrent patellar instability episodes at follow-up. Median Kujala score was 83 points (range 55–98).
Conclusion
Patellofemoral OA is a significant long-term risk of nonanatomic surgery for patellar instability and has a greater impact on subjective outcome than residual instability more than 10 years after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary patellar dislocation may be followed by recurrent dislocations and painful subluxation [8]. Recurrent symptoms may require surgery to stabilize the patella. Although surgery can prevent further dislocation and subluxation, it may not prevent patellofemoral (PF) pain and degenerative changes in the PF joint are common, especially after some surgical procedures [11, 14, 19]. Nonsurgical treatment may also lead to PF articular cartilage wear [14], but the process is poorly understood. The role of the initial chondral injury and bone bruises is also not known. In long term, comparative studies of the development of PF osteoarthrosis (OA) do not clearly indicate whether nonsurgical or surgical management are causative factors [14, 20, 21]. In addition, it is not known how articular cartilage lesions and PF OA after patellar stabilizing surgery impacts patient satisfaction in long-term follow-up.
The aim of this study was to evaluate the association of articular cartilage lesions and PF OA with patient satisfaction with a follow-up time of at least 10 years after surgery in patients who underwent traditional nonanatomic stabilizing surgery using either the Goldthwait [6] (transfer of the lateral half of the patellar tendon to medial tibia) or Krogius [12] (medial retinacular imbrication) method. The study hypothesis was that PF OA would be frequently found and associated with poor clinical long-term outcome. Outcome measures included recurrent instability rate, subjective satisfaction with the affected knee, and development of PF OA determined by plain radiographs and magnetic resonance (MR) imaging.
Materials and methods
As the purpose of the study was to evaluate whether PF OA explains patient dissatisfaction over the long term, only those who underwent traditional nonanatomic PF stabilizing surgery more than 10 years ago were considered to be included in this study. Based on previous reports, we expected to see OA characteristics after these nonanatomic procedures. The two most frequently performed traditional patellae stabilizing procedures at the study hospital were the Goldthwait and Krogius methods, and thus only those were included and those who underwent any other procedures were excluded from the study. To identify the patients, a computer search of the medical records for patients operated on for recurrent patellar dislocation at the study hospital from 1986 through 1997 was first performed. After the database search, to be included in the study, a well-documented patient history prior to surgery was required to be found in the medical records and preoperative radiographs were required to be available to assess the preoperative status of the PF joint. The Institutional Review Board and Medical Ethics Committee of the study hospital approved the study and written informed consent was obtained from each patient participated in the study.
A total of 52 cases with recurrent patellar dislocation that underwent a patellar stabilizing procedure by either the Goldthwait or Krogius methods with sufficient data available were enrolled in the study. All 52 study subjects were male military recruits treated during or before their military service period. Of the 52 patients invited to the follow-up visit, 37 (71%) participated in the follow-up examination. Baseline characteristics of the patients are shown in Table 1. Preoperative radiographs were used to assess the characteristics of the PF joint and as a comparison to follow-up radiographs to assess the development of OA. Because of the extensive follow-up time, preoperative MRIs were not available, as high-intensity scans only became popular in late 1990s.
All surgical procedures were performed by senior orthopedic surgeons. The Goldthwait procedure was performed according to the original technique. The lateral half of the patellar tendon was transferred behind the medial half of the tendon, and the transferred lateral half was attached to the medial tibia to prevent lateral dislocation. Similarly, the Krogius procedure was performed according to the original technique in which a strip of the medial retinaculum was first elevated and the lateral retinaculum was sectioned. Then the retinacular strip was transferred into the opening in the lateral retinaculum, and the medial incision was closed. Postoperative treatment included a cylinder cast or a posterior splint for a time of 2 to 6 weeks.
Follow-up examination was performed at a minimum of 10 years (median, 12 years; range, 10–21 years) postoperatively. A clinical examination and a systematic patient interview by the authors was performed using the anterior knee symptom scale developed by Kujala et al with a maximum possible score of 100 points (no symptoms). Regarding the recurrent instability after surgery, those who had clinically documented patellar redislocation(s) or reported several painful subluxation complaints at the follow-up were considered as having patellar instability. Patients were also asked if they were satisfied with the result or dissatisfied due to instability or pain in the affected knee. Physical activity assessment was performed using the Tegner [22] activity level scale. The Hughston Visual Analogue Scale (0 = no pain, 100 = most severe pain) was used to assess the patient’s subjective pain in the affected knee at follow-up.
To assess the PF joint articular cartilage, plain radiographs and MR images of the operated knee were obtained at the final follow-up, and preoperative radiographs were re-evaluated. Anteroposterior, lateral, and PF axial radiographs were taken at follow-up. Axial Merchant [15] views were used to analyze the medial and lateral PF joint spaces. The radiographic parameters measured on the axial radiographs included the sulcus angle and Caton-Dechamps [2] index for patellar height measured on the lateral views to detect patella alta. Patella alta was defined as a ratio greater than 1.2 [2]. Trochlear dysplasia was classified as described by Dejour et al. [5]. The severity of OA in the PF joint was assessed from plain radiographs by a senior radiologist specializing in musculoskeletal imaging who was not involved with the patient care. OA severity was graded from I to IV using the classification of Iwano et al. [9]: Stage 1 representing remodeling, Stage II joint narrowing (>3 mm), Stage III joint narrowing (<3 mm), and Stage IV more severe destruction (bone on bone).
In addition, at follow-up, MR imaging was performed to determine the location and severity of possible cartilage defects in the PF joint. MR imaging was performed on 34 of the 37 patients at follow-up; 2 patients were unable to undergo MR imaging and 1 severely obese patient could not fit into the MR imaging scanner. All MR images were obtained using a 1.0-Tesla MR imaging scanner (Signa Horizon; GE Medical Systems, Milwaukee, WI). A musculoskeletal radiologist reviewed all MR images. Four PF articular surfaces were analyzed, the medial and lateral patellar facets, and the anteromedial and anterolateral condyles of the femur. The trochlear groove (TG) region was thus divided into the lateral or medial side, based on the most affected surface area from the midline drawn based on the deepest part of the TG. Cartilage lesions were classified according to their depth using the numeric grading system developed by the International Cartilage Repair Society (ICRS) [1]. Grade I (softening) lesions were excluded because of the inaccuracy in differentiating these lesions from normal (ICRS Grade 0) cartilage by MR imaging. Thus, only Grade II to IV lesions were documented to avoid false-positive MR imaging findings [1]. ICRS Grade II refers to articular cartilage defects extending down to less than 50% of the cartilage depth, Grade III defects extend to deeper than 50% of the cartilage depth, and Grade IV defects refer to full-thickness articular cartilage loss.
Statistical methods
The Kruskal–Wallis test was used to test differences in nonparametric ordinal data, and independent samples t tests were used to test differences in continuous normally distributed data between the groups. Differences in the two-way tables were determined with the Pearson’s chi-square test or Fisher’s exact test when the expected cell count was less than five. Significance was set at P ≤ 0.05. SPSS 14.1 for Windows software (SPSS Inc, Chicago, IL) was used for the statistical analysis.
Results
Among all study subjects, eight (8/37, 22%) patients reported patellar instability (redislocation or subluxation) at the final follow-up. The satisfaction rate for the long-term result of surgical treatment was 46% (17/37) based on a subjective response to the query regarding satisfaction with the results in the affected knee, and 54% responded that they were dissatisfied due to patellar complaints. The results did not differ based on the surgical technique employed. Characteristics of the clinical findings between the methods of treatment are shown in Table 2.
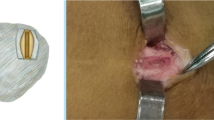
At the time of the initial surgery, none of the patients had PF OA characteristics in plain radiographs. With respect to the radiologic characteristics measured (Table 1), patella alta was observed in 29% (15/52) of patients and trochlear dysplasia was seen in 70% (26/37) of the controlled patients, mostly type A (17 patients) or B (7 patients). Type C in only 2 patients and 9 had normal trochlear morphology. At the final follow-up examination, plain radiographs demonstrated substantial PF OA characteristics including Iwano stage IV bone on bone PF OA in six patients (Fig. 1), three patients from each surgical procedure group.
Characteristics of the articular cartilage lesions detected by MR imaging within the PF joint are listed in Table 3. If both patellar and femoral sides of the PF joint were significantly affected, the Grade III or Grade IV lesions were most frequently on the lateral patellar facet (Fig. 2) and on the lateral side of the femoral trochlea. Interestingly, of the 25 knees in which only the patellar side was significantly affected, chondral lesions were observed on the medial patellar facet in all cases (Fig. 3), but less common on the lateral patellar facet, perhaps due to overtight medial restraints. There was also a noticeable high incidence of severe medial patellar facet articular cartilage lesions found among those who were subjectively dissatisfied with the knee, as shown in Table 3. The surgical method was not a contributing factor in the PF lesions found by MR imaging, as tested by comparing patients treated with each method.
To summarize the MR imaging findings, PF articular cartilage loss was frequently observed, with or without reported patellar instability (redislocation or subluxation). Though all patients who had an unstable patella at follow-up showed full-thickness articular cartilage lesions detected by MR imaging, the rate of the lesions indicated an even distribution between stable and unstable patellae. Thus, PF OA was not statistically associated with patellar instability at the final follow-up (Table 3), but dissatisfaction with the long-term result of the surgery was associated with PF OA (full-thickness articular cartilage loss on MR images and Iwano stage IV PF OA in plain radiographs; P = 0.022).
Discussion
The main findings of this study were that the PF OA is frequently found in long-term follow-up of nonanatomic patellar stabilizing procedures and poor subjective result is associated with PF OA. Especially high incidence, 89%, of medial patellar facet cartilage lesions was found among the patients dissatisfied with the result, indicating medial cartilage wear as a possible consequence of the surgery. To our knowledge, this study is the first to explore the long-term effect of PF OA assessed by MR imaging in relation to the subjective and objective clinical results of PF surgery. Subjective satisfaction with the surgery was reported by only 46% of the patients, and poor clinical results were associated with the presence of PF OA, indicating that in addition to recurrent patellar instability, PF OA played a significant role in patient satisfaction in the long run. PF OA was similarly observed in patients with or without patellar instability at the follow-up evaluation.
Recurrent patellar subluxation or dislocation may predispose patients to the development of PF OA [13]. Similarly, it might be that the nonanatomic procedures may result in uncontrolled cartilage forces especially in medial patellar facet affecting the deterioration of the PF joint cartilage due to increased pressure in the PF joint [17]. Also, the first dislocation, or any traumatic dislocation episode, produces bone bruises and may also cause cartilage damage, but this pathologic process in not well understood. Despite the various potential etiologies of PF OA, the results of this study suggest that a stable patella does not prevent the development and progression of PF OA, because the MR images obtained at follow-up showed full-thickness PF articular cartilage loss in 27 patients (78%), and all of the patients had at least ICRS Grade II PF chondral lesions 10 to 21 years after surgery. Thus, the surgical stabilization procedures used in this study did not appear to minimize the development of PF OA.
The main limitation of this study was the lack of precise information of the preoperative PF chondral status. Because MR imaging was not available at the time the surgery was performed, we used preoperative radiographs for comparison. The lack of female subjects limits the conclusions, although it is not known if PF OA development differs between the sexes. A nonsurgery control group would have produced additional evidence about the impact of surgery on the development of PF OA. Also, the group of four people who underwent subsequent surgery is considered a limitation regarding the evaluation of PF OA progression, even though they were considered to be included representing half of the patients with recurrent instability after stabilizing surgery. The strengths of this study include the substantial follow-up time and well-documented patient history, including the preoperative radiographs. Furthermore, as a result of the health requirements for military service, study subjects comprised healthy young male adults without significant knee complaints prior to entering military service. Although the subjects experienced patellar instability that interrupted their military service, the physical fitness at the time of surgery can be considered relatively good, as they were considered to be capable of undergoing military training.
Previously published data of patients with PF OA changes after surgically treated patellar dislocation report proportions between 4 and 70% [18, 20]. Crosby and Insall reported a disturbingly high rate of late PF OA in patients treated with the Hauser procedure [4]. In another study of the Hauser procedure, poor subjective results were always associated with PF OA [11]. The Goldthwait procedure is considered to be a reliable method, [10, 20] but a significant risk of OA was reported in a recent study in which the Goldthwait procedure was compared with medial patellofemoral ligament (MPFL) reconstruction [20]. The Krogius and Goldthwait procedures were previously compared in a study by Jalovaara et al. [10] in which the patients were followed for 3 to 7 years and the authors did not recommended the Krogius method due to an unacceptably high (42%) rate of recurrent instability. The development of PF OA was not assessed in their study. In this study, deterioration of the articular cartilage in the PF joint seen in MRI appeared to have progressed quite heavily before PF OA was graded as severe on the plain radiographs. A notable limitation of the previous studies is that only plain radiographs were used.
Nonsurgical long-term results have been described in only a few studies. Cofiel and Bryan [3] and Mäenpää and Lehto [13] described the results of 50 and 100 nonsurgically treated patellar dislocations with mean follow-up times of 10 and 13 years, respectively. Both studies also compared nonsurgical and surgical treatments and reported better outcome after nonsurgical treatment. The surgical methods used in those studies were also traditional realignment procedures that are no longer commonly performed. There is some evidence that the severity of PF cartilage lesions may not correlate well with the subjective results or PF scoring [16]. Few patients in this study had a reasonably well-preserved PF joint, but we could not find any clinical signs to explain why some PF joint cartilage was preserved much better than others.
As the main finding of the study was that PF OA has a significant role in patient satisfaction in the long run, we suggest further studies of modern anatomical surgical techniques including MPFL reconstructions [7] regarding the potential effect on preserving PF articular cartilage.
Conclusion
After a follow-up ranging from 10 to 21 years after surgery, PF OA characteristics were frequently observed on MR images obtained at follow-up. Full-thickness PF articular cartilage defects were detected in up to 78% of the patients, most frequently in the medial patellar facet, indicating that PF OA has significant role in long-term clinical result of the treatment and may be a consequence of nonanatomic surgical procedures. There is currently no clear method to prevent the development of PF OA in patients with patellar instability despite the fact that patellar stability can be achieved by various surgical methods.
References
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A (Suppl 2):58–69
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317–325
Cofield RH, Bryan RS (1977) Acute dislocation of the patella: results of conservative treatment. J Trauma 17:526–531
Crosby EB, Insall J (1976) Recurrent dislocation of the patella. Relation of treatment to osteoarthritis. J Bone Joint Surg Am 58:9–13
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Goldthwait JE (1903) Slipping or recurrent dislocation of the patella: with the report of eleven cases. American Journal of Orthopedic Surgery 1:293–308
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Hughston JC (1968) Subluxation of the patella. J Bone Joint Surg Am 50:1003–1026
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res 252:190–197
Jalovaara P, Seppanen-Lehmonen T, Lindholm RV (1988) Krogius and Roux-Goldthwait operations for recurrent patellar dislocation. Acta Orthop Belg 54:380–383
Juliusson R, Markhede G (1984) A modified Hauser procedure for recurrent dislocation of the patella. A long-term follow-up study with special reference to osteoarthritis. Arch Orthop Trauma Surg 103:42–46
Krogius A (1904) Zur Operative Behandlung der habituellen Luxation der Kniescheibe. Zentralbl Chir 31:254–257
Maenpaa H, Lehto MU (1997) Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med 25:213–217
Maenpaa H, Lehto MU (1997) Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res 339:156–162
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56:1391–1396
Niskanen RO, Paavilainen PJ, Jaakkola M, Korkala OL (2001) Poor correlation of clinical signs with patellar cartilaginous changes. Arthroscopy 17:307–310
Nomura E, Inoue M (2004) Cartilage lesions of the patella in recurrent patellar dislocation. Am J Sports Med 32:498–502
Nomura E, Inoue M, Kobayashi S (2007) Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 35:1851–1858
Rantanen J, Paananen M (1996) Modified Hauser operation for patellar instability. Immediate mobilization of 35 knees, a 5–8 year follow-up study. Acta Orthop Scand 67:455–458
Sillanpaa P, Mattila VM, Visuri T, Maenpaa H, Pihlajamaki H (2008) Ligament reconstruction versus distal realignment for patellar dislocation. Clin Orthop Relat Res 466:1475–1484
Sillanpaa PJ, Mattila VM, Maenpaa H, Kiuru M, Visuri T, Pihlajamaki H (2009) Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. J Bone Joint Surg Am 91:263–273
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Acknowledgments
We gratefully acknowledge the surgical expertise of Olli Kiviluoto, MD, PhD (Central Military Hospital, Helsinki, Finland) and the radiologic expertise of Martti Kiuru, MD, PhD (Central Military Hospital, Helsinki, Finland).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sillanpää, P.J., Mattila, V.M., Visuri, T. et al. Patellofemoral osteoarthritis in patients with operative treatment for patellar dislocation: a magnetic resonance-based analysis. Knee Surg Sports Traumatol Arthrosc 19, 230–235 (2011). https://doi.org/10.1007/s00167-010-1285-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1285-z