Abstract
Purpose
The purpose of our study was to evaluate the initial fixation strength of bridging techniques compared to other suture techniques for rotator cuff repair using a biomechanical animal model, which incorporated pretesting of intact tendons.
Methods
Seventy-six fresh bovine shoulders were used for testing seven suture configurations including simple suture (SS), mattress suture (MS), Mason-Allen (MA), modified double row (mDR), SpeedBridge (SpB), SpeedBridge with medial fixation (mSpB), and double-mattress SutureBridge (dmSuB) techniques. Cyclic loading was performed with all intact bone-tendon complex before (pretest) and after repair of the tendon (main test) at the level of 10 and 180 N at 100 Hz with displacement-controlled ramps of ±33 mm/s. The pretest was stopped after 200 cycles. For the main test, the loading scheme was continued for a maximum of 500 cycles or until failure.
Results
The mean elongation of all 76 intact tendons measured at the pretest was 3.8 ± 0.6 mm (2.4–5.4 mm). No differences of gap formations at the 1st cycle were detected between SS, MS, MA, and mDR. SpB showed significant higher gap formations compared to all other suture techniques (p = 0.001). No significant differences were detected between mSpB and dmSuB, whereas both techniques were significant different when compared to the other groups (p < 0.05).
Conclusions
In this study, results showed that bridging techniques with medial fixations have superior initial repair strength compared to other suture techniques. Knowledge of initial fixation strength of rotator cuff repair techniques may be of informative value to the surgeon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arthroscopic rotator cuff repair is one of the most common surgical procedures in the shoulder. Despite technical improvements, retear rates are still high [2, 14]. Healing of the rotator cuff depends not only on biological factors such as the quality of tendons and bones, blood supply to the cuff and the general state of health of a patient, but also on material and fixation methods. Failure of rotator cuff repair can be caused by tissue laceration at the tendon-suture interface as well as anchor pullout, knot slippage, suture breakage or suture pullout. However, repair failures commonly occur in the early postoperative phase, while load transfer is entirely carried through the fixation.
In the past 10 years, new suture materials and tendon-bone fixation techniques approached in order to increase the mechanical strength of the primary fixation: starting with single-row repairs [14, 17] to footprint reconstruction [9, 15, 18, 21, 22, 28, 29, 30] and more recently to knotless double-row footprint reconstruction [3]. Recent biomechanical studies demonstrated that the mechanical strength of a double-row cuff repair was superior to a single-row repair [18, 22, 26, 35]. However, other reports indicated no differences between the two techniques [24, 25]. A comparison of varying biomechanical protocols of tendon fixation techniques including various variables such as donors of specimen, storage of samples, anchor materials, methods to clamp samples, as well as cyclic loading schemas, is difficult. Nevertheless, biomechanical studies are necessary especially to test initial fixation strengths after rotator cuff repairs.
The purpose of the present study was to assess initial strengths of seven suture techniques using a biomechanical model, which incorporated pretesting of intact tendons. We hypothesized that bridging techniques would demonstrate superior initial fixation strengths compared to other suture techniques.
Materials and methods
A total of 76 fresh harvested bovine shoulders were obtained from a local abattoir. Each shoulder was dissected so that the infraspinatus muscle and tendon insertion was left intact, while all other soft tissue was removed. Before pretesting, the positions of the clamps for bone and tendon were marked to give the same clamping conditions for the main test. The pretest was performed to obtain biomechanical properties of the intact samples. Each shoulder was pretested for approximately 20 min (Fig. 1). Subsequently, the samples were stored in the refrigerator at 4°C until surgical manipulation with a maximum storage time of 5 h. The bovine infraspinatus tendons were about 3 mm thick and 35 mm in width. The tendon was sharply transected from the bone, and a rotator cuff tear was simulated by resecting the tendon from the lateral edge to a width of 20 mm.
Suture configuration
Each defect was repaired under direct vision by the same orthopedic surgeon (B.K.). Tendons were re-attached to the bone with bioabsorbable anchors (Arthrex, Naples, FL, USA). For the bone-tendon complex, a serrated clamp was used to attach the bone to the mounting plate of the test equipment. To simulate a physiological direction of the load applied to the bone-tendon configuration, the angel was individually adjusted with approximately 45° for each specimen (Fig. 2).
The tendons of the 1st group (n = 13) of specimens were repaired using simple sutures (SS). Two double-loaded 5.5-mm Bio-Corkscrew suture anchors (Arthrex) were inserted in a parallel line to the tendon edge with a center-to-center distance of approximately 1.5 cm, and four simple stitches were performed to restore the footprint (Fig. 3a).
Group 2 (n = 16) was repaired using a mattress sutures (MS) configuration (Fig. 3b) with two double-loaded 5.5-mm Bio-Corkscrew suture anchors inserted in a parallel line to the tendon edge with a center-to-center distance of approximately 1.5 cm. With four mattress sutures, one overlapping the other, the tendon was fixed to the bone.
The 3rd group (n = 17) was repaired with the modified Mason-Allen (MA) technique (Fig. 3c) according to Scheibel [34]. Two double-loaded 5.5-mm Bio-Corkscrew suture anchors were inserted in a parallel line to the tendon edge with a center-to-center distance of approximately 1.5 cm. Two parallel mattress sutures, one from each anchor, were tied with a simple stitch.
Group 4 (n = 10) was repaired with a modified double-row technique (Fig. 3d), whereat two medial placed double-loaded 5.5-mm Bio-Corkscrew suture anchors with a center-to-center distance of approximately 1.5 cm and one lateral double-loaded 5.5-mm Bio-Corkscrew suture anchor were placed in middle of the medial suture anchors and again with distance of approximately 1.5 cm of each anchor describing a triangle. The tendon was fixed with four mattress sutures from the medial row. And from the lateral anchor, two oblique stitches were performed running across each pair of mattress sutures.
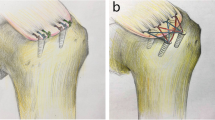
For the 5th group (n = 10) of specimens, the SpeedBridge (SpB; Arthrex) technique (Fig. 3e) was used with two 5.5-mm Bio-SwiveLock C anchors (Arthrex) single-loaded with FiberTape (Arthrex) inserted at the medial aspect of the footprint parallel to the tendon with a center-to-center distance of approximately 1.5 cm. Both tails of the FiberTape were passed simultaneously through the tendon tissue, no knot was tied, and the free tails of the stitches were fixated at the lateral edge of the footprint using another two 5.5-mm Bio-SwiveLock C anchors.
For group 6 (n = 5), a modification of the SpeedBridge (mSpB) technique (Fig. 3f) was used. In addition to the technique described above, two limbs of #2 FiberWire (Arthrex) of each medial SwiveLock anchor were passed through the tendon and tied in a mattress configuration.
Group 7 (n = 5) was the double-mattress SutureBridge [30] (dmSuB) technique (Fig. 3g). Two double-loaded 5.5-mm Bio-Corkscrew suture anchors loaded with #2 FiberWire were inserted parallel to the tendon with a center-to-center distance of approximately 1.5 cm. Each suture from each anchor was passed through the tendon in a mattress stitch configuration. Knots were tied, and one suture tail of each knot was removed. The remaining tails were fixated to the lateral end of the tendon crisscrossing the inner suture limbs using two 5.5-mm Bio-SwiveLock C anchors.
All sutures, with the exception of the knotless techniques, were tied in an arthroscopic way with the Duncan loop [16].
Cyclic loading
After surgical repairs, a servo-hydraulic material testing machine (DLFV-250/DZ-10-D, Walter&Bai AG, Switzerland) was used to cycle specimens. For the pretest and main test, cyclic loading was performed at the level of 10 and 180 N at 100 Hz with displacement-controlled ramps of ±33 mm/s [4, 5]. The period of each cycle was 5.0 s, approximately 2.5 s for each level. The loading scheme was stopped at 200 cycles for the pretest. For the main test, cyclic loading was continued for a maximum of 500 cycles. We set the endpoint at 500 cycles (1) because we noticed a plateau effect (a typical pattern in material testing) after certain numbers of cycles while testing the first few configurations, (2) because of the expanded time frame with more cycles for each test, and (3) to be able to make a direct comparison between weaker and stronger configurations. The load-to-failure measurement has not been included into our results, because we continued cyclic loading for more than 2,500 cycles for the first few configurations. Failure was defined as tear or when reaching 10-mm gap formation.
Evaluation of data
Elongations (pretest) and gap formations (main test) were measured using the internal position measurement system of the testing machine and the bending of the bone with an external dial gauge. According to a previous study, both devices performed measurements with an accuracy of 0.002 mm [1]. The built-in load cell had a maximum load of 10 kN with an accuracy of 1 N. Data were recorded at a frequency of 100 Hz using computer software (DIONPro, Walter&Bai AG, Switzerland).
By investigating the intact bone-tendon complex in the pretest, data from natural creep behavior such as tendon’s viscoelasticity and bending of the bone were subtracted from the main test to obtain precise information on the creep behavior due to the weakening of the suture techniques themselves. Cyclic displacement (elongation in mm) of the intact tendon at 200 cycles of the pretest and cyclic displacement (gap formation in mm) of the re-attached tendon at 1,200 and 500 cycle of the main test were recorded. Gap formation was obtained by individual subtracting the mechanical compliance (elongation) of the intact specimen (pretest) from the one of the sutured specimen (main test) [1]. Failures were not included to calculate average gap formation. Some data of SS, MS, MA, and mDR configuration were reported in previous findings [1]. Despite the heterogeneous distribution of this data set with varying numbers of samples in the different suture technique groups, we included measurements into the present study.
Statistical analysis
Based on previous data on gap formation (mean difference was approximately 5 mm [δ = 5] and SD difference was approximately 2 mm [σ = 2]) of our biomechanical investigations, a sample size of at least 5 specimens in each group was calculated to be required to detect a significant difference (90% power, α = 0.05) between two suture techniques. Descriptive statistics were used to present cyclic displacement data. Analysis of variance (ANOVA) was used to compare gap formations between suture technique groups. Additionally, Tukey’s post hoc analysis was use to determine specific differences between two suture techniques. Statistical significance was set at a p value of <0.05.
Results
Pretest data
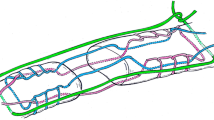
The mean elongation of 76 intact tendons measured at the pretest after 200 cycles was 3.8 ± 0.6 mm (range, 2.4–5.4 mm). The majority of tendons (81%) had an elongation between 3 and 5 mm. All elongation data of the pretest are shown in Fig. 4.
Suture techniques
All suture technique groups including 13 specimens repaired with SS, 16 with MS, 17 with MA, 10 with mDR, 10 with SpB, 5 with mSpB, and 5 with dmSuB passed the 1st cycle. A comparison between the suture technique groups at the 1st cycle showed that the SpB had significant higher gap formations compared to all other suture techniques (p = 0.001). No significant differences were detected between mSpB and dmSuB, whereas both techniques were significant different when compared to the other groups (p < 0.05). Detailed results of comparisons between suture techniques are displayed in Table 1.
The SpB technique was not only the suture configuration with the highest gap formation after 1 (mean 3.4 ± 1.3 mm) and 200 cycles (mean 6.1 ± 2.2 mm), it also was the fixation technique with the highest failures. Seven SpB (70%) configurations failed to reach 200 cycles due to suture cutting through tendons and none reached 500 cycles. A 10-mm failure was detected with 3 MA (18%) at 200 cycles and with 1 SS (8%) at 500 cycles. No failure was detected with MS, mDR, mSpB, and dmSuB suture techniques. The lowest gap formations were detected with bridging techniques with medial fixation (mSpB and dmSuB). Detailed data of all suture techniques are given in Fig. 5.
Box plots of gap formations (mm) of seven suture techniques including simple suture (SS; 1st-200th–500th cycle: n = 13–13–12), mattress suture (MS1; 1st-200th–500th cycle: n = 16–16–16), Mason-Allen (MA; 1st-200th–500th cycle: n = 17–14–14), modified double row (mDR; 1st-200th–500th cycle: n = 10–10–10), SpeedBridge (SpB; 1st-200th–500th cycle: n = 10–3–0), SpeedBridge with medial fixation (mSpB; 1st-200th–500th cycle: n = 5–5–5), and double-mattress SutureBridge (dmSuB; 1st-200th–500th cycle: n = 5–5–5). White boxes represent gap formations after the 1st cycle, light gray boxes after 200 cycles, and dark gray boxes show gap formations after 500 cycles. The median is represented by the line in the box. Circles represent outliers and asterisks are extreme values
Discussion
The present study supports the hypothesis that bridging techniques, with the exception of the knotless bridging technique, showed superior cyclic biomechanical properties to all other suture techniques. Significant differences in construct stability especially regarding the initial strength could be observed when comparing single row, double row, knotless and medial fixated bridging techniques. In particular, application of a knotted medial row (SpeedBridge with medial fixation and double-mattress SutureBridge) significantly increased resistance against gap formation and initial fixation strength compared to single-row techniques (simple suture, mattress suture, Mason-Allen fixation) as well as to the knotless SpeedBridge technique.
In biomechanical testing, loosening and gap formation commonly start at the site of medial tendon perforation due to creation of tendon substance defects during the penetration. Forces arrive at the medial row first, where knots might cause a distribution of the force and therefore lower friction. Hence, in suture configuration without medial fixations, mechanical friction might be increased resulting in early movement and might even tear. The present investigation showed that a notable initial strength was only reached with medial-row fixation and that medially fixated bridging techniques were stronger and less compliant than single-row fixation techniques, which is accordance with previous biomechanical studies [6, 29, 31].
A recent study by Maguire et al. [23] showed that a suture bridge construct with four medial mattress stitches was superior in terms of contact area of the footprint, failure load, and gapping compared to suture bridge configurations with two medial mattress stitches with or without knots. In contrary to our study, they did not find any difference in their so-called standard suture bridge constructs in strength and gap formation and whether the medial row was tied or not. However, it seems reasonable to suppose that the different findings are due to unequal applied loads (100 N compared to the 180 N used in this study).
Results of this study also confirm a recent biomechanical study comparing 2 transosseous-equivalent double-row rotator cuff repair techniques [36]. They detected no major difference in failure load, gap formation and strain patterns between their so-called conventional double-row technique, which is comparable to our double-mattress SutureBridge, and their novel double-row construct, which is identical to our medial fixated SpeedBridge technique. Moreover, we evaluated—as suggested by the group as a next technical step—their novel double-row construct (our knotless SpeedBrigde) and found that the horizontal medial stitch is crucial for construct stability.
Whereas a study by Burkhart and co-workers suggests that standard double-row rotator cuff repair was comparable with a knotless footprint reconstruction with a SwiveLock-FiberChain system in their yield and ultimate loads as well as their cycle displacements [3], a direct comparison of the two knotless techniques was not possible due to the different material used, different mode of lateral fixation and a considerably lower sample size.
Despite that a completely knotless technique without medial-row knots demonstrates compromised biomechanical properties, it may offer several advantages considering biological approaches. As only two tendon perforations for four ends of two FiberTapes are necessary, it may not decrease the intratendinous blood flow as much as after suture bridge transosseous-equivalent fixation [8].
Lower numbers of tendon perforations and avoidance of tendon strangling through medial knots may also lead to lower frequencies of consecutive tendon necrosis around the perforations in the early healing phase. On the other hand, two FiberTapes passed through together might leave major perforations and therefore decrease stability as suggested by a recent study [32]. Further results of the study by Pauly et al. [32] showed that the double-mattress SutureBridge configuration was the most stable biomechanical construct compared to conventional double-row configurations. However, differences in biomechanical protocols (e.g., human vs. animal, frozen vs. fresh, bone cement fixation vs. clamp) may contribute to incomparable results. At this point, we would like to point out the importance of pretesting the intact bone-tendon complex. To our opinion, elongations of the intact tendons ranging from 2 to 5 mm indicate varying tendon qualities. The natural expansion of the human supraspinatus footprint is 7–10 mm [27]. Yet, a 50% of complete failure is commonly defined at 5-mm gap formation [5]. Hence, a 50% of complete failure would have lower gap formations than intact tendon expansion. A variety of donors of shoulders have previously been used including fresh-frozen human shoulders [5, 11, 18, 22, 25, 35], as well as animal tendons such as bovine [20, 24, 33], pig [26] or sheep tendons [10]. A major advantage of our pretesting model excluding tendon qualities is that it can be applied to various cadaveric specimens without influencing suture technique testing. Furthermore, storage of samples until testing such as freezing the samples at −20°C may irreversibly affect the biomechanical quality of the tendons and therefore the suture-anchor system [5, 10, 20, 33]. Pretesting intact, but previously frozen tendons (even human shoulders) may be advisable to exclude such influencing factors. Thus, we suggest that pretesting should be part of biomechanical suture technique testing.
In this study, all knotless suture configurations failed by sutures cutting through the tendons, which might indicate that loading force exceeded friction force.
No differences in gap formation at 1st cycle were detected between single (SS, MS, MA) and common double-row (mDR) techniques, which would confirm clinical findings [7, 12, 15]. Similar results between mattress suture and double row regarding their initial fixation strength may also suggest performing mattress suture constructs as a suitable alternative to the technically quite demanding and time-consuming double-row fixation. A major advantage of the double-mattress SutureBridge repair and the SpeedBridge with medial fixation was the quick and easy surgical performance compared to the modified double-row technique.
Despite many advantages of the implementation of a pretest, one might argue that the biomechanical properties of the intact tendon-bone may be affected by the repeatedly loading of the samples. However, there was a time interval of approximately 4 h between pretest and main test. This rest period should be enough for the tendon-bone formation to recover to the original biomechanical properties. According to other studies, the applied maximum load of 180 N was also small enough to produce no irreversible damage to the intact tendon-bone formation [13, 37].
Additionally, the following experimental configurations were taken into account in our study model to minimize potential confounding effects while evaluating tendon-holding strength of different suture techniques. Some authors formed a crescent-shaped defect [5, 20, 24, 33, 35], others detached the tendon insertion completely [10, 19]. To apply the load only to the anchor-suture system, we also dissected the tendon from the bone completely, whereas a partial defect would result in a subdivision of the applied load. It would be partially carried out by the remaining natural joints between tendon and bone rather than by the anchor-suture system to be tested.
Weaknesses of this study relate mainly to the fact that biomechanical models are difficult to translate into the clinical setting. It is generally believed that weak initial fixation strength is associated with larger gap formations during cyclic loading. Biomechanical models provide useful information on suture techniques at time zero, whereas no information is given about the healing progress. Considering this matter, the question arises where to find the balance between optimal fixation strength to hold long enough for tendon healing and at the same time not compromising healing biology. Our results showed that more compliant suture techniques (e.g., SpB) compared to fixations with less gap formations (e.g., dmSuB) at the 1st cycle failed very early during cyclic loading. Thus, such suture contracts would possibly be too weak and fail before healing can start. Unfortunately, optimal initial strength and maximum gap formation to allow for rotator cuff healing is still unknown. We are aware of the limitation that the sample size of the suture technique groups was not equal (5–17 specimens); however, we used at least a statistically sufficient sample size (5 or more specimens) for each group. Further studies are needed to investigate and compare suture techniques, especially between bridging techniques, in more homogeneous groups. Another limitation of the study might be the assumption that pretesting of intact tendon is obligatory in biomechanical testing. However, results may or may not be biased by the subtraction of pretest elongations of the intact tendons of the measured gap formation of the main test. While pretesting of materials is mandatory in technical material testing, the usefulness of pretesting intact tendons needs to be validated. Furthermore, to set failure at 10-mm gap formation as it is also commonly performed in other studies [5, 32] might not be the ‘real’ gap formation, which would reflect poor clinical results.
Despite weaknesses of this biomechanical study investigating mechanical stability of suture repairs, information regarding initial fixation strength, which allows tendon-to-bone healing during rehabilitation, is of major importance in the clinical setting.
Conclusion
The results of the present study showed that bridging techniques with medial-row fixations seemed to have superior cyclic biomechanical properties regarding initial construct stability compared to other suture techniques. Information regarding initial fixation strength of rotator cuff repair techniques obtained by these findings may also be relevant in the clinical environment.
References
Anderl W, Reihsner R, Heuberer P, Kriegleder B, Eberhardsteiner J (2011) Comparison of the stability of different arthroscopic tendon fixation techniques in dynamic tests. Strain 47:421–429
Bishop J, Klepps S, Lo I, Bird J, Gladstone J, Flatow E (2006) Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Should Elbow Surg 15(3):290–299
Burkhart SS, Adams CR, Schoolfield JD (2009) A biomechanical comparison of 2 techniques of footprint reconstruction for rotator cuff repair: the SwiveLock-FiberChain construct versus standard double-row repair. Arthroscopy 25(3):274–281
Burkhart SS, Diaz Pagan JL, Wirth MA, Athanasiou KA (1997) Cyclic loading of anchor-based rotator cuff repairs: confirmation of the tension overload phenomenon and comparison of suture anchor fixation with transosseous fixation. Arthroscopy 13(6):720–724
Burkhart SS, Johnson TC, Wirth MA, Athanasiou KA (1997) Cyclic loading of transosseous rotator cuff repairs: tension overload as a possible cause of failure. Arthroscopy 13(2):172–176
Busfield BT, Glousman RE, McGarry MH, Tibone JE, Lee TQ (2008) A biomechanical comparison of 2 technical variations of double-row rotator cuff fixation: the importance of medial row knots. Am J Sports Med 36(5):901–906
Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D (2007) Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair?: a prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med 35(8):1247–1253
Christoforetti JJ, Krupp RJ, Singleton SB, Kissenberth MJ, Cook C, Hawkins RJ (2011) Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Should Elbow Surg doi:10.1016/j.jse.2011.02.012
Cole BJ, ElAttrache NS, Anbari A (2007) Arthroscopic rotator cuff repairs: an anatomic and biomechanical rationale for different suture-anchor repair configurations. Arthroscopy 23(6):662–669
Craft DV, Moseley JB, Cawley PW, Noble PC (1996) Fixation strength of rotator cuff repairs with suture anchors and the transosseous suture technique. J Should Elbow Surg 5(1):32–40
De Carli A, Vadala A, Monaco E, Labianca L, Zanzotto E, Ferretti A (2005) Effect of cyclic loading on new polyblend suture coupled with different anchors. Am J Sports Med 33(2):214–219
Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB, Maffulli N, Denaro V (2007) Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med 35(8):1254–1260
Fung YC (1984) Biomechanics: mechanical properties of living tissues. Springer, New York
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Jt Surg Am 86-A(2):219–224
Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C (2009) Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy 25(1):4–12
Hage JJ (2007) The Duncan loop: all knots and tangles. Arthroscopy 23(3):332–333
Harryman DT II, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA III (1991) Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Jt Surg Am 73(7):982–989
Kim DH, Elattrache NS, Tibone JE, Jun BJ, DeLaMora SN, Kvitne RS, Lee TQ (2006) Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med 34(3):407–414
Klinger HM, Buchhorn GH, Heidrich G, Kahl E, Baums MH (2008) Biomechanical evaluation of rotator cuff repairs in a sheep model: suture anchors using arthroscopic Mason-Allen stitches compared with transosseous sutures using traditional modified Mason-Allen stitches. Clin Biomech (Bristol, Avon) 23(3):291–298
Koganti AK, Adamson GJ, Gregersen CS, Pink MM, Shankwiler JA (2006) Biomechanical comparison of traditional and locked suture configurations for arthroscopic repairs of the rotator cuff. Am J Sports Med 34(11):1832–1838
Lo IK, Burkhart SS (2003) Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy 19(9):1035–1042
Ma CB, Comerford L, Wilson J, Puttlitz CM (2006) Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Jt Surg Am 88(2):403–410
Maguire M, Goldberg J, Bokor D, Bertollo N, Pelletier MH, Harper W, Walsh WR (2011) Biomechanical evaluation of four different transosseous-equivalent/suture bridge rotator cuff repairs. Knee Surg Sports Traumatol Arthrosc 19(9):1582–1587
Mahar A, Tamborlane J, Oka R, Esch J, Pedowitz RA (2007) Single-row suture anchor repair of the rotator cuff is biomechanically equivalent to double-row repair in a bovine model. Arthroscopy 23(12):1265–1270
Mazzocca AD, Millett PJ, Guanche CA, Santangelo SA, Arciero RA (2005) Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med 33(12):1861–1868
Milano G, Grasso A, Zarelli D, Deriu L, Cillo M, Fabbriciani C (2008) Comparison between single-row and double-row rotator cuff repair: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 16(1):75–80
Mochizuki T, Sugaya H, Uomizu M, Maeda K, Matsuki K, Sekiya I, Muneta T, Akita K (2009) Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. Surgical technique. J Bone Jt Surg Am 91(Suppl 2 Pt 1):1–7
Park MC, ElAttrache NS, Ahmad CS, Tibone JE (2006) “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy 22(12):1360.e1361–1360.e1365
Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ (2007) Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Should Elbow Surg 16(4):461–468
Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ (2007) Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Should Elbow Surg 16(4):469–4761
Pauly S, Fiebig D, Kieser B, Albrecht B, Schill A, Scheibel M (2011) Biomechanical comparison of four double-row speed-bridging rotator cuff repair techniques with or without medial or lateral row enhancement. Knee Surg Sports Traumatol Arthrosc 19(12):2090–2097
Pauly S, Kieser B, Schill A, Gerhardt C, Scheibel M (2010) Biomechanical comparison of 4 double-row suture-bridging rotator cuff repair techniques using different medial-row configurations. Arthroscopy 26(10):1281–1288
Petit CJ, Boswell R, Mahar A, Tasto J, Pedowitz RA (2003) Biomechanical evaluation of a new technique for rotator cuff repair. Am J Sports Med 31(6):849–853
Scheibel MT, Habermeyer P (2003) A modified Mason-Allen technique for rotator cuff repair using suture anchors. Arthroscopy 19(3):330–333
Smith CD, Alexander S, Hill AM, Huijsmans PE, Bull AM, Amis AA, De Beer JF, Wallace AL (2006) A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Jt Surg Am 88(11):2425–2431
Spang JT, Buchmann S, Brucker PU, Kouloumentas P, Obst T, Schroder M, Burgkart R, Imhoff AB (2009) A biomechanical comparison of 2 transosseous-equivalent double-row rotator cuff repair techniques using bioabsorbable anchors: cyclic loading and failure behavior. Arthroscopy 25(8):872–879
Viidik A (1979) Biomechanical behaviour of soft connective tissues. In: Akkas N, Aan de Rijn A (eds) Progress in biomechanics. Sijthoff and Nordhoff, The Netherlands, pp 75–113
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anderl, W., Heuberer, P.R., Laky, B. et al. Superiority of bridging techniques with medial fixation on initial strength. Knee Surg Sports Traumatol Arthrosc 20, 2559–2566 (2012). https://doi.org/10.1007/s00167-012-1922-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1922-9