Abstract
Purpose
This study investigated the relationship between femoral shaft bowing and the orientation of the surgical transepicondylar axis (TEA) in the coronal plane in varus knee osteoarthritis (OA).
Methods
A total of 82 knees scheduled to undergo total knee arthroplasty (TKA) for the treatment of varus knee OA were enrolled. The hip–knee-ankle angle (HKA) was measured preoperatively on anteroposterior whole-leg standing radiographs. The lateral angle between the TEA and the mechanical axis of the femur (MA-TEA) was measured in the coronal plane from preoperative computed tomography (CT) images. Femoral shaft bowing was measured on CT images. Pearson’s correlation coefficient was used to examine the correlation of the MA-TEA with the HKA and femoral shaft bowing.
Results
The MA-TEA correlated negatively with the HKA (r = − 0.321, P < 0.01) and positively with femoral shaft bowing (r = 0.415, P < 0.01).
Conclusions
The TEA changed to varus as femoral shaft bowing increased in patients with varus knee OA. This suggests that the TEA is not always the centre of the rotational axis of the femur after TKA. In addition, the TEA may not be useful as a consistent parameter in the coronal plane in patients with increasing femoral shaft bowing.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical transepicondylar axis (TEA) is a reliable reference in the axial plane for cutting the posterior condyle and rotating the femoral component in total knee arthroplasty (TKA). The axis is defined as the line through the sulcus of the medial epicondyle and the eminence of the lateral epicondyle [2]. The TEA represents an estimation of the functional flexion–extension axis of the knee [5].
The TEA is perpendicular to the mechanical axis of the femur in the coronal plane [3, 8]. One study indicated that this relationship could be generalized to patients with knee osteoarthritis (OA) [6]. On the other hand, another study demonstrated that the lateral angle between the TEA and the mechanical axis of the femur in the coronal plane was larger in varus knee OA than in non-varus knee OA [14]. These results seem to be controversial, and the factors affecting the orientation of the TEA in the coronal plane were unclear in previous studies.
Coronal and sagittal bowing of the femoral shaft is often seen in Asian patients with knee OA [1, 9,10,11, 13]. The femoral intramedullary guide angle is influenced by femoral shaft bowing in TKA [4, 12]. Femoral shaft bowing has been reported as the likely cause of inaccuracies in postoperative lower limb alignment and the femoral component angle [7]. The TEA is an useful landmark for predicting an appropriate orientation of the femoral component in the coronal plane when it is perpendicular to the mechanical axis of the femur. For example, the TEA plays an important role in patients with large bone defects or revision TKAs since the availability of the original anatomical landmarks is limited. However, the TEA may not always be perpendicular to the mechanical axis of the femur in patients with increasing femoral shaft bowing. The effect of femoral shaft bowing on the orientation of the TEA in the coronal plane has not been evaluated in previous studies. The purpose of this study was to investigate the relationship between femoral shaft bowing and the orientation of the TEA with respect to the mechanical axis of the femur in the coronal plane in patients with varus knee OA. It was hypothesized that the orientation of the TEA would change to varus and might not be useful as a consistent parameter in the coronal plane in knees with increasing femoral shaft bowing.
Materials and methods
This study was approved by the ethics committee of our hospital (B190700006), and informed consent was obtained from each patient.
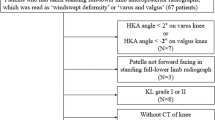
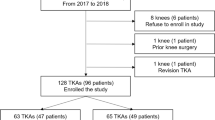
Sixty-nine patients (96 knees) were scheduled to undergo TKA from June 2011 to August 2013. Anteroposterior radiographs and computed tomography (CT) images of the whole leg were preoperatively obtained for surgical planning. Radiographs were performed in a one-leg standing position, with the knee in full extension. The X-ray beam was centered on the knee with the patella facing forward. Patients with osteonecrosis of the knee (1 knee), rheumatoid arthritis (7 knees), valgus knee (5 knees) or previous surgical treatment of the lower limbs (1 knee; previous surgery for hip fracture) were excluded. Thus, 57 patients with varus knee OA (82 knees) met the inclusion criteria in the present study. The patients’ demographic data are shown in Table 1.
Measurement of lower limb alignment
The hip–knee-ankle angle (HKA) was measured using Fujifilm OP-A software (Fujifilm, Tokyo, Japan) on anteroposterior whole-leg standing radiographs. The HKA was defined as the angle between the mechanical axes of the femur and tibia, with positive values representing valgus alignment.
Measurements of femoral shaft bowing and angle between mechanical axis of the femur and surgical transepicondylar axis
Whole-leg CT images (1.5-mm thick slices) were obtained with patients lying supine in a SOMATOM Sensation 16 CT system (Siemens, Munich, Germany). Data were incorporated into Orthomap 3D (Stryker, Kalamazoo, MI), enabling the selection of anatomical landmarks and the determination of 3-dimensional linear and angular measurements by simultaneously referring to the sagittal, coronal, and axial planes [6]. The Y-axis was defined as the line through the centre of the femoral head and the most proximal point of the femoral notch. The X-axis was defined as a line perpendicular to the Y-axis. The XY plane was created to include the TEA. The Z-axis was defined as the cross-product of the X- and Y-axes. The lateral angle between the TEA and the mechanical axis of the femur (MA-TEA) was measured on the XY plane (Fig. 1). According to previous studies [1, 13], the femoral diaphysis was divided into four equal parts on the reconstructed CT. Femoral shaft bowing was defined according to the angle between the axes of the first and fourth segments of the femoral shaft on the XY plane (Fig. 2); a positive value represented lateral bowing. In addition, the lateral angle between the midline in the fourth segment of the femoral shaft and the TEA (Distal-TEA) was measured on the XY plane (Fig. 3).
Statistical analysis
Data are shown as the means ± standard deviations and were confirmed to show a normal distribution using the Shapiro–Wilk test. Pearson’s correlation coefficient was used to examine the correlation between the HKA, femoral shaft bowing, or Distal-TEA, and the MA-TEA and the correlation between femoral shaft bowing and Distal-TEA. All statistical analyses were performed using SPSS (IBM Corporation, Armonk, NY). Values of P < 0.05 were considered statistically significant. Sample size calculation was performed using G*Power version 3.1.9.2 (Heinrich-Heine-Universität Düsseldorf, Germany). A priori power analysis (effect size = 0.3, significance level = 0.05, and power = 0.8) resulted in a sample size of 82. To examine the reproducibility of the measurements on CT images, 20 knees were randomly selected, and intra- and interobserver reliabilities were determined using intraclass correlation coefficients (ICCs) for each measurement.
Results
Radiographic and CT data are summarized in Table 2. MA-TEA varied widely, with a mean value exceeding 90°. MA-TEA correlated negatively with HKA (r = − 0.321, P < 0.01) (Fig. 4) and positively with both femoral shaft bowing (r = 0.415, P < 0.01) (Fig. 5) and Distal-TEA (r = 0.657, P < 0.01) (Fig. 6). In addition, femoral shaft bowing correlated negatively with Distal-TEA (r = − 0.287, P < 0.01) (Fig. 7).
The intra- and interobserver ICCs were 0.94 and 0.93 for femoral shaft bowing, 0.7 and 0.59 for MA-TEA, and 0.5 and 0.52 for Distal-TEA, respectively.
Discussion
The most important finding of this study was that the lateral angle between the TEA and the mechanical axis of the femur increased as femoral shaft bowing increased in the coronal plane. In this study, MA-TEA correlated negatively with HKA. This result supports the previous findings of Zhang et al. [14], who demonstrated that the lateral angle between the TEA and the mechanical axis of the femur in the coronal plane was larger in varus knee OA than in non-varus knee OA. It was suggested that the TEA was not perpendicular to the mechanical axis of the femur in the coronal plane when limited to cases with severe varus deformity.
In this study, MA-TEA increased with greater femoral shaft bowing. The reason why MA-TEA correlated negatively with HKA was unclear in the previous study [14]. The present study revealed that femoral shaft bowing was a contributing factor by which MA-TEA correlated negatively with HKA. On the other hand, Distal-TEA decreased with greater femoral shaft bowing. It was thought that the change in Distal-TEA represented a compensatory mechanism to maintain the TEA perpendicular to the mechanical axis of the femur in the coronal plane. The joint line should be parallel to the floor in the standing position. This force may change the orientation of the TEA against femoral shaft bowing. However, deformity of the distal femoral shaft could not completely compensate for the effect of femoral shaft bowing on the orientation of the TEA. Measured values in this study could be affected by other factors. For example, the degree of coronal bowing of the femoral shaft may be affected by femoral torsion. If the distal femur is twisted internally, coronal bowing will increase because a portion of the sagittal bowing is added to the coronal bowing. MA-TEA may also be affected by femoral torsion. The relationship between femoral torsion and femoral shaft bowing and MA-TEA should be elucidated in a future study.
In clinical practice, the TEA is a useful landmark for predicting an appropriate orientation of the femoral component in the coronal plane when it is perpendicular to the mechanical axis of the femur. For example, the TEA plays an important role in patients with large bone defects or revision TKAs since the availability of the original anatomical landmarks is limited. However, the TEA changed to varus as femoral shaft bowing increased in this study. The TEA may not be useful as a consistent parameter in the coronal plane in such knees. In addition, the functional flexion–extension axis of the knee after TKA would correspond to the TEA determined using the mechanical alignment method in cases with the TEA perpendicular to the mechanical axis of the femur. In contrast, the postoperative functional flexion–extension axis in knees with severe femoral shaft bowing may differ from the TEA, indicating a possible factor affecting clinical outcomes after TKA. Whether this discrepancy should be taken into account in procedures for TKA remains to be elucidated.
Various limitations to the present study need to be considered when interpreting the results. First, most patients in the present study were Japanese females who underwent TKA for moderate to severe varus knee OA, meaning that the present study provides more information on TKA in Japanese female patients with varus knee OA than in the general population. Second, both knees in 25 patients were analyzed in the present study. In the same patient, the measured values may be the same, although there is no literature on this issue. This could bias the results in the present study. Third, patients with flexion contracture were not excluded from the present study. This might affect HKA. Fourth, the values from a weight-bearing radiograph were compared to those of a non-weight- bearing CT. This might affect the results of this study. Fifth, the correlations were often quite fair. Finally, the statistical power of this study was slightly weak. The sample size should ideally be increased.
Conclusions
The MA-TEA increased with greater femoral shaft bowing in the coronal plane in patients with varus knee OA. This suggests that the TEA is not always the centre of the rotational axis of the femur after TKA. In addition, the TEA may not be useful as a consistent parameter in the coronal plane in patients with increasing femoral shaft bowing.
Abbreviations
- TEA:
-
Transepicondylar axis
- TKA:
-
Total knee arthroplasty
- OA:
-
Osteoarthritis
- CT:
-
Computed tomography
- HKA:
-
Hip–knee-ankle angle
- ICCs:
-
Intraclass correlation coefficients
References
Akamatsu Y, Kobayashi H, Kusayama Y, Kumagai K, Saito T (2016) Femoral shaft bowing in the coronal and sagittal planes on reconstructed computed tomography in women with medial compartment knee osteoarthritis: a comparison with radiograph and its predictive factors. Arch Orthop Trauma Surg 136:1227–1232
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Echhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Rubinstein D, Humphries S (2003) Three-dimensional morphology and kinematics of the distal part of the femur viewed in virtual reality. J Bone Jt Surg Am 85:97–104
Kim JM, Hong SH, Kim JM, Lee BS, Kim DE, Kim KA, Bin SI (2015) Femoral shaft bowing in the coronal plane has more significant effect on the coronal alignment of TKA than proximal or distal variations of femoral shape. Knee Surg Sports Traumatol Arthrosc 23:1936–1942
Kobayashi H, Akamatsu Y, Kumagai K, Kusayama Y, Aratake M, Saito T (2015) Is the surgical epicondylar axis the center of rotation in the osteoarthritic knee? J Arthroplasty 30:479–483
Kobayashi H, Akamatsu Y, Kumagai K, Kusayama Y, Ishigatsubo R, Muramatsu S, Saito T (2014) The surgical epicondylar axis is a consistent reference of the distal femur in the coronal and axial planes. Knee Surg Sports Traumatol Arthrosc 22:2947–2953
Lasam MP, Lee KJ, Chang CB, Kang YG, Kim TK (2013) Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin Orthop Relat Res 471:1472–1483
Lustig S, Lavoie F, Selmi TA, Servien E, Neyret P (2008) Relationship between the surgical epicondylar axis and the articular surface of the distal femur: an anatomic study. Knee Surg Sports Traumatol Arthrosc 16:674–682
Matsumoto T, Hashimura M, Takayama K, Ishida K, Kawakami Y, Matsuzaki T, Nakano N, Matsushita T, Kuroda R, Kurosaka M (2015) A radiographic analysis of alignment of the lower extremities—initiation and progression of varus type knee osteoarthritis. Osteoarthr Cartil 23:217–223
Mochizuki T, Tanifuji O, Koga Y, Sato T, Kobayashi K, Nishino K, Watanabe S, Ariumi A, Fujii T, Yamagiwa H, Omori G, Endo N (2017) Sex differences in femoral deformity determined using three-dimensional assessment for osteoarthritic knees. Knee Surg Sports Traumatol Arthrosc 25:468–476
Mullaji AB, Marawar SV, Mittal V (2009) A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J Arthroplasty 24:861–867
Palanisami D, Iyyampillai G, Shanmugam S, Natesan R (2016) Individualised distal femoral cut improves femoral component placement and limb alignment during total knee replacement in knees with moderate and severe varus deformity. Int Orthop 40:2049–2054
Yau WP, Chiu KY, Tang WM, Ng TP (2007) Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong) 15:32–36
Zhang Y, Wang X, Shao Y, Xia Q (2018) The orientation of the surgical epicondylar axis varies in varus and non-varus knees in the coronal plane. Knee Surg Sports Traumatol Arthrosc 26:2580–2586
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
SN: study design, data collection, interpreting the data and writing the paper. KK, HK: data collection. SY, TA, TO, MS, YI: interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Ethics approval
Ethical approval for the study was obtained from the institutional review board of Yokohama City University Hospital (B190700006).
Consent to participate
Informed and written consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nejima, S., Kumagai, K., Kobayashi, H. et al. Coronal shaft bowing of the femur affects varus inclination of the surgical transepicondylar axis in varus knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 29, 814–819 (2021). https://doi.org/10.1007/s00167-020-06025-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06025-1