Abstract
Purpose
Achilles tendon ruptures are devastating and recover slowly and incompletely. There is a great demand for biomolecular therapies to improve recovery, yet little is understood about growth factors in a healing tendon. Here, the role of growth factors during tendon healing in a rat model and their reaction to single and multiple growth factor treatment are explored.
Methods
Rat tendons were transected surgically and resutured. The expression of bFGF, BMP-12, VEGF and TGF-β1 was assessed by immunohistochemical analysis one to 8 weeks after surgery. Paracrine effects of TGF-β1 or BMP-12 added by adenoviral transfer, as well as the effect of autologous conditioned serum (ACS) on growth factor expression, were evaluated.
Results
bFGF, BMP-12 and VEGF expression was highest 1 week after transection. bFGF and BMP-12 declined during the remaining period whereas VEGF expression persisted. TGF-β1 expression dramatically increased after 8 weeks. ACS treatment increased bFGF (P = 0.007) and BMP-12 (P = 0.004) expression significantly after 8 weeks. Also overall expression of bFGF, BMP-12 and TGF-β1 regardless of time point was significantly greater than controls with ACS treatment (P < 0.05). Both BMP-12 and TGF-β1 treatments had no significant effect. No effect was observed in VEGF with any treatment.
Conclusion
bFGF, BMP-12, VEGF and TGF-β1 are differentially expressed during tendon healing. Additional BMP-12 or TGF-β1 has no significant influence, whereas ACS generally increases expression of all factors except VEGF. Staged application of multiple growth factors may be the most promising biomolecular treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tendon ruptures and tears are common injuries that heal slowly and are often treated surgically. However, clinical outcomes are not always satisfactory [21]. Growth factors play an important role in tendon healing [15], and there is increasing confidence that accelerated and improved healing may be achievable by biological intervention.
The physiological course of tendon healing with an emphasis on growth factor expression has been studied for various models of tendon pathology, including rotator cuff tears [10, 23, 32, 40] and Achilles tendon ruptures in a rat model [3, 8, 9, 19, 29]; in vitro studies have used tenocyte cultures [6].
There have been a number of experiments in which recombinant growth factors have been applied in attempts to accelerate tendon healing in an animal model, but most have used only a single factor and results have been variable. Experiments designed to study the endogenous expression of growth factors have measured expression over only a few days or even just at a single time point. Thus, the natural expression of growth factors over time and the influence of growth factors added to promote tendon healing remains unclear [15, 22].
To address this issue, a rat model of acute traumatic Achilles tendon rupture without tendinopathy was chosen and four growth factors—basic Fibroblast growth Factor (bFGF), bone morphogenic factor 12 (BMP-12), vascular endothelial growth factor (VEGF) and transforming growth factor beta (TGF-β1)—that have an established and prominent role during tendon healing [22, 24] were measured.
Previous experiments have shown that basic fibroblast growth factor (bFGF, FGF-2) stimulates proliferation and thereby increases the cellularity of a healing tendon [1, 10, 36]. Bone morphogenic factor 12 (BMP-12, a.k.a. CDMP-3 or GDF-7) is important for tenoblast and fibroblast differentiation [5, 19, 23, 32], and vascular endothelial growth factor (VEGF) plays an essential role in angiogenesis [26, 40]. Transforming growth factor beta one (TGF-β1) is known to influence the healing of fibrous tissues including tendons. It is secreted by infiltrating macrophages and platelets and is known to stimulate proliferation and matrix organisation [2, 9, 13, 16, 27].
The hypothesis was that growth factors would be elevated at the beginning of tendon healing and would then gradually decrease as healing progressed. Stimulating this process with exogenous growth factors would lead to a prolonged endogenous expression of the growth factors over time.
To verify this either bone morphogenic factor 12 (BMP-12) as a specific inductor of tendon and ligament tissue, transforming growth factor beta (TGF-β1) as a treatment with diverse effects or autologous conditioned serum (ACS) as a representative of biological treatment with multiple growth factors was added.
Materials and methods
Rat Achilles tendon healing model
Approval for all animal procedures was obtained beforehand from the local Institutional Animal Care and Use Committee of Harvard Medical School (Boston, MA, USA). Sixty male adult Sprague-Dawley rats (weight 400–425 g, >10 weeks old) were used.
Fifteen animals per group were used for natural expression of growth factors, controls, BMP-12, TGF-β1 and ACS groups. For each group, 3 animals each were euthanised after 1, 2, 4 and 8 weeks. The unoperated contralateral tendons of the animals not treated were used to establish a baseline for the stainings.
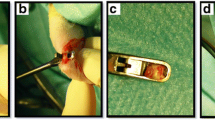
Animals were placed under general anaesthesia with isoflurane. The right hind leg was shaved and disinfected with Betadine. After placement on a warm sterile field, a 3-cm incision was made above the right Achilles tendon. The peritendon was opened and the Achilles tendon cut at a right angle to the collagen fibres, creating a 5-mm gap proximal to the calcaneal insertion. The plantaris tendon was transected, preventing a splinting phenomenon.
In animals used for examination of endogenous expression of growth factors and animals in the control and ACS group, Achilles tendon, peritendon and skin were sutured back together.
For animals in groups with BMP-12 or TGF-β1 treatment, the transfected muscle grafts were placed with two single stitches around the side of tendon injury after end-to-end suture repair.
After regaining consciousness, the rats received buprenorphine injections twice daily for 2 days.
Growth factors
BMP-12 or TGF-β1 cDNA was transferred to 4-mm round muscle flaps harvested from a donor rat by gene transfer using recombinant adenovirus vectors as described previously [19]. In short, serotype 5 recombinant adenoviral vector was used, recombinant adenoviruses (Ad.BMP-12 or Ad.TGF-β1) were propagated in 293/Cre8 cells and muscle grafts incubated with particles in DMEM medium with 5% foetal bovine serum for 24 h before implantation. Expression of BMP-12 and TGF-β1 has been found to be increased 4–7 days after transfection [19].
ACS was used from a previous study as described [20]. In short, pooled rat blood was incubated for 9 h at 37°C in Orthokine syringes (Orthogen AG, Duesseldorf, Germany) containing glass beads. Samples were then centrifuged and frozen at −20°C. For injection, aliquots were thawed on ice and allowed to reach room temperature. A volume of 170 μl of ACS were injected once every 24 h for 3 days directly into the area of the sutured repair using a 1-ml insulin syringe. According to previous studies, ACS contains increased levels of TGF-β1, bFGF and VEGF compared to basal serum concentrations, as well as inflammatory and anti-inflammatory cytokines. However, Platelet-derived growth factor-BB (PDGF-BB) in rat derived ACS and insulin-like growth factor 1 (IGF-1) in human derived ACS were not substantially increased [20, 37].
Immunohistochemical analysis
Animals were placed under general anaesthesia with isoflurane and asphyxiated with CO2. To harvest the whole muscle–tendon–bone units a 5-cm incision was made from below the knee down to the plantar fascia of the foot. Muscle–tendon–bone units were explanted by transection of the middle part of the gastrocnemius muscle and of the calcaneus.
The tendons were immediately placed in 4% buffered formalin (pH 7.4) for 24 h, dehydrated and embedded in paraffin wax. Endogenous peroxidase was blocked by 30-min incubation in 1% hydrogen peroxide in phosphate-buffered saline (PBS). After washing in PBS, sections were incubated for 1 h with 2% powdered milk in PBS to block nonspecific protein binding. Sections were incubated with the primary antibody over night at 4°C, followed by three 5-min washes. For amplified detection with biotin–avidin–peroxidase, sections were incubated with biotinylated secondary antibody (rabbit anti-mouse biotin label or goat anti rabbit biotin label, Dako, Denmark) for 30 min at room temperature, washed three times with PBS and incubated with avidin-biotinylated-peroxidase complex (Vectastain ABC Kit Elite Standard, Vector, CA, USA) for 30 min at room temperature. This was followed by three 5-min washes with PBS. Substrate (solution with Tris, peroxide and 3,3 Diaminobenzidine tablets, Sigma, Munich) was added for 5 min. Sections were washed in tap water three times and stained with haematoxylin and eosin. Primary antibodies used were against bFGF (rabbit polyclonal; Abcam, Cambridge UK), BMP-12 (rabbit polyclonal; AbD Serotec, Oxford, UK), VEGF (mouse monoclonal; Abcam, Cambridge, UK) and TGF-β1 (rabbit polyclonal; Santa Cruz, CA, USA).
Histological scoring was supported by digital image analysis (Image-Pro Plus, Media Cybernetics, Silver Spring, MD, USA). Samples were taken from 5 distinct locations, including the central part of the rupture, the left and right borders, borders towards the muscle insertion and the calcaneal insertion. Scores of the 5 sections were then averaged to a whole score for the tendon.
The immunoreactive score used is widely accepted for quantification of immunohistological stainings [4, 14, 28, 30, 35, 39]. The characterisation of relative amount and location of the protein of interest and the high sensitivity are of great advantage. The score was calculated by assigning points for overall staining (1 for no staining to 4 for strong staining) and for overall stained cells (1 for no cells to 5 for over 80% of cells) and multiplying both to a general score. Sections were scored by two independent blinded observers with high inter-observer reliability (Spearman’s correlation coefficient 0.86). Scores also correlated strongly with digital image analysis of overall stained area (coefficient 0.85).
Statistical analysis
Analysis of variance (ANOVA) was performed on time courses and differences between groups. Where ANOVA was significant, multiple comparisons were performed with the Tukey-HSD post hoc test. Results were considered significant with a P-value of <0.05. Statistics, plots of means and standard deviations were produced with R v. 2.10.1.
Results
Natural course of growth factor expression during tendon healing
bFGF, BMP-12, TGF-β1 and VEGF were detected in all samples and displayed clearly distinct time courses of expression (Fig. 1), thereby validating the immunohistological scoring performed.
Immunoreactive scores for primary antibodies against bFGF, BMP-12, VEGF and TGF-β1 at different time points after tendon transection. The scores are plotted as means. Every point in the plot represents the mean value of 3 samples for the respective time point. Points at ‘0 weeks’ represent the mean score of normal tendon. P-values refer to the difference to normal tendon. See text for further description
Expression levels of bFGF (P = 0.012) and BMP-12 (P = 0.008) were significantly higher 1 week after transection compared to unoperated rat Achilles tendons whereas no significant difference was observed for TGF-β1 and VEGF.
After 2, 4 and 8 weeks bFGF expression was close to the expression found in unoperated tendon. Similarly, BMP-12 expression decreased rapidly over time. From 2 weeks onwards, expression of BMP-12 was similar to the expression observed in untreated tendons.
VEGF expression was elevated after 1 week, decreasing to normal at week 2 and slightly increasing to 3 points at weeks 4 and 8.
Interestingly, TGF-β1 showed a different pattern of expression compared to the other three growth factors. It was elevated at week 1 and subsequently declined to the level of normal tendon at weeks 2 and 4. However, expression increased again after 8 weeks. Changes in TGF-β1 staining scores more strongly reflected the number of stained cells at each time point. Representative histological images are shown in Fig. 2.
Auto- and paracrine effects of BMP-12, TGF-β1 or ACS on growth factor expression
ACS had the greatest effect on growth factor expression. It increased bFGF significantly after 8 weeks compared to controls (P = 0.007) and BMP-12 (P = 0.004). A nearly significant elevation of bFGF was also observed with ACS in week 4 compared to BMP-12 (P = 0.074) and TGF-β1 (P = 0.084). Comparing the expression of BMP-12, TGF-β1 and VEGF between groups at single time points did not yield any significant differences (Figures 3, 4, 5, 6).
Expression of bFGF over time as measured by immunoreactive score. For weeks 1, 2, 4 and 8, grey boxes indicate the mean values of immunoreactive scores for controls and groups stimulated with either ACS (+ACS), TGF-β1 (+TGF) or BMP-12 (+BMP) as indicated. Whiskers indicate the upper standard deviation; the lower symmetrical interval is omitted for reasons of clarity and comprehensibility. Brackets with stars on top indicate significant pairings, **P < 0.01
Expression of BMP-12 over time as measured by immunoreactive score. For weeks 1, 2, 4 and 8, grey boxes indicate the mean values of immunoreactive scores for controls and groups stimulated with either ACS (+ACS), TGF-β1 (+TGF) or BMP-12 (+BMP) as indicated. Whiskers indicate the upper standard deviation; the lower symmetrical interval is omitted for reasons of clarity and comprehensibility
Expression of TGF-β1 over time as measured by immunoreactive score. For weeks 1, 2, 4 and 8 grey boxes indicate the mean values of immunoreactive scores for controls and groups stimulated with either ACS (+ACS), TGF-β1 (+TGF) or BMP-12 (+BMP) as indicated. Whiskers indicate the upper standard deviation; the lower symmetrical interval is omitted for reasons of clarity and comprehensibility
Expression of VEGF over time as measured by immunoreactive score. For weeks 1, 2, 4 and 8, grey boxes indicate the mean values of immunoreactive scores for controls and groups stimulated with either ACS (+ACS), TGF-β1 (+TGF) or BMP-12 (+BMP) as indicated. Whiskers indicate the upper standard deviation; the lower symmetrical interval is omitted for reasons of clarity and comprehensibility
Overall bFGF expression regardless of time point was significantly greater in the ACS group compared to controls and the BMP-12 and TGF-β1 groups (all P < 0.002). Overall BMP-12 expression was also greater in the ACS group compared to controls and the BMP-12 and TGF-β1 groups (all P < 0.05). Overall TGF-β1 expression was greater in the ACS group compared to controls and the TGF-β1 group (all P < 0.05). There was no significant difference between groups for the overall expression of VEGF.
Discussion
The most important findings of the present study were the distinct time courses of the measured growth factors and their increase with ACS stimulation. Affirming the initial hypothesis, the expression of bFGF, BMP-12, VEGF and TGF-β1 was elevated in the 1 week of healing, possibly in response to the inflammation after rupture. As the healing progressed, each growth factor followed a slightly different path, most likely interacting with the effects of other growth factors. BMP-12 and bFGF expression both declined rapidly after the 1 week of healing, possibly because inflammation was resolving at this stage. After 2–4 weeks, both growth factors approached their basal expression levels.
TGF-β1 showed an initially high expression, declined rapidly to normal concentrations and increased again strongly in week 8, probably reflecting remodelling and scar formation in the late stages of tendon healing. VEGF expression was initially higher than normal and remained above normal for the entire 8-week period. This may reflect the importance of neoangiogenesis in tendon healing. However, it is surprising that VEGF expression did not decline at the end of this period because it coincides with an elevated expression of TGF-β1, which has been reported to suppress VEGF expression in tendon [8]. Also, from a tissue architecture point of view, a decrease in neoangiogenesis due to scar formation after 8 weeks might be expected [34].
In contrast to the second hypothesis, ACS displayed the greatest effect on the endogenous expression of growth factors, while the addition of TGF-β1 or BMP-12 did not affect or seemed to even decrease their expression. This may indicate a reactive suppression due to the addition of BMP-12 or TGF-β1 and may signify that addition of a single growth factor cannot emulate the complex interactions of healing.
According to previous studies, ACS contains increased levels of TGF- β1, bFGF and VEGF, as well as inflammatory and anti-inflammatory cytokines [20, 37].
Schippinger found no significant systematic influence and no significant increase of IGF-1 using ACP (autologous conditioned plasma) after intramuscular application [31]. Due to the fast absorption and degradation of the cytokines, it was not expected that the dosage of ACS used would have any generalised effect or an effect on the contralateral tendon.
Limitations of this study were the use of transected Achilles tendons without tendinopathy, the time of follow-up and the restricted number of growth factors to eminent key factors during tendon healing.
However, it was not intended to mimic the pathophysiology of human tendinopathy, the most frequent and devastating disease leading to Achilles tendon ruptures [17, 34]. Instead, the study concentrated on transected Achilles tendons that simulate a rupture in an otherwise healthy tendon in order to illuminate the normal process of tendon healing and to investigate the effect of additional growth factors. This knowledge is crucial because it allows one to approach the pathologically changed Achilles tendon with more understanding of the pathological differences.
The time points for examination of the growth factor expression were chosen based upon a similar study of rotator cuff healing in rats [38] and reflect the time course of the different phases of tendon healing, namely early inflammation, reorganisation and late tissue remodelling.
Tendon ruptures lead to a considerable loss of function of the injured extremity. During healing, the ruptured tendon forms a regenerate within the first few weeks, yet despite intensive remodelling over the following months a complete regeneration of the tendon is never achieved [15]. Tendon healing is a complex and highly regulated process that is initiated, sustained and terminated by a large variety of biomolecular and biomechanical stimuli [11, 22]. The scar tissue that is formed is mostly mechanically inferior and cannot perform as well as a normal tendon [3, 19, 25].
It is established that patients profit from an early functional therapy after Achilles tendon repair (e.g., [7, 33]). Current development of biomolecular therapies aims to further improve healing results [33]. Current trends may lead to a gross oversimplification of the biological processes and complex interactions between growth factors in a healing tendon.
Based on the results of the present study, staged application of different growth factors is likely to have a greater effect than the application of a single growth factor at one time point, a conclusion independently favoured by Molloy et al. [22] and Oliva et al. [24]. ACS provides a convenient means of applying multiple, autologous growth factors. Several studies have shown its beneficial effect on the healing tendon in rats, both in healing time and resulting mechanical properties of the healed tendon [12, 18, 20]. Further studies may determine the right dosage and intervals for an optimal therapy.
In view of a possible clinical application of biological augmentation of tendon healing in man, there is no doubt about the improvement by biological intervention. However, any treatment aiming to mimic the natural biological process should not focus on a single growth factor. Considering the highly complex process of healing and the influence of exogenous cytokines on endogenous growth factors, a truly practical treatment will require much development. Nevertheless, the future of growth factor based therapies is promising.
Conclusion
Tendon healing involves the coordinated, interactive mediation of many growth factors. The four endogenous growth factors studied here showed different expression patterns during tendon healing and were differentially affected by the exogenous application of BMP-12, TGF-β1 and ACS.
The present study suggest that the 1 week of tendon healing is a crucial period of growth factor stimulation and that ACS has the greatest influence on later expression especially of bFGF and BMP-12. Future research should focus on the complex interactions—synergism or antagonism—of growth factors in order to create a solid basis for biomolecular treatment.
Abbreviations
- ACS:
-
Autologous conditioned serum
- bFGF:
-
Basic fibroblast growth factor, a.k.a. FGF-2
- BMP:
-
Bone morphogenic protein
- CDMP:
-
Cartilage-derived morphogenic protein
- GDF:
-
Growth and differentiation factor
- IGF-1:
-
Insulin-like growth factor 1
- PDGF:
-
Platelet-derived growth factor
- TGF-β1:
-
Transforming growth factor beta 1
- VEGF:
-
Vascular endothelial growth factor
References
Chan BP, Fu S, Qin L, Lee K, Rolf CG, Chan K (2000) Effects of basic fibroblast growth factor (bFGF) on early stages of tendon healing: a rat patellar tendon model. Acta Orthop Scand 71(5):513–518
Chan KM, Fu SC, Wong YP, Hui WC, Cheuk YC, Wong MW (2008) Expression of transforming growth factor beta isoforms and their roles in tendon healing. Wound Repair Regen 16(3):399–407
Eliasson P, Andersson T, Aspenberg P (2009) Rat Achilles tendon healing: mechanical loading and gene expression. J Appl Physiol 107(2):399–407
Fabricius E, Kruse-Boitschenko U, Khoury R, Wildner G, Raguse J, Klein M (2009) Immunohistochemical determination of the appropriate anti-hTERT antibodies for in situ detection of telomerase activity in frozen sections of head and neck squamous cell carcinomas and tumor margin tissues. Int J Oncol 34(5):1257–1279
Forslund C, Rueger D, Aspenberg P (2003) A comparative dose-response study of cartilage-derived morphogenetic protein (CDMP)-1, -2 and -3 for tendon healing in rats. J Orthop Res 21(4):617–621
Fu SC, Cheuk YC, Chan KM, Hung LK, Wong MW (2008) Is cultured tendon fibroblast a good model to study tendon healing? J Orthop Res 26(3):374–383
Gwynne-Jones DP, Sims M, Handcock D (2011) Epidemiology and outcomes of acute Achilles tendon rupture with operative or nonoperative treatment using an identical functional bracing protocol. Foot Ankle Int 32(4):337–343
Hou Y, Mao Z, Wei X, Lin L, Chen L, Wang H, Fu X, Zhang J, Yu C (2009) Effects of transforming growth factor-beta1 and vascular endothelial growth factor 165 gene transfer on Achilles tendon healing. Matrix Biol 28(6):324–335
Hou Y, Mao Z, Wei X, Lin L, Chen L, Wang H, Fu X, Zhang J, Yu C (2009) The roles of TGF-beta1 gene transfer on collagen formation during Achilles tendon healing. Biochem Biophys Res Commun 383(2):235–239
Ide J, Kikukawa K, Hirose J, Iyama K, Sakamoto H, Fujimoto T, Mizuta H (2009) The effect of a local application of fibroblast growth factor-2 on tendon-to-bone remodeling in rats with acute injury and repair of the supraspinatus tendon. J Shoulder Elbow Surg 18(3):391–398
Jung HJ, Fisher MB, Woo SL (2009) Role of biomechanics in the understanding of normal, injured, and healing ligaments and tendons. Sports Med Arthrosc Rehabil Ther Technol 1(1):9
Kajikawa Y, Morihara T, Sakamoto H, Matsuda K, Oshima Y, Yoshida A, Nagae M, Arai Y, Kawata M, Kubo T (2008) Platelet-rich plasma enhances the initial mobilization of circulation-derived cells for tendon healing. J Cell Physiol 215(3):837–845
Kashiwagi K, Mochizuki Y, Yasunaga Y, Ishida O, Deie M, Ochi M (2004) Effects of transforming growth factor-beta 1 on the early stages of healing of the Achilles tendon in a rat model. Scand J Plast Reconstr Surg Hand Surg 38(4):193–197
Liu F, Wang JG, Wang SY, Li Y, Wu YP, Xi SM (2008) Antitumor effect and mechanism of Gecko on human esophageal carcinoma cell lines in vitro and xenografted sarcoma 180 in Kunming mice. World J Gastroenterol 14(25):3990–3996
Longo UGLA, Maffulli N, Denaro V (2010) Tissue engineered biological augmentation for tendon healing: a systematic review. Br Med Bull 98(1):31–59
Lorda-Diez CI, Montero JA, Martinez-Cue C, Garcia-Porrero JA, Hurle JM (2009) Transforming growth factors beta coordinate cartilage and tendon differentiation in the developing limb mesenchyme. J Biol Chem 284(43):29988–29996
Lui PPY, Maffulli N, Rolf C, Smith RKW (2011) What are the validated animal models for tendinopathy? Scand J Med Sci Sports 21(1):3–17
Lyras DN, Kazakos K, Verettas D, Polychronidis A, Tryfonidis M, Botaitis S, Agrogiannis G, Simopoulos C, Kokka A, Patsouris E (2009) The influence of platelet-rich plasma on angiogenesis during the early phase of tendon healing. Foot Ankle Int 30(11):1101–1106
Majewski M, Betz O, Ochsner PE, Liu F, Porter RM, Evans CH (2008) Ex vivo adenoviral transfer of bone morphogenetic protein 12 (BMP-12) cDNA improves Achilles tendon healing in a rat model. Gene Ther 15(16):1139–1146
Majewski M, Ochsner PE, Liu F, Flückiger R, Evans CH (2009) Accelerated healing of the rat Achilles tendon in response to autologous conditioned serum. Am J Sports Med 37(11):2117–2125
Majewski M, Widmer KH, Steinbrück K (2002) Achilles tendon ruptures: 25 year’s experience in sport-orthopedic treatment. Sportverletz Sportschaden 16(4):167–173
Molloy T, Wang Y, Murrell G (2003) The roles of growth factors in tendon and ligament healing. Sports Med 33(5):381–394
Murray DH, Kubiak EN, Jazrawi LM, Araghi A, Kummer F, Loebenberg MI, Zuckerman JD (2007) The effect of cartilage-derived morphogenetic protein 2 on initial healing of a rotator cuff defect in a rat model. J Should Elb Surg 16(2):251–254
Oliva F, Via AG, Maffulli N (2011) Role of growth factors in rotator cuff healing. Sports Med Arthrosc 19(3):218–226
Otoshi K, Kikuchi S, Ohi G, Numazaki H, Sekiguchi M, Konno S (2011) The process of tendon regeneration in an Achilles tendon resection rat model as a model for hamstring regeneration after harvesting for anterior cruciate ligament reconstruction. Arthroscopy 27(2):218–227
Petersen W, Pufe T, Unterhauser F, Zantop T, Mentlein R, Weiler A (2003) The splice variants 120 and 164 of the angiogenic peptide vascular endothelial cell growth factor (VEGF) are expressed during Achilles tendon healing. Arch Orthop Trauma Surg 123(9):475–480
Pryce BA, Watson SS, Murchison ND, Staverosky JA, Dünker N, Schweitzer R (2009) Recruitment and maintenance of tendon progenitors by TGFbeta signaling are essential for tendon formation. Development 136(8):1351–1361
Remmele W, Stegner HE (1987) Vorschlag zur einheitlichen Definition eines immunreaktiven Scores (IRS) für den imunhistochemischen Östrogenrezeptornachweis (ER-ICA) in Mammagewebe. [Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue]. Pathologe 8(3):138–140
Rickert M (2008) BMP-14 gene therapy increases tendon tensile strength in a rat model of Achilles tendon injury. J Bone Jt Surg Am 90(2):445–446
Rodeo SA, Seneviratne A, Suzuki K, Felker K, Wickiewicz TL, Warren RF (2000) Histological analysis of human meniscal allografts. A preliminary report. J Bone Jt Surg Am 82-A (8):1071–1082
Schippinger G, Oettl K, Fankhauser F (2011) Influence of intramuscular application of autologous conditioned plasma on systemic circulating IGF-1. J Sports Sci Med 2011(10):439–444
Seeherman HJ, Archambault JM, Rodeo SA, Turner AS, Zekas L, D’Augusta D, Li XJ, Smith E, Wozney JM (2008) rhBMP-12 accelerates healing of rotator cuff repairs in a sheep model. J Bone Jt Surg Am 90(10):2206–2219
Sharma P, Maffulli N (2005) The future: rehabilitation, gene therapy, optimization of healing. Foot Ankle Clin 10(2):383–397
Sharma P, Maffulli N (2006) Biology of tendon injury: healing, modeling and remodeling. J Musculoskelet Neuronal Interact 6(2):181–190
Soslow RA, Ying L, Altorki NK (1997) Expression of acidic fibroblast growth factor in Barrett’s esophagus and associated esophageal adenocarcinoma. J Thorac Cardiovasc Surg 114(5):838–843
Thomopoulos S, Das R, Sakiyama-Elbert S, Silva MJ, Charlton N, Gelberman RH (2010) bFGF and PDGF-BB for tendon repair: controlled release and biologic activity by tendon fibroblasts in vitro. Ann Biomed Eng 38(2):225–234
Wright-Carpenter T, Klein P, Schäferhoff P, Appell HJ, Mir LM, Wehling P (2004) Treatment of muscle injuries by local administration of autologous conditioned serum: a pilot study on sportsmen with muscle strains. Int J Sports Med 25(8):588–593
Würgler-Hauri CC, Dourte LM, Baradet TC, Williams GR, Soslowsky LJ (2007) Temporal expression of 8 growth factors in tendon-to-bone healing in a rat supraspinatus model. J Should Elb Surg 16(5 Suppl):198–203
Yao JL, Ryan CK, Francis CW, Kohli M, Taubman MB, Khorana AA (2009) Tissue factor and VEGF expression in prostate carcinoma: a tissue microarray study. Cancer Invest 27(4):430–434
Zhang F, Liu H, Stile F, Lei MP, Pang Y, Oswald TM, Beck J, Dorsett-Martin W, Lineaweaver WC (2003) Effect of vascular endothelial growth factor on rat Achilles tendon healing. Plast Reconstr Surg 112(6):1613–1619
Author information
Authors and Affiliations
Corresponding author
Additional information
Patricia E. Heisterbach and Atanas Todorov are equally contributing first authors.
Rights and permissions
About this article
Cite this article
Heisterbach, P.E., Todorov, A., Flückiger, R. et al. Effect of BMP-12, TGF-β1 and autologous conditioned serum on growth factor expression in Achilles tendon healing. Knee Surg Sports Traumatol Arthrosc 20, 1907–1914 (2012). https://doi.org/10.1007/s00167-011-1772-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1772-x