Abstract
Purpose
The first purpose of this study was to examine whether fluoroscopic-based navigation system contributes to the accuracy and reproducibility of the bone tunnel placements in single-bundle anterior cruciate ligament (ACL) reconstruction. The second purpose was to investigate the application of the navigation system for double-bundle ACL reconstruction.
Methods
A hospital-based case–control study was conducted, including a consecutive series of 55 patients. In 37 patients who received single-bundle ACL reconstruction, surgeries were performed with this system for 19 knees (group 1) and without this system for 18 knees (group 2). The positioning of the femoral and tibial tunnels was evaluated by plain sagittal radiographs. In 18 patients who received double-bundle ACL reconstruction using the navigation system (group 3), the bone tunnel positions were assessed by three-dimensional computed tomography (3D-CT). Clinical assessment of all patients was followed with the use of Lysholm Knees Score and IKDC.
Results
Taking 0% as the anterior and 100% as the posterior extent, the femoral tunnels were 74.9 ± 3.0% in group 1 and 71.5 ± 5.8% in group 2 along Blumensaat’s line, and the tibial tunnels were 42.3 ± 1.4% in group 1 and 42.5 ± 4.6% in group 2 along the tibia plateau. The bone tunnel positions in group 1 were located significantly closer to the position planned preoperatively and varied less in both femur and tibial side, compared with those without navigation (group 2). (Femur: P < 0.05, Tibia: P < 0.001) 3D-CT evaluation of double-bundle ACL reconstruction (group 3) also demonstrated that the bone tunnel positions of both anteromedial (AM) and posterolateral (PL) were placed as we expected.
Conclusion
The fluoroscopic-based navigation system contributed to the more reproducible placement of the bone tunnel during single-bundle ACL reconstruction compared with conventional technique. Additionally, this device was also useful for double-bundle ACL reconstruction.
Level of evidence
Case–control study, Therapeutic study, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
One of the most critical factors for successful anterior cruciate ligament (ACL) reconstruction and long-term stability is the bone tunnel placements [15, 20, 22, 40]. However, to place the bone tunnels in reproducible and correct positions is technically challenging under only arthroscopic view in ACL reconstruction. Previous radiological and cadaveric studies indicate that approximately 10–40% of drill holes in primary ACL reconstructions have been incorrectly placed [4, 18, 38]. New strategies to acquire ideal graft placements as expected in ACL reconstructions are therefore emerging.
To this end, navigation systems have been developed to assist in the accuracy of tunnel placement [7, 23] and the restoration of the knee kinematics more closely to physiologic condition after ACL reconstruction [25, 34, 41]. However, there is little evidence examining the feasibility and usefulness for the bone tunnel creation of navigation system in the clinical setting [8, 14, 29].
Furthermore, precise placements of bone tunnels are more significant in double-bundle ACL reconstruction [13, 33], which has been popular recently due to good rotational stability [1, 31]. Therefore, the navigation system is sure to be useful in this technique.
The aim of this study was to prove the hypothesis that fluoroscopic-based navigation system contributes to the accuracy and reproducibility of bone tunnel placements in single-bundle ACL reconstruction than those of conventional method. The second object of this study was to examine the application of the navigation system to double-bundle ACL reconstruction from the aspects of radiographic outcomes.
Materials and methods
A hospital-based case–control study was conducted, including a consecutive series of 55 patients (26 men, 29 women) who underwent primary reconstruction of the ACL by a single surgeon (T.H.), between 2006 and 2008, using a hamstring tendon autograft. The study was performed with the approval of the institutional review board, and all patients signed the consent form drafted for the study. All patients in this study received surgery at one institution (Takatsuki General Hospital), and all patients involved in this study were followed up for at least 3 years. Patients with associated ligament injuries requiring surgical treatment, evidence of chondral damage, or degeneration were excluded from this study. Those who refused to participate in this study were also excluded.
Among them, 19 knees in 19 patients (9 men, 10 women) underwent single-bundle ACL reconstruction using the fluoroscopic-based navigation system (group 1). Another 18 knees in 18 patients (8 men, 10 women) were underwent single-bundle ACL reconstruction without this system and were served as the control group (group 2). Double-bundle ACL reconstruction was performed by the use of navigation in other 18 patients (9 men, 9 women; group 3). Demographic data of the patients are shown in Table 1. All patients were followed up for at least 36 months postoperation. The mean follow-up period was 47.6 months (range, 36–60 months). All patients had unilateral injures. Associated surgery at the time of reconstruction included partial menisectomy (7 knees) and meniscal repair (10 knees).
Navigation system
A computer-assisted fluoroscopic-based navigation system (Vectorvison® ACL system, BrainLAB, Heimstetten, Germany) was used in this study. This system comprises a C-arm fluoroscope and a navigation system. The navigation system has two devices consisting of a core machine with a digitizing camera, which localizes the C-arm calibration target and all of the trackable instruments, and the navigation display. The mean probe tip error of this system is reported to be 0.97 ± 0.49 mm [10, 21].
At the beginning of the surgery, a reference frame was rigidity attached to the midshaft of the distal femur and proximal tibia by two threaded pins to track the position of the patient’s leg during the procedure. And anteroposterior (AP) and lateral view images of the knee joint were obtained by C-arm fluoroscopy to capture the calibration target and the reference frame simultaneously by the camera. Next, to provide detailed information on planned positions, the notch geometry and the insertion areas of the ACL on femoral and tibial side were roughly traced under arthroscopic control using navigation pointers. After registration was completed, operative instruments with reference markers were displayed on the fluoroscopic image of the navigation monitor in a real-time manner, regardless of the actual position of the knee during operation.
Surgical procedure
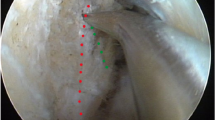
When we used the navigation system, the centers of bone tunnels in femur and tibia were planned on the lateral radiograph using the navigation system according to the Quadrant methods [5] for the femur and Staublis methods [35] for the tibia. In the single-bundle reconstruction, the center of the tibial tunnel was aimed 43% along the tibial plateau, with 0% as the anterior and 100% as the posterior extent. The center of the femoral insertion of the ACL was aimed at low and shallow corner of the deepest and highest quadrant (Fig. 1a). In the double-bundle ACL reconstruction, the center of the anteromedial (AM) tibial bone tunnel was placed 30% and posterolateral (PL) tibial bone tunnel was 44% along the tibial plateau as recommended by previous reports [42] (Fig. 1b). On the femoral side, as shown in the previous cadaveric studies [39, 42], the AM tunnel was aimed at 25% from the deep margin in a deep-shallow direction and at 16% from Blumensaat’s line in a high-low direction, and the PL tunnel was aimed at 30% in a deep-shallow direction and at 42% in a high-low direction, according to the quadrant method described by Bernard et al. [5] (Fig. 1c).
a The ideal bone tunnel positions in single-bundle ACL reconstruction. White closed circles show ideal bone tunnel positions. b The ideal tibial bone tunnel positions in double-bundle ACL reconstruction. c The ideal femoral bone tunnel positions in double-bundle ACL reconstruction. Black closed triangle shows the AM bundle, and black closed circle shows the PL bundle
The system was able to show the predicted position of bone tunnels and the ACL graft route on the navigation (Fig. 2). We created bone tunnels at the setup positions using a transtibial technique. If there is a possibility of the predicted bone tunnel communication or the notch impingement, it requires a minimum amount of adjustment. Finally, the graft was placed and then fixed with Endo-button CL (Smith & Nephew, Andover, MA) on the femur and a cancellous bone screw on the tibia at 20° of knee flexion.
Femoral and tibial arthroscopic navigated K-wire drilling in operation of the navigation surgery. The reference frames of the tibia (a) and femur (b) and a tibial drill guide (c) are seen. Display of the navigation images on the screen shows the expected bone tunnel placements in fluoroscopic image, in addition to the conventional arthroscopic view
When we did not use the navigation system, the center of the tibial tunnel was placed around where the ACL had been attached. And the femoral tunnel was aimed to place at the 10:30-o’clock position in a right knee and the 1:30-o’clock position in a left knee with reference to original footprint under arthroscopic view. The other surgical procedures did not differ from those in navigation groups.
Postoperative rehabilitation
Postoperatively, continuous passive motion (CPM) exercises were started immediately after surgery, and weight bearing was begun as soon as tolerable, usually on the third postoperative day. Patients were encouraged to resume a full range of joint motion by 12 weeks. Jogging started after 4 months, and return to full sports activity was permitted from 6 months at the earliest.
Radiological assessments
The location of the bone tunnels was evaluated on non-weight-bearing lateral-view radiograph 1, 6, and 12 months after surgery. The lateral view was obtained in an intermediary position, by carefully confirming the rotation of the knee. In the double-bundle ACL reconstruction (group 3), 3D-CT was taken 3 months after surgery. All parameters on radiographs were independently assessed by two observers (Y.K. and Y.H.) using an image analyzer [Volume Graphics GmbH Studio MAX software (Heidelberg, Germany)] and calculated to one decimal place. The results reported represent those of observer 1 (Y.K.). The decision to use the results of one examiner was made once reliability was established. Intra-observer Spearman–Brown coefficient was 0.87, and the intra-class correlation was 0.84, which Landis and Koch [24] suggest may be substantial agreement.
In single-bundle reconstruction groups (group 1, 2), the center position of the tibial tunnel was calculated and expressed as a percentage of the total length of the tibia plateau on the lateral radiograph (a/t in Fig. 3a). Placement of the center of the femoral tunnel was also assessed as a percentage of the total length of the Blumensaat’s line on the lateral radiograph (b/f in Fig. 3a).
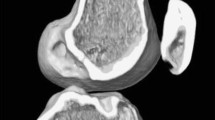
a Radiographic parameters used to evaluate the positioning of the tibial and femoral tunnel in this study. The method of measuring the tunnel position in single-bundle ACL reconstruction is demonstrated in the sagittal radiograph. The center of the tibial tunnel was expressed as a percentage of the total length of the tibia plateau on the lateral radiograph (a/t). The center of the femoral tunnel was expressed as a percentage of the total length of the Blumensaat’s line on the lateral radiograph (b/f). a, the distance of the center of tibia tunnel from the anterior edge of tibia plateau; b, the distance of the center of femur tunnel from the anterior femoral condyle; t, the total length of the tibia plateau; f, the total length of the Blumensaat’s line. b The method of measuring the tunnel position in double-bundle ACL reconstruction is demonstrated in the 3D-CT
In cases of the double-bundle reconstruction group (group 3), three-dimensional computed tomography (3D-CT) was used to assess the bone tunnel placement. Femoral tunnels were assessed on the sagittal plane, and tibial tunnels were assessed on the axial plane (Fig. 3b).
Clinical assessments
To compare the functional state among the three groups, all patients were assessed preoperatively and 24 months after surgery using the International Knee Documentation Committee forms (IKDC) evaluation and Lysholm knee score. Postoperative ligamentous stability was assessed using the Lachman test and Pivot-shift examinations and graded per IKDC criteria. Assessments were performed by a surgeon (T.H.) and a physiotherapist (not an author). The examiners were not informed about operative techniques (navigated or conventional, single-bundle or double-bundle) used in each patient. All patients had long pants during testing in order to hide the scars left by the trackers. Postoperative complications were also evaluated.
Statistical analysis
Based on the previous pilot study, we determined that we would need 17 samples to detect difference in bone tunnel placements as calculated using G*power 3.1 [9] when alpha was set at 0.05 and power was set at 0.9. Similarly, 15 patients in each group would be required to demonstrate a difference in clinical assessment when alpha was set at 0.05 and power was set at 0.9. The results were statistically analyzed using a software package (Graph Pad Prism™, MDF software, Inc). All values were expressed as mean ± standard deviation (SD). Statistical analysis was performed using the F test for analysis of variance of the two groups. The multiple comparisons among groups were made using a one-way analysis of variance (ANOVA). Post hoc analysis was performed by Fisher’s protected least significant difference test. The comparison of clinical instability results was performed with Fisher’s exact test and chi-square test. Statistical significance was defined as P < 0.05.
Results
Bone tunnel positions of single-bundle ACL reconstruction
In the navigation group (group 1), the midpoint of the tibial tunnel was located at a mean (and standard deviation) of 42.3 ± 1.4% posterior along the tibial plateau. The midpoint of the femoral tunnel was located at a mean of 74.9 ± 3.0% posterior along Blumensaat’s line. In the control group (group 2), the midpoint of the tibial tunnel was located at a mean of 42.5 ± 4.6% posterior along the tibial plateau, and the midpoint of the femoral tunnel was located at a mean of 71.5 ± 5.8% posterior along Blumensaat’s line. The distributions of the midpoint of placements of the tibial and femoral tunnels are shown in Fig. 4a. Measurement data at the tibial and femoral side in single-bundle ACL reconstruction are shown in Table 2.
a The distribution of the radiological femoral and tibial tunnel placements in single-bundle ACL reconstruction. Closed box shows group 1 (navigation group), and closed diamond shows group 2 (control group). b 3D-CT evaluation of double-bundle ACL reconstruction. Closed triangles demonstrate the distribution of the bone tunnel of the AM, and closed circles demonstrate the distribution of the bone tunnel of the PL. Open triangle and circle show the ideal bone tunnel placements as planned before the operation. *P < 0.05, **P < 0.001
When we compared the bone tunnel placements and dispersion of the single-bundle ACL reconstruction between both groups, the bone tunnels using navigation (group 1) were located more closely to the position which we had planned before the operation and varied less on both the femur and the tibial side (P < 0.05, P < 0.001, respectively).
Bone tunnel positions of double-bundle ACL reconstruction
In the 3D-CT evaluation of the double-bundle ACL reconstruction, the dispersions of the bone tunnel positions are demonstrated in Fig. 4b. Measurement data at the tibial and femoral side in double-bundle ACL reconstruction are shown in Table 3. 3D-CT images showed that the centers of the PL tunnels of the tibia side tended to be located posterior to our predicted positions in order to avoid connection with the AM tunnels. However, the other tunnel positions were placed as planned before the operation.
Physical examination
The mean Lysholm knee scale was 92.8 ± 5.5 (group 1), 90.2 ± 8.3 (group 2), and 93.3 ± 3.5 (group 3), and the mean subjective IKDC score was 91.1 ± 5.5 (group 1), 87.8 ± 5.1 (group 2), and 92.5 ± 4.0 (group 3). In this study, we found no statistical differences in Lysholm Knee scale and subjective IKDC score among the three groups.
The Lachman examination was positive in three cases postoperatively, described as IKDC criteria 1. Two patients were in group 2, and the other one was in group 1. The Pivot-shift examination was positive in five cases described as IKDC criteria 1 (glide) postoperatively. Three patients were in group 2, and the other two were in group 1. No postoperative instability was found in group 3. However, there was no statistical difference among three groups in Lachman test and Pivot-shift test in this short series.
Complications
One patient (group 1) suffered a local infection at the tibia insertion for the navigation antenna. Surgery and the postoperative courses were uneventful for all other patients in all groups.
Discussion
The major finding of the present study was that the fluoroscopic-based navigation system improves the accuracy and reproducibility of tunnel placement in single-bundle ACL reconstruction. Moreover, in the cases of double-bundle ACL reconstruction, we could place the bone tunnels as planned using this navigation system as illustrated in postoperative 3D-CT scanning.
Individual variation in joint geometry and the difficulty in intra-operative arthroscopic identification of correct insertions are supposed to be the main causes of bone tunnel misplacement [4, 6, 18]. For example, the intercondylar roof angle varies from 22° to 64° [2]. In chronic cases, original anatomical foot prints are indefinable, and anterior subluxation of the tibia is revealed [3]. Because it is difficult to evaluate such variation and identify the correct insertions by arthroscopy, the surgeon sometimes needs to confirm the location of the guide pin by intra-operative radiography or fluoroscopy [12, 19]. However, recognition of the exact pin position using regular radiography is difficult because the radiographs are often obtained in an improper orientation. The navigation system is helpful in tackling such problems. There are two advantages with the use of this navigation system for ACL reconstruction: (1) This device renders the reconstruction more reproducible, eliminating the problem of skeletal variation among patients, and (2) a surgeon can perform the ACL reconstruction under not only an arthroscopic but also a navigated view in real time and prevent the breakout of the posterior femur wall and the roof impingements by the prediction of tunnel positions before drilling. Therefore, accurate guide pin placement to the designed position can be easily accomplished during the first attempt. The results of this study showed that we could place the bone tunnels more reproducible placement to the designed position by using this navigation system than control group. This outcome is consistent with our hypothesis that navigation system is useful to improve the accuracy of the bone tunnel placement.
For ACL reconstruction surgery, there are two types of navigation system, image-free navigation [14, 17] and fluoroscopic-based navigation, which is based on an image monitor [23, 26]. Image-free ACL navigation systems determine the tunnel position based on intra-operative bone surfacing parameters. However, similar to conventional arthroscopic methods, they are restricted by arthroscopic problems of identifying the ACL insertions. Therefore, these navigation systems resulted in a considerable variation among operators. In contrast, fluoroscopic-based ACL navigation systems, as used in this study, require image acquisition at the beginning of the surgery. Once the images have been recorded, the procedure with this system is simple. The contribution of fluoroscopic images to the identification of ACL insertion and mapping of the bone surface can help achieve a reproducible drill hole planning for ACL reconstruction according to radiological parameters, thus facilitating precise drill-hole placement. Klos et al. [23] reported that the technique with the navigation system significantly reduced the variability of graft placement in their clinical trial. For the placement of the tibial portion of the graft, the SD of the anterior/posterior graft location decreased from 6% to less than 3%. Additionally, Nakagawa et al. [26] also referred that fluoroscopic-based navigation was useful for technically demanding revision ACL reconstructions.
In context with double-bundle ACL reconstruction, navigation systems are of special interest. Recently, some previous reports demonstrated the usefulness of navigation-assisted anatomical double-bundle ACL reconstruction [27, 36, 37]. In our study, we could place the bone tunnels as planned using this navigation system as illustrated in postoperative 3D-CT scanning. As far as we know, this is the first report that demonstrates the clinical application of the fluoroscopic-based navigation system for double-bundle ACL reconstruction. However, there are still some problems to solve before the navigation system can come into widespread clinical use for double-bundle reconstruction; namely, the most optimal places for double-bundle ACL reconstruction are still controversial [16, 28, 39, 42]. To perform anatomic AM and PL bone tunnel placements, topographical osseous anatomical landmarks such as resident’s ridge [32] and lateral bifurcate ridge [11] on the femoral side, and the medial and lateral intercondylar tubercles on the tibial side [30] were reported to be important. Ishibashi et al. demonstrated that the osseous landmarks can be very useful during navigation-assisted ACL reconstruction in their cadaveric study [17]. We believe that this fluoroscopic-based navigation system also contributed to identify such osseous landmarks more clearly by combining intra-operative fluoroscopic images with actual arthroscopic images.
We did not compare navigation-based double-bundle ACL reconstruction with conventional methods, and this may be appear to be a limitation of this study warrants discussion. However, there was little previous clinical study reporting the effect of navigation on double-bundle ACL reconstruction, and our primary object was to demonstrate the therapeutic potential of navigation system as a new tool for double-bundle ACL reconstruction. Another point that requires discussion is no statistic difference between navigation groups and control group in clinical outcomes in our short-time follow-up study. The role of fluoroscopic navigation system on clinical performance and longevity need further investigation with larger sample sizes and longer-term randomized trials.
We believe that the fluoroscopic-based navigation system will be valuable as an assisting device for conventional arthroscopic ACL reconstruction because this system improves visibility of the surgical field and increases the geometric accuracy during surgical procedure. Moreover, we believe that we can do technically demanding double-bundle ACL reconstruction more safely by using this system.
Conclusion
This study demonstrated that computer-assisted fluoroscopic-based navigation system can improve the accuracy for designed ACL insertion site and decrease the dispersion of the femur and tibial bone tunnel placements in single-bundle ACL reconstruction. Additionally, the availability of the system for double-bundle ACL reconstruction was shown in this paper. It is necessary to consider the extra work involved in the navigation system; however, the use of fluoroscopic navigation system may be helpful in placing the bone tunnel in the predetermined position with accuracy and repeatability during ACL reconstruction.
References
Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N (2010) Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med 38:25–34
Almekinders LC, Chiavetta J (2001) Tibial subluxation in anterior ligament-deficient knees: implications for tibial tunnel placement. Arthroscopy 17:960–962
Amis AA, Jakob RP (1998) Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg Sports Traumatol Arthrosc 6(Suppl 1):S2–S12
Behrend H, Stutz G, Kessler MA, Rukavina A, Giesinger K, Kuster MS (2006) Tunnel placement in anterior cruciate ligament (ACL) reconstruction: quality control in a teaching hospital. Knee Surg Sports Traumatol Arthrosc 14:1159–1165
Bernard M, Hertel P, Hornung H, Cierpinski T (1997) Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg 10:14–22
Bicer EK, Lustig S, Servien E, Selmi TA, Neyret P (2010) Current knowledge in the anatomy of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 18:1075–1084
Burkart A, Debski RE, McMahon PJ (2001) Precision of ACL tunnel placement using traditional and robotic techniques. Comput Aided Surg 6:270–278
Cheng T, Liu T, Zhang G, Zhang X (2011) Computer-navigated surgery in anterior cruciate ligament reconstruction: are radiographic outcomes better than conventional surgery? Arthroscopy 27:97–100
Faul F, Erdfelder E, Lang AG et al (2007) G*power 3: a flexible statistical power analysis program for social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Foley KT, Simon DA, Rampersaud YR (2001) Virtual fluoroscopy: computer-assisted fluoroscopic navigation. Spine 26:347–351
Fu FH, Jordan SS (2007) The lateral intercondylar ridge-a key to anatomic anterior cruciate ligament reconstruction. J Bone Joint Surg Am 89:2103–2104
Halbrecht J, Levy IM (1993) Fluoroscopic assist in anterior cruciate ligament reconstruction. Arthroscopy 9:533–535
Hantes ME, Liantsis AK, Basdekis GK, Karantanas AH, Christel P, Malizos KN (2010) Evaluation of the bone bridge between the bone tunnels after anatomic double-bundle anterior cruciate ligament reconstruction: a multidetector computed tomography study. Am J Sports Med 38:1618–1625
Hart R, Krejzla J, Svab P, Kocis J, Stipcak V (2008) Outcomes after conventional versus computer-navigated anterior cruciate ligament reconstruction. Arthroscopy 24:569–578
Howell SM, Taylor MA (1993) Failure of reconstruction of the anterior cruciate ligament due to impingement by the intercondylar roof. J Bone Joint Surg Am 75:1044–1055
Iriuchishima T, Ingham SJ, Tajima G, Horaguchi T, Saito A, Tokuhashi Y, Van Houten AH, Aerts MM, Fu FH (2010) Evaluation of the tunnel placement in the anatomical double-bundle ACL reconstruction: a cadaver study. Knee Surg Sports Traumatol Arthrosc 18:1226–1231
Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S (2006) Future of double-bundle anterior cruciate ligament (ACL) reconstruction: incorporation of ACL anatomic data into the navigation system. Orthopedics 29:S108–S112
Jaureguito JW, Paulos LE (1996) Why grafts fail. Clin Orthop Relat Res 325:25–41
Kasten P, Szczodry M, Irrgang J, Kropf E, Costello J, Fu FH (2010) What is the role of intra-operative fluoroscopic measurement to determine tibial tunnel placement in anatomical anterior cruciate ligament reconstruction? Knee Surg Sports Traumatol Arthrosc 18:1169–1175
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217
Khadem R, Yeh CC, Sadeghi-Tehrani M (2000) Comparative tracking error analysis of five different optical tracking systems. Comput Aided Surg 5:98–107
Khalfayan EE, Sharkey PF, Alexander AH, Bruckner JD, Bynum EB (1996) The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med 24:335–341
Klos TV, Habets RJ, Banks AZ, Banks SA, Devilee RJ, Cook FF (1998) Computer assistance in arthroscopic anterior cruciate ligament reconstruction. Clin Orthop Relat Res 354:65–69
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Lane CG, Warren RF, Stanford FC, Kendoff D, Pearle AD (2008) In vivo analysis of the pivot shift phenomenon during computer navigated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 16:487–492
Nakagawa T, Hiraoka H, Fukuda A (2007) Fluoroscopic-based navigation-assisted placement of the tibial tunnel in revision anterior cruciate ligament reconstruction. Arthroscopy 23:441–444
Nakagawa T, Takeda H, Nakajima K (2008) Intraoperative 3-dimensional imaging-based navigation-assisted anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:1161–1167
Pietrini SD, Ziegler CG, Anderson CJ, Wijdicks CA, Westerhaus BD, Johansen S, Engebretsen L, LaPrade RF (2011) Radiographic landmarks for tunnel positioning in double bundle ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 19:792–800
Plaweski S, Cazal J, Rosell P, Merloz P (2006) Anterior cruciate ligament reconstruction using navigation: a comparative study on 60 patients. Am J Sports Med 34:542–552
Purnell ML, Larson AI, Clancy W (2008) Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med 36:2083–2090
Seon JK, Gadikota HR, Wu JL, Sutton K, Gill TJ, Li G (2010) Comparison of single- and double-bundle anterior cruciate ligament reconstructions in restoration of knee kinematics and anterior cruciate ligament forces. Am J Sports Med 38:1359–1367
Shino K, Suzuki T, Iwahashi T (2010) The resident’s ridge as an arthroscopic landmark for anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18:1164–1168
Snow M, Stanish WD (2010) Double-bundle ACL reconstruction: how big is the learning curve? Knee Surg Sports Traumatol Arthrosc 18:1195–1200
Song EK, Seon JK, Park SJ, Hur CI, Lee DS (2009) In vivo laxity of stable versus anterior cruciate ligament-injured knees using a navigation system: a comparative study. Knee Surg Sports Traumatol Arthrosc 17:941–945
Staubli HU, Rauschning W (1994) Tibial attachment area of the anterior cruciate ligament in the extended knee position. Anatomy and cryosections in vitro complemented by magnetic resonance arthrography in vivo. Knee Surg Sports Traumatol Arthrosc 2:138–146
Taketomi S, Nakagawa T, Takeda H, Nakajima K, Nakayama S, Fukai A, Hirota J, Kachi Y, Kawano H, Miura T, Fukiu N, Nakamura K (2011) Anatomical placement of double femoral tunnels in anterior cruciate ligament reconstruction: anteromedial tunnel first or posterolateral tunnel first? Knee Surg Sports Traumatol Arthrosc 19:424–431
Tensho K, Kodaira H, Yasuda G, Yoshimura Y, Narita N, Morioka S, Kato H, Saito N (2011) Anatomic double-bundle anterior cruciate ligament reconstruction, using CT-based navigation and fiducial markers. Knee Surg Sports Traumatol Arthrosc 19:378–383
Topliss C, Webb J (2001) An audit of tunnel position in anterior cruciate ligament reconstruction. Knee 8:59–63
Tsukada H, Ishibashi Y, Tsuda E, Fukuda A, Toh S (2008) Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci 13:122–129
Vergis A, Gillquist J (1995) Graft failure in intra-articular anterior cruciate ligament reconstructions: a review of the literature. Arthroscopy 11:312–321
Voos JE, Musahl V, Maak TG, Wickiewicz TL, Peale AD (2010) Comparison of tunnel positions in single-bundle anterior cruciate ligament reconstructions using computer navigation. Knee Surg Sports Traumatol Arthrosc 18:1282–1289
Zantop T, Wellmann M, Fu FH, Petersen W (2008) Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med 36:65–72
Acknowledgments
The authors would like to thank Ms. Janina Tubby and Mr. Daniel Gilpin for help in preparing the manuscript. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article, nor have any funds been received in support of this study.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Kawakami, Y., Hiranaka, T., Matsumoto, T. et al. The accuracy of bone tunnel position using fluoroscopic-based navigation system in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20, 1503–1510 (2012). https://doi.org/10.1007/s00167-011-1726-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1726-3