Abstract
With the abundance of anatomic double bundle ACL reconstruction techniques that currently exist and limited patient outcome data, one has to ask whether or not they should be used and if so, which one, and what is the learning curve for the average knee surgeon to become competent with the technique that they select? The purpose of this literature review is to summarize existing anatomic double bundle ACL reconstruction surgical and rehabilitation techniques and the clinical and biomechanical study evidence that currently exists. In choosing to perform anatomic double bundle ACL reconstruction we suggest that the knee surgeon should look for evidence of: (1) control of the pivot shift phenomenon, (2) improved transverse plane rotatory knee control during the performance of sports type movements, (3) a decreased likelihood of revision procedures either for ACL reconstruction or for treatment of associated primary or recurrent meniscal injuries, (4) improved patient self-reports of perceived function, satisfaction, and quality of life, and (5) radiographic evidence of a lower incidence and/or magnitude of osteoarthritic changes compared to conventional single bundle ACL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 75,000–100,000 ACL reconstruction surgeries are performed annually in the USA [35]. However, 85% of orthopaedic surgeons perform less than ten ACL reconstruction procedures per year [52]. The majority of the literature on ACL reconstruction has reported 80–90% patient outcome success rates, however, approximately 10–30% of patients continue to experience persistent knee pain and instability [12, 28]. If revision surgery is necessary, the most prevalent cause is faulty surgical technique, particularly improper tibial and femoral bone tunnel placement [52, 55, 87].
A true consensus does not exist for optimal ACL reconstruction femoral tunnel position or for determining the landmarks that best identify its true location. Using cadaveric dissection and radiographic techniques, Colombet et al. [16] provided detailed anteromedial (AM) and posterolateral (PL) ACL bundle attachment locations independent of knee flexion angle based on Amis and Jakob’s line. Mochizuki et al. [75] in studying ten cadaveric knee specimens using digital photography reported that the distance from the attachment center of each AM and PL bundle to the posterior femoral articular surface border averaged 6.3 ± 0.6 mm and 8.6 ± 0.6 mm, respectively. The center of the AM and PL bundles was described as 1:40 and 3:10 o’clock intraarticular “lateral wall clock” positions, respectively, at the left knee. Using cadaveric specimens and radiographic techniques, Giron et al. [34] compared femoral tunnel position using double incision, transtibial, and anteromedial portal tunnel drilling techniques reporting that each could be used to effectively achieve sufficiently deep femoral tunnel positioning. Most surgeons who use a single tunnel technique recommend using a 1:00 o’clock femoral tunnel position, some however recommend moving more horizontally to a 3:00 o’clock position referenced to the left knee [21].
Disagreement also exists regarding graft type, fixation method, and the need for graft bundle tensioning [2, 3]. The most common grafts used for ACL reconstruction today are quadruple stand hamstring and bone-patellar tendon-bone autografts [41, 52], however, trends are moving toward other graft sources, including allografts [22, 41, 56]. Because of their greater length and strength, allografts and hamstring autografts become increasing more useful when, the selected ACL reconstruction technique attempts to reconstruct more than one functional ACL bundle [12].
Each of the two primary ACL bundles has a unique function [5–7, 18, 31, 40, 45, 47, 61, 62, 82, 84], however, the intermediate bundle has a more variable morphology and its functional significance is less well understood [82, 101]. The AM bundle and PL bundle are oriented near parallel with the knee extended, and twist around each other as the knee flexes [104]. Mott [77] and later Zaricznyj [121] were two of the first to report using a double bundle technique to anatomically reconstruct the ACL. In an attempt to more closely recreate native anatomy and better replicate natural ACL function more knee surgeons are beginning to employ anatomic double bundle ACL reconstruction techniques. However, in association with these innovations questions arise regarding the efficacy of selecting a relatively unproven surgical technique versus conventional single bundle ACL reconstruction techniques which having accumulated a considerable and growing body of long-term outcome data to support their efficacy [20, 21, 42]. Potential complications associated with anatomic double bundle ACL reconstruction includes more difficult revision with double tunnels, notch impingement with a larger tibial side footprint, a lack of appropriate guide instrumentation for tunnel placements, greater likelihood for incorrect tunnel placement (particularly when multiple tunnels are created), no consensus on graft tensioning or for the flexion-extension angle for graft fixation, the potential for intra-tunnel bone bridge fracturing [9, 120], and numerous techniques with a very limited number of clinical studies to support the superiority of any one of them [52]. Complications reported following anatomic double bundle ACL reconstruction including inflammatory responses to intra-articular sutures [11], endobutton pulling through with the PL bundle graft and fracturing the femoral metaphyseal surface [11], and supracondylar femoral fracture [105].
If anatomic double bundle ACL reconstruction techniques are found to be more effective than conventional single bundle ACL reconstruction techniques for re-establishing ACL function by better controlling both tibial translation and rotation, should this procedure be performed on all patients or only those who might benefit most from its proposed benefits? Fu [26] has asked whether or not some patients have greater transverse plane rotational dependence at the knee than others? If an anatomic double bundle ACL reconstruction technique is chosen, the increased number of tunnels or graft bundles that are created may lead to a greater potential number and severity of complications should revision surgery be needed. With the abundance of anatomic double bundle ACL reconstruction techniques that are discussed in this report, what is the learning curve for the average knee surgeon to become competent with the one that they select? This literature review summarizes existing anatomic double bundle ACL reconstruction surgical techniques and the clinical and biomechanical study evidence that currently exists. From existing information a criteria for selecting an anatomic double bundle ACL reconstruction technique will be proposed.
ACL anatomy
Although the mid-substance diameter of the AM bundle is 7 ± 1 mm and that of the PL bundle is 6 ± 1 mm, fan-shaped femoral and tibial attachment sites range from 3 to 5 times the mid-substance diameters [40, 106]. In evaluating 20 intact knees from aborted fetuses at 18–23 weeks gestation, Ferretti et al. [23] reported two distinct ACL bundles within the same compartment that were covered by a synovial membrane and divided by a vascular septum. Levicoff et al. [63] in examining 12 intact knee joints from aborted fetuses at 18–23 weeks gestation reported two bundles located within the same synovial membrane compartment with varying bundle sizes between specimens suggesting that some knees might have a genetic advantage over others with respect to rotational stability and strength. They suggested the need to detail the effects of environmental factors in post-natal ligament development, however, they admitted that this might be difficult given that the bundles were in the same compartment covered by a synovial membrane [63]. Steckel et al. [104] in studying the macroscopic anatomy of six cadaveric knee specimens identified an AM bundle and a PL bundle in all specimens. However, in examining 47 cadaveric knee specimens, Ito et al. [50] reported that although 55% displayed evidence of a macroscopic double bundle, 45% had a macroscopic single bundle, 19% had microscopic double bundles and 26% had a microscopic single bundle. Additionally, their investigation revealed no anatomical evidence of clearly separate bundle insertion sites. Shino et al. [101] has described reconstructing the AM bundle, the PL bundle, and the more variable and less understood intermediate bundle. Perfectly replicating anatomic double bundle ACL graft placement may not be as important as creating double bundles that adequately simulate the reciprocating mechanical function of the native ACL bundles [71] in association with the posterior cruciate ligament [74]. Alluding to the functional differentiation between the AM and PL bundles of the ACL, Fu et al. [27] reported that the AM bundle is more often torn from its femoral insertion site while the PL bundle more often demonstrates mid-substance tears or elongation. They suggested that future studies should focus on bundle specific ACL injury mechanisms [27].
Double bundle ACL biomechanics
The AM bundle of the ACL is normally tighter in flexion and the PL bundle is tighter in extension [6, 45, 62]. These bundles have differing tension levels as the knee flexion angle changes and the PL bundle is particularly important for providing transverse plane rotational knee stability as the knee nears full extension [5, 29, 62, 98]. Sakane et al. [98] in studying native ACL bundle function in cadaveric knee specimens under anterior tibial loads (22–110 N) between 0–90° flexion using a robotic manipulator reported non-uniform bundle function with PL bundle tension affected more by knee flexion angle and anterior tibial load. They concluded that both bundles should be reconstructed to adequately restore native ACL function [98]. Gabriel et al. [29] also measured in situ native ACL forces in cadaveric knee specimens with 134 N loads at 0°, 30°, 60°, and 90° knee flexion, with and without combined 5 Nm internal rotation loads and 10 Nm valgus knee torque at 15° and 30° knee flexion. They reported that PL bundle in situ forces were greatest at full knee extension and decreased with increasing flexion. In situ AM bundle forces progressively increased up to 60° knee flexion. Under combined rotatory loads PL bundle in situ forces were higher at 15° and lower at 30° knee flexion. They concluded that the PL bundle is particularly important under combined loads when the knee is near full extension.
Lateral femoral condylar “roll-back” normally occurs with a relatively stable medial compartment during knee flexion and the ACL contributes to the “screw home” movement associated with external tibial rotation during end range knee extension. In the ACL deficient knee, however, there is a relative posterior and medial shift of the femoral condyles relative to the tibia [44, 51, 64] that may contribute to the progressive use of a more capsuloligamentous postural dependency during weight bearing.
In biomechanical studies using cadaveric knee specimens, Woo et al. [113] and Yagi et al. [115] have shown how conventional single bundle ACL reconstruction is effective at limiting anterior tibial translation, however, it does not effectively control combined internal rotation and valgus loads. Yagi et al. [115] reported that an anatomic double bundle ACL reconstruction better controlled transverse plane rotational loads at 30° knee flexion recreating approximately 91% of the control observed in non-impaired knee specimens compared to only 66% using a conventional single bundle ACL reconstruction technique. Biomechanical studies using cadaveric knee specimens however have reported that a more horizontally placed femoral tunnel using conventional single bundle ACL reconstruction techniques also increases transverse plane rotational knee stability and anterior tibial translational stability [65, 79]. Yamamoto et al. [116] reported that lateral tunnel placement with a conventional single bundle ACL reconstruction, however, only restores both transverse plane rotational knee stability and anterior tibial translational stability similarly to an anatomic double bundle ACL reconstruction when the knee is near full extension with reduced effectiveness at greater knee flexion angles. Mae et al. [66] evaluated AM and PL graft bundle forces following anatomic double bundle ACL reconstruction using two femoral and two tibial tunnels, endobutton femoral side fixation and graft tensioning at 25° knee flexion. Among 11 patients, they reported that the AM bundle carried 42.3 ± 5.7% of the total force at 0° knee flexion, while the PL bundle carried 57.7 ± 5.7% of the total force. At 90° knee flexion the AM bundle handled 64.1 ± 11.1% of the total force while the PL bundle handled 33.9 ± 11.1%. They concluded that these findings were similar to the reciprocating forces observed in the native ACL [66].
In their initial study comparing a double bundle “over-the-top” versus a single bundle “through-the-condyle” ACL reconstruction technique using polyester implants in cadaveric knee specimens, Radford et al. [93] reported that the “over-the-top” technique provided better anterior tibial translational stability at both 20° and 90° knee flexion. In a follow-up study using an in vivo sheep model and the same technique, however, they reported increased anterior tibial translational laxity compared to normal for both techniques and the double bundle ACL reconstruction group displayed more femoral condyle articular cartilage degeneration than the single bundle ACL reconstruction group at 6 months following surgery [92]. They concluded that clinical use of double bundle ACL reconstruction was not indicated based on study results and on the increased surgical complexity. Powers et al. [90] in comparing a double banded anatomical polyethylene fiber ACL prosthesis implanted either anatomically or conventionally in a goat model, reported no differences between groups for passive knee range of motion, anterior–posterior laxity, or joint space appearance at 3 months following surgery.
Mae et al. [67] in a biomechanical study using cadaveric knee specimens and quadrupled semitendinosus-gracilis (STG) autografts reported that anatomic double bundle ACL reconstruction using two femoral tunnels and one tibial tunnel controlled anterior tibial translational laxity better than a single femoral tunnel technique, however, they did not evaluate transverse plane rotational stability. Sbihi et al. [99] in comparing anterior tibial translational laxity in conventional single bundle or anatomic double bundle ACL reconstruction using cadaveric knee specimens reported that both techniques provided equivalent stability at 60° and 90° knee flexion, however, the double bundle technique provided greater control of anterior tibial translational laxity at 20° knee flexion. Summaries of the methods and results for in vitro biomechanical studies of anatomic double bundle ACL reconstruction function are reported in Table 1.
Conventional single bundle ACL reconstruction in vivo biomechanics
A growing body of clinical research evidence has demonstrated that conventional single bundle ACL reconstruction does not restore normal transverse plane knee rotatory control during walking, stair descent-sudden directional change, jump landing-sudden directional change, lunges, and downhill running [30, 94–96, 108]. Summaries of in vivo human biomechanical studies that have evaluated transverse plane rotatory knee control under ACL deficient conditions and following conventional single bundle ACL reconstruction are reported in Table 2. To date, we could not identify similar studies that have evaluated this variable following anatomic double bundle ACL reconstruction.
Anatomic double bundle ACL reconstruction surgical techniques
Some have proposed modifying the conventional single bundle ACL reconstruction technique to improve transverse plane rotatory knee stability by creating the lateral femoral tunnel through the anteromedial portal rather than using a transtibial approach [65, 79]. This enables tunnel placement at a more horizontal 2:00 or 10:00 o’clock position on the lateral wall of the femoral condyle rather than on the lateral condyle roof [14]. Shino et al. [102] described an anatomic double bundle ACL reconstruction that used a slotted bone-patellar tendon-bone autograft implanted “sideways” in an attempt to replicate AM and PL bundle function. Takeuchi et al. [107] described an anatomic double bundle ACL reconstruction technique that used one femoral and one tibial tunnel with a bone-hamstring-bone composite graft and interference screw fixation with back-up titanium spike fixation at the tibia. With this technique the graft bundle was simply twisted to create AM and PL bundles. By using a STG autograft that had a bone component, they suggested that fixation was improved without creating patellofemoral joint disorders due to bone-patellar tendon-bone graft harvest. They did not however report any patient outcome data. Bellier et al. [10], Christel et al. [15], Vidal et al. [110] and Fu et al. [27, 28] have described anatomic double bundle ACL reconstruction techniques using two femoral and two tibial tunnels and either ST and G autografts, or two tibialis anterior allografts. The technique reported by Fu et al. [27, 28], Vidal et al. [110] and Zelle et al. [122] used endobuttons to provide femoral fixation and bioabsorbable interference screws and staples, to provide tibial fixation (Fig. 1), while Bellier et al. [10] and Christel et al. [15] used the same fixation methods but without tibial side staples. Fu et al. [27, 28] suggested that in cases with a partially torn ACL that had an intact AM bundle, one advantage of their technique was that it enabled isolated PL bundle reconstruction to better restore transverse plane rotatory knee stability. Patient outcome data however was not reported. Caborn and Chang [13] reported use of a notched single femoral and single tibial tunnel anatomic double bundle ACL reconstruction technique with fixation provided by bioabsorbable interference screws (Fig. 2). Their technique emphasized accurate tunnel placement within the femoral and tibial footprints as well as the proper orientation of the bundles based on current anatomic knowledge (Fig. 3). As with other studies however no patient outcome data was reported other than mentioning “encouraging” early findings among 15 patients with no pivot shift recurrence. Morgan and Caborn [76] also reported an anatomic double bundle ACL reconstruction technique that used a tibial retroscrew to increase graft tension with screw advancement and to enhance fixation in the cortical bone of the proximal tibia. When the surgeon deemed it to be necessary, “backup” tibial fixation could be achieved with a second interference screw placed from outside-in, in an antegrade fashion, posterior to the graft, or with a post and washer. Among 50 patients who were a minimum of 2 years post-ACL reconstruction using this technique, none displayed anterior laxity >1 mm and no short term complications were reported. Ha et al. [36] reported an anatomic double bundle ACL reconstruction technique that used an Achilles tendon allograft with a single bone plug placed in the femoral tunnel. To achieve double bundles they split and twisted the graft on the tibial side fixing the AM bundle in slight knee flexion and the PL bundle in extension. No patient outcome data was reported. Marcacci et al. [68] in using an anatomic double bundle ACL reconstruction technique with one femoral and one tibial tunnel and suture-to-bone bridge fixation reported that the greater cross-sectional area and bone-tendon interface provided by the double bundle technique was advantageous (Fig. 4). Cha et al. [14] and Pederzini et al. [88] cited similar benefits associated with greater graft cross-sectional area and bone-tendon interface in using an STG autograft with two femoral and two tibial tunnels, and a quadriceps tendon autograft with one femoral and two tibial tunnels, respectively. Cuomo et al. [17] reported using a transtibial approach to place the femoral tunnel slightly anterodistal to the native ACL insertion location to enable better anatomic double bundle ACL graft function. Ogawa et al. [85] reported that an anatomic double bundle ACL reconstruction was no more effective than a conventional single bundle ACL reconstruction for restoring the normal tibiofemoral relationship as defined by the presence of a fixed anterior subluxation of 3 mm. Summaries of double bundle ACL reconstruction surgical techniques that do not report clinical findings are reported in Table 3.
Two femoral, two tibial tunnel anatomic double bundle ACL reconstruction with endobutton femoral side and interference screw tibial side fixation with back-up staples [27]
Appropriate anteromedial and posterolateral ACL bundle attachments (left femoral condyle) [13]
Clinical studies of anatomic double bundle ACL reconstruction
In a follow-up study of 202 patients at 2 years following conventional single bundle ACL reconstruction, Kocher et al. [57] reported no significant relationship between measurements of anterior tibial translational laxity and any subjective function values. The presence of a positive pivot shift, however, related significantly to lower patient satisfaction, more frequent partial and full giving way, difficulty cutting or twisting, activity limitations, poorer overall knee function, lesser sports participation, and lower Lysholm scores. The results of this study suggest that the long-term capacity for any ACL reconstruction technique to control a functional pivot shift appears to be essential to the success or failure of the intervention. This study certainly supports the premise for developing an ACL reconstruction technique that more effectively controls the functional pivot shift phenomenon.
No clear, easy to use, quantifiable method currently exists to measure the pivot shift or in vivo transverse plane rotational knee stability as part of the standard clinical examination. Reports have used 3D motion analysis, motion MRI in limited ranges of knee motion, stereofluoroscopy, and knee modeling techniques, however, no quantifiable method of measuring the pivot shift phenomenon during manual joint laxity assessment or transverse plane rotatory knee control during functional task performance that can be used both in the operating room and in the clinic has been established. Proponents of anatomic double bundle ACL reconstruction techniques have suggested improved reconstruction durability, anterior tibial translational stability and transverse plane rotational knee stability, however, very limited objective clinical evidence exists that supports its influence on improving patient outcomes. Perhaps some of the new technologies being designed for computer navigated ACL reconstruction can be adapted to also be used to provide quantifiable clinical pivot shift and transverse rotatory knee stability measurements [46, 49, 59, 72, 100]. Muneta et al. [78] in reporting 2-year follow-up results for 54 of 62 consecutive patients who underwent anatomic double bundle ACL reconstruction using a multi-strand STG autograft reported a “trend” toward enhanced anterior tibial translational stability compared with their previous experiences using a conventional single bundle ACL reconstruction technique. In describing an anatomic double bundle ACL reconstruction technique that relied on single tibial and femoral tunnels and an “over-the-top” bundle placement, Hara et al. [39] suggested that the technique was “physiologically more durable”, however, patient outcome results were not provided. Kubo et al. [60] in examining 4 of 14 patients for anterior tibial translational knee laxity following anatomic double bundle ACL reconstruction reported a “good” result and reported that the technique was a “useful method” for patients who required a “physiologically more durable ACL reconstruction”, however, patient outcome data was not provided. Hamada et al. [37] in a non-randomized study using a semitendinosus or STG autograft compared the knee stability of 160 patients who underwent anatomic double bundle ACL reconstruction using either a single or double femoral socket and who followed the same rehabilitation protocol. At 2-year follow-up with 106 available patients they reported no statistically significant group differences for IKDC Knee Ligament Evaluation grade or for anterior tibial translational laxity. They reported that the double femoral socket group displayed a “trend” toward having superior anterior tibial translational stability [37].
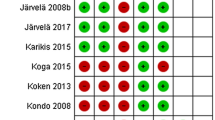
Toritsuka et al. [109] performed second look arthroscopic examinations on 153 patients at 5–51 months following anatomic double bundle ACL reconstruction using multi-stranded hamstring autografts and a single femoral socket (n = 96) or a double femoral socket (n = 60) reporting no significant differences for anterior tibial translational laxity, however, the double femoral socket technique displayed superior graft tension or thickness. They reported that in either group the grafts that displayed the greatest laxity had been implanted the longest [109]. Yasuda et al. [117, 119] described an anatomic double bundle ACL reconstruction technique that used two tibial and two femoral tunnels. With their technique all four ends of two STG autografts were placed at the center of the anatomical insertions of the AM and PL bundles of the ACL. They used the anteromedial portal to create the PL femoral tunnel. In a prospective comparative cohort study of 72 patients who underwent either conventional single bundle ACL reconstruction (Fig. 5), non-anatomic double bundle ACL reconstruction (Fig. 6) or anatomic double bundle ACL reconstruction (Fig. 7) using polyester tape to increase graft length, they reported significantly less anterior tibial translational laxity and clinical pivot shift laxity in the anatomic double bundle ACL reconstruction group compared to the single bundle ACL reconstruction group. They concluded that the anatomic double bundle ACL reconstruction technique was superior to the single bundle ACL reconstruction technique. Differences, however, were not observed between their anatomic and non-anatomic double bundle ACL reconstruction techniques [117]. In a later study, Yasuda et al. [118] reported their results at 2 years post-surgery for 72 patients who underwent one of three different ACL reconstruction techniques performed by the same surgeon using STG autografts (Group I = single bundle, transtibial tunnel method, Group II = single tibial tunnel, double femoral tunnel, and Group III = double tibial tunnel and double femoral tunnels). Using the Noyes Subjective Knee Assessment they reported no group differences, however, at 30° knee flexion, Group III displayed less anterior tibial translational laxity than Group II, and Group II displayed less laxity than Group I. Group III also displayed less clinical pivot shift laxity compared to the other groups [118]. Ishibachi et al. [49] in performing an intraoperative evaluation of an anatomic double bundle ACL reconstruction technique reported “improved knee stability” and “biomechanical advantages”, however, no patient outcome data was reported. In a prospective, randomized controlled trial of 108 patients at 24–36 months following either conventional single bundle or anatomic double bundle ACL reconstruction using one tibial and two femoral tunnels and a STG autograft that was tensioned and fixed at 90° knee flexion, Adachi et al. [1] reported no differences between groups for anterior tibial translational laxity with the knee at 20° or 70° knee flexion or for knee joint position sense “proprioception” using passive joint angle reproduction accuracy measurements. Other than a reduced need for notchplasty with the anatomic double bundle ACL reconstruction group, they stated that they could not demonstrate an advantage using an anatomic double bundle ACL reconstruction rather than a conventional single bundle ACL reconstruction. Their study, however, did not evaluate transverse plane rotatory knee stability. Giron et al. [33] compared three different double bundle ACL reconstruction techniques (Group A = single bundle, Group B = double bundle (one tibial, two femoral tunnels), and Group C = double bundle (two tibial, two femoral tunnels). At 12 months post-surgery an independent clinical examination revealed no statistically significant advantage to either of the double bundle ACL reconstruction procedures. In a recent prospective, non-randomized study that compared three sequential groups of 25 patients following either single bundle, single incision transtibial ACL reconstruction, double bundle ACL reconstruction with a single incision transtibial technique, or a double bundle, two incision, outside-in technique at a minimum of 1 year [32] and then at 2 years post-surgery, Aglietti et al. [3] reported that patients who received the double bundle, two incision, outside-in ACL reconstruction had superior anteroposterior stability and less residual pivot shift instability than patients who received the single bundle, single incision transtibial ACL reconstruction. Summaries of clinical studies of anatomic double bundle ACL reconstruction function are reported in Table 4.
One femoral, one tibial tunnel anatomic double bundle ACL reconstruction with polyester tape extensions, endobutton femoral fixation, staple tibial fixation [118]
Two femoral, one tibial tunnel anatomic double bundle ACL reconstruction with polyester tape extensions, endobutton femoral fixation, staple tibial fixation [118]
Two femoral, two tibial tunnel anatomic double bundle ACL reconstruction with polyester tape extensions, endobutton femoral fixation, staple tibial fixation [118]
Three or more bundles
Min et al. [73] and Shino et al. [101] have reported using triple bundle ACL reconstruction techniques to include reconstruction of the intermediate ACL bundle (Fig. 8). Prodromos and Joyce [91] have reported using a five strand STG autograft (three semitendinosus, two gracilis strands) to improve knee stability. They suggested that this type of graft might be particularly useful for anatomic double bundle ACL reconstruction. Reports such as these reflect the continuing modifications and evolution of anatomic double bundle ACL reconstruction surgical techniques and the confusion associated with the use of differing terminology such as tunnel versus socket, graft bundle versus strand, and anatomic versus non-anatomic, etc.
Two femoral, three tibial tunnel anatomic triple bundle ACL reconstruction with endobutton femoral fixation and suture-mini-plate tibial fixation [101]
Discussion
Our literature review strongly suggests that quantitative measurements of the pivot shift phenomenon, transverse plane rotational knee instability, and patient function during sports activities following anatomic double bundle ACL reconstruction are extremely limited. Although basic science evidence provides support for some anatomic double bundle ACL reconstruction techniques, a breadth of differing techniques have been developed, few provide strong clinical evidence, and an even smaller number of randomized controlled studies have been performed [1]. Surgical innovations occur rapidly while basic and clinical scientific evidence follows behind more methodically at a comparatively slower rate in a seemingly perpetual game of “catch-up”. Given the relationship between innovative surgical techniques and product development, the cynic must ask, given the scarcity of quantitative objective data, are these techniques being developed primarily for improved patient care or for innovative surgeons to develop more interesting methods for correcting a problem that has largely already been corrected?
The intention of this literature review is to provide the knee surgeon with the existing evidence for anatomic double bundle ACL reconstruction and to provide suggested criteria that they should consider when selecting a particular technique. We suggest that in choosing to use an anatomic double bundle ACL reconstruction technique the knee surgeon should look for evidence of: (1) control of the pivot shift phenomenon, (2) improved transverse plane rotatory knee control during the performance of sports type movements, (3) a decreased likelihood of revision procedures either for ACL reconstruction or for treatment of associated primary or recurrent meniscal injuries, (4) improved patient self-reports of perceived function, satisfaction, and quality of life, and (5) radiographic evidence of a lower incidence and/or magnitude of osteoarthritic changes compared to conventional single bundle ACL reconstruction techniques. As Fu [26] has stated, however, objective quantitative assessment of the pivot shift phenomenon following ACL reconstruction is currently lacking and is greatly needed. In association with improved pivot shift and transverse plane rotatory knee control, evidence should be provided that the menisci are less likely to be injured and that the onset and magnitude of knee osteoarthritis can be better prevented.
We propose that given the current level of evidence, the knee surgeon has to ask which anatomic double bundle ACL reconstruction technique best replicates native ACL double bundle function with the least surgical technique complexity, and the least invasive revision technique requirement should it be needed? Most reports describe surgical techniques in great detail, however they provide very little, if any data regarding objective clinical patient outcomes and when outcomes data are reported they are usually for less than a 2-year post-operative period. Given the novelty of this method of ACL reconstruction, the absence of long-term patient outcome data is not surprising and the individuals or groups who have designed these innovations are no doubt in the process of acquiring these data. What is surprising, however, is the seemingly blind enthusiasm and minimal questioning that has followed the development and use of these techniques given their very limited evidence of efficacy. Ostensibly this has happened based on in vitro biomechanical test evidence using cadaveric knee specimens. From the results of these studies, proponents have suggested that patient outcomes should be better than those that would be obtained with a conventional single bundle ACL reconstruction technique. However, we currently do not know to what extent an anatomic double bundle ACL reconstruction positively influences patient function differently from a conventional single bundle ACL reconstruction. We question whether or not greater attention to a criteria based return to play conditioning program would provide similar or greater benefits to the patient as an anatomic double bundle ACL reconstruction [80, 81]? Another important question given the existing 80–90% success rates with conventional single bundle ACL reconstruction techniques, even with their 10–30% complication rates, is do all patients who require ACL reconstruction warrant an anatomic double bundle ACL reconstruction? Fu [26] has suggested that patients may vary in their dependence on double bundle ACL function for transverse plane rotational knee stability. Recently when asked this question, Dr. Alberto Gobbi (personal communication) stated that he believed that in the future, both conventional single bundle and anatomic double bundle ACL reconstruction techniques would be used, with the latter technique being reserved for patients who have greater transverse plane rotatory knee stress demands. Can we prospectively screen high-risk individuals to determine which ones have greater transverse plane requirements?
Reports have suggested that the osteoarthritis progression may continue following initial knee injury even if the ACL is reconstructed [8, 24, 83, 111], particularly if the patient has an associated meniscal injury [19, 43] and/or chooses to continue participating in sports activities that require pivoting, cutting, sudden stopping, and jump landing movements. Some have suggested that this progression is the same or worse than it would have been if the ACL were not reconstructed, particularly when a recurrent functional pivot shift exists [53, 54, 57, 58]. Conceivably, an anatomic double bundle ACL reconstruction should better control this. Do proponents of anatomic double bundle ACL reconstruction techniques propose that all patients who have sustained an ACL injury undergo this procedure so that they can more quickly return to unabated sporting activities following expedited rehabilitation? Given the aforementioned evidence that ACL reconstruction alone may not mitigate the knee osteoarthritis progression, will re-creation of anatomic double bundle ACL function alone make a substantial difference in delaying or preventing the knee osteoarthritis onset and progression by better controlling the pivot shift and enhancing transverse plane rotational knee control [123]? How should ACL deficient patients be counseled regarding their upcoming surgery? Should they be told that because of its improved transverse plane rotatory knee stability, having undergone an anatomic double bundle ACL reconstruction they will be better prepared to return to sporting activities than an individual who has undergone a conventional single bundle ACL reconstruction? Although this is currently unsubstantiated, assumedly the answer to this question would be yes, however, what is said regarding the knee osteoarthritis progression? Should revision be needed, what is said to the patient regarding how their selection of an anatomic double bundle ACL reconstruction may influence revision surgery complexity should it be needed? Given the plethora of anatomic double bundle ACL reconstruction techniques that have been reported, prior to selecting a particular technique it would seem that the knee surgeon should have reflected on and developed evidence based answers for each of these questions well in advance of any of these eventualities.
Another concern is whether or not the rehabilitation program or functional milestone progression should differ for patients who have undergone an anatomic double bundle ACL reconstruction? Conceivably, if this procedure provides superior transverse plane rotatory knee stability, should the essential rehabilitation program milestones have earlier and higher level dynamic transverse plane rotational knee stability performance expectations, particularly regarding the composite lower extremity neuromuscular control that is so vital to 3D dynamic knee postural stability? Reported rehabilitation progressions do not seem to identify any substantive differences from practices commonly used following conventional single bundle ACL reconstruction (Table 5). Also, how should functional pivot shift control and transverse plane rotational knee stability during the performance of sporting movements be quantified with repeated long-term measurements? Where are we in developing more objective methods to increase both the measurement precision and the functional relevance of our standard clinical examination tests? As mentioned earlier, perhaps the same or similar technology that has recently been developed for surgical navigation and ACL reconstruction integrity evaluation in the operating room can be integrated into the clinic to quantify these factors that are so essential to determining surgical and rehabilitative intervention effectiveness and long-term patient outcome [57, 58].
When selecting between conventional single bundle and anatomic double bundle ACL reconstruction techniques, the knee surgeon needs to also consider how it will impact graft fixation options. For example, when two femoral tunnels are created, or when a more horizontally placed single femoral tunnel technique is used, cross-pin fixation methods are eliminated from consideration. While interference screws certainly have advantages when performing these procedures, metal screws make MRI visualization difficult and would be particularly problematic should revision be necessary with an anatomic double bundle ACL reconstruction. While devices such as endobuttons or staples are useful for soft tissue tendon graft fixation with anatomic double bundle ACL reconstruction techniques, the knee surgeon must be cognizant of their number (particularly when multiple tunnels are used), their material (metal or synthetics, versus bioabsorbable), and their influence on graft-tunnel healing and remodeling, particularly to avoid long-term instability associated with tunnel widening and windshield wiper or bungee cord effects [97].
As anatomic double bundle ACL reconstruction techniques continue to evolve with tremendous promise, but very limited evidence, other patient care factors such as appropriate patient selection and education, behavioral change needs, and functionally valid criteria upon which to base return to sporting activity readiness continue to lag behind [80, 81]. Concurrently, a growing body of patient outcome studies with more than 10–20-year data following conventional single bundle ACL reconstruction are accumulating a substantial body of evidence supporting their efficacy [25]. Although further development of anatomic double bundle ACL reconstruction techniques will and should occur, and larger, better designed patient outcome studies will be forthcoming, it is vital that the orthopaedic surgery community reflects upon whether or not it should be placing similar or greater emphasis on these other patient care factors. Anatomic double bundle ACL reconstruction should provide superior pivot shift resistance and thereby with appropriate rehabilitation should increase the likelihood for patients to develop improved transverse plane rotatory knee control than conventional single bundle ACL reconstruction. Questions remain, however, if it will serve to better protect the menisci and mitigate the onset and progression of osteoarthritic knee changes and if the increased surgical complexity and revision potential justifies any potential benefits.
References
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y (2004) Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg 86B(4):515–520
Aglietti P, Cuomo P, Giron F, Boerger TO (2005) Double-bundle anterior cruciate ligament reconstruction: Surgical technique. Oper Tech Orthop 15(2):111–115
Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N (2007) Single- and double-incision double-bundle ACL reconstruction. Clin Orthop 454:108–113
Ahn JH, Lee SH (2007) Anterior cruciate ligament double-bundle reconstruction with hamstring tendon autografts. Arthroscopy 23(1):109.e1–109.e4
Amis AA, Bull AMJ, Lie DTT (2005) Biomechanics of rotational instability and anatomic anterior cruciate ligament reconstruction. Oper Tech Orthop 15(1):29–35
Amis AA, Dawkins GPC (1991) Functional anatomy of the anterior cruciate ligament: fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg 73B(2):260–267
Arnoczky SP (1983) Anatomy of the anterior cruciate ligament. Clin Orthop 172:19–25
Asano H, Muneta T, Ikeda H et al (2004) Arthroscopic evaluation of the articular cartilage after anterior cruciate ligament reconstruction: a short-term prospective study of 105 patients. Arthroscopy 20(5):474–481
Bell K, Egan M, Fu F, Gilbertson L, Smolinski P (2006) Assessment of femoral fracture risk: a finite element analysis of single versus double-bundle ACL reconstruction. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #41
Bellier G, Christel P, Colombet P et al (2004) Double-stranded hamstring graft for anterior cruciate ligament reconstruction. Arthroscopy 20(8):890–894
Brucker PU, Zelle BA, Fu FH (2005) Inflammatory response to intraarticular suture placement in anatomic anterior cruciate ligament double-bundle reconstruction: a case study. Oper Tech Orthop 15(2):151–153
Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH (2006) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 22(9):1000–1006
Caborn DN, Chang HC (2005) Single femoral socket double-bundle anterior cruciate ligament reconstruction using tibialis anterior tendon: description of a new technique. Arthroscopy 21(10):1273.e1–1273.e8
Cha PS, Brucker PU, West RV et al (2005) Arthroscopic double-bundle anterior cruciate ligament reconstruction: an anatomic approach. Arthroscopy 21:1277.e1–1277.e8
Christel P, Franceschi JP, Sbihi A et al (2005) Anatomic anterior cruciate ligament reconstruction: the French experience. Oper Tech Orthop 15(2):103–110
Colombet P, Robinson J, Christel P et al (2006) Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy 22(9):984–992
Cuomo P, Boddu Siva Rama RK, Bull AMJ, Amis AA (2006) The effect of different tensioning strategies on knee kinematics after double-bundle anterior cruciate ligament reconstruction. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #40
Dodds JA, Arnoczky SP (1994) Anatomy of the anterior cruciate ligament: A blueprint for repair and reconstruction. Arthroscopy 10(2):132–139
Englund M, Roos EM, Lohmander LS (2003) Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a 16-year follow-up of meniscectomy with matched controls. Arth Rheum 48(8):2178–2187
Eriksson E (2005) Preface. Do we need to perform double-bundle anterior cruciate ligament reconstructions? Oper Tech Orthop 15(1):4
Eriksson E (2006) Single-bundle, double-bundle or triple-bundle? Knee Surg Sports Traumatol Arthrosc 14(6):503–504
Feller JA (2005) Graft choices for anterior cruciate ligament reconstruction. ISAKOS Winter Newsletter
Ferretti M, Levicoff E, McPherson T, Zelle B, Fu F (2006) The two bundles of the anterior cruciate ligament: anatomical and histological study in human fetuses. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #36
Fink C, Hoser C, Hackl W, Navarro RA, Benedetto KP (2001) Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture—is sports activity a determining variable? Int J Sports Med 22:304–309
Fink C, Pflüglmayer M, Tecklenburg K, Irenberger A, Hoser C (2006) 20–25-year follow-up of operative versus non-operative treatment of anterior cruciate ligament rupture. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #44
Fu FH (2005) Editorial: anatomic anterior cruciate ligament reconstruction: the next evolution. Oper Tech Orthop 15(2):85
Fu FH, Zelle BA, Beasley LS (2005) The double-bundle technique: the restoration of normal kinematics. Proceedings of Arthroscopy Association of North America 2005 Specialty Day, Washington, DC, February 26, 2005, pp 284–289
Fu FH, Starman JS, Ferretti M (2006) Anatomic double bundle ACL reconstruction: the restoration of normal knee kinematics. In: Symposia sports/arthroscopy: controversies in soft tissues ACL reconstruction: Allograft vs. autograft, double tunnel vs. single tunnel, cortical vs. aperture fixation. Symposium at the 73rd Annual Meeting of the American Academy of Orthopaedic Surgeons, Chicago, IL, March 22–26, 2006, pp 384–385
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22(1):85–89
Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N (2003) Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med 31(1):75–79
Girgis FG, Marshall JL, Monajem A (1975) The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop 106:216–231
Giron F, Aglietti P, Cuomo P, Losco M, Mondanelli N (2006) Double-bundle ACL reconstruction: Single versus double incision. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #43
Giron F, Aglietti P, Mondanelli N, Cuomo P (2006) Single versus double bundle techniques in ACL reconstruction using a DSTG graft. Preliminary results. Proceedings of the 5th Biennial ISAKOS Congress, Hollywood, Florida, April 3–7, 2005, Oral Presentation #56
Giron F, Buzzi R, Aglietti P (1999) Femoral tunnel position in anterior cruciate ligament reconstruction using three techniques. A cadaver study. Arthroscopy 15(7):750–756
Griffin LY, Agel J, Albohm MJ et al (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8(3):141–150
Ha CW (2005) Improved technique of anatomic reconstruction of anteromedial and posterolateral bundles of ACL—a split double-bundle technique. Proceedings of the 5th Biennial ISAKOS Congress, Hollywood, Florida, April 3–7, 2005, E-poster # 337
Hamada M, Shino K, Horibe S et al (2001) Single-versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with endobutton femoral fixation: a prospective study. Arthroscopy 17(8):801–807
Hara K, Arai Y, Ohta M et al (2005) A new double-bundle anterior cruciate ligament reconstruction using the posteromedial portal technique with hamstrings. Arthroscopy 21(10):1274.e1–1274.e6
Hara K, Kubo T, Suginoshita T, Shimizu C, Hirasawa Y (2000) Reconstruction of the anterior cruciate ligament using a double bundle. Arthroscopy 16(8):860–864
Harner CD, Baek GH, Vogrin TM et al (1999) Quantitative analysis of human cruciate ligament insertions. Arthroscopy 15(7):741–749
Harner CD, Fu FH, Irrgang JJ, Vogrin TM (2001) Anterior and posterior cruciate ligament reconstruction in the new millennium: A global perspective. Knee Surg Sports Traumatol Arthrosc 9:330–336
Harner CD, Poehling GG (2004) Double bundle or double trouble? Arthroscopy 20(10):1013– 1014
Hart AJ, Buscombe J, Malone A, Dowd GSE (2005) Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at 10 years. J Bone Joint Surg 87B(11):1483–1487
Hill PF, Vedi V, Williams A et al (2000) Tibiofemoral movement 2: The loaded and unloaded living knee studied by MRI. J Bone Joint Surg 82B:1196–1198
Hole RL, Lintner DM, Kamaric E, Moseley JB (1996) Increased tibial translation after partial sectioning of the anterior cruciate ligament: the posterolateral bundle. Am J Sports Med 24(4):556–560
Hufner T, Meller R, Kendoff D et al (2005) The role of navigation in knee surgery and evaluation of three-dimensional knee kinematics. Oper Tech Orthop 15:64–69
Ichiyama H, Yasuda K, Kondo E, Azuma C, Tohyama H (2005) An in vivo study on tension changes in the anteromedial and posterolateral bundles created with the anatomical two-route anterior cruciate ligament reconstruction procedure. Proceedings of the 5th Biennial ISAKOS Congress, Hollywood, Florida, April 3–7, 2005, Oral Presentation #119
Irrgang JJ (1993) Modern trends in anterior cruciate ligament rehabilitation: Nonoperative and postoperative management. Clin Sports Med 12:797–813
Ishibashi Y, Tsuda E, Tazawa K, Sato H, Toh S (2005) Intraoperative evaluation of the anatomical double-bundle anterior cruciate ligament reconstruction with the OrthoPilot navigation system. Orthop 28(10):s1277–s1282
Ito M, Murase K, Tanaka S, Takahei T, Nakamura, N (2005) Clinical and anatomical study about double bundles in the anterior cruciate ligament. Proceedings of the 5th Biennial ISAKOS Congress, Hollywood, Florida, April 3–7, 2005, E-poster #156
Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg 82B:1189–1195
Johnson D (2006) Pro single bundle ACL reconstruction. In: Symposia sports/arthroscopy: controversies in soft tissues ACL reconstruction: Allograft vs. autograft, double tunnel vs. single tunnel, cortical vs. aperture fixation. Symposium at the 73rd Annual Meeting of the American Academy of Orthopaedic Surgeons, Chicago, IL, March 22–26, 2006, pp 388–389
Jonsson H, Riklund-Ahlstrom K, Lind J (2004) Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand 75(5):594–599
Kanamori A, Woo SLY, Ma CB et al (2000) The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot shift test: a human cadveric study using robotic technology. Arthroscopy 16:633–639
Khalfayan EE, Sharkey SF, Alexander HA et al (1996) The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med 24:335–341
Kim SJ, Jung KA, Song DH (2006) Arthroscopic double-bundle anterior cruciate ligament reconstruction using autogenous quadriceps tendon. Arthroscopy 22(7):797.e1–797.e5
Kocher M, Steadman J, Briggs K, Sterett W, Hawkins R (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32:629–634
Kocher MS, Steadman JR, Briggs K et al (2002) Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg 84A(9):1560–1572
Koh JSB, Nagai T, Motojima S, Sell TC, Lephart SM (2005) Concepts and measurement of in vivo tibiofemoral kinematics. Oper Tech Orthop 15:43–48
Kubo T, Hara K, Suginoshita T et al (2000) Anterior cruciate ligament reconstruction using the double bundle method. J Orthop Surg (Hong Kong) 8(2):59–63
Kummer B, Yamamoto Y (1988) Funktionelle anatomie der kruzbaender. Arthroscopie 1:2–10
Kurosawa H, Yamakoshi K, Yasuda K, Sasaki T (1991) Simultaneous measurement of changes in length of the cruciate ligaments during knee motion. Clin Orthop 265:233–240
Levicoff EA, Ferretti M, Macpherson TA et al (2006) An anatomical and histological evaluation of the developing ACL in the fetus. Proceedings of the 52nd Annual Meeting of the Orthopaedic Research Society. Chicago, IL, March 19–26, 2006, Paper #1160
Li G, Moses JM, Papannagari R et al (2006) Anterior cruciate ligament deficiency alters the in vivo motion of the tibiofemoral cartilage contact points in both the anteroposterior and mediolateral directions. J Bone Joint Surg 88A(8):1826–1834
Loh JC, Fukuda Y, Tsuda E et al (2003) Knee stability and graft function following anterior cruciate ligament reconstruction: Comparison between 11 o’clock and 10 o’clock femoral tunnel placement. Arthroscopy 19(3):297–304
Mae T, Shino K, Matsumoto N et al (2006) Force sharing between two grafts in the anatomical two-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 14(6):505–509
Mae T, Shino K, Miyama T et al (2001) Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: Biomechanical analysis using a robotic simulator. Arthroscopy 17(7):708–716
Marcacci M, Molgora AP, Zaffagnini S et al (2003) Anatomic double-bundle anterior cruciate ligament reconstruction with hamstrings. Arthroscopy 19(5):540–546
Marcacci M, Zaffagnini S, Iacono F et al (2006) Prospective randomized study of single plus lateral plasty versus double bundle ACL technique at minimum 3 years follow-up. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #37
Marcacci M, Zaffagnini S, Marchesini L, Delcogliano M, Bruni D (2005) Anatomic anterior cruciate ligament reconstruction using the over-the-top passage of hamstring tendons. Oper Tech Orthop 15(2):123–129
Markolf KL, Burchfield DM, Shapiro MM et al (1995) Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res 13:930–935
Martelli S, Zaffagnini S, Bignozzi S, Bontempi M, Marcacci M (2006) Validation of a new protocol for computer-assisted evaluation of kinematics of double-bundle ACL reconstruction. Clin Biomech 21(3):279–287
Min B, Roh J, Jin C, Song K (2005) Intra-articular triple bundle technique for anterior cruciate ligament reconstruction. Proceedings of the 5th Biennial ISAKOS Congress, Hollywood, Florida, April 3–7, 2005, E-poster #442
Miyasaka T, Matsumoto H, Suda Y et al (2002) Coordination of the anterior and posterior cruciate ligaments in constraining the varus-valgus and internal-external rotatory instability of the knee. J Orthop Sci 7:348–353
Mochizuki T, Muneta T, Nagase T et al (2006) Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy 22:356–361
Morgan CD, Caborn D (2005) Anatomic graft fixation using a retrograde biointerference screw for endoscopic anterior cruciate ligament reconstruction single-bundle and 2-bundle techniques. Tech Orthop 20(3):297–302
Mott HW (1983) Semitendinosus anatomic reconstruction for cruciate ligament insufficiency. Clin Orthop 172:90–92
Muneta T, Sekiya I, Yagishita K et al (1999) Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy 15(6):618–624
Musahl V, Plakseychuk A, VanScyoc A et al (2005) Varying femoral tunnels between the anatomical footprint and isometric positions: Effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med 33(5):712–718
Myer GD, Paterno MW, Ford KR et al (2006) Rehabilitation after anterior cruciate ligament reconstruction: Criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther 36(6):385–402
Myklebust G, Bahr R (2005) Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med 39:127–131
Norwood LA, Cross MJ (1979) Anterior cruciate ligament: Functional anatomy of its bundles in rotatory instabililities. Am J Sports Med 7:23–26
Noyes F, Mooar P, Matthews D et al (1983) The symptomatic anterior cruciate-deficient knee. Part I The long-term functional disability in athletically active individuals. J Bone Joint Surg 65A:154–162
Odensten M, Gillquist J (1985) Functional anatomy of the anterior cruciate ligament and a rationale for reconstruction. J Bone Joint Surg 67A:257–262
Ogawa T, Takeda Y, Fujii K et al (2006) Can the double-bundle technique restore the normal tibiofemoral relationship after successful ACL reconstruction? Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #42
Otsubo H, Nakamura N, Nakata K et al (2006) Arthroscopic evaluation of anatomic two-bundle anterior cruciate ligament reconstruction using hamstring tendon autograft. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #33
Paessler H (1997) Revisionseingriffe nach vorderer Kreuzbandoperation underneuerlicher Instabilitat: Ursachenanalyse und taktische Vorgehen. Hefte zu “Der Unfallchirurg” 268:447–450
Pederzini L, Adriani E, Botticella C, Tosi M (2000) Technical note: double tibial tunnel using quadriceps tendon in anterior cruciate ligament reconstruction. Arthroscopy 16(5):9e
Petersen W, Tretow H, Weimann A et al (2006) Biomechanical evaluation of two techniques for double bundle ACL reconstruction: One tibial tunnel versus two tibial tunnels. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #38
Powers DL, Jacob PA, Drews MJ (1991) Anatomical reconstruction of the anterior cruciate ligament in goats. J Investigative Surg 4(2):191–202
Prodromos C, Joyce B (2006) Five strand hamstring anterior cruciate ligament reconstruction: presentation of a new technique with better stability at 7–9-year follow-up than four strand. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #84
Radford WJ, Amis AA, Kempson SA, Stead AC, Camburn M (1994) A comparative study of single-and double-bundle ACL reconstructions in sheep. Knee Surg Sports Traumatol Arthrosc 2(2):94–99
Radford WJ, Amis AA (1990) Biomechanics of a double prosthetic ligament in the anterior cruciate deficient knee. J Bone Joint Surg 72B(6):1038–1043
Ristanis S, Giakas G, Papageorgiou CD et al (2003) The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surg Sports Traumatol Arthrosc 11(6):360–365
Ristanis S, Stergiou N, Patras K et al (2006) Follow-up evaluation 2 years after ACL reconstruction with bone-patellar tendon-bone graft shows that excessive tibial rotation persists. Clin J Sports Med 16:111–116
Ristanis S, Stergiou N, Patras K et al (2005) Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy 21:1323–1329
Rodeo SA, Kawamura S, Kim HJ et al (2006) Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit. Am J Sports Med 34(11):1790–1800
Sakane M, Fox RJ, Woo SL et al (1997) In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res 15(2):285–293
Sbihi A, Franceschi JP, Christel P et al (2004) Anterior cruciate ligament reconstruction: biomechanical comparison on cadaver specimens using a single or double hamstring technique. Rev Chir Orthop Reparatrice Appar Mot 90(7):643–650
Shafizadeh S, Huber HJ, Grote S et al (2005) Principles of fluoroscopic-based navigation in anterior cruciate ligament reconstruction. Oper Tech Orthop 15:70–75
Shino K, Nakata K, Nakamura N et al (2005) Anatomic anterior cruciate ligament reconstruction using two double-looped hamstring tendon grafts via twin femoral and triple tibial tunnels. Oper Tech Orthop 15:130–134
Shino K, Nakata K, Nakamura N et al (2005) Anatomically oriented anterior cruciate ligament reconstruction with a bone-patellar tendon-bone graft via rectangular socket and tunnel: a snug- fit and impingement-free grafting technique. Arthroscopy 21(11):1402.e1–1402.e5
Siebold R, Dehler C (2006) ACL reconstruction with hamstrings: prospective randomized comparison of “double-bundle” to “single-bundle” technique. Proceedings of the 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #45
Steckel H, Starman JS, Baums MH et al (2006) Anatomy of the anterior cruciate ligament double bundle structure: a macroscopic evaluation. Scand J Med Sci Sports (online first)
Suginoshita T, Tsukahara T, Yoshiaki K, Komiyama H, Kubo T (2005) Suprcondylar femoral fracture after double bundle anterior cruciate ligament reconstruction using hamstring tendons: report of a case. Proceedings of the 5th Biennial ISAKOS Congress, Hollywood, FL, April 3–7, 2005, EPoster #387
Takahashi M, Doi M, Abe M, Suzuki D, Nagano A (2006) Anatomical study of the femoral and tibial insertions of the anteromedial and posterolateral bundles of human anterior cruciate ligament. Am J Sports Med 34:787–792
Takeuchi R, Saito T, Mituhashi S et al (2002) Double-bundle anatomic anterior cruciate ligament reconstruction using bone-hamstring-bone composite graft. Arthroscopy 18(5):550–555
Tashman S, Collon D, Anderson K, Kolowich P, Anderst W (2004) Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 32(4):975–983
Toritsuka Y, Shino K, Horibe S et al (2004) Second-look arthroscopy of anterior cruciate ligament grafts with multistranded hamstring tendons. Arthroscopy 20(3):287–293
Vidal AF, Brucker PU, Fu FH (2005) Anatomic double-bundle anterior cruciate ligament reconstruction using tibialis anterior tendon allografts. Oper Tech Orthop 15(2):140–145
Von Porat A, Roos EM, Roos H (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63(3):269–273
Weimann A, Tretow H, Zantop T et al (2006) Biomechanical evaluation of two techniques for double bundle ACL reconstruction: one tibial tunnel versus two tibial tunnels. Proceedings of the 52nd Annual Meeting of the Orthopaedic Research Society. Chicago, IL, March 19–26, 2006. Paper #1140
Woo SL, Kanamori A, Zeminski J et al (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg 84A(6):907–914
Yagi M, Kuroda R, Hoshino Y et al (2006) Prospective-randomized comparison of single antero-medial, single postero-lateral and anatomic ACL reconstruction. 12th ESSKA 2000 Congress, Innsbruck, Austria, May 24–27, 2006, Oral Presentation #32
Yagi M, Wong EK, Kanamori A et al (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30(5):660–666
Yamamoto Y, Hsu WH, Woo SL et al (2004) Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med 32(8):1825–1832
Yasuda K, Kondo E, Ichiyama H et al (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20(10):1015–1025
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among three different procedures. Arthroscopy 22(3):240–251
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2005) Surgical and biomechanical concepts of anatomic anterior cruciate ligament reconstruction. Oper Tech Orthop 15(2):96–102
Zantop T, Haase A, Weimann A et al (2006) Bridge stability: Impact of bridge width in double bundle ACL reconstructions on the structural properties of the graft/femur complex. Proceedings of the 52nd Annual Meeting of the Orthopaedic Research Society. Chicago, IL, March 19–26, 2006, Paper #1139
Zaricznyj B (1987) Reconstruction of the anterior cruciate ligament of the knee using a doubled tendon graft. Clin Orthop 220:162–175
Zelle BA, Brucker PU, Feng MT, Fu FH (2006) Anatomical double-bundle anterior cruciate ligament reconstruction. Sports Med 36(2):99–108
Zelle BA, Herzka AS, Harner CD, Irrgang JJ (2005) Evaluation of clinical outcomes in anterior cruciate ligament surgery. Oper Tech Orthop 15:76–84
Zhao J, Peng X, He Y, Wang J (2006) Two-bundle anterior cruciate ligament reconstruction with eight-stranded hamstring tendons: Four-tunnel technique. Knee 13:36–41
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Crawford, C., Nyland, J., Landes, S. et al. Anatomic double bundle ACL reconstruction: a literature review. Knee Surg Sports Traumatol Arthr 15, 946–964 (2007). https://doi.org/10.1007/s00167-007-0343-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-007-0343-7